Abstract
Objective
To examine the relationship between obesity and mammography use in a large population of black and white women.
Methods
Baseline data from 18,756 black and 6,304 white women enrolled in the Southern Community Cohort Study were used to examine the association between body mass index categories (healthy weight: 18.5–24.9 kg/m2, overweight: 25–29.9 kg/m2, and obesity classes I: 30–34.9 kg/m2, II: 35–39.9 kg/m2, and III: 40+ kg/m2) and mammogram use in the past two years. Cross-sectional analyses were conducted using logistic regression controlling for socioeconomic measures, medical conditions, insurance coverage, and lifestyle factors.
Results
Among white women, obesity class III was associated with a reduced likelihood of recent mammography compared to healthy weight women (OR = 0.70, 95% CI 0.56–0.87) that appeared unrelated to income and insurance coverage. A deterring effect of obesity was not evident among black women; instead, overweight and obesity were associated with small elevations in mammography use compared to healthy weight.
Conclusions
In light of rising obesity rates and known associations between obesity and breast cancer risk and prognosis, a deterring effect of extreme obesity on mammography screening for white women is a concern that should be addressed by screening programs and by further directed research into the factors underlying this association.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer accounts for nearly one in three female cancer diagnoses in the United States, and approximately 213,000 new cases of invasive breast cancer are expected in 2006 [1]. Screening mammography has been shown to be effective in reducing breast cancer mortality [2] and, despite recent controvery [3], the United States Preventive Services Task Force and other health organizations currently recommend screening at intervals of 1–2 years for all women over the age of 40 who are at average risk for breast cancer [4].
Obese women are reported to be less likely than non-obese women to receive screening mammography [5–8]. The reasons for this discrepancy are not well-understood, but factors such as physician bias, negative self-perception and poor body image, and higher illness burden among obese women have all been suggested [6, 7]. There is strong variation in the prevalence of obesity by race in the United States. According to the 1999–2002 National Health and Nutrition Examination Survey (NHANES), 30% of white women versus 50% of black women were classified as obese [9]. Further, recent results from the National Health Interview Survey (NHIS) suggest that obese white women are less likely to receive screening mammography but that this pattern does not hold for black women; however, these analyses included relatively small numbers of black women compared to white women [6, 7]. Therefore, in order to improve screening behavior rates among obese women, we must first understand the interaction between race and obesity in relation to mammography use.
The goal of the current analysis was to examine the association between body size and mammography use, and to evaluate the potentially modifying effect of race on this relationship, among women enrolled in the Southern Community Cohort Study which includes a large sample of both black and white women of generally similar socioeconomic status in the age range appropriate for mammography screening.
Materials and methods
Study population
The SCCS is a prospective epidemiologic cohort study with ongoing participant enrollment across the southeastern U.S., the aim of which is to investigate racial disparities in cancer occurrence [10]. The study was approved by the institutional review boards at Vanderbilt University and Meharry Medical College. To date, participants have been enrolled in-person at 48 community health centers (CHCs) in urban and rural areas across the states of Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia. CHCs are government-funded health care facilities that provide basic health services primarily to low-income individuals [11]. They typically do not provide mammography services. Participants were enrolled by randomly approaching people entering the CHCs (patients, persons accompanying patients, etc.) who appeared to be age 40–79 and screening them for eligibility and interest in study participation. In addition to the age criteria, participants were required to be English-speaking and not to have undergone treatment for cancer within the past year. For the present cross-sectional analysis of baseline data, we identified all female cohort members enrolled since the beginning of the study (March 2002) through June 2006 (n = 30,760).
