Abstract
Objective
A history of diabetes has been hypothesized to decrease prostate cancer risk, but studies have not always considered confounding or effect modification by dietary or lifestyle factors.
Methods
We examined the association between diabetes history and subsequent prostate cancer risk in 328,316 men enrolled in the NIH-AARP Diet and Health Study. Participants were ages 50–71 years and without a prostate cancer diagnosis at baseline in 1995. A prior history of physician-diagnosed diabetes was assessed using a self-administered mailed questionnaire. Cases of prostate cancer were ascertained by matching the cohort to state cancer registries. Multivariable relative risks (RR) and 95% confidence intervals (CI) of prostate cancer were estimated using Cox regression.
Results
During 5 years and 1,432,676 person-years of follow-up, 11,193 prostate cancer cases were ascertained. The age-adjusted and multivariable RRs of prostate cancer comparing men with diabetes to those without diabetes were 0.69 (95% CI = 0.64, 0.74) and 0.71 (95% CI = 0.66, 0.76), respectively, indicating no important confounding. The inverse association between diabetes and prostate cancer was particularly strong among men in the highest category of routine physical activity at work or home (RR = 0.41; 95% CI = 0.23, 0.74; p value for test of interaction = 0.03). Findings were similar for organ-confined and advanced prostate cancer.
Conclusion
Results from this large prospective study suggest that a history of diabetes is associated with a decreased risk of prostate cancer. The relationship strengthened with high levels of routine physical activity. Because increased physical activity is associated with lower circulating levels of insulin and testosterone, our findings support a role of hypoinsulinemia and low androgenicity linking diabetes to decreased prostate cancer risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a major health problem in the United States, affecting nearly 10% of the population [1]. The prevalence of diagnosed diabetes has increased substantially over the past decade [1], in parallel with increasing levels of adiposity [2], decreasing levels of physical activity [3], and aging of the population [4]. Diabetes rates are expected to continue an upward trajectory in the U.S. and globally in the years to come [5].
Diabetes has long been recognized as increasing the risk of several types of cancer [6]. In contrast, a growing epidemiologic literature suggests that diabetes protects against the development of prostate cancer [7]. The most salient biological mechanisms relate to decreased levels of insulin [8] and testosterone [9] among men with diabetes. With over 230,000 new cases each year, prostate cancer is the most commonly diagnosed cancer among U.S. men [10]. Despite its high incidence, the etiology of prostate cancer remains poorly understood [11]. Thus, any observed link between diabetes and prostate cancer provides an important opportunity to help clarify the biological mechanisms through which diabetes may decrease the risk of prostate cancer. Also, given the substantial incidence of both diabetes and prostate cancer, any factor that might modify the relationship between the two would have significant clinical and public health relevance.
The purpose of this study was to examine the association between diabetes and prostate cancer in a large cohort study with comprehensive data on diet, medical history, screening behaviors, and staging of prostate cancer outcomes. Our study differs from most previous investigations by exploring a multi-racial population with several thousand prostate cancer cases among white men and several hundred prostate cancer cases among black, Hispanic, and Asian men. A further aim was to investigate whether the relation of diabetes to prostate cancer risk varied by established or potential prostate cancer risk factors.
Materials and methods
Study population
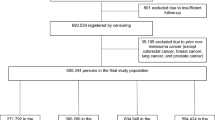
The National Institutes of Health (NIH)-AARP (formerly known as the American Association of Retired Persons) Diet and Health Study was established in 1995 when a baseline screening questionnaire that elicited information on medical history and lifestyle characteristics was mailed to 3.5 million AARP members [12]. Recipients were men and women who were ages 50–71 years and resided in one of six U.S. states (CA, FL, LA, NJ, NC, and PA) or two metropolitan areas (Atlanta, GA, and Detroit, MI) known to have high-quality cancer registries, adequate minority representation, and large AARP memberships. A total of 566,407 individuals (16.2%) completed the screening questionnaire satisfactorily. After excluding 226,736 women and 11,355 men reporting prevalent prostate cancer at baseline, the analytic cohort included 328,316 men.
Cohort follow-up
Cohort participants were followed up using two annual linkages. Change-of-address was ascertained by matching the cohort to the National Change of Address database maintained by the U.S. Postal Service, and updated through processing of undeliverable mail, other address change update services, and directly from participants’ notifications. Vital status was ascertained by linkage of the cohort to the Social Security Administration Death Master File in the U.S. Follow-up searches of presumed deaths in the National Death Index (NDI) Plus provided verification and cause of death information. Follow-up time extended from 25 October 1995 to 31 December 2000.
