Abstract
Background
Increased engagement with community-based practices is a promising strategy for increasing clinical trials access of diverse patient populations. In this study we assessed the ability to utilize a patient-advocacy organization led clinical network to engage diverse practices as field sites for clinical research.
Methods
GO2 for Lung Cancer led recruitment efforts of 17 field sites from their Centers of Excellence in Lung Cancer Screening Network for participation in an implementation-effectiveness trial focused on smoking cessation integration into screening programs for lung cancer. Sites were engaged by one of three methods: 1) Pre-Grant submission of letters of support, 2) a non-targeted study information dissemination campaign to network members, and 3) proactive, targeted outreach to specific centers informed by previously submitted network member data. Detailed self-reported information on barriers to participation was collected from centers that declined to join the study.
Results
Of 17 total field sites, 16 were recruited via the targeted outreach campaign and 1 via pre-grant letter of support submission. The sites covered 13 states and 4 United States geographic regions, were varied in annual screening volumes and years of screening program experience and were predominantly community-based practices (10 of 17 sites). The most reported reason (by 33% of sites) for declining to participate as a field site was inadequate staffing bandwidth for trial activities. This was especially true in community-based programs among which it was reported by 45% as a reason for declining.
Conclusions
Our results suggest that this model of field site recruitment leveraging an existing partnership between an academic research team and an informal clinical network maintained by a disease-specific patient advocacy organization can result in engagement of diverse, community-based field sites. Additionally, reported barriers to participation by sites indicate that solutions centered around providing additional resources to enable greater capacity for site staff may increase community-practice participation in research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Only 3% to 5% of cancer patients in the US participate in clinical trials despite National Comprehensive Cancer Network guidelines recommending clinical trial consideration as part of a high-quality standard of care [1]. Additionally, demographic and racial/ethnic disparities in clinical trial enrollment exist [2, 3], limiting the broad applicability of trial results to all members of the patient population. Over 80% of cancer patients are treated in community-based practice settings [4], but most clinical trials are conducted in academic practice settings. As a result, many patients are not treated in locations where appropriate trials are taking place and thus face additional hurdles (travel, negotiating novel health systems, etc.) to trial participation. Engaging with community-based practices may help bring more research and clinical trial opportunities directly to patients and thus could increase opportunities to enroll diverse patient populations. Additionally, involving a range of practice settings in clinical trials will help in closing the gap between research discovery and real-world clinical application [5].
Previous studies have found that formal cooperative groups and practice-based research networks with robust research infrastructure can be effective for engaging clinical sites [6,7,8,9,10] in therapeutic and cancer care delivery research. Although engaging well-resourced formal networks may be efficient for many translational studies, diverse patients being seen at community-based practices that are not part of these networks have fewer opportunities for trial participation, exploring ways to engage community practices beyond these formal network settings could help increase trial access and diversity. Among the strategies for engaging clinical sites in research, leveraging existing connections, building trusting partnerships, and personalizing outreach and recruitment methods to local site concerns and characteristics are recommended [5, 7, 9]. Patient Advocacy Groups (PAGs), who in many areas are forming relationships with the clinical community to ensure implementation of and access to high quality care for the patient communities they represent, may also be effective partners in helping research teams connect with and engage community sites in research studies.
A lung cancer focused PAG, GO2 for Lung Cancer (GO2), has created an extensive national network of over five hundred (500 +) Centers of Excellence in Lung Cancer Screening (COE-LCS). All COE-LCS network members provide low-dose computed tomography (LDCT) for early detection of lung cancer and must report and meet several member eligibility criteria reflecting compliance with high quality lung cancer screening (e.g., shared decision-making processes, having referral processes to multidisciplinary clinical teams for follow up and treatment when appropriate). The COE-LCS network represents an ongoing partnership between GO2 and COE-LCS centers, with GO2 facilitating peer-to-peer learning and resource-sharing opportunities, including an e-newsletter and annual conference, supporting an on-line community committed to addressing challenges in implementing lung cancer screening, with technical assistance from GO2 staff for designing program development and quality improvement initiatives, and facilitating data-sharing. Network members complete an annual survey describing key organizational characteristics of their screening program and receive access to personalized quality care benchmarking reports. A key strength of GO2’s COE-LCS is the inclusion of both academic and community-affiliated LCS programs as well as LCS programs serving diverse patient populations in rural and urban settings. Although the COE-LCS network lacks characteristics of formal research networks, such as dedicated funding, designated research staff and a centralized research management infrastructure, we hypothesized that, COE-LCS members would be receptive to establishing a partnership with a clinical research team thereby, enhancing field site recruitment for lung cancer research studies.