Data collection
Trained interviewers conducted comprehensive, in-person, baseline interviews with all participants that covered various aspects of health and behavior, including body size, personal and family medical history, reproductive history, diet, physical activity, tobacco use, health care utilization, and demographic characteristics. This interview was conducted at the CHC at the time of study enrollment. During the interview, participants were asked: “Have you ever had a mammogram?” Participants responding “yes” were also asked “When was your last mammogram?” A standard definition of the term mammogram was provided when necessary. From these data we determined whether women had a mammogram within the past two years (i.e., ≤2 years ago), in line with standard screening mammography recommendations [4] and consistent with the metric used by previous studies examining obesity and recent mammogram use [5–8].
Current weight and height were self-reported by participants. We calculated current body mass index (BMI) as weight in kilograms divided by the square of height in meters. We categorized BMI using nationally defined cutpoints [12]. Women with a BMI between 18.5 and 24.9 kg/m2 (considered healthy weight) were used as the referent group in our analyses. Overweight and obesity were defined as overweight (BMI 25.0–29.9 kg/m2), obesity class I (BMI 30.0–34.9 kg/m2), obesity class II (BMI 35.0–39.9 kg/m2) and obesity class III or extreme obesity (BMI ≥ 40 kg/m2) [12].
Statistical analysis
We excluded from the study population 1,278 (4.2%) women who identified their racial/ethnic background as something other than only Black/African-American or only Caucasian/White, 515 (1.7%) women who reported a prior diagnosis of breast cancer, 3,100 (10.1%) women who were less than 42 years of age because our metric of having a mammogram within the past two years would put them outside of the bottom age range (40 years) for mammography screening recommendations [4], 329 (1.1%) women whose BMI was less than 18.5 kg/m2, and 478 (1.6%) women who were missing information about mammography use, height or weight, leaving a total of 25,060 participants (18,756 black, 6,304 white) to serve as our study population.
Logistic regression was used to measure the association (presented as odds ratios (OR) with 95% confidence intervals (95% CI)) between the categories of BMI and mammography use within the past two years (yes/no) [13]. Race was considered to be a potential effect modifier. The likelihood ratio test (LRT) was used to compare models with all women (black and white) with and without an interaction term between race and BMI category. Based on the LRT p-value (with a cut-off set a priori as <0.10), the data for black and white women were analyzed separately.
Several factors reported in the baseline interview were considered a priori to be possible confounders of the relation between BMI and mammography use, including age, measures of socioeconomic status and access to health care (i.e., income, education, health insurance coverage), parity, cigarette smoking status, a history of obesity-related conditions that could lead to more frequent contact with the health care system (i.e., diabetes, hypertension, high cholesterol, heartburn/acid reflux, heart disease, and arthritis), time since last physician visit (as a proxy of the frequency of contact with health care providers), and family history of breast cancer. These formed the core group of adjustment factors and were included in the regression models using the categories shown in Table 1. Other variables evaluated as potential confounders (using a >10% change-in-estimate criterion) but found not to make an appreciable change in the results were marital status, the number of breast self-examinations performed within the past year, geographic population density (determined from the 2000 U.S. Census for the census tract of the CHC where the participant was enrolled) as a possible surrogate for access or proximity to facilities offering mammography, and depressive symptom score (based on the short version of the Center for Epidemiologic Studies Depression Scale) [14]. None of these variables were included in the models presented here.
Results
White women were slightly more likely than black women to have reported ever having had a mammogram (87.4 vs. 85.0%), whereas black women were slightly more likely than white women to report having had a mammogram within the past two years (73.0 vs. 68.7%). Despite the slightly older age distribution of the white women (Table 1), both of these racial differences in mammography use remained statistically significant after age adjustment (data not shown). Due to the study design involving participant enrollment at CHCs, the majority (61%) of the study population had a total household income of less than $15,000 per year, a substantial proportion (40%) reported having no health insurance, and 32% had less than a high school education. The distributions of these sociodemographic indicators were similar by race. Obesity (BMI ≥ 30 kg/m2) was more prevalent among the black women (58%) than the white women (49%).