Case ascertainment
Incident cases of prostate cancer were identified by probabilistic linkage to eight state cancer registries. For matching purposes, we have virtually complete data on first and last name, address history, gender, and date of birth. Social Security number is available in whole or part for 85% of our cohort. All suspect matches underwent a review to reject potential matches that were unlikely to be true (approximately 4%), and uncertain matches underwent final manual review. We conducted a validation study comparing registry findings to self-reports and medical records and found that approximately 90% of all cancer cases in our cohort were validly identified using linkage to cancer registries [13]. The North American Association of Central Cancer Registries (NAACCR) certifies all eight cancer registries, which are estimated to be 95% complete for cancers reported up to two years prior [14]. Date and cause of death from linkage to the NDI also identified prostate cancer deaths. Staging procedures corresponded to the TNM stage of disease classification [15] and were based on clinical or clinical and surgical findings, and stage was assigned the highest reported value, based on clinical and prostatectomy results. Prostate cancers with stages T1–T2 and N0M0 were classified as organ-confined cancers. Cases with stages T3–T4 or N1 or M1, or those who died of prostate cancer were classified as advanced prostate cancers. Information on Gleason sum was not available. The Special Studies Institutional Review Board (IRB) of the U.S. National Cancer Institute approved this study. Completion of the self-administered baseline questionnaire was considered to imply informed consent.
Assessment of diabetes mellitus
On the baseline questionnaire, participants were requested to report whether they had ever been told by a doctor that they had any of nine listed medical conditions, one of which was diabetes. The questionnaire did not inquire about the time since the diagnosis of diabetes and it did not differentiate between type 1 and type 2 diabetes. Approximately 95% of all diabetes cases are type 2 [1]; for the purpose of our analysis, we considered a report of diabetes on the questionnaire to be type 2 diabetes.
Statistical analysis
Cox proportional hazard regression with age as the time scale was used to estimate the relative risks (RR) and corresponding 95% confidence intervals (CI) of prostate cancer. Tests of the proportional hazard assumptions for exposures and covariates included in our models indicated no departures. Follow-up began at the age at which the baseline questionnaire was received and scanned. Follow-up ended on the date of prostate cancer diagnosis (for incident prostate cancers), date of prostate cancer death (for fatal prostate cancers), death from any other cause, move out of the registry catchment areas, or the end of study in 31 December 2000, whichever occurred first. We ran separate Cox proportional hazards models for total, organ-confined, and advanced prostate cancers, and prostate cancer deaths. The prostate cancer subtype under study was censored at their date of diagnosis (or at the date of death, for prostate cancer deaths). For example, men with organ-confined prostate cancers were censored at their date of diagnosis and were not counted as cases in analyses involving advanced cancers. Likewise, men with advanced prostate cancers were censored at their date of diagnosis and were not counted as cases in analyses involving organ-confined cancers.
The multivariable model contained the following possible prostate cancer risk factors or factors that were associated with prostate cancer in our study: current age, body mass index at baseline, height, education, race, family history of prostate cancer, smoking status, vigorous physical activity, supplemental vitamin E use, supplemental zinc use, alcohol intake, and energy-adjusted intakes of red meat, alpha-linolenic acid, tomato products, fish, calcium, and vitamin D from diet and supplements. For each covariate, we used an indicator variable for a missing response, if required. In a sub-analysis among 195,812 men (59.6% of the total analytic cohort) who completed a supplementary questionnaire in 1996–1997 that sought more detailed information on cancer risk factors and cancer screening practices, we additionally adjusted for body mass index at age 18, history of prostate cancer screening using digital rectal examination (DRE), and history of screening for elevated prostate-specific antigen (PSA).
We lacked information on the diagnosis date of diabetes among men in our study, and therefore we were not able to directly examine duration of diabetes in relation to subsequent prostate cancer risk. However, we estimated risk associated with diabetes according to the number of years elapsed since baseline. We conducted stratified analyses to examine whether the diabetes and prostate cancer relationship was modified by other potential risk factors for prostate cancer. Tests for interaction were performed with the use of likelihood-ratio tests. All reported p values were based on two-sided tests. Statistical analyses were performed using Statistical Analysis Systems (SAS) release 8.2 (SAS Institute, Cary, NC).
Results
During 1,432,676 person-years of follow-up from 1995 through 2000, we ascertained 11,193 cases of prostate cancer, of which 9,582 were organ-confined, 1,611 were advanced, and 135 were prostate cancer deaths. Of the 11,193 prostate cancer cases identified, 10,244 (92%) were among white men. The mean durations (ranges) of follow-up in censored men and men who developed prostate cancer were 4.4 years (1 day to 5.2 years) and 2.4 years (1 day to 5.1 years), respectively. About 150 men were diagnosed with prostate cancer and 308 men were censored within one month of entry. The mean (SD) ages at study entry and exit were 62.2 (5.3) and 66.6 (5.3) years, respectively.