To describe the process of using the COE-LCS network to engage diverse practices as field sites for a research study, GO2 partnered with investigators at Memorial Sloan Kettering Cancer Center and New York University School of Global Public Health leading the Cessation and Screening to Save Lives (CASTL) trial [11]. Funded by the National Cancer Institute, the overall objective of the CASTL trial was to identify optimal treatment strategies for improving cessation outcomes among adults seeking lung cancer screening (LCS) [11]. GO2 functioned as a recruitment core by identifying and managing field site recruitment through the COE-LCS network. The main goal was to describe and assess GO2 led site outreach strategies. We also sought to identify barriers to research participation within the network to better understand the strengths and limitations of this approach to field-site recruitment.
Methods
Field site eligibility criteria
GO2 sought to recruit lung cancer screening sites for the CASTL trial by targeting voluntary members of GO2’s nationwide COE-LCS network. To be eligible for participation, potential field sites were required to have at least one year of lung cancer screening experience and have a clinical volume of conducting at least 20 LDCT screenings per month (either initial/baseline or repeat annual scans). A site stipend of $7000 payable at predetermined trial milestones (i.e., activation, 50% accrual, study close out) was provided to help offset costs of trial participation.
Outreach methods
GO2 staff were responsible for field site selection using three outreach strategies during different stages of the study grant: pre-grant award solicitation of letters of support, a post-grant award non-targeted dissemination campaign, and a post-grant award targeted proactive outreach campaign. First, prior to the grant application submission, letters of support (LOS) were obtained from a subset of COE-LCS sites that had a record of past engagement in GO2 related projects. These LOS were requested via email and follow up phone contact (if no response to email). The letters indicated initial interest in participating as a field site for CASTL and were included in the grant application. After the grant was awarded, GO2 recontacted these initial sites and confirmed trial eligibility. Second, once the grant was awarded, a non-targeted dissemination campaign was implemented in which GO2 staff shared trial opportunity information in a weekly e-newsletter sent to all COE-LCS network members. Sites were encouraged to contact a GO2 staff member via an email address or phone number if they had interest in being considered as a field site. Sites responding to the newsletter announcement were screened for trial eligibility by GO2 staff. Third, after the grant was awarded, a targeted, proactive outreach campaign was conducted in which GO2 staff identified COE-LCS network members that met trial eligibility criteria, as defined above, based on the most recent available site data (2016–18) from GO2’s annual COE-LCS network survey. If a site had provided a pre-grant award LOS or contacted GO2 expressing interest in the study after seeing the e-newsletter ad from the non-targeted dissemination campaign they were not selected for this proactive outreach. Eligible sites were contacted by GO2 staff via email twice at two-week intervals and then by phone if there was no response to prior emails. GO2 prioritized reaching out first to sites where publicly available site data or GO2 COE-LCS survey collected data on patient demographics indicated the site served minoritized populations that are traditionally under-represented among clinical trial participants. Upon successful contact, GO2 staff provided detailed trial information, confirmed site eligibility, and assessed interest in participation as a field site.
Staff representatives from confirmed eligible and interested sites were subsequently invited to participate in a 60-min trial informational webinar, co-led by GO2 and CASTL staff at Memorial Sloan Kettering Cancer Center (MSK). This introductory webinar provided detailed information about the CASTL protocol, timeline, field site responsibilities, financial incentives, the regulatory process, and other logistics. After completion of the webinar, GO2 staff followed up with sites and confirmed site interest.