Table 1 also shows the percentage of women receiving a mammogram in the past two years for each stratum of the a priori set of confounders. As expected, the percentage of women who underwent mammography within the past two years generally increased with increasing age and household income, and was positively related to having a college education. Women without any health insurance were less likely to have had a recent mammogram compared to women with some form of coverage (62 vs. 78%), and current smokers were less likely to report a recent mammogram (62%) than former and never smokers (77%). Black and white women with a history of chronic medical conditions (i.e., diabetes, hypertension, high cholesterol, heartburn/acid reflux, heart disease, and arthritis) were, overall, more likely to report having a recent mammogram than women without these conditions.
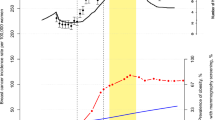
For both black and white women, the crude percentage of women reporting a mammogram within the past two years increased with increasing BMI up to 35 kg/m2 and then leveled off and decreased (Table 1), but the relationship between BMI and mammography use significantly differed by race (LRT p < 0.0001). In particular, the increase in mammography use associated with rising BMI was more pronounced among black women, and for white women the drop off in mammography use associated with a BMI ≥ 40 kg/m2 was more pronounced. After multivariate adjustment, black women at every level of overweight and obesity were more likely to have had a mammogram in the past two years than black women of healthy weight (Table 2 and Fig. 1a). Among white women, multivariate adjustment eliminated the crude positive association between BMI and mammography use, and there was a marked decrease in the likelihood of having had a mammogram within the past two years among women with a BMI ≥ 40 kg/m2 [OR = 0.70, 95% CI 0.56–0.87] (Table 2 and Fig. 1b). The changes in the BMI estimates in Table 2 between the crude and adjusted-ORs were driven largely by personal health and health-care related confounders including smoking status, time since last physician visit, co-morbidities, and type of health insurance. For comparison purposes, in Fig. 1a and b, adjusted ORs from the present analysis are plotted alongside those from previous studies that examined the relationship between BMI and mammography use in the past two years separately for black and white women [6, 7, 15]. Since the relationship between obesity and breast cancer differs between pre and post-menopausal women, we repeated the analyses in Table 2 separately for pre- and post-menopausal women with similar results in both groups (data not shown).
a and b. Adjusted odds ratios for the current analysis and recent publications [6, 7, 15] that examined the relationship between body mass index (BMI) and recent mammography use within the past two years separately for black (Fig. 1a) and white (Fig. 1b) women. Odds ratios calculated by the authors from data provided by Zhu et al. [7]
We noted an inverse relationship between socioeconomic status and obesity among white women in this study population, where the proportion who were obese in each income level was as follows: <$15,000: 51%, $15,000–24,999: 54%, $25,000–49,999: 46%, ≥$50,000: 36%. There was substantially less association between obesity and income among the black women (<$15,000: 58%, $15,000–24,999: 60%, $25,000–49,999: 59%, ≥$50,000: 53%). To evaluate whether the reduced likelihood of mammography use among extremely obese white women was a result of residual confounding by income, we ran income-specific regression models for white women, and the decrease in mammography use was apparent for women with a BMI ≥ 40 kg/m2 at each of the four income levels [For income <$15,000: OR = 0.78, 95% CI 0.60–1.03; Income $15,000–24,999: OR = 0.76, 95% CI 0.47–1.22; Income $25,000–49,999: OR = 0.41, 95% CI 0.21–0.79; and Income ≥$50,000: OR = 0.48, 95% CI 0.14–1.69]. Similarly, we observed decreased mammography use among extremely obese white women in a regression model restricted to women with no health insurance coverage [OR = 0.74, 95% CI 0.55–1.00] as well as in a model restricted to women with private health insurance [OR = 0.38, 95% CI 0.22–0.65].
