Abstract
Objective
The aim of this study was to examine associations of smoking at the time of diagnosis with the risk of prostate cancer death in a population-based cohort of men with prostate cancer.
Methods
Data were from 752 prostate cancer patients aged 40–64 years, who were enrolled in a case–control study and under long-term follow-up for mortality. Cox proportional hazards models were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for associations between smoking and prostate cancer-specific and other cause mortality.
Results
Compared to never smoking, smoking at the time of diagnosis was associated with a significant increase in risk of prostate cancer-specific mortality. After controlling for demographic characteristics, Gleason grade, stage at diagnosis, and primary treatment, the HR was 2.66 (95% CI: 1.10–6.43).
Conclusions
Smoking at the time of diagnosis, independent of key clinical prognostic factors, is associated with an increased risk of prostate cancer death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many epidemiological studies have examined the association between smoking and prostate cancer incidence and found, overall, that smoking does not increase prostate cancer risk [1]. However, at least seven large cohort studies have reported that smoking at the time of study entry increased the risk of prostate cancer death [2–8]. These seemingly discordant findings could be due to an association of smoking with higher grade or more advanced stage disease at the time of diagnosis [9, 10], or could also be attributable to effects of smoking on the outcome of prostate cancer following its initial diagnosis and treatment. Only six studies [11–16], with inconsistent findings, have examined the association of smoking at the time of diagnosis with prostate cancer outcomes. Three of such studies are limited to cohorts of men treated with radiation therapy [11, 12] or with advanced prostate cancer receiving androgen deprivation therapy (ADT) [13]. Two other studies only included men diagnosed at a single medical center and the follow-up period was short [14, 15]. One study has examined smoking and prostate cancer outcomes among men receiving radical prostatectomy, which is the treatment most often used for relatively healthy, younger men with local stage disease, but this study was small and analyses were not fully controlled for covariates [16]. Thus, current research is far too limited to draw conclusions regarding the effects of smoking on prostate cancer outcomes.
In this study, we address whether smoking, both at and prior to the time of diagnosis, affects subsequent risk of prostate cancer death. Unlike previous studies, our sample is population-based and thus includes men who were diagnosed with all grades and stages of the disease and who received a range of initial treatments. Results from this study are relevant to the question of whether smoking cessation after prostate cancer diagnosis could improve survival.
Materials and methods
Study participants and data collection
Study participants were 752 newly diagnosed prostate cancer patients who were enrolled in a population-based case–control study. Details on the design of this study have been described previously [17]. Briefly, eligible participants were Caucasian and African-American male residents of King County (Seattle) Washington, ages 40–64 years, who were newly diagnosed with histologically-confirmed prostate cancer from 1 January 1993 through 31 December 1996. All cases were identified through the Seattle-Puget Sound SEER cancer registry and included all patients aged 40–59 years and a random 75% sample of whites aged 60–64 years at diagnosis.
All study participants provided informed consent for participation. Participants completed a structured in-person interview conducted by trained male interviewers. Detailed information was collected on demographic (e.g., age, race, and education) and lifestyle characteristics, anthropometry (height, weight), family history of prostate cancer, and medical and prostate cancer screening histories. A detailed lifetime smoking history prior to the cancer diagnosis date was collected, which included ages at onset and cessation, duration, and dose of cigarette smoking. Tumors were graded using the Gleason scoring system [18], and classified into 2–6, 7 with a primary pattern of 3 (3 + 4), and 7 with a primary pattern of 4 (4 + 3) or 8–10. The 7 (3 + 4) category included 22 patients with a Gleason score of 7 but unknown predominant grades. Cancer stage was defined by SEER as localized (Stages A and B, confined to the prostate), regional (Stage C, regional spread outside the prostatic capsule), and distant (Stage D, metastases) using pathological data for men undergoing radical prostatectomy and clinical information for all others [19]. The patient cohort is linked to the SEER database quarterly to ascertain vital status and underlying cause of death if deceased.
Endpoints
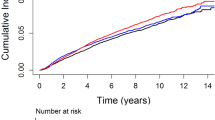
Two mortality endpoints were examined: prostate cancer-specific and other cause mortality. For patients who died, the primary cause of death was determined through the SEER registry, which obtains mortality data from the state of Washington, and verified by death certificates. Of the 752 patients in this cohort, 54 died of prostate cancer and 81 died of other causes.