At baseline, a total of 34,029 men (10.4%) reported having been previously diagnosed with diabetes (Table 1). This is consistent with the prevalence of diabetes in the 1988–1994 U.S. National Health and Nutrition Survey for men 50–74 years of age (range, 9.6–11.8%) [16]. Men reporting a history of diabetes were more likely to describe themselves as black, Hispanic, or Asian and to be less educated, heavier, and more sedentary than men without a history of diabetes. In addition, men with a history of diabetes drank less alcohol but they consumed a diet higher in red meat than men without diabetes. Diabetic men also reported a slightly lower family history of prostate cancer than non-diabetic men.
In age-adjusted analysis, the RR relating history of diabetes to prostate cancer was 0.69 (95% CI = 0.64, 0.74) (Table 2). Further adjustment for baseline body mass index, height, education, race/ethnicity, family history of prostate cancer, and smoking status did not materially alter the association (RR = 0.70; 95% CI = 0.65, 0.75). Additional control for physical activity and dietary intakes of red meat, alcohol, alpha-linolenic acid, calcium, vitamin D from diet and supplements, fish, tomato products, supplemental vitamin E, and supplemental zinc also had virtually no effect on the relative risk estimate (RR = 0.71; 95% CI = 0.66, 0.76).
After we excluded the first year of follow-up, the multivariable risk estimate was essentially unchanged (RR = 0.70; 95% CI = 0.65, 0.76). Additional adjustment for body mass index at age 18 also had no impact (RR = 0.69; 95% CI = 0.63, 0.77). Further, the relation was not altered after subsequent control for history of DRE or history of screening for elevated PSA, individually (data not shown) or in combination (RR = 0.69; 95% CI = 0.63, 0.77).
When data were analyzed by tumor stage at prostate cancer diagnosis, the multivariable RR was 0.71 (95% CI = 0.65, 0.76) for organ-confined prostate tumors and 0.71 (95% CI = 0.59, 0.86) for advanced tumors (Table 2). The multivariable RR for prostate cancer death comparing men with diabetes to those without diabetes was 0.84 (95% CI = 0.48, 1.46). Diabetic men are less likely to be upstaged because they are less often treated with surgery because of concerns about comorbidity. To account for potential bias caused by this circumstance, we repeated our analyses of organ-confined and advanced prostate cancers after disregarding information on pathological staging and using clinical staging information only. Results were virtually unchanged (data not shown).
The relation of diabetes to prostate cancer risk strengthened with an increasing number of years since baseline (Table 3). The multivariable RR of prostate cancer for men with less than one year of follow-up was 0.72 (95% CI = 0.62, 0.84) and it was 0.62 (95% CI = 0.51, 0.76) for men who were followed-up for four or more years (p value for test of interaction = 0.0001).
We examined whether the effect of diabetes was modified by established or potential risk factors for prostate cancer (Table 4). The inverse relation between diabetes and prostate cancer was particularly strong among men in the highest category of routine physical activity at work or home (RR = 0.41; 95% CI = 0.23, 0.74; p value for test of interaction = 0.03). Also, the association of diabetes to prostate cancer appeared to be stronger among men in the highest category of vigorous physical activity (RR = 0.59; 95% CI = 0.49, 0.70), although the test for interaction was not statistically significant (p value = 0.12). Those findings were not materially altered after the first year of follow-up was excluded (data not shown). The inverse relation with diabetes was more pronounced among men with greater frequency of undergoing a DRE (p value for test of interaction = 0.002). Associations between diabetes and prostate cancer were largely similar across various subgroups of men defined by age, race/ethnicity, family history of prostate cancer, education level, current and adolescent body mass index, adult weight change, and waist circumference (all p values for test of interaction ≥0.14).
Discussion
In this large, prospective study, we observed a significant inverse association between history of diabetes and subsequent prostate cancer risk. The relation of diabetes to prostate cancer risk was stronger among physically active than inactive men. The association was not modified by age, race/ethnicity, family history of prostate cancer, education, current or adolescent body mass, adult weight gain, or waist circumference.