We conducted additional analyses to examine whether co-morbid conditions influenced the association between mammography use and obesity. In an analysis restricted to black women who reported never being diagnosed with any of the six obesity-related conditions we included in our analysis (diabetes, high blood pressure, high cholesterol, heartburn/acid reflux, heart disease, and arthritis), we found that above-healthy weight (BMI ≥ 25 kg/m2) black women were slightly more likely to have had a mammogram within the past two years [OR = 1.14, 95% CI 0.96–1.37] compared to healthy weight black women. Among white women without any of these six conditions, being above-healthy weight was associated with decreased recent mammography use (OR = 0.62, 95% CI 0.46–0.84).
Discussion
In this large study population of black and white women of screening age, the most extreme level of obesity (BMI ≥ 40 kg/m2) was found to be inversely related to recent mammography use among white women, while black women at nearly all levels of overweight and obesity were more likely to have had a recent mammogram than black women of healthy weight. The associations remained even after adjustment for socioeconomic factors, health insurance coverage, and co-morbidities that could affect health care utilization.
These results generally correspond with the few previous examinations of obesity and mammography use that have been conducted separately for black and white women [6, 7, 15]. The previous studies found that extremely obese white women were 10–40% less likely than healthy weight white women to have had a mammogram in the past two years [6, 7, 15], but unlike our study, some also found a deficit in mammography screening at obesity levels less than 40 kg/m2 [6, 15]. Among black women, the findings have been less consistent. Ostybe et al. [15] did not find any association between body mass index and recent mammography use among black women, while Wee et al. [6] and Zhu et al. [7] both found recent mammography use somewhat more likely among women in the overweight through moderate obesity categories and slightly less likely at the most extreme level of obesity. Previous findings for black women suffered from a lack of precision due to the relatively small number of black women included in these analyses.
If causal, a deterring effect of extreme obesity on mammography screening for white women is of concern because of the overall rising prevalence of obesity in the U.S. [9] and the link between obesity and breast cancer. Studies of primarily white women have shown that obesity is associated with an increase in post-menopausal breast cancer risk (with relative risks ranging from 1.1 to 2.7) and with poorer prognosis in both pre and post-menopausal women [16–20]. Thus, if obesity is associated with decreased screening among obese white women, breast cancer mortality could feasibly increase in the future as obesity rates continue to rise.
Physician bias has been postulated as one explanation for lower rates of screening observed among obese women [5–8, 15] However, in our study, participants who had gone five years without a mammogram or who had never had one were asked to choose among several reasons why they had not received a mammogram recently, and the proportion who answered ‘Not recommended by my doctor’ was similar among obese and non-obese black (25 and 26%, respectively) and white women (20 and 21%, respectively).
Negative body self-perception among extremely obese women is another possible explanation for decreased mammography screening in this group. The seemingly different trend for black women where extreme obesity does not translate into less frequent mammogram use compared to healthy weight black women is consistent with research that suggests that black women report having less body dissatisfaction, preferring a larger body size, and defining a larger ideal body size [21, 22]. While not a direct assessment of body self-perception related to weight, in our study, the proportion of white women reporting ‘Embarrassment’ as a reason they hadn’t received a recent mammogram increased with increasing BMI. In the healthy weight category, 1.3% of white women reported ‘Embarrassment’ while the proportion increased with BMI (1.6% among overweight women, and 1.8, 3.3, and 4.8% in obesity classes I, II, and III, respectively). In contrast, the proportion of women reporting ‘Embarrassment’ was similar across BMI categories among the black women (0.5% among healthy weight women, 0.9% among overweight women, and 0.8, 0.8, and 1.0% in obesity classes I, II, and III, respectively). However, these findings should be interpreted with caution because they are based on very small numbers. If in fact white women are more self-conscious about having a larger body size than black women, this may explain some of the differences seen in mammography screening behavior among extremely obese women. Our baseline interview did not elicit information specifically focused on self-perception related to weight, and thus we were unable to evaluate the role that markers of self-image may have on screening practices.