Site onboarding
All eligible sites with confirmed interest in joining CASTL were then connected with CASTL’s Research Project Manager (RPM) from MSK’s Data Coordinating Center for site onboarding. The RPM coordinated trial start up and trial activation activities to ensure that sites had completed all regulatory, contractual, and other tasks required for trial activation and participant enrollment. To improve the efficiency of project management, regulatory oversight and to reduce burden on the local participating LCS sites, MSK served as the single IRB of Record for this multi-institutional trial. The CASTL study was approved by the MSK Cancer Center Institutional Review Board (IRB # 17–500). All sites were approved for ceding regulatory oversight based on assessment of IRB accreditation, research infrastructure, potential conflicts of interest and other relevant regulatory considerations. Once approved by the MSK Human Research Protection Program, Reliance Agreements, Memoranda of Agreement and Data Transfer Agreements were fully executed. Site coordinators were verbally consented, trained by the trial PIs to deliver trial interventions, and attended a trial activation call with the RPM to discuss workflow integration, trial management and data reporting before recruitment began at their site.
Data collection and analysis
The process of prospective field site engagement was documented in detail throughout the recruitment and onboarding process. If a screening program was found to be ineligible, the reasons were documented. If a site withdrew their agreement to participate, a short “exit-assessment” was conducted with a site representative to inquire about the reasons for withdrawing. A standardized, open-ended question, “Thank you for your time in considering the CASTL study – would you be able to share briefly with us the main reasons and barriers that that led to your decision not to participate?”, was asked to site representatives with follow-up probes as needed. Site representatives were contacted twice via email and once via phone to provide a response to the question before being considered non-responsive. Descriptive statistics were used to report recruitment and enrollment status by outreach strategy, demographics of sites, and reasons for refusal.
Results
Site recruitment outcomes
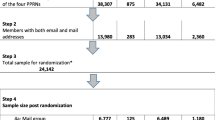
Figure 1 illustrates site recruitment outcomes for each of the three site recruitment strategies
Site Recruitment Flow Diagram: CONSORT figure showing yield of the three site recruitment outreach methods for the CASTL study. The three methods included: 1) Letters of Support: Prior to the study grant award, asking pre-selected sites with history of past engagement with GO2 to submit a letter of support for the CASTL grant application and then inviting those that met trial eligibility to join as a field site upon receiving grant funding; 2) Non-Targeted Dissemination Campaign: After the study grant award, sending an ad with trial information to network members via a regular weekly network email newsletter, and 3) Targeted Proactive Outreach Campaign: After the study grant award, directly contacting a select number of sites, that were pre-determined to meet trial eligibility criteria through responses provided to a regular annual network survey, with trial information. A single network member represents a single medical facility providing LDCT screening. Individual network members may either operate as a single-facility screening program or be part of a larger multi-facility screening program. Reasons sites provided for not joining trial are indicated at each stage; sites could report multiple reasons. SCOE=Screening Center of Excellence
Pre-grant submission letters of support
In total, 15 COE-LCS network members provided LOS prior to the initial grant submission. Seven of the 15 sites that provided LOS were ultimately invited to join the trial, based on GO2 confirmation of eligibility and pre-assessment of site demographics for ability to support diverse patient recruitment. Of these seven programs, five (71%) attended a trial webinar and one program agreed to serve as a field site.
Non-targeted dissemination campaign
Post-grant award, 527 COE-LCS network members were sent the e-newsletter that included study information. Thirteen interested respondents (2% of facilities receiving the newsletter) sought more information about participation in the CASTL trial. Unfortunately, none of the 13 sites that responded to the e-newsletter announcement joined the CASTL trial.
Targeted proactive outreach campaign
Among the total COE-LCS network, 260 screening programs (47%) had provided data on at least one annual survey between 2016–2018, enabling them to be assessed for targeted proactive outreach. If a site had responded to the e-newsletter ad from the non-targeted dissemination campaign at any point, it was not considered further for targeted proactive outreach. Of the remaining sites, 70 were selected for further outreach, based on GO2 assessment of meeting eligibility criteria based on survey responses, patient population demographics and perceived ability to support diverse patient recruitment, and GO2 knowledge of past engagement with network initiatives. Post-grant award, GO2 staff reached out directly to staff contacts at each of these targeted sites to extend invitations to participate in the CASTL trial. Fifty-three of these 70 sites (76%) expressed initial interest and were invited to schedule introductory 1:1 webinars co-led by the GO2 and MSK teams. Out of these 53 targeted sites that expressed potential interest in enrollment, 31 (53%) attended a trial webinar and ultimately 16 (30%) enrolled as field sites for CASTL.