Early population studies on diabetes and prostate cancer reported mixed results [6, 17–29], none of which were statistically significant, which may have been due to limited statistical power [17, 18, 20, 22, 24–29], reverse causation [24, 28], or failure to account for potential confounding [17–24, 26, 27]. In 1991, Adami et al. [30] were the first to report a statistically significant 30% decreased risk of prostate cancer among men diagnosed with diabetes. Since then, ten prospective studies [31–40] and four case–control studies [41–44] have found a statistically significant [36–40, 42–44] or non-significant [31–35, 41] inverse association between impaired glucose tolerance or diabetes and prostate cancer. In contrast, two prospective studies [45, 46], three case–control studies [47–49], and one cross-sectional study [50] observed a positive relation between the two that was statistically non-significant, and one prospective [51] and one case–control study [52] noted a null association. A meta-analysis [7] that included 14 studies published up to 2002 reported that a history of diabetes is related to a weak reduction in the risk of prostate cancer (RR = 0.91; 95% CI = 0.86, 0.96). With over twice as many prostate cancer cases as in that first meta-analysis on the topic, a recent meta-analysis [53] of 19 relevant studies published up to 2005 concluded that diabetes history is associated with a modest decrease in prostate cancer risk (RR = 0.84; 95% CI = 0.76–0.93).
Our finding of an approximate 30% reduction in prostate cancer risk among diabetic men is strikingly consistent with several of the more recent cohort studies on this topic. The largest among these is the Cancer Prevention Study (CPS)-II, which included 5,318 cases and reported that men with diabetes had a 33% lower risk of prostate cancer than men without diabetes (RR = 0.67; 95% CI = 0.60, 0.75) [39]. A similar risk reduction was seen in the Health Professionals Follow-up Study (RR = 0.75; 95% CI = 0.59, 0.95) [36], the Physicians Health Study (RR = 0.64; 95% CI = 0.43, 0.95) [38], and a prospective study nested in the General Practitioners Research Database (RR = 0.72; 95% CI = 0.59, 0.87) [40].
In our study, the apparent protective influence of diabetes did not strengthen when we repeated our analyses using more advanced stages of prostate cancer or using prostate cancer deaths as alternative outcomes. The most likely explanation for the weak association between diabetes and prostate cancer death observed in our study is limited statistical power with n = 15 exposed cases of fatal prostate cancer. Alternatively, it is possible that while diabetes may prevent the initiation of prostate cancer, it will have little or no effect on the subsequent progression of prostate cancer. That notion is consistent with the observation that a history of diabetes is not related to presenting with high risk prostate cancer at diagnosis [54, 55], although several [36, 38, 39, 42], but not all [43, 46] studies have found the inverse relation with diabetes to be more pronounced for advanced than localized prostate cancer.
We lacked data on the diagnosis date of diabetes, but given the age range of men in our study (50–71 years) and the mean age at diagnosis of diabetes among U.S. adults (46.7 years) [56], it is likely that the majority of participants reporting a history of diabetes were diagnosed more than 10 years prior to study baseline. Our finding of a suggestively stronger diabetes and prostate cancer association with an increasing number of years elapsed since study baseline is consistent with most of the few studies [36–39, 48] that reported an inverse association between time since diabetes diagnosis and prostate cancer. Alternatively, increased medical surveillance upon diagnosis of diabetes may have resulted in prostate cancers being diagnosed earlier, thereby spuriously decreasing prostate cancer risk during the later years of follow-up in our study. In contrast to our and other investigations [36–39, 48], one study [46] noted a positive relation between duration of diabetes and prostate cancer risk, but that finding was based on 22 cases of prostate cancer and there was no evidence of a clear dose-response relationship.
We specifically addressed the relation of diabetes to prostate cancer among non-white men because minority groups in the U.S. are particularly affected by diabetes [1] and black men show disproportionately high rates of prostate cancer [10]. We found an inverse association between diabetes and prostate cancer risk among black, Hispanic, and Asian men, although the risk estimates were not statistically significant due to small numbers of cases. Alternative sources of available data regarding the relation of diabetes to prostate cancer among non-white men are limited to three case–control studies [26, 42, 43]. One of these studies [43] included 171 cases among black men and reported a strong inverse association between diabetes and prostate cancer (odds ratio (OR) = 0.36; 95% CI = 0.21, 0.62). In contrast, another U.S. study [42] found a positive relation of diabetes to prostate cancer among black men based on 17 cases (OR = 3.16; 95% CI = 0.67, 15.0). That study [42] also examined men of Hispanic ethnicity and found an inverse relation of diabetes to prostate cancer but the analysis involved only two cases. The only available data on Asian men comes from an older study from Japan [26] which reported a statistically non-significant, slight increase in risk of prostate cancer among men with diabetes (OR = 1.17; 95% CI was not provided).
