Abstract
Objective
To determine how physicians responded when investigators inquired about contacting patients identified through a central cancer registry, and to examine participation rates under physician permission versus notification approaches.
Methods
We analyzed existing data from seven observational epidemiologic studies conducted in North Carolina between 1993 and 2004, capitalizing on a ‘natural experiment’ that arose when the state registry changed from a policy requiring investigators to obtain physician permission to one requiring only physician notification.
Results
When a notification approach was used, physicians approved researcher contact with a higher proportion of patients, and a higher proportion of physicians approved contact with or provided eligibility information about all patients requested, compared with a permission approach. Among physicians who were contacted under both approaches, the proportion of patients for whom they approved contact or provided information was significantly higher when they were notified. Physician notification was also associated with higher patient contact and overall response rates. Patient cooperation rates did not differ between the two approaches, suggesting that patients did not respond negatively to the fact that their physician was not explicitly asked to provide permission.
Conclusion
Notification is likely an efficient way of involving patients’ physicians, providing opportunity for physician input but avoiding the burdens associated with requiring their permission.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Population-based research is essential for understanding cancer etiology, outcomes, and quality of care. Because central cancer registries provide a population-based roster of newly diagnosed cases, they can be an invaluable resource for identifying and recruiting participants for such research. Policies for research recruitment are not uniform across registries, however, and there are insufficient data about the scientific and ethical acceptability of various approaches. For example, in a survey of all US central cancer registries [1], approximately 80% of responding registries allowed researcher contact with patients and 88% of these required or strongly recommended involving the treating physician in the recruitment process. Some required permission from the patient’s physician before the patient was contacted, while others required only that the physician be notified of planned patient contact. Potential advantages of involving the treating physician are that he or she can help manage privacy risks and exclude at the outset patients who are deceased, too ill, or otherwise ineligible. On the other hand, placing the physician in the role of ‘gatekeeper’ may limit participant accrual in otherwise beneficial research, which is itself an ethical concern [2].
Our objective was to examine how physicians in North Carolina responded to investigators’ inquiries about contact with patients identified through the central cancer registry. North Carolina is of particular interest due to a natural experiment that arose in 2003 when the registry changed from a policy requiring investigators to obtain physician permission to one requiring only that physicians be notified. We hypothesized that:
(1) Physicians would allow contact with more patients when they were notified by investigators compared with when they were required to grant permission. Some physicians likely do not respond to investigator inquiries regardless of whether a permission or notification approach is used. Non-response is taken as passive refusal under permission approaches, but as passive permission under notification approaches.
(2) Study participation rates would be higher when a physician notification approach was used compared with a physician permission approach. By allowing investigators contact with more patients, physician notification will result in the enrollment of more eligible participants.
Methods
Data sources
Study information
We obtained physician and patient response information from the records of all observational epidemiologic research conducted at the University of North Carolina (UNC) at Chapel Hill for which cases were identified via rapid case ascertainment through the North Carolina Central Cancer Registry (Table 1). Our analysis included every case sampled for each UNC study, without regard to whether the patient was subsequently enrolled.
For each patient, UNC study records included the name and address of the treating physician, the date researchers sent a letter to the physician inquiring about patient contact, and the physician’s response. Possible responses were:
-
Approved patient contact
-
Provided information that the patient was ineligible based on study criteria, too ill to participate, deceased, or had declined contact
-
Refused patient contact
For each patient whose physician approved contact, study records also contained the patient’s final disposition with regard to research recruitment. These included ineligible, deceased, unable to contact, too ill (by self-report), refused, or participated.
Physician information
We obtained additional information about treating physicians from the North Carolina Health Professions Data System (NCHPDS) [8]. Annual data were obtained for 1993 through 2003 on federal and non-federal, in-state and out-of-state, active and inactive medical doctors and doctors of osteopathy. For each physician, these data included name, address, and medical license number, as well as professional and demographic characteristics. We obtained further information about the location of physicians’ practices using the US Department of Agriculture’s Rural-Urban Continuum Codes [9].
UNC study data were obtained through data use agreements with the principal investigator of each study and NCHPDS data were used with permission from the North Carolina Medical Board. The UNC Public Health Institutional Review Board approved this project.
