Abstract
Purpose
The phase 3 MONALEESA-2 study demonstrated that addition of ribociclib (RIB) to letrozole (LET) significantly improved progression-free survival (PFS) in patients (pts) with hormone receptor-positive (HR+), HER2-negative (HER2−) advanced breast cancer (ABC). Here, we evaluated duration of response (DoR), tumor shrinkage, PFS by treatment-free interval (TFI), and health-related quality of life (HRQoL).
Methods
Postmenopausal women (N = 668) with HR+ , HER2− ABC and no prior systemic therapy for ABC were randomized to RIB (600 mg/day; 3 weeks on/1 week off) plus LET (2.5 mg/day; continuous) or placebo (PBO) plus LET. Primary end point was PFS; HRQoL was the secondary end point; DoR was exploratory end point and PFS by TFI was post hoc analysis.
Results
Of 501 pts with measurable disease and confirmed complete or partial response, median DoR was 26.7 months (95% CI, 24.0–NR) in the RIB arm versus 18.6 months (95% CI, 14.8–23.1) in the PBO arm. At 8 weeks, more pts in the RIB arm (32%) versus the PBO arm (17%) experienced best percentage change ≥ 60%. The average pain reduction was greater in the RIB arm (26%) versus the PBO arm (15%). PFS benefit was seen with RIB vs PBO, irrespective of TFI.
Conclusion
RIB plus LET versus PBO plus LET is associated with earlier and more durable tumor response, greater degree of tumor shrinkage and pain reduction, and PFS benefit irrespective of TFI. These data further support RIB plus LET as a first-line treatment option for postmenopausal women with HR+ , HER2− ABC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hormone receptor-positive (HR+) tumors are the most common subtype of breast cancer, constituting 75% of all breast cancers [1, 2]. Endocrine therapy (ET)-based regimens are the cornerstone of treatment in patients with HR+ , human epidermal growth factor receptor 2-negative (HER2−) advanced breast cancer (ABC) [3]. However, de novo or acquired endocrine resistance leads to tumor recurrence and approximately 50% of patients with advanced disease do not respond to first-line treatment with endocrine therapy [4,5,6]. Several mechanisms are implicated in ET resistance in HR+ breast cancer [7, 8]. The cyclin D–cyclin-dependent kinases 4 and 6 (CDK4/6)–inhibitor of CDK4 (INK4)–retinoblastoma tumor suppressor protein (Rb) pathway induction has been identified as one of the most common mechanisms of ET resistance and poor clinical outcome in HR+ ABC [9]. The inhibition of cyclin D–CDK4/6–INK4–Rb pathway has improved outcomes for HR+ , HER2− ABC, in both first-line and in patients whose disease had progressed after ET [10,11,12,13].
Ribociclib (LEE011) is an orally bioavailable, selective small-molecule inhibitor of CDK4 and CDK6 that blocks the phosphorylation of retinoblastoma protein, thereby preventing cell-cycle progression and inducing G1 phase arrest [14]. Ribociclib has demonstrated promising antitumor activity in xenograft models of estrogen receptor-positive (ER+) breast cancer as a single agent and in combination with letrozole and phosphatidylinositol 3-kinase (PI3K) inhibitors [15]. In a phase 1b study of postmenopausal women with ER+ , HER2− ABC, ribociclib had an acceptable safety profile and showed signs of clinical activity in combination with letrozole, particularly in patients who had received no previous systemic treatment for advanced disease, with an overall response rate of 46% and a clinical benefit rate of 79% among patients with measurable disease [16].
A planned interim analysis of the phase 3 Mammary Oncology Assessment of LEE011′s (ribociclib’s) Efficacy and Safety (MONALEESA-2) study (NCT01958021; data cutoff January 29, 2016) demonstrated that addition of ribociclib to letrozole significantly improved progression-free survival (PFS) in postmenopausal women with HR+ , HER2− ABC [hazard ratio, 0.56; 95% confidence interval (CI), 0.43–0.72; P = 3.29 × 10−6] [17]. At an updated analysis, after 26.4 months of follow-up, treatment benefit with ribociclib was maintained [18]. The overall response rate was 43 versus 29% for all patients treated with ribociclib plus letrozole versus placebo + letrozole and 55 versus 39% for those with measurable disease, respectively [18].
