Abstract
Aim
Second ipsilateral breast tumor event (2ndIBTE) occurring after primary radio-surgical treatment can be treated by either salvage mastectomy or 2nd conservative treatment (2ndCT) including an accelerated partial breast re-irradiation (APBrI). We analyzed the impact of the GEC-ESTRO APBI classification (GAC) on the oncological outcome after APBrI.
Materials and methods
Between 2000 and 2016, 159 patients (pts) underwent a 2ndCT. After lumpectomy, APBrI was performed using either low-dose (30–55 Gy reference isodose) or high-dose rate brachytherapy (28–34 Gy). Oncological outcome including 3rdIBTE, regional (RFS) or metastasis-free survival (MFS), specific (SS) and overall survival (OS) was analyzed according to GAC. Univariate (UVA) and multivariate analyses (MVA) were conducted to identify significant prognostic factors for 3rdIBTE.
Results
With a median follow-up of 71 months (range 62–85 months), 60 pts (42%), 61 pts (42.7%) and 22 pts (15.4%) were classified as low-risk (LR), intermediate-risk (IR) and high-risk (HR), respectively. For the whole cohort, 6-year 3rdIBTE-free survival, RFS, MFS, SS and OS rates were 97.4, 96.4, 90.3, 92.9 and 91.2%, respectively. Six-year 3rdIBTE-free survival rates for LR, IR and HR were 100, 95.8 and 92.9%, respectively (p = 0.003), while no significant differences were found between the three GAC groups for RFS, MFS, SS. In UVA, lympho-vascular invasion (p = 0.009), positive margins (p = 0.0001) and GAC high-risk group (p = 0.001) were considered as significant prognostic factors for 3rdIBTE, while, in MVA, high-risk group (p = 0.009) was the only prognostic factor.
Conclusion
In case of 2ndIBTE, GAC could be used as a decision helping tool to discuss conservative or radical treatment options. Patient information remains crucial in order to accurately define the salvage therapy modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a major matter of public health with a worldwide incidence of 1,671,149 patients (pts) in 2012 [1]. With an increasing incidence rate of early stage breast cancer of 250 per 100,000 women, localized breast cancer surgical management has been constantly evolving, from mutilating mastectomy, which was the gold standard until late 80s, to radio-surgical conservative treatment [2].
The 20-year cumulative incidence rate of 2nd ipsilateral breast tumor event (2ndIBTE) after a first conservative radio-surgical treatment is around 15%, raising the question of standard of care regarding this specific subpopulation [3]. For decades, salvage mastectomy (SM) has been considered as the only therapeutic alternative although second conservative treatment (2ndCT) concept has been introduced since the beginning of the 80s, which consists of a surgical lumpectomy with or without re-irradiation of the tumor bed [4, 5]. The Breast Cancer Working Group of the Groupe Européen de Curiethérapie of the European Society for Radiotherapy and Oncology (GEC-ESTRO) reported the results of a cohort of 217 pts who underwent 2ndCT combining lumpectomy plus interstitial brachytherapy. The 5-year 2nd local recurrence rate was 5.6%, with 11% of grade 3–4 late toxicities [6].
As of today, the choice between 2ndCT and SM remains under debate but both options can be discussed with the patient. Basically, facing to a 2ndIBTE, the first step is to consider the guidelines regarding the tumor features: if there is an indication of mastectomy (which remains the same whether it is a 1st or a 2ndIBTE), 2ndCT is definitely ruled out. If SM is not mandatory, technical feasibility of a 2ndCT has to be evaluated. Indeed, the clinical consequences of the first surgery and irradiation, the total dose, the resultant breast size and the cosmetic impact have to be taken into consideration. Nevertheless, the patient’s choice remains crucial and the majority of the patients want to avoid as much as possible a mutilating salvage surgery with or without breast reconstruction [7].
Currently, the treatment decision is mainly based on these factors. Little data are provided by the literature for helping patients and physicians in the decision making process. GEC-ESTRO and American Society for Radiation Oncology (ASTRO) proposed accelerated partial breast irradiation (ABPI) classifications based on three groups representing graduate local-recurrence risk [8,9,10]. Those APBI classifications were initially used to discuss (or not) a shorter adjuvant irradiation for primary tumor. In order to make the salvage decision process more accurate, we proposed to evaluate the impact of ABPI classifications applied to 2ndIBTE.