Data procedures
We merged the records from each UNC study with one year of NCHPDS data at a time, and created one value for each NCHPDS variable by assigning its mode. We then merged in the 2003 North Carolina rural-urban continuum codes based on the physician’s modal address, added a variable to identify the UNC study, and appended the data sets together.
We assigned each record in the appended data set to either the ‘permission group’ or the ‘notification group’ based on two criteria. First, records where the physician letter date was prior to 1 April 2003 (when the North Carolina Central Cancer Registry changed its policy from permission to notification) were assigned to the permission group. Records with physician letter dates on or after 1 April 2003 were assigned to the notification group. Second, several studies that recruited patients prior to April 2003 used a ‘blanket consent’ option (Table 1). In these studies, physicians were initially contacted using a permission approach, but were given the option of signing a form granting researchers permission to contact patients identified in the future as potentially eligible for the study. Physicians who signed this form were notified about subsequent patients, and therefore records associated with these physicians were assigned to the notification group.
Data measures and analysis
Data were analyzed using Stata 8.0® (College Station, TX). We descriptively compared physician and patient responses in the permission group to those in the notification group using Pearson’s χ2 test. To test our first hypothesis, we conducted weighted least squares regression using the following model:
Physician Cooperation is a continuous variable, aggregated at the physician/policy level, indicating the proportion of all patients requested under each policy (permission versus notification) for whom the physician either approved researcher contact or provided information. These responses were grouped together on the premise that approving contact or providing information on the patient’s behalf are distinct from refusing contact in terms of supporting both patient autonomy and research. Each physician/policy observation was weighted by the total number of patients about which the physician was asked under that policy, and standard errors were adjusted for clustering on physician license number to account for repeated observations on physicians who were asked about patients under both policies.
Policy, the main explanatory variable of interest, is a dichotomous variable indicating whether the physician/policy observation occurred under permission or notification. The other explanatory variables were physician characteristics: Primary or secondary medical specialty (surgeon versus non-surgeon), sex (male versus female), race/ethnicity (white/non-Hispanic versus other), last year of medical school (before 1980 versus 1980 or after, based on the 1979 publication of the Belmont Report [10], a landmark report that set forth basic principles of ethical research), primary or secondary practice setting (medical school/university versus other), and rural/urban continuum (metropolitan versus non-metropolitan).
To assess our second hypothesis, we calculated three participation rates (Table 2), adapted from the work of Slattery et al. [11], in the permission group and in the notification group:
-
Patient Contact Rate: The percentage of patients with whom there was contact
-
Patient Cooperation Rate: The percentage of patients who participated among those who were contacted
-
Overall Response Rate: The proportion of patients who participated among those who were selected and eligible
To compare rates, we used a case study technique called ‘pattern matching’ [12]. Under pattern-matching logic, if the observed pattern matches the theorized pattern, it suggests evidence of internal validity and the presence of a causal relationship.
Results
Physician characteristics
The appended data set comprised 1,351 physicians. Of these, 555 were contacted only under permission, 417 were contacted only under notification, and 379 were contacted under both approaches. Virtually all were matched with information from NCHPDS (Table 3), and the proportions matched in the permission versus notification group did not differ significantly (97.9% versus 98.4%, p = 0.483). Surgery was the primary or secondary specialty for most, and a substantial majority were male, white/non-Hispanic, graduated from medical school ≥1980, practiced in a non-academic setting, and located in a metropolitan area (Table 3).
Physician responses and physician cooperation
There were 9,909 patients in the appended data set. The mean number of patients per physician was 6.3 in the permission group and 5.1 in the notification group (Table 4), although individual physicians were asked about as many as 95 patients per study.
Among the 1,351 physicians in the appended data set, 38.1% were offered the option of signing a blanket consent form and over half (54.0%) of these did so. The remaining 61.9% were either contacted prior to April 2003 in studies that did not offer a blanket option, or were contacted after April 2003 when the need for blanket consent no longer applied.