Statistical analysis
Unadjusted prostate cancer-specific and other cause mortality rates were calculated by dividing the number of deaths by the corresponding number of person-years of follow-up. Cox proportional hazard models were used to estimate hazard ratios (HR) and 95% confidence intervals (CI) for prostate cancer-specific and other cause mortality [20]. Survival time, defined as time from diagnosis to death, was the time-dependent variable used in the analysis. The censoring date for living cases was 1 June 2007, the most recent date that participants were matched with the cancer registry database.
All analyses were adjusted for age, race, education, BMI, total energy and the percentage energy from fat intake, Gleason score, cancer stage at diagnosis, and primary treatment. Controlling for other variables including family history of prostate cancer, PSA level at diagnosis, alcohol intake, and exercise did not materially affect parameter estimates and were therefore not included in final models. Tests for linear trend across categories were performed by modeling smoking as an ordinal variable in the model that included the covariates, as described by Breslow and Day [21].
We also examined the effect of cigarette smoking on prostate cancer mortality within strata defined by Gleason score, stage of disease at diagnosis, primary treatment, and co-morbid conditions, and tested whether effects of smoking differed across these strata using the likelihood ratio test.
Results
Table 1 gives the distributions of demographic and clinical characteristics of study participants and corresponding unadjusted mortality rates for prostate cancer-specific and other cause mortality. Most men were Caucasian, had been diagnosed with localized stage and Gleason score <7 cancer, and were treated with radical prostatectomy. Sixteen percent of men smoked cigarettes at the time of diagnosis and 11% had quit within the 10-year period before diagnosis. Unadjusted prostate cancer-specific mortality rates were higher among men who were current smokers, African-Americans, obese, diagnosed with regional or distant stage disease or treated with radiation or ADT, or who had ≥42% energy from fat, a serum PSA level of 20.0 ng/ml or greater, or a tumor classified as a Gleason score of 7 (3 + 4) or higher. Other cause mortality was higher among smokers, but did not differ by Gleason score, cancer stage, or serum PSA level.
Table 2 gives adjusted hazard ratios for associations of smoking with risk of prostate cancer-specific and other cause mortality. As expected, smoking was strongly associated with other cause mortality, and it was also strongly associated with prostate cancer-specific mortality. Compared to never smokers, smokers at the time of diagnosis had a 2.66 relative hazard of prostate cancer-specific death (P = 0.03). Overall, there was no significant difference in risk between never and former smokers. However, after stratifying men into those who had quit <10 or ≥10 years before diagnosis, recent quitters had a modest increase in risk of prostate cancer-specific mortality (HR: 1.48, P = 0.48), whereas those who had quit 10 or more years before diagnosis had a decreased risk (HR: 0.45, P = 0.06). There was an increase in risk of prostate cancer-specific mortality with increasing total pack-years smoked during the 10 years preceding diagnosis, but the trend was not statistically significant (P for trend among smokers at or within 10 years of diagnosis date was 0.86); results were similar among the subgroup of men who were smokers at the time of diagnosis (data not shown).
We also examined associations of smoking with risk of prostate cancer-specific mortality, stratified by Gleason score (2–6 or 7 (3 + 4) vs. 7 (4 + 3) or 8–10), stage at diagnosis (local vs. regional/distant), primary treatment (radical prostatectomy vs. other), and co-morbidity status (yes vs. none). Associations did not differ significantly across these strata. However, comparing smokers at the time of diagnosis to never smokers, hazard ratios for prostate cancer mortality were larger for men with local stage disease (HR: 6.28, 95% CI: 1.54–25.58), men receiving radical prostatectomy (HR: 10.48, 95% CI: 2.0–55.0), or men without any co-morbid conditions (HR: 5.53, 95% CI: 1.57–19.48). Larger studies will be necessary to address whether the effect of smoking differs in these subgroups. We also examined whether study findings could be confounded by use of secondary treatments, but found no differences in use of secondary treatments by smoking status.