The aim of this study was to determine whether the oncological outcome of patients presenting a 2ndIBTE could be impacted by their affiliation to an APBI classification group.
Material and method
This observational, single-center, retrospective study was performed in the Antoine Lacassagne Center in Nice, France, from 2000 to 2017. Data were collected from patients’ files. Third IBTE was considered as primary end-point, while the following items were considered as secondary end-points: regional recurrence occurring in the ipsilateral axillary area (regional-free survival—RFS); distant metastasis rates (metastasis-free survival—MFS); specific (SS) and overall survival (OS) rates. This study was approved by the local ethics committee.
Patient features
Target population were women who presented a 2ndIBTE occurring after a radio-surgical conservative treatment performed for the primary tumor. Second IBTE was considered as a local event occurring within the pre-treated breast at least 1 year after the 1stIBTE, excluding in-breast skin and/or sub-cutaneous metastatic diseases. A second conservative treatment (2ndCT) combining salvage lumpectomy plus accelerated partial breast re-irradiation (APBrI) was proposed consisting in multicatheter interstitial brachytherapy (MIB) using either low (LDR) or high-dose rate (HDR).
Except for patient with a formal indication of salvage mastectomy (histological factors, major late breast tissue toxicity induced by the first radio-surgical treatment, breast size, or patient’s wish), 2ndCT was proposed as an alternative for patients who were reluctant to radical salvage surgery, irrespective of the APBI classification groups. Consequently, patients with poor prognostic factors (lympho-vascular involvement, extensive intra-ductal component, high Ki 67, poor histological differentiation…) were also considered as eligible candidates for 2ndCT with APBrI.
All patients received detailed information concerning the risks and benefits of this salvage treatment procedure.
Treatment features
The 2ndCT process has already been described [11]. Briefly, it consisted in a lumpectomy with four clips clamped into the lumpectomy cavity and one on the pectoralis muscle. Axillary lymph node assessment was not performed for patient who already underwent axillary dissection at the time of primary treatment.
Vector implantation for MIB was performed pre- or post-operatively following the Paris System geometric recommendations [12, 13].
For LDR brachytherapy (pre-operative implant), the majority of the implants were performed in two planes (75% out of 27 pts). For the delineation of the CTV, a target volume corresponding to the margin resection of the cavity adding a 2-cm radial security margin was selected, with a distance between catheters of 1–1.5 cm. Moreover, a minimal distance of 0.5 cm regarding the skin and the ribs was applied, to minimize the risk of skin toxicity and pathological rib fracture, respectively. About 5 days after the surgery, catheters were loaded by 192Ir wires. Treatment planes were obtained from two orthogonal X-ray films, while the dose was prescribed on the 85% of the reference isodose calculated on the central plane. The prescribed dose ranged from 30 to 55 Gy (88% of the patients received a dose ranged between 40 and 50 Gy).
For HDR brachytherapy, the number of planes varied from 1 to 4. The implant was performed under local anesthesia, in case of post-operative procedure. A post-implant CT was performed the day after surgery. The CTV delineation consisted in an expansion of 1 cm around the clips. The dose distribution was optimized manually by varying time and stop position of the radio-active source. The prescribed dose to the CTV fluctuated between 28 and 34 Gy in 8–10 fractions, twice daily (61% of the patients received 34 Gy), delivered over 5 consecutive days, during an ambulatory procedure.
Adjuvant treatments (hormonal therapy, chemotherapy, or anti-HER2-targeted therapy) were used according to our center guidelines.
Accelerated partial breast irradiation classification groups
In order to perform a reproducible analysis, both GEC-ESTRO [8] and ASTRO [10] APBI classifications were used. However, due to the lack of axillary lymph node re-staging for the large majority of the patients, the N-status was not considered as prognostic criteria and excluded from the analysis. Indeed, if pNx status was considered, most of the patients would fall into the “high-risk” or “unsuitable” group for GEC-ESTRO and ASTRO APBI classifications, respectively. GEC-ESTRO and ASTRO APBI classifications were evaluated separately.