Overall, physicians approved researcher contact with 91.5% of patients requested, provided information about 3.4%, and refused researcher contact with 5.1%. However, responses differed significantly depending on the approach used (Table 4). Compared with physicians in the notification group, those in the permission group approved contact with a smaller proportion of patients (88.7% versus 95.4%, p<0.001), provided information about a larger proportion (4.3% versus 2.2%, p<0.001), and refused researcher contact with a larger proportion (7.0% versus 2.4%, p<0.001). With regard to Physician Cooperation, 87.0% of physicians in the permission group approved or provided information for all patients requested, while 2.1% refused researcher contact with all patients requested. In the notification group, these proportions were 91.3% and 1.4%, respectively.
In regression analysis (Table 5), the type of physician involvement had a significant impact on Physician Cooperation. Controlling for other factors in the model, the proportion of patients for whom the physician either approved researcher contact or provided information was, on average, 4.1 percentage points lower in the permission group than in the notification group. We repeated this analysis in a data set restricted to only those physicians who were contacted under both permission and notification, and also in each study where recruitment spanned the policy change from permission to notification. In each case, the type of physician involvement had a significant effect (data not shown). For example, among physicians contacted under both approaches, Physician Cooperation was 3.7 percentage points lower (standard error = 1.7, p = 0.027) when they were asked permission compared with when they were notified.
Patient responses and participation rates
Among patients whose physician approved researcher contact, the proportion in each study who refused to participate ranged from 10.7% to 30.4% (Table 6), but did not differ significantly in the physician permission group compared with the physician notification group (14.2% versus 14.3%, p = 0.913).
The Patient Contact Rate in each study ranged from 86.6% to 96.8%, and was higher in the notification group compared with the permission group (93.8% versus 90.5%) (Table 6). The Patient Cooperation Rate ranged from 61.0% to 87.7%, and was similar in the notification and permission groups (81.6% versus 82.0%). The Overall Response Rate ranged from 52.6% to 84.1%, and was higher in the notification group than in the permission group (75.2% versus 72.9%).
Both physician and patient responses differed significantly in the Prostate Study compared with the other studies. Physicians in the Prostate Study approved researcher contact with a smaller proportion of patients (86.6% versus 92.5%, p<0.001) and refused contact with a larger proportion (8.6% versus 4.4% p<0.001). Only 74.7% of the physicians in the Prostate Study approved researcher contact or provided information for all patients requested, compared with 90.2% of physicians in the other studies. The proportion of patients who were ineligible was significantly higher than in the other studies (32.3% versus 7.0%, p<0.001), as was the proportion who refused to participate (16.7% versus 13.8%, p = 0.004).
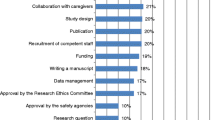
When the Prostate Study was excluded as an outlier, the differences in participation rates between the notification group and the permission group increased (Figure 1). The Patient Contact Rate was 3.0 percentage points higher in the notification group compared with the permission group (94.9% versus 91.9%), the Patient Cooperation Rate was 1.6 percentage points higher (84.2% versus 82.6%), and the Overall Response Rate was 4.3 percentage points higher (79.2% versus 74.9%).
Discussion
Using data from seven population-based studies in North Carolina, we sought to determine how physicians responded when investigators conducting observational epidemiologic research inquired about contacting patients identified through the central cancer registry, and to examine participation rates under physician permission versus notification approaches. The results provided strong support for our first hypothesis. When a notification approach was used, physicians approved researcher contact with a higher proportion of patients, and a higher proportion of physicians approved contact or provided information for all patients requested, compared with a permission approach. These findings were further confirmed in regression analysis, which showed that Physician Cooperation was significantly lower when a permission approach was used. It is likely that some physicians do not respond under either approach, which would be taken as passive refusal in permission studies but as passive permission in notification studies, thus allowing investigators access to more patients.
We also found that physicians provided information (e.g., that the patient was ineligible) less often when notified rather than asked permission. One explanation could be that no physician response is required under a notification approach. The implementation of the Health Information Portability and Accountability Act (HIPAA) in 2003 may also have played a role. The North Carolina Central Cancer Registry changed its policy in part because some physicians were concerned about whether actively providing permission for patient contact could be a violation of HIPAA, as compared with being notified but not required to respond. HIPAA concerns may extend to the provision of information relevant to study recruitment as well.