Discussion
In this study of men under age 65 when diagnosed with prostate cancer, smoking at the time of diagnosis was associated with a 2.66 relative hazard of prostate cancer-specific death. Men who had quit within the 10 years before diagnosis had a non-significant 1.48 relative hazard of prostate cancer-specific death.
Six studies have examined the association of smoking at the time of diagnosis with risk of prostate cancer death. Pickles et al. [11] followed 601 men with local stage cancer receiving external beam radiation treatment for a median of 59 months and documented 28 prostate cancer deaths; they reported a non-significant increase (6-year prostate death rate 10% in smokers vs. 3.7% in former and non-smokers, P = 0.08) in prostate cancer-specific death. Pantarotto et al. [12] followed a cohort of 434 men with local stage prostate cancer receiving external beam radiation treatment for a median of 70 months, documenting 58 deaths; the relative hazards for prostate cancer-specific mortality were 1.78 (P = 0.18) and 1.39 (P = 0.55) for previous and current smokers, respectively. Oefelein et al. followed a cohort of 222 who were diagnosed with metastatic disease or had developed metastases after previous treatment for a median of 141 months, documenting 77 deaths; median overall survival time was 38, 47 and 60 months in current, former or never smokers, respectively (P = 0.00001) [13]. Yu et al. reported that ever smokers had a 1.46 relative hazard for prostate caner-specific death compared to non-smokers [14]. Daniell followed 235 men with non-stage A cancer and documented 57 deaths, the 5-year prostate cancer-specific mortality was 39% in smokers and 17% in nonsmokers (P < 0.001) [15]. Finally, Jager et al. followed a cohort of 214 men diagnosed with regional stage disease for a median of 50 months and documented 47 prostate cancer deaths; they reported that smokers had a 3.2 relative hazard for prostate cancer-specific death compared to non-smokers, and found a similar association among 194 men who received radical prostatectomy, but these analyses were not controlled for key covariates such as age [16]. Our study differs from these studies in several aspects. Our patients were incident cases identified from a population-based cancer registry, and included all men regardless of cancer stage or treatment; previous studies included only men receiving radiation treatment, men with regional stage or metastatic disease, or men from a single medical cancer. Our study patients were also younger and our median follow-up period was longer than in other studies. It is possible that findings on smoking and prostate cancer outcomes would have been more uniform across studies if there had been longer follow-up and less competitive mortality from other causes.
Our results regarding mortality among men who had quit smoking before cancer diagnosis are difficult to interpret. Compared to never smokers, men who stopped smoking 10 or more years before diagnosis had a lower risk of prostate cancer-specific mortality after control for prognostic factors such as grade and stage. The reason for this result is unclear, but it may be due to confounding by healthy behaviors associated with quitting smoking when younger or it could simply be due to chance. Men who stopped smoking within 10 years of diagnosis had only a modest, non-significantly increased risk of prostate cancer death.
Studies evaluating the risk of prostate cancer-specific mortality are difficult, both because attributing cause of death to prostate cancer may be biased and because mortality from prostate cancer generally occurs more than a decade after diagnosis. We carefully considered whether attribution of death to prostate cancer could be biased by smoking, because smokers have a higher death rate overall. If this was true, we would expect a stronger association of smoking with prostate cancer mortality among men with other co-morbid conditions. Instead, we found a larger hazard ratio for prostate cancer-specific mortality among men reporting no other co-morbid conditions. Our participants were also middle-aged at the time of diagnosis (i.e., <65 years) and had fewer co-morbid conditions than would be expected in a random sample of men diagnosed with prostate cancer given that the median age at diagnosis is 68 years according to SEER data. Thus, the men in our sample had longer life expectancies and provided an optimal opportunity to evaluate longer-term outcomes of prostate cancer patients.