Follow-up
Patients were systematically examined by the radiation oncologist one month after brachytherapy to evaluate early toxicity. Then, patients were seen every 6 months by the surgeon, the medical or radiation oncologist with a clinical examination. Late toxicities evaluation used the Common Classification for Adverse Events 4.0. Cosmetic results were reported by the radiation oncologist and/or the surgeon using a cosmetic score derived from the scoring system described by Harris et al. [14]: excellent, good, fair and poor. Radiologic surveillance was yearly investigated by mammogram with or without breast ultrasonography examination.
Statistical analysis
Description of the study population and of the different investigated parameters was made using absolute and relative frequencies for the qualitative data and summarized using descriptive statistics such as median, extreme for quantitative data. Statistical comparisons were performed using the χ2 test for qualitative data and non-parametric matched pairs Wilcoxon test for quantitative data. Overall survival (OS) was defined by the interval between the date of 2nd surgery and death due to any cause/to the disease. Specific survival (SS) was defined by the time between the date of 2nd surgery and death due to breast cancer. Third IBTE-free survival, regional-free survival (3rdIBTE-FS), regional-free survival (RFS) and metastasis-free survival (MFS) were calculated between the date of 2nd surgery and these respective events and were estimated using the Kaplan–Meier method. Patients still alive at the last visit were censored at the date of last follow-up. Median follow-up with 95% confidence intervals was calculated by reverse Kaplan–Meier method. In univariate analysis, the survival curves were compared using the log-rank test. In multivariable analysis, association between several parameters and 3rdIBTE-free survival was expressed as a hazard ratio with a 95% confidence interval, which was estimated with the use of a Cox proportional-hazards model. Collinearity between variables entered in the model was evaluated using the ‘r’ Pearson correlation coefficient. If r > 0.40, one of the two variables was considered as redundant and had to be removed from the model. Proportional hazards were verified for all entered variables. All p values inferior to 0.05 (two-sided) were considered statistically significant. Data were entered and stored on a Microsoft Excel® file. All statistical analyses were performed in 5% alpha risk using R.3.2.2 software on Windows®.
Results
Patient and tumor features
Between 2000 and 2017, 159 patients (pts) presented a 2ndIBTE and underwent a 2ndCT. Among them, 143 pts were analyzed in order to respect a minimum follow-up of 24 months for the last included patient.
The median time interval between surgery for the primary and salvage lumpectomy was 13.8 years (1.6–35.3). Patient features for primary and 2ndIBTE are summarized in Table 1. Median age was 52 years (24–83) and 66 years (31–90) for primary and 2ndIBTE, respectively. Primary tumors were mostly adenocarcinomas (79%), a size smaller than 20 mm (74%), grade 2 (47%), positive hormonal receptor status (86.9%). Some data concerning histological factors (Ki67, Her2 status…) are missing due to the date of the first event. All the patients underwent adjuvant whole breast irradiation (WBI) with a median delivered dose of 53.8 Gy (45–66). Second IBTE occurred in or close to the primary tumor quadrant in 51.6% and 33.6%, respectively. For 2ndIBTE, histology was invasive ductal carcinoma for 113 pts (79%), tumor size smaller than 20 mm for 123 pts (86%), histological grade 2 for 65 pts (48%), positive hormonal receptor status for 121 pts (91.6%) and non-overexpressed HER2 status for 121 pts (95.3%). Negative margin dissection was achieved in 91%, while lympho-vascular invasions were observed in 9%.
Concerning systemic treatments, in ad equation with the histological features, most of the patients underwent endocrine treatment (82%). Adjuvant chemotherapy was used in 11%, while Trastuzumab was prescribed in 2.8%.
Oncological outcome
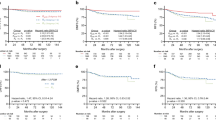
For the whole cohort, the median follow-up was 71 months (62–85 months). Six patients developed a 3rdIBTE after 2ndCT leading to a 6-year 3rdIBTE-free survival rate of 97.4% (0.94–1) (Fig. 1). Six-year RFS, MFS, SS and OS rates were 96.4, 90.3, 92.9 and 91.2%, respectively (Figs. 2, 3). Four patients presented a regional recurrence, and distant metastatic progression was observed for 12 patients (36 months after 2ndCT for 10 pts). Oncological outcome (mainly in terms of 3rd IBTE) was not significantly impacted by the brachytherapy dose rate (2/27 and 4/116 for LDR and HDR, respectively).