The reasons that overweight and obese black women might be more likely to have a mammogram than healthy weight black women are not clear. We had hypothesized that heavier women may have more contact with health care providers related to care for chronic obesity-related conditions. However, this same reasoning would be expected to hold for white women, yet we observed no increase in mammography use among overweight and obese white women. It is possible that the modest positive association between BMI and mammography use is due to residual confounding by unmeasured or incompletely measured factors related to co-morbidities or health care utilization.
Despite the low-income status of the study population, the rate of mammogram use within the past two years (72% for our study population overall) is comparable to that seen in the general population. According to the 2004 Behavioral Risk Factor Surveillance System (BRFSS), the median percentage of women aged 40 and over nationwide reporting mammography within the past two years is 75% [23]. This may be an encouraging indication that screening guidelines are being met with moderate success in an underserved population [24]. However, it may be that CHC attendees who chose to participate in the SCCS were selectively more health conscious and therefore more likely to participate in cancer screening activities. In addition, CHCs tend to actively refer their patients to mammography services according to an internal survey done among CHC staff. Thus, as with most epidemiologic studies that rely on volunteers, issues related to study participant selection might limit our ability to generalize our findings regarding the prevalence of mammography utilization outside of this study. However, this would not affect the validity of our evaluation of the relationship between BMI and mammography use among black compared with white women within this study. Moreover, to the extent that our results did not differ by income level (and that we had approximately 4,000 women with a total household income above $25,000 per year to evaluate), our findings may be applicable regardless of income.
Strengths of the study include the population of over 18,000 black women and over 6,000 white women systematically identified and interviewed in a standardized manner. Further strengthening our study are the large numbers of women available at all levels of overweight and obesity; 16% of the black women and 13% of the white women in the current analysis had a BMI ≥ 40 kg/m2, compared to 5–7% of black and 2–3% of white women in previous studies [6, 7].
Limitations should also be considered. BMI was calculated from self-reported participant height and weight. While the nature of the in-person interview should minimize gross under- or over-reporting of height and weight values, reports in the literature indicate that heavier women are more likely to under-report their weight and over-report their height, leading to underestimates of their true BMI [25]. If BMI was misclassified, the ORs reported may not accurately represent the true effect at various BMI cutpoints, and, for example, the decline in mammography use among white women may in fact not be manifest until a BMI greater than the cutoff of 40 kg/m2. However, our general classification of BMI in categories of 5 kg/m2 should limit the effect of such misclassification, as even moderate misclassification in self-reported BMI could still place an individual within the same BMI category as their true measured BMI. Another potential limitation is that our baseline questionnaire did not ask about the reason for the woman’s most recent mammogram. It is likely that a small proportion of the mammograms reported were for diagnostic purposes rather than screening purposes, but this should have a negligible effect on the observed associations because of the small number of mammograms expected to be involved.
In summary, our findings among low-income women are generally supportive of those from previous reports that extremely obese white women are less likely to receive mammograms, and they extend the current knowledge regarding mammography practices among black women with a large sample size across all levels of overweight and obesity. Due to the known associations between obesity and breast cancer and the rising rate of obesity in women of all races, future research directed toward understanding the role of socioeconomic, clinical, and psychological factors related to body size and mammography practice will be of increasing importance.