Several mechanisms could explain an association of smoking with poor prostate cancer outcomes. It is possible that the phenotype of prostate cancer that develops in a smoker is more aggressive than in a non-smoker. In this case, smoking cessation after diagnosis may not affect long-term outcome. Smoking also produces reactive oxygen species, which can increase oxidative stress and promote the accumulation of somatic mutations in cancer cells [22–25], and it induces a generalized inflammatory response, which could contribute to tumor proliferation [26]. In both of these scenarios, smoking cessation after diagnosis could reduce tumor aggressiveness. Smoking may also affect prostate cancer progression through its effects on sex hormones concentrations. Cigarette smoking in men is associated with higher levels of total and free testosterone, dihydrotestosterone, and sex hormone-binding globulin [27, 28] and lower levels of estradiol [29]. Lastly, smoking may influence prostate cancer outcomes through suppression of immune response [30, 31]. The long latency of prostate cancer before diagnosis combined with our finding that men who smoked at the time of diagnosis were much more likely to have poor outcomes than men who had recently quit before diagnosis suggest that smoking promotes the acquisition of aggressive tumor characteristics and that cessation could indeed benefit prostate cancer patients’ survival.
This study has several strengths. First, we evaluated outcomes in a population-based sample regardless of treatment or cancer stage. Second, we had a long duration of follow-up (median duration: 11.5 years) for a total of 752 prostate cancer patients. Finally, cause of death was obtained from the SEER cancer registry as coded by the Washington State nosologist and was verified by reviewing copies of death certificates, which should limit bias due to other causes of smoking-related death. There are also several limitations of this study. First, the small number of African-Americans limits our ability to examine the effect of smoking in this subgroup that has a higher risk of prostate cancer mortality. Second, we have no information about smoking cessation after diagnosis. However, this is likely a conservative bias if smoking cessation decreases the risk of prostate cancer death. Finally, in stratified analyses, the number of deaths in each stratum was small, limiting the power to test whether associations of smoking differed by clinical prognostic factors.
Our findings suggest that smoking at the time of diagnosis is associated with a substantial increase in the risk of prostate cancer-specific death, which may explain why smoking is consistently associated with an increase in risk of prostate cancer mortality, but not in incidence. Men who had quit within 10 years of diagnosis may also have a modestly increased risk of prostate cancer-specific death. We cannot address directly whether smoking cessation after diagnosis would improve long-term cancer outcomes. Nevertheless, the much stronger association in current smokers compared to recent quitters at the time of diagnosis suggests that tobacco exposure may promote the acquisition of more aggressive tumor phenotypes, and that cessation could slow such progression after treatment. We believe it prudent to advise smokers who are diagnosed with prostate cancer to stop smoking as a means to reduce their likelihood of death due to prostate cancer.
References
Hickey K, Do KA, Green A (2001) Smoking and prostate cancer. Epidemiol Rev 23:115–125
Hsing AW, McLaughlin JK, Schuman LM et al (1990) Diet, tobacco use, and fatal prostate cancer: results from the Lutheran Brotherhood Cohort Study. Cancer Res 50:6836–6840
Rodriguez C, Tatham LM, Thun MJ, Calle EE, Heath CW (1997) Smoking and fatal prostate cancer in a large cohort of adult men. Am J Epidemiol 145:466–475
Coughlin SS, Neaton JD, Sengupta A (1996) Cigarette smoking as a predictor of death from prostate cancer in 348,874 men screened for the multiple risk factor intervention trial. Am J Epidemiol 143:1002–1006
Giovannucci E, Rimm EB, Ascherio A et al (1999) Smoking and risk of total and fatal prostate cancer in United States health professionals. Cancer Epidemiol Biomarkers Prev 8:277–282
Eichholzer M, Stahelin HB, Ludin E, Bernasconi F (1999) Smoking, plasma vitamins C, E, retinol, and carotene, and fatal prostate cancer: seventeen-year follow-up of the prospective basel study. Prostate 38:189–198