According to the APBI GEC-ESTRO classification, 60 pts (42%), 61 pts (43%) and 22 pts (15%) were classified as low-, intermediate- and high-risk groups. Using the ASTRO 2016 classification, suitable and cautionary patient groups represented 43% and 42%, respectively (unsuitable group 15%). For the GEC-ESTRO classification, 6-year 3rdIBTE-free survival rates were 100, 95.8 and 92.9%, respectively, for low-, intermediate- and high-risk groups (p = 0.003). For the ASTRO classification, 6-year 3rdIBTE free survival rates were 100, 96.2 and 92.9%, respectively, for suitable, cautionary and unsuitable risk groups (p = 0.004). No significant differences were observed in terms of RFS, MFS, SS and OS between the three APBI risk groups (Table 2). Among the six patients who presented a 3rdIBTE, 5 pts belonged to the high-risk/unsuitable group while the remaining patient was classified as intermediate risk/cautionary (Table 3). The features of the 3rdIBTEs are summarized in Table 3. For the whole cohort, one patient presented a 3rdIBTE at 54 months. Primary tumor (1stIBTE) was an invasive ductal carcinoma, while the 2ndIBTE occurred 146 months later with an invasive ductal carcinoma associated with lympho-vascular invasion and positive surgical margins. Third IBTE was an invasive ductal carcinoma. All of the three breast events appeared in the same area. This patient belonged to the high-risk/unsuitable group. A second patient had a 3rdIBTE 71 months after the 2ndIBTE. The three tumors were invasive lobular carcinoma (time interval between 1st and 2ndIBTE = 62 months). They were all localized in the same quadrant. A bifocal tumor was observed on the 2ndIBTE lumpectomy specimen. The 3rdIBTE was still bifocal. This patient belonged to the intermediate-risk/cautionary group. Four others 3rdIBTE (high-risk/unsuitable group) were observed at 83, 92, 93 and 114 months.
In order to find significant prognostic factors for 3rdIBTE, different variables related to the 2ndIBTE were analyzed in univariate analysis (age, tumor size, histological grade, margin status, lympho-vascular invasion, ki67, ABPI-risk group and time interval between 1st and 2nd surgery). Lympho-vascular invasion (p = 0.009), positive margins (p = 0.0001) and high-risk/unsuitable group of the ABPI classification (p = 0.001) were the three significant prognostic factors for 3rdIBTE. In multivariate analysis, high-risk/unsuitable ABPI group was the only significant prognosis factor for 3rdIBTE (p = 0.009), leading to consider that patients belonging to the high-risk group have a 9.66 relative risk for developing a 3rdIBTE.
Toxicity profile
Among the 143 pts, the maximum complication rate observed after 2ndCT (at the last follow-up) was 33% (47 pts), 26% (37 pts), 2.8% (4 pts) and 0.7% (1 pt) for grades 1, 2, 3 and 4, respectively. The observed complications consisted mainly in cutaneous (32.5%) and sub-cutaneous fibrosis (30.1%), while telangiectasia (8.4%) and hyper-pigmentation (17%) were less frequent. One patient presented grade 4 ulceration. Regarding cosmetic outcome, excellent/good result was noticed for 122 pts (85%), while poor result was observed for 6 pts (4.6%). Excellent cosmetic results were obtained for 62% and 74% for HDR and LDR cohort, respectively.
Discussion
The treatment choice in case of 2ndIBTE has been under debate for the past few years, with no clear established guidelines. Salvage mastectomy was the historical treatment, based on retrospective and comparative series. With the emergence of conservative treatment for primary breast tumor, the possibility of a second breast preservation progressively gained interest [4].