Change in tumor burden is considered as a likely predictor of long-term outcome in patients with advanced cancer, and tumor shrinkage may be associated with improved quality of life [19]. Delayed deterioration in global QoL and pain symptoms correspond with a delay in disease progression [13]. Additionally, the treatment-free interval (TFI) has been reported as a prognostic factor and predictive marker of benefit of next treatment line across various tumors [20]. Recently reported results from a TFI analysis of abemaciclib suggest that TFI could be a potential clinical factor to determine patient subgroups who may derive benefit in patients with HR+ , HER2− ABC [21].
Here, we present the health-related quality of life (HRQoL) outcomes in patients from the MONALEESA-2 trial as well as results from preplanned exploratory analyses which evaluated tumor response and post hoc analysis of impact of TFI on PFS.
Patients and methods
Study design and participants
MONALEESA-2 (NCT01958021) is a phase 3, randomized, double-blind, international trial that enrolled postmenopausal women with HR+ , HER2− ABC who had received no prior systemic therapy for advanced disease from 223 centers in 29 countries worldwide [17]. Details of the study and participants have been reported previously [17]. Patients were required to have measurable disease with at least 1 measurable lesion as per response evaluation criteria in solid tumors (RECIST) version 1.1 [22] or at least 1 predominantly lytic bone lesion. All patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Patients were excluded if they had inflammatory breast cancer, central nervous system metastases, cardiac disease or Fridericia’s corrected QT interval (QTcF) > 450 ms, or impairment of gastrointestinal function that would have altered study drug absorption. Patients must not have received prior systemic therapy for advanced disease, except for ≤ 14 days of letrozole or anastrozole. The use of concomitant medications with known risk of prolonging the QT interval or inducing Torsades de Pointes was prohibited.
This study was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. An independent ethics committee and institutional review boards approved the study protocol and any subsequent amendments at each participating center. A study steering committee monitored study conduct in line with the protocol. Written informed consent was obtained from all the patients.
Randomization
Patients were randomized 1:1 to receive either oral ribociclib plus letrozole (ribociclib arm) or placebo plus letrozole (placebo arm). Randomization was stratified according to the presence of liver and/or lung metastases. Screening and treatment allocation were performed using an interactive voice and web response system. Patients and investigators were blinded to the assigned treatment; both ribociclib and placebo were identical in label, packaging, appearance, and administration schedule. Treatment crossover from placebo to ribociclib was not permitted.
Treatment and procedures
Details of study treatment and procedures have been reported previously [17]. Briefly, patients received either oral ribociclib (600 mg per day on a 3-weeks-on, 1-week-off schedule in 28-day treatment cycles) plus letrozole (2.5 mg per day on a continuous schedule) or placebo plus letrozole until disease progression, unacceptable toxicity, death, or discontinuation for any other reason. Ribociclib dose adjustments including dose interruption, reduction, and permanent discontinuation were permitted for the management of adverse events. Dose modifications of letrozole were not permitted.
Outcomes
The primary end point of the study was locally assessed PFS, according to RECIST, version 1.1, and has been reported previously [17]. The evaluation of patient-reported outcomes (PROs) for HRQoL was a secondary end point. The exploratory end points were time to response, duration of response. Time to response [complete response (CR) or partial response (PR)] was defined as the time interval between the date of randomization and the first documented response (CR or PR, which had to be confirmed subsequently). The duration of response was defined as the time from documentation of tumor response to disease progression. Post hoc analysis of PFS by subgroup according to TFI was also performed. TFI was defined as the time from last hormonal therapy to randomization and was calculated only for patients with prior hormonal therapy.
Assessments
Tumor response was assessed locally according to RECIST version 1.1 [22]. Computed tomography/magnetic resonance imaging assessments were conducted at screening, then every 8 weeks for the first 18 months, and every 12 weeks thereafter. For tumor shrinkage analyses, the patients were divided into the following 4 equal groups according to their best percentage change in target lesion size in the total population, irrespective of treatment arm: Group 1 (greatest decrease in tumor size): best percentage change in the target lesion size of at least − 60%; Group 2: best percentage change in target lesion size of between − 35 and − 60%; Group 3: best percentage change in target lesion size of between − 14 and − 35%; Group 4 (smallest decrease in tumor size): best percentage change in target lesion size of less than − 14% or tumor growth. Patients were excluded from the quartile analysis if the best percentage change was unavailable or if their best overall response was unknown.
TFI was analyzed at the following time points in both treatment groups: ≤ 24, > 24, ≤ 36, > 36, ≤ 48, > 48 months.