We considered whether the inverse association between diabetes and prostate cancer was due to a bias against being diagnosed with prostate cancer among diabetic men. In our study, men with and without diabetes were similarly likely to have undergone a recent DRE or PSA test, which argues counter to the presence of such a bias. Other studies have shown that diabetic men do not have lower PSA levels [54, 57] or a lower prostate volume [57] than non-diabetic men, circumstances that could delay or prevent a diagnosis of prostate cancer among diabetic men. Because we did not collect information on PSA values, we cannot rule out that lower PSA levels in diabetic men caused a delay in the detection of prostate cancer compared to men without diabetes during the relatively short period of follow-up (five years) in our study. In contrast, heightened medical surveillance of individuals diagnosed with diabetes is also a possibility but cannot explain our findings because such detection bias would result in spuriously increased (as opposed to decreased) prostate cancer diagnoses among diabetics. When we addressed in more detail possible diagnostic bias by stratifying our sample according to prostate cancer screening history, we noted a strong inverse association between diabetes and prostate cancer among men with a recent DRE, which further makes detection bias unlikely. Divergently, an association between diabetes and prostate cancer was not evident among men without a recent DRE, possibly because men with infrequent visits to a doctor are less likely to receive prostate cancer screening examinations, a diagnosis of diabetes, or a diagnosis of prostate cancer than men who see their doctor regularly. A similar, but much weaker pattern was observed when we stratified our sample according to history of screening for elevated PSA.
Although our study lacked data on the type of diabetes, nearly 95% of diabetes cases are type 2 [1], which implies that the inverse association between diabetes and prostate cancer risk observed in our study essentially pertains to type 2 diabetes. Our approach of ascertaining diabetes on the basis of self-reported positive history alone bears the potential for misclassifying diabetes status, but such non-differential misclassification would underestimate the apparent protective effect of diabetes on prostate cancer risk. In addition, the validity of self-report for diabetes has shown excellent agreement (97.2%) with medical records [58].
We could not investigate whether a man’s diabetes was managed by diet and physical activity, factors that have been associated with a reduced risk of prostate cancer [59]. However, adjustment for a wide range of dietary and lifestyle factors had virtually no impact on our risk estimates, suggesting that confounding by a healthy lifestyle among men diagnosed with diabetes is unlikely to explain our results. We were unable to discern whether the lower risk of prostate cancer among diabetics was due to medication taken to treat diabetes rather than a mechanism related to diabetes itself. Data on the influence of antidiabetics on prostate cancer are limited to two studies [40, 42], both of which reported a decreased risk of prostate cancer among diabetics who were prescribed either insulin or sulphonylureas. The intriguing findings from those two studies [40, 42] require confirmation.
Although our data strongly suggest that men with type 2 diabetes are at significantly decreased risk of developing prostate cancer than men without diabetes, the underlying biological mechanisms remain speculative. The inverse association between diabetes and prostate cancer indicates that metabolic or hormonal perturbations concurrent with diabetes progression lower the risk of prostate cancer. Early forms of type 2 diabetes are accompanied by hyperinsulinemia, which is related to decreased levels of insulin-like growth factor binding protein (IGFBP-3) and sex-hormone binding globulin (SHBG), and consequently increased levels of circulating IGF-1 and testosterone [8]. In contrast, as diabetes advances to hypoinsulinemic stages, IGFBP-3 and SHBG levels increase, and IGF-1 and testosterone levels decrease [8]. In addition to low circulating levels of IGF-1 and testosterone levels among individuals with long-standing diabetes, a direct deleterious effect of hyperglycemia on testicular Leydig cell function and testosterone production [9] may also contribute to the apparent protective effect of diabetes on prostate cancer risk.
In support of a role of hypoinsulinemia and low androgenicity, we found a stronger inverse relation of diabetes to prostate cancer risk in physically active than inactive men. Although this may represent a chance finding, physical activity lowers circulating levels of insulin independently of body mass [60] and it lowers bioavailable testosterone levels [61]. Our finding of a stronger inverse relation between diabetes and incident prostate cancer than prostate cancer deaths suggests that among men who developed fatal prostate cancer, the apparent protective effect of low insulin levels was partially offset by the adverse effect of low testosterone levels on prostate tumor differentiation. Heightened androgenic stimulation has been hypothesized to prevent the dedifferentiation of the prostate epithelium, whereas a low testosterone milieu may promote the development of a hormonally insensitive, less differentiated and ultimately fatal prostate cancer [62, 63].