References
American Cancer Society (2006) Cancer Facts & Figures 2006. American Cancer Society, Atlanta
Humphrey LL, Helfand M, Chan BKS, Woolf SH (2002) Breast cancer screening: a summary of the evidence for the U.S. Preventive services task force. Ann Intern Med 137:347–360
Olsen O, Gøtzsche PC (2001) Screening for breast cancer with mammography. Cochrane Database Syst Rev 4:CD001877
U.S. Preventive Services Task Force (2002) Screening for breast cancer: recommendations and rationale. Agency for Healthcare Research and Quality, Rockville, MD http://www.ahrq.gov/clinic/3rduspstf/breastcancer/brcanrr.htm
Wee CC, McCarthy EP, Davis RB, Phillips RS (2000) Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med 132:697–704
Wee CC, McCarthy EP, Davis RB, Phillips RS (2004) Obesity and breast cancer screening, the influence of race, illness burden, and other factors. J Gen Intern Med 19:324–331
Zhu K, Wu H, Jatoi I, Potter J, Shriver C (2006) Body mass index and use of mammography screening in the United States. Prev Med 42:381–385
Fontaine KR, Heo M, Allison DB (2001) Body weight and Cancer Screening among Women. J Womens Health Gend Based Med 10:463–470
Flegal KM, Carroll MD, Ogden CL, Johnson CL (2002) Prevalence and trends in obesity among US adults, 1999–2000. JAMA 288:1723–1727
Signorello LB, Hargreaves MK, Steinwandel MD et al (2005) The Southern Community Cohort Study: establishing a cohort to investigate health disparities. J Natl Med Assoc 97:972–979
Hargreaves M, Arnold C, Blot WJ (2006) Community health centers: their role in the treatment of minorities and in health disparities research. In: Satcher D, Pamies R (eds) Multicultural medicine and health disparities. McGraw-Hill, New York, NY, pp 485–494
Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults (1998) Arch Int Med 158:1855–1867
Hosmer DW, Lemeshow S (1989) Applied logistic regression. John Wiley & Sons, Inc., New York, NY
Andresen EM, Maligner JA, Carter WB, Patrick DL (1994) Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med 10:77–84
Ostbye T, Taylor DH Jr, Yancy WS Jr, Krause KM (2005) Associations between obesity and receipt of screening mammography, Papanicolaou tests, and influenza vaccination: results from the health and retirement study (HRS) and the asset and health dynamics among the oldest old (AHEAD) study. Am J Public Health 95:1623–1630
Carmichael AR, Bates T (2004) Obesity and breast cancer: a review of the literature. Breast 13:85–92
Key TJ, Verkasalo PK, Banks E (2001) Epidemiology of breast cancer. Lancet Oncol 2:133–140
Stephenson GD, Rose DP (2003) Breast cancer and obesity: an update. Nutr Cancer 45:1–16
McTiernan A, Gilligan MA, Redmond C (1997) Assessing individual risk for breast cancer: risky business. J Clin Epidemiol 50:547–556
Abrahamson PE, Gammon MD, Lund MJ et al (2006) General and abdominal obesity and survival among young women with breast cancer. Cancer Epidemiol Biomarkers Prev 15:1871–1877
Anderson LA, Eyler AA, Galuska DA, Brown DR, Brownson RC (2002) Relationship of satisfaction with body size and trying to lose weight in a national survey of overweight and obese women aged 40 and older. Prev Med 35:390–396
Fitzgibbon ML, Blackman LR, Avellone ME (2000) The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res 8:582–589
Centers for Disease Control and Prevention (CDC) (2004) Behavioral risk factor surveillance system survey data. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Atlanta, Georgia, 5 September 2006. http://apps.nccd.cdc.gov/brfss/display.asp?yr=2004&cat=WH&qkey=4421&state=US
Coughlin SC, Uhler RJ, Bobo JK, Caplan L (2004) Breast cancer screening practices among women in the United States, 2000. Cancer Causes Control 15:159–170
Rowland ML (1990). Self-reported weight and height. Am J Clin Nutr 52:1125–1133
Acknowledgments
We thank Michael T. Mumma for geo-coding the Community Health Centers and providing a link to the corresponding US Census data. We would also like to thank Heather M. Munro for her statistical review during the preparation of this manuscript. Financial Support: The Southern Community Cohort Study is supported by grant R01 CA92447 from the National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cohen, S.S., Signorello, L.B., Gammon, M.D. et al. Obesity and recent mammography use among black and white women in the Southern Community Cohort Study (United States). Cancer Causes Control 18, 765–773 (2007). https://doi.org/10.1007/s10552-007-9019-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-007-9019-3