As an analogy to the essential role of adjuvant radiotherapy after breast conservative treatment for primary tumors, the concept of adjuvant re-irradiation of the tumor bed after salvage lumpectomy became a mandatory part of the 2ndCT [3, 15]. To our knowledge, there has been no phase III trial comparing SM versus 2ndCT and the likelihood of the emergence of such a trial remains quite uncertain because of methodological and ethical considerations [16]. Based on several old comparative series, the 3rdIBTE after SM is about 10–15% (ranging from 3 to 32%) with equivalent results obtained after 2ndCT + APBrI [15]. More recently, the GEC-ESTRO Breast Cancer Working Group reported the results of salvage lumpectomy + APBrI with 3rdIBTE actuarial rates at 5 and 10 years of 5.6% and 7.2%, respectively [6]. The choice between those two salvage treatments, which seems to achieve comparable local control, is mainly based on histopathological factors. If they lead to consider a SM, a 2ndCT must be ruled out. On the other hand, in the absence of bad histopathological prognosis factors, breast size after the primary conservative treatment and the cutaneous and subcutaneous consequences of the first irradiation should be taken into account in order to discuss a 2ndCT + APBrI (Fig. 4). Finally, the patient’s choice remains crucial after a full and detailed explanation of the risk and benefits of each salvage treatment.
In our study, regarding the oncological outcomes of the whole cohort, the 6-year 3rdIBTE-FS, RFS, MFS, SS and OS rates were 97.4, 96.4, 90.3, 92.9 and 91.2%, respectively. In Guix et al. study, 36 pts who presented a 2ndIBTE (mainly stages I and II) underwent a 2ndCT (salvage lumpectomy + HDR-MIB APBrI) [17]. The authors reported a 10-year local control rate of 89.4% with a 10-year overall survival rate of 96.7%. The GEC-ESTRO study reported a similar local control with a 5-year actuarial 3rdIBTE-free survival rate of 94.4% [6]. The authors reported 5-year actuarial MFS, SS and OS rates of 88.9, 90.5 and 88.7%, respectively, which were quite similar to our results after 6 years of follow-up.
In these two studies, the re-irradiation of the tumor bed was performed with multicatheter interstitial brachytherapy based on LDR or HDR which remains currently the most approved re-irradiation technique. However, different APBrI techniques have been described [18,19,20,21,22]. Trombetta et al. reported the results of a cohort of 18 pts with a 2ndIBTE who underwent a 2ndCT combining salvage lumpectomy plus a balloon-device based brachytherapy (34 Gy in 10 fractions over 5 days). After a median follow-up of 39.6 months, the authors observed 11% of 3rdIBTE [18]. Intraoperative 50 kv X-ray radiotherapy (IORT) has also been investigated. Kraus-Tiefenbacher et al. performed IORT for 17 pts and reported, after a median follow-up of 37 months, 11.7% of 3rdIBTE [19]. In the same way, Ching et al. observed a 3rdIBTE-FS rate of 100% in a small cohort of 12 pts (MFU: 14 months) [20]. More recently, using 50 kv IORT APBrI technique, Thangarajah et al. presented encouraging results in a cohort of 41 pts (MFU close to 5 years) with a rate of 3rdIBTE-FS close to 90% [21]. Electron beam IORT APBrI was investigated by Blandino et al. who treated 29 pts with a 5-year local control rate of 92.3% [22]. Recently, the oncological outcome and toxicity results of the RTOG1014 prospective trial were reported at the 2018 ASTRO meeting. In this protocol, APBrI used a 3D conformational external beam radiation technique delivering a total dose of 45 Gy in 15 fractions (twice daily). In a cohort of 65 pts with a median follow-up of 3.64 year, the authors observed a 2nd breast conservation rate, DMFS and OS of 94.8% with 6.9% of late grade 3 treatment-related complication rate.
Regarding the oncological outcome according to the GEC-ESTRO APBI classification, we reported 6-year 3rdIBTE-free survival rates of 100, 95.8 and 92.9% for low-, intermediate- and high-risk groups, respectively. The GEC-ESTRO APBI phase III compared WBI versus APBI for selected primary early-stage breast cancer (low- and intermediate-risk groups) [23]. The authors reported a 5-year local relapse rate (2ndIBTE) of 1.44% which appears quite comparable with our 2ndCT results (no and only one 3rdIBTE for low- and intermediate-risk patient, respectively). Those results lead to consider that, in case of low- and intermediate-risk breast cancer, lumpectomy plus MIB-APBI achieve excellent local control rates whatever the status of breast tumor (primary or 2ndIBTE). Moreover, recently at the 2018 ASTRO annual meeting, the GEC-ESTRO reported the results of a propensity score-matched analysis comparing SM (215 pts) versus 2nd CT (215 pts) using MIB. With a MFU of 65 months, no significant difference was observed between the two salvage treatments in terms of DFS, OS, MSF or 3rd IBTE.