The principle implications of our study are in clarifying whether our findings are applicable to other populations and improving our knowledge of the biological mechanisms through which diabetes influences the risk of prostate cancer. Refining our understanding of diabetes and prostate cancer may enable us to identify certain groups of men at high risk for prostate cancer that may be targeted for increased screening frequency or early pharmacological or lifestyle interventions. The clinical or public health implications of our study are less obvious; despite the possibility of a protective effect of diabetes on prostate cancer risk, impaired glucose tolerance has overwhelmingly adverse effects on general health status. Thus, future studies should continue to replicate these findings, including in non-white populations. In addition, the biological pathways through which diabetes may ameliorate prostate carcinogenesis warrant further investigation.
References
Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM, Saydah SH, Williams DE, Geiss LS, Gregg EW (2006) Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care 29:1263–1268
Flegal KM, Carroll MD, Ogden CL, Johnson CL (2002) Prevalence and trends in obesity among US adults, 1999–2000. Jama 288:1723–1727
CDC (2005) Trends in leisure-time physical inactivity by age, sex, and race/ethnicity–United States, 1994–2004. MMWR Morb Mortal Wkly Rep 54:991–994
U.S. Census Bureau, Population Division (2006) Age Data. Available at: http://www.census.gov/population/www/socdemo/age.html. Accessed June 30 2006
Yach D, Stuckler D, Brownell KD (2006) Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med 12:62–66
O’Mara BA, Byers T, Schoenfeld E (1985) Diabetes mellitus and cancer risk: a multisite case-control study. J Chronic Dis 38:435–441
Bonovas S, Filioussi K, Tsantes A (2004) Diabetes mellitus and risk of prostate cancer: a meta-analysis. Diabetologia 47:1071–1078
Giovannucci E (2003) Nutrition, insulin, insulin-like growth factors and cancer. Horm Metab Res 35:694–704
Pitteloud N, Hardin M, Dwyer AA, Valassi E, Yialamas M, Elahi D, Hayes FJ (2005) Increasing insulin resistance is associated with a decrease in Leydig cell testosterone secretion in men. J Clin Endocrinol Metab 90:2636–2641
American Cancer Society (2005) Cancer facts and figures 2005. American Cancer Society, Atlanta
Gronberg H (2003) Prostate cancer epidemiology. Lancet 361:859–864
Schatzkin A, Subar AF, Thompson FE, Harlan LC, Tangrea J, Hollenbeck AR, Hurwitz PE, Coyle L, Schussler N, Michaud DS, Freedman LS, Brown CC, Midthune D, Kipnis V (2001) Design and serendipity in establishing a large cohort with wide dietary intake distributions : the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol 154:1119–1125
Michaud DS, Midthune D, Hermansen S, Leitzmann MF, Harlan L, Kipnis V, Schatzkin A (2005) Comparison of cancer registry case ascertainment with SEER estimates and self-reporting in a subset of the NIH-AARP Diet and Health Study. J Registry Manage 32:70–75
NAACR (2002) Standards for completeness, quality, analysis, and management of data, vol. 3. North American Association of Central Disease Registries
AJCC (1997) Cancer staging manual. Lippincott-Raven, Philadelphia, PA
Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, Wiedmeyer HM, Byrd-Holt DD (1998) Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988–1994. Diabetes Care 21:518–524
Wilson EB, Maher HC (1932) Cancer and tuberculosis with some comments on cancer and other diseases. Am J Cancer 16:227–250
Glicksman AS, Rawson RW (1956) Diabetes and altered carbohydrate metabolism in patients with cancer. Cancer 9:1127–1134
Bell ET (1957) Carcinoma of the pancreas. I. A clinical and pathologic study of 600 necropsied patients. II. The relation of carcinoma of pancreas to diabetes mellitus. Am J Pathol 33:499–523
Lancaster HO, Maddox JK (1958) Diabetic mortality in Australia. Australias Ann Med 7:145–150
Steele JM, Sperling WL (1961) Relationship between diabetes mellitus and cancer. A study of the records for eight years at the Robert Packer Hospital. Guthrie Clin Bull 30:63–67
Kessler II (1970) Cancer mortality among diabetics. J Nat Cancer Inst 44:673–686
Wynder EL, Mabuchi K, Whitmore WF, Jr (1971) Epidemiology of cancer of the prostate. Cancer 28:344–360
Henderson BE, Bogdanoff E, Gerkins VR, SooHoo J, Arthur M (1974) Evaluation of cancer risk factors in a retirement community. Cancer Research 34:1045–1048