The EORTC QLQ-C30 was completed by patients at the beginning of each visit at screening, every 8 weeks following randomization for the first 18 months, every 12 weeks thereafter until disease progression, and at the end of treatment. Changes from baseline were analyzed using a linear effect model that incorporated treatment, stratification factors, and baseline scores. The cutoff for clinically meaningful change in EORTC QLQ-C30 scores was defined as > 5 points [23].
Results
Patient characteristics
A total of 668 patients were enrolled (334 into each treatment arm) between January 2014 and March 2015 (Fig. 1). Overall, 501 patients (256 in the ribociclib plus letrozole arm and 245 in the placebo plus letrozole arm) had measurable disease at baseline. Patient characteristics were generally well balanced between treatment arms, with the exception of a higher proportion of patients with visceral metastases in the placebo arm vs the ribociclib arm in Group 1 (83.8% vs. 63.5%) (Table 1).
Tumor response
Ribociclib plus letrozole was associated with a trend in favor of shorter time to response when compared with placebo plus letrozole. At 6 months, 37.2% of patients in the ribociclib arm achieved early response versus 23.2% of patients in the placebo arm (Fig. 2).
At the first tumor evaluation at 8 weeks decreased tumor size was observed in a higher proportion of patients in the ribociclib arm (76%; 180 of 238) versus the letrozole arm (67%; 152 of 227; Fig. 3). Patients with measurable disease at baseline in the ribociclib arm experienced a faster and more sustained decrease in tumor size compared with those in the placebo arm (Fig. 4). A consistent decrease in tumor size was also observed in patients with lung and/or liver metastases.
Duration of response
Ribociclib plus letrozole was associated with a trend in favor of longer duration of response. In patients with measurable disease and a confirmed complete response or partial response, the median duration of response was 26.7 months (95% CI, 24.0–not reached) for the ribociclib plus letrozole arm vs 18.6 months (95% CI, 14.8–23.1) for the placebo plus letrozole arm (Fig. 5). The probability of remaining progression-free at 24 months was 60% for patients receiving ribociclib plus letrozole versus 35% for those receiving placebo plus letrozole.
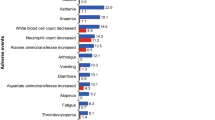
Tumor shrinkage
Overall, 444 patients were evaluable for tumor shrinkage quartile analyses. A higher proportion of patients treated with ribociclib plus letrozole (32%) versus placebo plus letrozole (17%) had the greatest decrease in tumor size (Group 1, 60%) (Fig. 6). The proportion of patients with the least decrease in tumor size or having tumor growth (Group 4, 14%) was lower in the ribociclib plus letrozole (n = 43) versus placebo plus letrozole arm (n = 68). This was representative of an overall shift in tumor response, such that patients receiving ribociclib plus letrozole were more likely to experience greater tumor shrinkage, and patients receiving placebo plus letrozole were more likely to experience less tumor shrinkage, or even tumor growth.
Pain reduction
As reported previously, overall HRQoL (global health status/quality of life score) was maintained from baseline and was similar in both treatment arms (27.7 months to 10% of deterioration in the ribociclib plus letrozole arm vs 26.7 months in the placebo plus letrozole arm; hazard ratio, 0.944 (95% CI, 0.720–1.237) [24]. At 8 weeks, among all patients with available percentage change from baseline, the average pain reduction was greater in the ribociclib arm versus the placebo arm (26% vs. 15%, respectively). The median percentage change from baseline in EORTC QLQ-C30 pain symptom score in patients receiving ribociclib plus letrozole was − 40 vs. − 29% in those receiving placebo plus letrozole. A clinically meaningful mean reduction in pain (> 5 points) was observed in patients receiving ribociclib plus letrozole (− 6.3 points) but not in patients receiving placebo plus letrozole (− 2.7 points). For patients with clinical benefit, the mean change in pain score from baseline was − 7.0 points in the ribociclib plus letrozole arm and − 1.3 in the placebo plus letrozole arm (Table 2).
Treatment-free interval
In a post hoc analysis, PFS benefit with ribociclib was maintained irrespective of the TFI in patients who received prior (neo) adjuvant endocrine therapy. The hazard ratios for PFS were consistent across all TFI subgroups (> 24 vs. ≤ 24 months; > 36 vs. ≤ 36 months; > 48 vs. ≤ 48 months) (Fig. 7). The hazard ratios for PFS in these subgroups were consistent with that reported for the overall population [17].