For high-risk group patients, we reported a 6-year 3rdIBTE-free survival rate of 92.9% significantly lower compared to low- and intermediate-risk groups (p = 0.003) while the relative risk of 3rdIBTE was 9.66. This sub-group of patients tends to have a more aggressive disease (positive margins, lympho-vascular involvement, extensive DCIS, multifocality or large tumor size …) leading to consider 2ndCT for high-risk group with caution. However, if for 1stIBTE high-risk patients, the recommendation would be WBI instead of APBI, in case of 2ndIBTE, a mutilating treatment (SM) should be discussed as the only alternative to a 2ndCT. Actually, Lee et al. described the deleterious impact of mastectomy (even with a surgical reconstruction) regarding body image, self-confidence and quality of life [7, 24]. Mastectomy was even associated with a higher rate of unemployment [25]. Therefore, in case of 2ndIBTE and mainly for high-risk group patients, discussion and information given to the patient regarding treatment options and their potential outcomes is crucial. An indication of 2ndCT must also be carefully examined regarding patients with lympho-vascular involvement and positive surgical margins, which appeared to be prognosis factor for a 3rdIBTE in univariate analysis.
Overall survival results of the whole cohort are encouraging with a 6-year OS rate of 91.2%, with a 6-year MFS and SS rates of 90.3% and 92.9%, respectively. While these results are comparable to the 5-year OS (88.9%), MFS (90.5%) and SS (88.7%) rates reported in the 2ndCT GEC-ESTRO study [6], 5-year OS for low- and intermediate-risk primary tumor reported in the GEC-ESTRO APBI phase III trial, appear higher (97.3%) [23]. In our study, most of the patient who presented a metastatic diffusion belonged to the low-risk group with a 6-year MFS of 85.3, 93.1 and 95.2% for low-, intermediate- and high-risk groups, respectively. In the low-risk group, all the metastatic patients (8 pts) displayed systemic disease during the first 48 months of follow-up and 50% (4 pts) within the first 2 years. The mechanism of these early relapses in low-risk patients is not clearly elucidated and needs to be analyzed in a larger cohort.
Our study presents some weaknesses such as its retrospective nature, the limited number of patients and follow-up, which limit the analysis of the oncological outcome especially for low-risk patients in terms of MFS. However, according to our knowledge, this is the first analysis of the use of APBI classification in the therapeutic decision process in case on 2ndIBTE.
Conclusion
When considering 2ndIBTE, the debate still remains on how to consider this event: true recurrence of the 1stIBTE or a new (independent) event? The concordance of the local control rates for low- and intermediate-risk groups, reported by the GEC-ESTRO APBI phase III (primary tumor) and ours (2ndIBTE) suggests that the question appears less crucial regarding local outcome while the control of systemic disease remains a critical issue.
In case of 2ndIBTE, a second conservative treatment with MIB-APBrI can be proposed as a safe and efficient alternative to salvage mastectomy. In order to refine the therapeutic decision, the GEC-ESTRO APBI classification could be used as a potential decision making and prognosis tool for second conservative treatment while patient information remains fundamental mainly for high-risk patients.