Ragozzino M, Melton LJ 3rd, Chu CP, Palumbo PJ (1982) Subsequent cancer risk in the incidence cohort of Rochester, Minnesota, residents with diabetes mellitus. J Chronic Dis 35:13–19
Mishina T, Watanabe H, Araki H, Nakao M (1985) Epidemiological study of prostatic cancer by matched-pair analysis. Prostate 6:423–436
Checkoway H, DiFerdinando G, Hulka BS, Mickey DD (1987) Medical, life-style, and occupational risk factors for prostate cancer. Prostate 10:79–88
Thompson MM, Garland C, Barrett-Connor E, Khaw KT, Friedlander NJ, Wingard DL (1989) Heart disease risk factors, diabetes, and prostatic cancer in an adult community. Am J Epidemiol 129:511–517
Levine W, Dyer AR, Shekelle RB, Schoenberger JA, Stamler J (1990) Post-load plasma glucose and cancer mortality in middle-aged men and women. 12-year follow-up findings of the Chicago Heart Association Detection Project in Industry. Am J Epidemiol 131:254–262
Adami HO, McLaughlin J, Ekbom A, Berne C, Silverman D, Hacker D, Persson I (1991) Cancer risk in patients with diabetes mellitus. Cancer Causes Control 2:307–314
Smith GD, Egger M, Shipley MJ, Marmot MG (1992) Post-challenge glucose concentration, impaired glucose tolerance, diabetes, and cancer mortality in men. Am J Epidemiol 136:1110–1114
Coughlin SS, Neaton JD, Sengupta A (1996) Cigarette smoking as a predictor of death from prostate cancer in 348,874 men screened for the Multiple Risk Factor Intervention Trial. Am J Epidemiol 143:1002–1006
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ (2004) Diabetes Mellitus as a Predictor of Cancer Mortality in a Large Cohort of US Adults. Am J Epidemiol 159:1160–1167
Wideroff L, Gridley G, Mellemkjaer L, Chow WH, Linet M, Keehn S, Borch-Johnsen K, Olsen JH (1997) Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst 89:1360–1365
Hjalgrim H, Frisch M, Ekbom A, Kyvik KO, Melbye M, Green A (1997) Cancer and diabetes–a follow-up study of two population-based cohorts of diabetic patients. J Intern Med 241:471–475
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Willett WC (1998) Diabetes mellitus and risk of prostate cancer (United States). Cancer Causes & Control 9:3–9
Weiderpass E, Ye W, Vainio H, Kaaks R, Adami HO (2002) Reduced risk of prostate cancer among patients with diabetes mellitus. Int J Cancer 102:258–261
Zhu K, Lee IM, Sesso HD, Buring JE, Levine RS, Gaziano JM (2004) History of diabetes mellitus and risk of prostate cancer in physicians. Am J Epidemiol 159:978–982
Rodriguez C, Patel AV, Mondul AM, Jacobs EJ, Thun MJ, Calle EE (2005) Diabetes and risk of prostate cancer in a prospective cohort of US men. Am J Epidemiol 161:147–152
Gonzalez-Perez A, Garcia Rodriguez LA (2005) Prostate cancer risk among men with diabetes mellitus (Spain). Cancer Causes Control 16:1055–1058
La Vecchia C, Negri E, Franceschi S, D’Avanzo B, Boyle P (1994) A case-control study of diabetes mellitus and cancer risk. Br J Cancer 70:950–953
Rosenberg DJ, Neugut AI, Ahsan H, Shea S (2002) Diabetes mellitus and the risk of prostate cancer. Cancer Invest 20:157–165
Coker AL, Sanderson M, Zheng W, Fadden MK (2004) Diabetes mellitus and prostate cancer risk among older men: population-based case-control study. Br J Cancer 90:2171–2175
Lightfoot N, Conlon M, Kreiger N, Sass-Kortsak A, Purdham J, Darlington G (2004) Medical history, sexual, and maturational factors and prostate cancer risk. Ann Epidemiol 14:655–662
Steenland K, Nowlin S, Palu S (1995) Cancer incidence in the National Health and Nutrition Survey I. Follow-up data: diabetes, cholesterol, pulse and physical activity. Cancer Epidemiol Biomarkers Prev 4:807–811
Will JC, Vinicor F, Calle EE (1999) Is diabetes mellitus associated with prostate cancer incidence and survival? Epidemiology 10:313–318
Hsieh CC, Thanos A, Mitropoulos D, Deliveliotis C, Mantzoros CS, Trichopoulos D (1999) Risk factors for prostate cancer: a case-control study in Greece. Int J Cancer 80:699–703
Tavani A, Gallus S, Bosetti C, Tzonou A, Lagiou P, Negri E, Trichopoulos D, La Vecchia C (2002) Diabetes and the risk of prostate cancer. Eur J Cancer Prev 11:125–128
Rousseau MC, Parent ME, Pollak MN, Siemiatycki J (2006) Diabetes mellitus and cancer risk in a population-based case-control study among men from Montreal, Canada. Int J Cancer 118:2105–2109
Hammarsten J, Hogstedt B (2004) Clinical, haemodynamic, anthropometric, metabolic and insulin profile of men with high-stage and high-grade clinical prostate cancer. Blood Press 13:47–55