We found that the Prostate Study was an outlier in several respects. Although strictly observational, this study explored issues related to treatment and outcomes and, in particular, attempted to recruit patients prior to the initiation of treatment. In addition to a large proportion of patients being found ineligible because treatment had already begun, it may be that some physicians are more likely to refuse patient contact for studies investigating the treatment decision-making process and outcomes, compared with studies that focus only on risk factors.
The results also provided support for our second hypothesis. Physician notification was associated with higher Patient Contact and Overall Response rates. Patient Cooperation did not differ under notification compared with permission, suggesting that patients did not respond negatively to the fact that their physician was not explicitly asked to provide permission. When the Prostate Study was excluded, Patient Cooperation was actually higher under physician notification. These findings are consistent with previous studies of patients’ attitudes toward physician permission in observational epidemiologic research, which suggested that research participants were generally glad their physician allowed researchers to contact them and that many would have agreed to take part without prior physician permission [13–15].
Assuming that permission and notification are both ethical approaches to research recruitment through cancer registries, our findings suggest that notification is an efficient way to involve the treating physician. In general, physician involvement may facilitate relationships between physicians and researchers, and may also be a positive influence with some patients [13, 14]. However, other patients may view the ‘physician-as-gatekeeper’ role as paternalistic, and the established physician-patient relationship assumed as an advantage of this role does not always exist. Many central cancer registries (including the one in North Carolina) do not routinely collect information that identifies patients’ physicians [1]. Therefore, the physician-of-record available to researchers is often the surgeon listed on the pathology report, who may have no ongoing responsibility for or knowledge of the patient’s condition. Further, physicians may be asked about a large number of patients and requiring their permission does not‘guarantee careful consideration of patients’ eligibility nor added privacy protection [16]. Notification provides‘opportunity for physician input, but frees both the physician and the researcher from the burden of a required response when the physician has no objection to patient contact, which our analysis suggests is the case most of the time.
Our study had a number of strengths. The data included substantial numbers of patients and physicians. They were obtained from research on several types of cancer conducted by five different principal investigators with seven different project managers. All data analyzed came from one institution, allowing us to better isolate the effects of permission versus notification.
Several factors may limit the interpretation of our findings. First, a great deal of effort has been expended in North Carolina to develop relationships among the central cancer registry, reporting entities, researchers, and physicians. In the Carolina Breast Cancer Study, for instance, presentations were made at each hospital in the study area to preview study objectives and extensive efforts were made to assure physicians that patient care was not an objective of epidemiologic studies [17]. In states and institutions that have not yet developed these relationships, the differences between permission and notification could be greater than found here.
Second, patient-level characteristics (e.g., age, sex, race) may be a confounder in the relationship between physician approach and physician response. We believe this was unlikely to be a major issue in our analysis because of the diversity of populations associated with the types of cancer studied under each approach. However, future research could reveal differences in physician response based on patients’ demographic characteristics, which may prove useful for refining recruitment approaches. Understanding patients’ preferences about physician involvement – including what patients believe or expect about how their physician would make decisions on their behalf – is another important area for future research. Shedding light on these issues is important for weighing the advantages and disadvantages of the physician-as-gatekeeper role and for developing balanced approaches to privacy and accrual concerns.