Ultimately, we recruited a diverse set of 17 trial sites nationwide (Table 1) with varying annual screening volumes (ranging from 240–2700 LDCT scans annually), usual care practices for smoking cessation, and years of experience running a LCS program (ranging from 1–14 years). Among the final 17 sites enrolled in the trial, 10 (59%) were community-based screening sites and 7 (40%) were academic-based screening sites. Sites were primarily located in large or clustered urban settings in 13 states and covered 4 geographic regions of the continental United States (Fig. 2 and Table 1).
Site refusal reasons
We collected detailed information on the reasons screening programs declined trial participation (Figs. 1 and 3A). Overall, the most reported reason for refusal was “competing staff priorities” (33%) suggesting that existing demands on staff would not allow adequate additional bandwidth for research trial activities. The second most common reason reported by 20% was “low screening volume”, meaning that the program perceived their current screening volume, regardless of meeting study eligibility levels, wouldn’t allow them to meet patient recruitment goals in a timely manner. Almost all programs declining participation due to “low screening volume” (7 of 8 sites) were from programs that responded to the newsletter ad. Other refusal reasons were: “competing research priority” (program was already participating in another smoking cessation study or project targeting people with active tobacco use who are also seeking lung cancer screening); “concern about disruption to workflow” (program perceived that integrating the trial protocol could disrupt routine LDCT screening operations); “inadequate financial incentive” (program felt the time and expense of trial participation exceeded the incentive offered), and “trial intervention similar to site standard” (program felt smoking cessation intervention being studied was too similar to current standard of care and did not want to randomize participants to the various treatment conditions). There were different reasons for refusal reported by academically affiliated screening programs and community-based programs (Fig. 3B). The most frequent reasons reported by academic programs were defined by prioritization of research opportunities and target patient population availability (“competing research priority” and “low screening volume” (30% of programs reported each)). However, the top refusal reason reported by community-based sites was centered entirely on lack of internal staffing resources to support a research study (“competing staff priorities” (reported by 45% of programs)).
Reasons for site refusal: A Top overall reasons that screening programs declined to join the CASTL trial. Bars represent the proportion of sites providing the indicated reason. Sites could provide multiple reasons. Data is from N = 39 screening programs that were able to be contacted to provide a reason for declining to join. B Top reasons that screening programs declined to join the CASTL trial by affiliation type. Bars represent the proportion of programs that provided the indicated reason. Sites could provide multiple reasons. Data are from N = 10 academic-affiliated sites and N = 29 community (no academic affiliation) sites that were able to be contacted to provide a reason for declining to join
Discussion
We examined the utility of leveraging an informal, patient advocacy-led, clinical network to recruit and engage diverse LCS sites for an implementation effectiveness clinical trial. Utilizing the existing COE-LCS network, recruitment efforts successfully engaged a geographically diverse set of 17 field sites that were predominantly community-based programs that are often under-represented in multi-site research studies. Most field sites were in urban settings, consistent with the current geographic locations of lung cancer screening programs and the COE-LCS national network [12,13,14]. The success of this field site recruitment approach is particularly notable given that the COE-LCS network is a relatively informal voluntary network of community-based LCS sites without a formal research infrastructure, such as centralized research staff and research regulatory oversight typically available in more traditional practice-based research networks and other multi-center cooperative trial groups. In addition, the COE-LCS network is by design and mission centered around supporting translation of evidence-based care guidelines into real-world clinical practice, and this synergy with the aims of implementation-effectiveness research may indicate further that the network is particularly suited to support these types of studies. To our knowledge, this paper describes a first of its kind multi-pronged field site recruitment approach leveraging a community-engaged, research partnership between a disease-specific, PAG and an academic research team.