Batty GD, Shipley MJ, Marmot M, Smith GD (2004) Diabetes status and post-load plasma glucose concentration in relation to site-specific cancer mortality: findings from the original Whitehall study. Cancer Causes Control 15:873–881
Tavani A, Gallus S, Bertuzzi M, Dal Maso L, Zucchetto A, Negri E, Franceschi S, Ramazzotti V, Montella M, La Vecchia C (2005) Diabetes mellitus and the risk of prostate cancer in Italy. Eur Urol 47:313–317; discussion 317
Kasper JS, Giovannucci E (2006) A Meta-analysis of Diabetes Mellitus and the Risk of Prostate Cancer. Cancer Epidemiol Biomarkers Prev 15:2056–2062
Chan JM, Latini DM, Cowan J, Duchane J, Carroll PR (2005) History of diabetes, clinical features of prostate cancer, and prostate cancer recurrence-data from CaPSURE (United States). Cancer Causes Control 16:789–797
Kane CJ, Bassett WW, Sadetsky N, Silva S, Wallace K, Pasta DJ, Cooperberg MR, Chan JM, Carroll PR (2005) Obesity and prostate cancer clinical risk factors at presentation: data from CaPSURE. J Urol 173:732–736
Centers for Disease Control and Prevention (2006), National Diabetes Surveillance Program Age at Diagnosis Among Adults Aged 18–70 Years. Available at: http://www.cdc.gov/diabetes/statistics/age. Accessed June 30 2006
Burke JP, Jacobson DJ, McGree ME, Roberts RO, Girman CJ, Lieber MM, Jacobsen SJ (2006) Diabetes and benign prostatic hyperplasia progression in Olmsted County, Minnesota. Urology 67:22–25
Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ (2004) Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 57:1096–1103
Hsing AW, Chokkalingam AP (2006) Prostate cancer epidemiology. Front Biosci 11:1388–1413
Regensteiner JG, Shetterly SM, Mayer EJ, Eckel RH, Haskell WL, Baxter J, Hamman RF (1995) Relationship between habitual physical activity and insulin area among individuals with impaired glucose tolerance. The San Luis Valley Diabetes Study. Diabetes Care 18:490–497
Daly W, Seegers CA, Rubin DA, Dobridge JD, Hackney AC (2005) Relationship between stress hormones and testosterone with prolonged endurance exercise. Eur J Appl Physiol 93:375–380
Hoffman MA, DeWolf WC, Morgentaler A (2000) Is low serum free testosterone a marker for high grade prostate cancer? J Urol 163:824–827
Platz EA, Leitzmann MF, Rifai N, Kantoff PW, Chen YC, Stampfer MJ, Willett WC, Giovannucci E (2005) Sex steroid hormones and the androgen receptor gene CAG repeat and subsequent risk of prostate cancer in the prostate-specific antigen era. Cancer Epidemiol Biomarkers Prev 14:1262–1269
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, National Cancer Institute. We are indebted to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation. We thank Leslie Carroll at Information Management Services for data support and Tawanda Roy at the Nutritional Epidemiology Branch for research assistance. Cancer incidence data from the Atlanta metropolitan area were collected by the Georgia Center for Cancer Statistics, Department of Epidemiology, Rollins School of Public Health, Emory University. Cancer incidence data from California were collected by the California Department of Health Services, Cancer Surveillance Section. Cancer incidence data from the Detroit metropolitan area were collected by the Michigan Cancer Surveillance Program, Community Health Administration, State of Michigan. The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System under contract to the Department of Health (DOH). The views expressed herein are solely those of the authors and do not necessarily reflect those of the contractor or DOH. Cancer incidence data from Louisiana were collected by the Louisiana Tumor Registry, Louisiana State University Medical Center in New Orleans. Cancer incidence data from New Jersey were collected by the New Jersey State Cancer Registry, Cancer Epidemiology Services, New Jersey State Department of Health and Senior Services. Cancer incidence data from North Carolina were collected by the North Carolina Central Cancer Registry. Cancer incidence data from Pennsylvania were supplied by the Division of Health Statistics and Research, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calton, B.A., Chang, S.C., Wright, M.E. et al. History of diabetes mellitus and subsequent prostate cancer risk in the NIH-AARP Diet and Health Study. Cancer Causes Control 18, 493–503 (2007). https://doi.org/10.1007/s10552-007-0126-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-007-0126-y