References
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J et al (2015) Reprint of: cancer incidence and mortality patterns in Europe: Estimates for 40 countries in 2012. Eur J Cancer 51:1201–1202
Bleyer A, Welch HG (2013) Effect of three decades of screening mammography on breast-cancer incidence: editorial comment. Obstet Gynecol Surv 68:440–442
Fisher B, Anderson S, Bryant J et al (2002) Twenty-year follow-up of a randomized trial comparing total for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241
Kurtz JM, Amalric R, Brandone H et al (1988) Results of wide excision for mammary recurrence after breast-conserving therapy. Cancer 61:1969–1972
Maulard C, Housset M, Brunel P et al (1995) Use of perioperative or split-course interstitial brachytherapy techniques for salvage irradiation of isolated local recurrences after conservative management of breast cancer. Am J Clin Oncol 18:348–352
Hannoun-Levi JM, Resch A, Gal J et al (2013) Accelerated partial breast irradiation with interstitial brachytherapy as second conservative treatment for ipsilateral breast tumour recurrence: multicentric study of the GEC-ESTRO Breast Cancer Working Group. Radiother Oncol 108:226–231
Lee CNH, Pignone MP, Deal AM et al (2018) Accuracy of predictions of patients with breast cancer of future well-being after immediate breast reconstruction. JAMA Surg. https://doi.org/10.1001/jamasurg.2017.6112
Polgár C, Van Limbergen E, Pötter R et al (2010) Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group. Radiother Oncol 94:264–273
Smith BD, Arthur DW, Buchholz TA et al (2009) Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO). Int J Radiat Oncol Biol Phys 74:987–1001
Correa C, Harris EE, Leonardi MC et al (2017) Accelerated partial breast irradiation: executive summary for the update of an ASTRO evidence-based consensus statement. Pract Radiat Oncol 7:73–79
Hannoun-Levi JM, Castelli J, Plesu A et al (2011) Second conservative treatment for ipsilateral breast cancer recurrence using high-dose rate interstitial brachytherapy: preliminary clinical results and evaluation of patient satisfaction. Brachytherapy 10:171–177
Chassagne D, Dutreix A, Ash D et al (1997) Introduction. J Int Comm Radiat Units Meas os30:1. https://doi.org/10.1093/jicru/os30.1.1
Gahbauer R, Landberg T, Chavaudra J et al (2004) References. J ICRU 4:95–100
Harris JR, Levene MB, Svensson G, Hellman S (1979) Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys 5:257–261
Hannoun-Levi J-M, Ihrai T, Courdi A (2013) Local treatment options for ipsilateral breast tumour recurrence. Cancer Treat Rev 39:737–741
Trombetta M, Hannoun-Levi JM (2017) Treatment of second ipsilateral breast tumor event: a need for a new type of evidence for avoiding mastectomy. Eur J Surg Oncol 43:849–850
Guix B, Lejárcegui JA, Tello JI et al (2010) Exeresis and brachytherapy as salvage treatment for local recurrence after conservative treatment for breast cancer: results of a ten-year pilot study. Int J Radiat Oncol Biol Phys 78:804–810
Trombetta M, Hall M, Julian TB (2014) Long-term followup of breast preservation by re-excision and balloon brachytherapy after ipsilateral breast tumor recurrence. Brachytherapy 13:488–492
Kraus-Tiefenbacher U, Bauer L, Scheda A et al (2007) Intraoperative radiotherapy (IORT) is an option for patients with localized breast recurrences after previous external-beam radiotherapy. BMC Cancer 7:1–7
Thangarajah F, Heilmann J, Malter W et al (2018) Breast conserving surgery in combination with intraoperative radiotherapy after previous external beam therapy: an option to avoid mastectomy. Breast Cancer Res Treat 168:739–744
Chin C, Jadeja P, Taback B et al (2017) Evaluation of partial breast reirradiation with intraoperative radiotherapy after prior thoracic radiation: a single-institution report of outcomes and toxicity. Front Oncol 7:1–6
Blandino G, Guenzi M, Belgioia L et al (2017) Adjuvant intraoperative radiotherapy for selected breast cancers in previously irradiated women: evidence for excellent feasibility and favorable outcomes. Reports Pract Oncol Radiother 22:277–283
Strnad V, Ott OJ, Hildebrandt G et al (2016) 5-year results of accelerated partial breast irradiation using sole interstitial multicatheter brachytherapy versus whole-breast irradiation with boost after breast-conserving surgery for low-risk invasive and in situ carcinoma of the female breast: a ran. Lancet 387:229–238
Lee CNH, Deal AM, Huh R et al (2017) Quality of patient decisions about breast reconstruction after mastectomy. JAMA Surg 152:741–748
Wang L, Hong BY, Kennedy SA et al (2018) Predictors of unemployment after breast cancer surgery: a systematic review and meta-analysis of observational studies. J Clin Oncol 36:1868–1879
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JMHL is consultant for BEBIG Company. The other co-authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Antoine Lacassagne Cancer Center ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was performed according to the current French laws.
Rights and permissions
About this article
Cite this article
Montagne, L., Gal, J., Chand, ME. et al. GEC-ESTRO APBI classification as a decision-making tool for the management of 2nd ipsilateral breast tumor event. Breast Cancer Res Treat 176, 149–157 (2019). https://doi.org/10.1007/s10549-019-05221-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05221-z