Three site engagement strategies were utilized: 1) requesting programs to submit pre-grant submission letters of support; 2) a non-targeted study information dissemination campaign, and 3) a targeted proactive outreach campaign to potential field sites. It is noteworthy that the conventional strategy of obtaining a pre-submission letter of support from potential sites for an initial grant application was not associated with strong likelihood of site participation. Sites providing a pre-grant submission LOS may not have fully considered the benefits and burdens of trial participation. In addition, considering that the time lag between obtaining letters of support and extramural funding decisions for research projects is generally more than 6 months, organizational changes (e.g., staffing, leadership) may preclude actual trial participation.
The targeted proactive outreach campaign, in which sites were selected for direct outreach via a pre-screening process utilizing both annual survey data and GO2 prior relationships with individual network members was the most effective outreach approach, yielding a higher participation rate than either the pre-grant LOS or the non-targeted dissemination campaign. Of note, several sites that expressed initial interest in response to the non-targeted dissemination did not meet site eligibility criteria for trial participation and all but one field site was ultimately recruited via the targeted proactive engagement method. These findings indicate that one of the primary advantages of the COE-LCS network for field site recruitment was the ability to pre-identify sites meeting specific eligibility criteria and leverage pre- existing staff relationships and community partnerships, rather than using traditional, established dissemination channels (e.g., newsletter) to solicit trial participation from the large number of COE-LCS programs. These findings suggest that collaborative partnerships between GO2 and the COE-LCS network members and the availability of pre-existing site data collected annually from network members enhanced field site recruitment efforts. Enhancing the pragmatic design of the trial, the participating field sites have varied clinical volume, screening experience, patient characteristics, and location, suggesting that the proactive targeted recruitment method engaged relatively heterogeneous lung cancer screening programs.
To further evaluate the specific strengths and limitations of this field site recruitment approach, we also identified barriers to research participation among COE-LCS network members. Competing staff priorities was the most common reason reported by sites who declined participation. This barrier was most commonly reported by almost half of the community-based sites. In contrast, in sites affiliated with academic institutions, the top reasons for refusal were either multiple completing research opportunities or concerns about not having enough eligible patients for study recruitment. Given that community-based COE-LCS network programs have historically reported in annual GO2 survey data a higher average screening volume than the academic programs in the network, this may partially explain the increased demands on staff time/bandwidth, along with concerns about not having adequate patient population for achieving the site accrual targets. As demands on program staff appeared to be a primary barrier to research participation in the community setting, solutions centered around providing additional financial or human resources to increase capacity for screening site staff to meet trial participation demands could help enhance site recruitment efforts. Since community-based screening programs appear to see a higher volume of patients, providing this kind of support may be key to engaging sites serving diverse populations of study participants and may enhance this PAG-led approach.
Conclusion
These results suggest that field site recruitment leveraging an existing partnership between an academic research team and an informal clinical network maintained by a disease-specific PAG can be fruitful for engaging community field sites often underrepresented in clinical research. Our experience conducting a smoking cessation implementation-effectiveness trial in the context of lung cancer screening will need to be replicated to determine the wide applicability of this model for other clinical trials. Additionally, we identified key barriers to research participation reported by different types of field sites that will likely need to be proactively addressed to enhance future site recruitment efforts following this model. All in all, the findings support the idea that PAGs, who have established relationships with the clinical community through their programmatic work, can be effective partners in diverse field site recruitment efforts.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- GO2:
-
GO2 for Lung Cancer
- COE-LCS:
-
Centers of Excellence in Lung Cancer Screening
- LDCT:
-
Low-dose computed tomography
- CASTL:
-
Cessation and Screening to Save Lives trial
- MSK:
-
Memorial Sloan Kettering Cancer Center
- RPM:
-
Research Project Manager
- IRB:
-
Institutional Review Board
- LOS:
-
Letters of support
- LCS:
-
Lung Cancer Screening
References
Unger JM, Vaidya R, Hershman DL, Minasian LM, Fleury ME. Systematic review and meta-analysis of the magnitude of structural, clinical, and physician and patient barriers to cancer clinical trial participation. J Natl Cancer Inst. 2019;111(3):245–55.
Kwiatkowski K, Coe K, Bailar JC, Swanson GM. Inclusion of minorities and women in cancer clinical trials, a decade later: have we improved?. Cancer. 2013;119(16):2956–63.