Giovannucci E, Liu Y, Platz EA, Stampfer MJ, Willett WC (2007) Risk factors for prostate cancer incidence and progression in the health professionals follow-up study. Int J Cancer 121:1571–1578
Hsing AW, McLaughlin JK, Hrubec Z, Blot WJ, Fraumeni JF (1991) Tobacco use and prostate cancer: 26-year follow-up of US veterans. Am J Epidemiol 133:437–441
Cerhan JR, Torner JC, Lynch CF et al (1997) Association of smoking, body mass, and physical activity with risk of prostate cancer in the Iowa 65+ Rural Health Study (United States). Cancer Causes Control 8:229–238
Plaskon LA, Penson DF, Vaughan TL, Stanford JL (2003) Cigarette smoking and risk of prostate cancer in middle-aged men. Cancer Epidemiol Biomarkers Prev 12:604–609
Pickles T, Liu M, Berthelet E, Kim-Sing C, Kwan W, Tyldesley S (2004) The effect of smoking on outcome following external radiation for localized prostate cancer. J Urol 171:1543–1546
Pantarotto J, Malone S, Dahrouge S, Gallant V, Eapen L (2007) Smoking is associated with worse outcomes in patients with prostate cancer treated by radical radiotherapy. BJU Int 99:564–569
Oefelein MG, Resnick MI (2004) Association of tobacco use with hormone refractory disease and survival of patients with prostate cancer. J Urol 71:2281–2284
Yu GP, Ostroff JS, Zhang ZF, Tang J, Schantz SP (1997) Smoking history and cancer patient survival: a hospital cancer registry study. Cancer Detect Prev 21:497–509
Daniell HW (1995) A worse prognosis for smokers with prostate cancer. J Urol 154:153–157
Jager T, Eisenhardt A, Rubben H, Lummen G (2007) Does cigarette smoking influence the survival of patients with prostate cancer? Urologe A 46:397–401
Stanford JL, Wicklund KG, McKnight B, Daling JR, Brawer MK (1999) Vasectomy and risk of prostate cancer. Cancer Epidemiol Biomarkers Prev 8:881–886
Gleason DF, Mellinger GT (1974) Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol 111:58–64
Stanford JL, Stephenson RA, Coyle LM et al (1999) Prostate cancer trends 1973–1995, SEER program NIH Publication. US Government Printing Office, Washington, DC
Cox DR (1972) Regression models with life-tables (with discussion). J Roy Statistic Soc: Series B 34:187–220
Breslow NE, Day NE (1980) Statistical methods in cancer research, vol 1 - The analysis of case–control studies. In: Davis W (ed) Intl Agency for Research on Cancer, Lyon
Hecht SS (2003) Tobacco carcinogens, their biomarkers and tobacco-induced cancer. Nat Rev Cancer 3:733–744
Pryor WA (1997) Cigarette smoke radicals and the role of free radicals in chemical carcinogenicity. Environ Health Perspect 105(Suppl 4):875–882
Kiyosawa H, Suko M, Okudaira H et al (1990) Cigarette smoking induces formation of 8-hydroxydeoxyguanosine, one of the oxidative DNA damages in human peripheral leukocytes. Free Radic Res Commun 11:23–27
Marnett LJ (2000) Oxyradicals and DNA damage. Carcinogenesis 21:361–370
Palapattu GS, Sutcliffe S, Bastian PJ et al (2005) Prostate carcinogenesis and inflammation: emerging insights. Carcinogenesis 26:1170–1181
Dai WS, Gutai JP, Kuller LH, Cauley JA (1988) Cigarette smoking and serum sex hormones in men. Am J Epidemiol 128:796–805
Field AE, Colditz GA, Willett WC, Longcope C, McKinlay JB (1994) The relation of smoking, age, relative weight, and dietary intake to serum adrenal steroids, sex hormones, and sex hormone-binding globulin in middle-aged men. J Clin Endocrinol Metab 79:1310–1316
Ferrini RL, Barrett-Connor E (1998) Sex hormones and age: a cross-sectional study of testosterone and estradiol and their bioavailable fractions in community-dwelling men. Am J Epidemiol 147:750–754
Holt PG, Keast D, Mackenzie JS (1978) Immunosuppression in the mouse induced by long-term exposure to cigarette smoke. Am J Pathol 90:281–284
Smoking and immunity. (Editorial 1993) Lancet 335:1561–1563
Acknowledgments
Supported by grants P50-CA97186, RO1-CA56678, and contract N01-CN-05230 from the National Cancer Institute, NIH, with additional support from the Fred Hutchinson Cancer Research Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gong, Z., Agalliu, I., Lin, D.W. et al. Cigarette smoking and prostate cancer-specific mortality following diagnosis in middle-aged men. Cancer Causes Control 19, 25–31 (2008). https://doi.org/10.1007/s10552-007-9066-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-007-9066-9