Abstract
AURKA is an important protein in the regulation of G2 to M transition during mitosis. Due to this regulatory function, it has been hypothesized to be a potential cancer susceptibility gene. Two non-synonymous polymorphisms (F31I and V57I) have been associated with breast cancer risk in prior studies. We sought to confirm these findings in a large case control study nested within a prospective cohort, the Nurses' Health Study. Post-menopausal women who were homozygous for the 31I and 57V alleles had an increased risk of invasive breast cancer (OR 1.63, 95% CI 1.08–2.45). We also performed a meta-analysis to summarize the findings of this and prior studies of association between the F31I polymorphism and breast cancer risk (Summary OR 1.29, 95% CI 1.08–1.53, p-heterogeneity = 0.29). These results confirm prior findings that AURKA represents a low penetrance breast cancer susceptibility gene.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
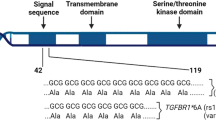
AURKA (STK15, Aurora kinase) is involved in cell cycle regulation, in particular the passage from G2 to M, through the formation of mitotic spindle formation [1]. While this gene is found to be amplified in many tumor types, including breast cancer [2], the loss of over expression of AURKA has been correlated with the transition of in situ to invasive ductal carcinoma [3].
Ewart-Toland et al. [4] found that the polymorphic Ile allele of F31I was more effective at transforming rat cells to a more malignant phenotype. This and other polymorphisms have been associated with breast cancer risk in four retrospective case-control studies (Table 1). Sun et al. found a significant increase in risk (OR 1.76, 95% CI 1.16-2.66) associated with the homozygous state of the Ile allele at the F31I (rs2273535) polymorphism of AURKA, while Dai et al. did not (OR 1.2, 95% CI 0.9-1.6), in hospital-based [5] and population-based [6] case-control studies of Han Chinese women. Lo et al. also did not observe a statistically significant (p=0.32 of association under an additive model) association between this polymorphism and breast cancer risk in a hospital based case-control study in Taiwan [7], however they did observe association between haplotypes of AURKA and breast cancer. It is interesting to note that the prevalence of the homozygous state of the Ile allele in Asian populations (~45%) is drastically different that that of Caucasians (~4%). Egan et al. described an increase in risk associated with a compound genotype of two non-synonymous polymorphisms, F31I and V57I (rs1047972), with individuals homozygous for the 31I and 57V alleles having a nearly 2-fold increase in risk of postmenopausal invasive breast cancer [8]. We studied these two polymorphisms in a case-control study nested within the prospective Nurses’ Health Study.
Materials and methods
Genotyping assays for the AURKA polymorphisms (F31I, rs2273535; and V57I, rs1047972) were performed by the 5′ nuclease assay (TaqMan) on the ABI Prism 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA). TaqMan primers, probes, and conditions for genotyping assays are available on request from the authors. Our study included a total of 1259 incident breast cancer cases (1021 invasive, 208 in situ and 30 unknown or undetermined histology) diagnosed after blood draw up to June 1, 2000, and 1742 matched controls, drawn from 32,826 women who gave a blood sample in 1989-90. Controls were randomly selected participants who were free of diagnosed cancer (except non-melanoma skin cancer), and matched to cases based on age, menopausal status, recent post-menopausal hormone use, and time, day, and month of blood collection. Greater than 95% of the samples were successfully genotyped on the first attempt, with samples that failed genotyping being removed from further analyses.
We used SAS v8.2 (SAS Institute, Cary, NC) for most statistical analyses. Odds ratios (OR) and 95% confidence intervals (CI) were calculated using both conditional and unconditional logistic regression, controlling for matching factors, age at menopause, age at menarche, age at first birth and parity, history of benign breast disease, and family history of breast cancer using PROC PHREG (conditional regression) and PROC LOGISTIC (unconditional regression). We tested for departures from Hardy-Weinberg equilibrium using PROC ALLELE. Interactions were tested by likelihood ratio tests comparing the model with main effects for each variable of interest to the model with the two variables cross-tabulated. Meta-analyses were conducted using the rmeta package in R 1.7.1. All p-values reported are two sided.
Results and discussion
Our results were similar to those observed by Egan et al. [8]. Meta-analyses of the prior studies (shown in Table 1) and our study show a significant increase in breast cancer risk for women homozygous for the I allele of F31I (Summary OR 1.28, 95% CI 1.08-1.53). The test of heterogeneity between studies was not significant (p = 0.29).
Both polymorphisms studied were in Hardy-Weinberg equilibrium in controls (p>0.41). There were no significant differences in risk estimates generated by conditional and unconditional models, and Table 2 reports those from the multivariate unconditional regressions. We observed a borderline significant association between homozygosity of the 31I allele and overall breast cancer risk (OR 1.40, 95% CI 0.97-2.02, Table 2). No statistically significant association was observed with the V57I polymorphism. When restricting our analyses to post-menopausal women, those homozygous for the 31I allele were at 57% increased risk of invasive breast cancer (OR 1.57, 95% CI 1.05-2.33, Table 2). Our results in combining the two genotypes are similar to those seen by examining the V31I allele alone. In analyses restricted to post-menopausal women, we found that women homozygous for both the 31I and 57V were at 63% increased risk of invasive breast cancer (OR 1.63, 95% CI 1.08-2.45, Table 2). We observed, a higher risk of invasive breast cancer in lean post-menopausal women homozygous for 31I (BMI < median of 25 kg/m2, OR 1.90; 95% CI 1.11-3.25), as opposed to heavier post-menopausal women (BMI ≥ median of 25 Kg/m2, OR 1.06; 95% CI 0.64-1.76).