Pang HH, Wang X, Stinchcombe TE, Wong ML, Cheng P, Ganti AK, et al. Enrollment trends and disparity among patients with lung cancer in national clinical trials, 1990 to 2012. J Clin Oncol. 2016;34(33):3992–9.
Pfister DG, Rubin DM, Elkin EB, Neill US, Duck E, Radzyner M, Bach PB. Risk adjusting survival outcomes in hospitals that treat patients with cancer without information on cancer stage. JAMA Oncol. 2015;1(9):1303–10.
Solberg LI. Recruiting medical groups for research: relationships, reputation, requirements, rewards, reciprocity, resolution, and respect. Implement Sci. 2006;1:25.
Asch S, Connor SE, Hamilton EG, Fox SA. Problems in recruiting community-based physicians for health services research. J Gen Intern Med. 2000;15(8):591–9.
Ellis SD, Bertoni AG, Bonds DE, Clinch CR, Balasubramanyam A, Blackwell C, et al. Value of recruitment strategies used in a primary care practice-based trial. Contemp Clin Trials. 2007;28(3):258–67.
Geiger AM, O’Mara AM, McCaskill-Stevens WJ, Adjei B, Tuovenin P, Castro KM. Evolution of cancer care delivery research in the NCI community oncology research program. J Natl Cancer Inst. 2020;112(6):557–61.
Graham DG, Spano MS, Stewart TV, Staton EW, Meers A, Pace WD. Strategies for planning and launching PBRN research studies: a project of the Academy of Family Physicians National Research Network (AAFP NRN). J Am Board Fam Med. 2007;20(2):220–8.
Howard RL, Avery AJ, Bissell P. Description of a multifaceted strategy for recruiting general practitioners and community pharmacists to talk about medication errors. Int J Pharm Pract. 2006;14(3):205–9.
Ostroff JS, Shelley DR, Chichester LA, King JC, Li Y, Schofield E, et al. Study protocol of a multiphase optimization strategy trial (MOST) for delivery of smoking cessation treatment in lung cancer screening settings. Trials. 2022;23(1):664.
Eberth JM, Bozorgi P, Lebrón LM, Bills SE, Hazlett LJ, Carlos RC, King JC. Geographic availability of low-dose computed tomography for lung cancer screening in the United States, 2017. Prev Chronic Dis. 2018;15:E119.
Fedewa SA, Kazerooni EA, Studts JL, Smith RA, Bandi P, Sauer AG, et al. State variation in low-dose computed tomography scanning for lung cancer screening in the United States. J Natl Cancer Inst. 2021;113(8):1044–52.
Martin AN, Hassinger TE, Kozower BD, Camacho F, Anderson RT, Yao N. Disparities in lung cancer screening availability: lessons from Southwest virginia. Ann Thorac Surg. 2019;108(2):412–6.
Acknowledgements
The authors would like to acknowledge Sharon Chan for her contributions relating to reviewing background literature for the trial.
Funding
This work was funded by the following grants R01CA207442 (Drs. Ostroff and Shelley) and P30CA008748 (Craig B. Thompson, MD and Dr. Ostroff).
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: Conceptualization and methodology: ACi, JSO, DS, JCK, ACr; Data collection: ACi, RA, LC, ACr; Formal analysis: ES; Data analysis and interpretation: ACi, LC, JSO, JCK, DS; Writing – Original Draft: ACi, LC; Writing – Review and Editing: All Authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Memorial Sloan Kettering Cancer Center Institutional Review (IRB#17–500) serving as the single IRB for this multi-site clinical trial. All research was conducted in adherence with ethical standard of the responsible committee on human experimentation (institutional and national) and with Helsinki Declaration. Informed consent was obtained from all study participants prior to participation in study activities.
Consent for publication
Not applicable.
Competing interests
JSO has received royalties from Up-to-Date. The other co-authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ciupek, A., Chichester, LA., Acharya, R. et al. Utilizing a patient advocacy-led clinical network to engage diverse, community-based sites in implementation-effectiveness research. BMC Health Serv Res 24, 891 (2024). https://doi.org/10.1186/s12913-024-11376-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11376-3