References
Beskow LM, Sandler RS, Weinberger M (2006) Policies for research recruitment through U.S. central cancer registries: Balancing privacy and scientific issues. Am J Public Health (in press)
LM Beskow JR Botkin M Daly et al. (2004) ArticleTitleEthical issues in identifying and recruiting participants for familial genetic research Am J Med Genet 130A 424–431 Occurrence Handle10.1002/ajmg.a.30234
B Newman PG Moorman R Millikan et al. (1995) ArticleTitleThe Carolina Breast Cancer Study: integrating population-based epidemiology and molecular biology Breast Cancer Res Treat 35 51–60 Occurrence Handle10.1007/BF00694745 Occurrence Handle1:STN:280:ByqA3sjjvFE%3D Occurrence Handle7612904
NJ Shaheen LM Silverman T Keku et al. (2003) ArticleTitleAssociation between hemochromatosis (HFE) gene mutation carrier status and the risk of colon cancer J Natl Cancer Inst 95 154–159 Occurrence Handle1:CAS:528:DC%2BD3sXovFeluw%3D%3D Occurrence Handle12529348
CB Begg A Hummer U Mujumdar et al. (2004) ArticleTitleFamilial aggregation of melanoma risks in a large population-based sample of melanoma cases Cancer Causes Control 15 957–965 Occurrence Handle15577298
PA Godley J Clark D Gellantly S Jackson JA Talcott (2005) ArticleTitleRace and prostate cancer: attitudes toward diagnosis and treatment among newly diagnosed patients J Clin Oncol 23 531
National Cancer Institute Cancer Control & Population Sciences. Cancer Care Outcomes Research & Surveillance Consortium [Web Page]. Accessed Oct 10, 2005. Available at http://healthservices.cancer.gov/cancors/
Cecil G. Sheps Center for Health Services Research. North Carolina Health Professions Data System [Web Page]. Accessed Oct 10, 2005. Available at http://www.shepscenter.unc.edu/hp/
USDA Economic Research Service. Rural-Urban Continuum Codes [Web Page]. Accessed Oct 10, 2005. Available at http://www.ers.usda.gov/Data/RuralUrbanContinuumCodes/
National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research. Washington DC: US Government Printing Office (1979)
ML Slattery SL Edwards BJ Caan RA Kerber JD Potter (1995) ArticleTitleResponse rates among control subjects in case-control studies Ann Epidemiol 5 245–249 Occurrence Handle1:STN:280:ByqA3s%2FhsVU%3D Occurrence Handle7606315
RK Yin (1994) Analyzing Case Study Evidence. Case Study Research: Design and Methods EditionNumber2 Sage Publications Thousand Oaks, CA
DA Savitz RF Hamman C Grace K Stroo (1986) ArticleTitleRespondents’ attitudes regarding participation in an epidemiologic study Am J Epidemiol 123 362–366 Occurrence Handle1:STN:280:BimC38jis1Q%3D Occurrence Handle3511679
CC Boring E Brockman N Causey HR Gregory RS Greenberg (1984) ArticleTitlePatient attitudes toward physician consent in epidemiologic research Am J Public Health 74 1406–1408 Occurrence Handle1:STN:280:BiqD28bpsVE%3D Occurrence Handle6507697
DP Funch JR Marshall (1981) ArticleTitlePatient attitudes following participation in a health outcome survey Am J Public Health 71 1396–1398 Occurrence Handle1:STN:280:Bi2D1cfptVQ%3D Occurrence Handle7316006
JH Gurwitz E Guadagnoli MB Landrum RA Silliman R Wolf JC Weeks (2001) ArticleTitleThe treating physician as active gatekeeper in the recruitment of research subjects Med Care 39 1339–1344 Occurrence Handle10.1097/00005650-200112000-00009 Occurrence Handle1:STN:280:DC%2BD3MnntFOnsw%3D%3D Occurrence Handle11717575
TE Aldrich D Vann PG Moorman B Newman (1995) ArticleTitleRapid reporting of cancer incidence in a population-based study of breast cancer: one constructive use of a central cancer registry Breast Cancer Res Treat 35 61–64 Occurrence Handle10.1007/BF00694746 Occurrence Handle1:STN:280:ByqA3sjjvFI%3D Occurrence Handle7612905
Acknowledgements
The authors thank Christopher F. Martin and Mary Beth Bell for their input and assistance in carrying out this project; Dr. Andrew F. Olshan, Dianne Mattingly, and Jessica Tse for their role in providing study data; and the Cecil G. Sheps Center for Health Services Research at UNC and the North Carolina Medical Board for providing access to NCHPDS data. This project was financially supported by a grant from the National Cancer Institute (R25-CA57726) for the University of North Carolina-Chapel Hill Lineberger Cancer Control Education Program
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beskow, L.M., Millikan, R.C., Sandler, R.S. et al. The Effect of Physician Permission Versus Notification on Research Recruitment through Cancer Registries (United States). Cancer Causes Control 17, 315–323 (2006). https://doi.org/10.1007/s10552-005-0521-1
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-005-0521-1