Egan et al. had observed that heavier women were at increased risk with the 31I homozygous genotype when contrasted with leaner women. However, since neither the p-value for the interaction in our study (p=0.27) or theirs (p=0.99) was statistically significant between BMI and AURKA genotypes on breast cancer risk, these differences are most likely due to chance. In pre-menopausal women, Egan et al. observed a non-significant inverse association among women homozygous for the I allele at V57I (OR 0.38, 95% CI 0.14-1.07) which is very similar to our study (OR 0.35 95% CI 0.09-1.44). While neither study has large numbers of pre-menopausal women, the similarity between the two findings warrants examination in studies with larger numbers of pre-menopausal women. We observed no difference in the distribution of BMI or duration of menstruation (menarche to first birth or menopause in nulliparous women) between genotypes among cases or controls (data not shown). No differences in risk were observed upon stratification by history of benign breast disease, first degree family history of breast cancer, or estrogen/progesterone receptor status of tumors in the cases.
In conclusion, these polymorphisms in the AURKA gene appear to be associated with an increase in breast cancer risk, which is similar in both Caucasian and Asian populations. This increase in risk is independent of established hormone related risk factors for breast cancer.
References
EA Nigg (2002) ArticleTitleCentrosome aberrations: cause or consequence of cancer progression? Nat Rev Cancer 2 815–825 Occurrence Handle1:CAS:528:DC%2BD38Xotlert70%3D Occurrence Handle12415252 Occurrence Handle10.1038/nrc924
H Zhou J Kuang L Zhong et al. (1998) ArticleTitleTumour amplified kinase STK15/BTAK induces centrosome amplification, aneuploidy and transformation Nat Genet 20 189–193 Occurrence Handle1:CAS:528:DyaK1cXms1eis78%3D Occurrence Handle9771714 Occurrence Handle10.1038/2496
A Hoque J Carter W Xia et al. (2003) ArticleTitleLoss of aurora A/STK15/BTAK overexpression correlates with transition of in situ to invasive ductal carcinoma of the breast Cancer Epidemiol Biomarkers Prev 12 1518–1522 Occurrence Handle1:CAS:528:DC%2BD3sXhtVSqs7vM Occurrence Handle14693746
A Ewart-Toland P Briassouli JP Koning Particlede et al. (2003) ArticleTitleIdentification of Stk6/STK15 as a candidate low-penetrance tumor-susceptibility gene in mouse and human Nat Genet 34 403–412 Occurrence Handle1:CAS:528:DC%2BD3sXmt1Skurc%3D Occurrence Handle12881723 Occurrence Handle10.1038/ng1220
T Sun X Miao J Wang et al. (2004) ArticleTitleFunctional Phe31Ile polymorphism in Aurora A and risk of breast carcinoma Carcinogenesis 25 2225–2230 Occurrence Handle1:CAS:528:DC%2BD2cXhtVWgs73F Occurrence Handle15271856 Occurrence Handle10.1093/carcin/bgh244
Q Dai QY Cai XO Shu et al. (2004) ArticleTitleSynergistic effects of STK15 gene polymorphisms and endogenous estrogen exposure in the risk of breast cancer Cancer Epidemiol Biomarkers Prev 13 2065–2070 Occurrence Handle1:CAS:528:DC%2BD2cXhtVOjsLvL Occurrence Handle15598762
YL Lo JC Yu ST Chen et al. (2005) ArticleTitleBreast cancer risk associated with genotypic polymorphism of the mitosis-regulating gene Aurora-A/STK15/BTAK Int J Cancer 115 276–283 Occurrence Handle1:CAS:528:DC%2BD2MXjvFWjsL4%3D Occurrence Handle15688402 Occurrence Handle10.1002/ijc.20855
KM Egan PA Newcomb CB Ambrosone et al. (2004) ArticleTitleSTK15 polymorphism and breast cancer risk in a population-based study Carcinogenesis 25 2149–2153 Occurrence Handle1:CAS:528:DC%2BD2cXhtVWgs7zF Occurrence Handle15271853 Occurrence Handle10.1093/carcin/bgh231
Acknowledgements
We would like to thank Patrice Soule and her laboratory for sample preparation, and Dr. Hardeep Ranu and her laboratory for genotyping and data management. We are indebted to the participants in the Nurses' Health Study for their continuing dedication and commitment. Supported by National Institutes of Health research grants CA87969, CA49449 and CA65725. D.G.C. is supported by training grant CA 09001-27 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cox, D.G., Hankinson, S.E. & Hunter, D.J. Polymorphisms of the AURKA (STK15/Aurora Kinase) Gene and Breast Cancer Risk (United States). Cancer Causes Control 17, 81–83 (2006). https://doi.org/10.1007/s10552-005-0429-9
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10552-005-0429-9