Discussion
In this exploratory analysis of the MONALEESA-2 trial, ribociclib plus letrozole demonstrated rapid and durable tumor response as early as 8 weeks and maintained PFS benefit irrespective of TFI in postmenopausal women with HR+ , HER2− ABC who had received no prior systemic therapy for advanced disease. HRQoL analysis showed that ribociclib plus letrozole led to greater pain reduction, as early as 8 weeks.
In MONALEESA-2, the ORR in the ribociclib arm versus placebo arm was 40.7% versus 27.5% [17]. ORR with palbociclib plus letrozole versus placebo plus letrozole in PALOMA-2 was 42.1% versus 34.7% [25] while in MONARCH-3, the ORR with abemaciclib plus nonsteroidal aromatase inhibitor (NSAI) was 59.0% versus 44.0% with placebo plus NSAI [21]. Although CDK4/6 inhibitors in combination with ET improved ORR compared to ET alone, the data presented here show that ribociclib led to faster tumor response as early as 8 weeks in postmenopausal women with HR+ , HER2− ABC and measurable disease at baseline who had received no prior systemic therapy for advanced disease.
Emerging data suggest that tumor shrinkage can predict long-term survival in patients with breast cancer. A recently published modeling analysis suggests that change in tumor size at 8 weeks may predict overall survival in the first-line ABC therapy [26]. In MONALEESA-2, a higher proportion of patients with measurable disease at baseline in the ribociclib arm (76%) versus the placebo arm (67%) showed a decrease in tumor size at 8 weeks. Similarly, at 8 weeks, the proportion of patients who had the greatest decrease in tumor size (Group 1) was higher in the ribociclib arm (32%) versus placebo arm (17%). To our knowledge, ribociclib in combination with letrozole is the only CDK4/6 inhibitor showing tumor shrinkage as early as 8 weeks in patients with HR+ , HER2− ABC who had not received prior therapy for advanced disease.
A longer duration of response with ribociclib plus letrozole (26.7 months) versus placebo plus letrozole (18.6 months) was observed in MONALEESA-2. In PALOMA-2, the duration of response was longer with palbociclib plus letrozole (22.5 months) versus placebo plus letrozole (16.8 months) [25]. In MONARCH-3, the median duration of response was not reached with abemaciclib plus NSAI versus 14.1 months with placebo plus NSAI in patients with HR+ , HER2− ABC who had not received prior systemic therapy in the advanced setting [21]. Overall, these results suggest that the treatment with ribociclib resulted in more durable responses in patients with HR+ , HER2− ABC who had not received prior therapy for advanced disease.
The potential of TFI as a prognostic and predictive marker of benefit of next treatment has been demonstrated across several tumor types [20]. In this subgroup analysis based on TFI of MONALEESA-2, PFS benefit with ribociclib was maintained with consistent hazard ratios across all patient subgroups irrespective of TFI. In contrast, an exploratory analysis of MONARCH-3 demonstrated that only patients with a TFI of < 36 months derived PFS benefit with abemaciclib plus NSAI compared with patients with longer TFI > 36 months. The TFI data from MONALEESA-2 suggest that the PFS benefit with ribociclib was independent of TFI in patients with HR+ , HER2− ABC.
Ribociclib in combination with letrozole also resulted in a clinically meaningful reduction in EORTC QLQ-C30 pain score at week 8. As reported previously, in MONALEESA-2 the overall HRQoL (global health status/quality of life score) was maintained from baseline and was similar in both treatment arms [24]. In the PALOMA-3 study, the estimated overall global QoL scores (p = 0.0313) and improvement from baseline in pain score (p = 0.0011) significantly favored palbociclib plus fulvestrant group [27]. Palbociclib plus ET combination also resulted in a 36% of reduction in the risk of QoL deterioration [13]. Similarly, abemaciclib monotherapy also showed improvement from baseline in pain score (p = 0.003) [28]. The data presented here are the first with a CDK4/6 inhibitor to show a clinically meaningful decrease in pain as early as 8 weeks.
In conclusion, the results from these exploratory analyses suggest that ribociclib in combination with letrozole is associated with earlier and more durable tumor response, as well as greater tumor shrinkage at 8 weeks. The PFS benefit irrespective of TFI and improvement in pain symptoms with ribociclib plus letrozole further support the clinical benefit of ribociclib. These additional analyses from MONALEESA-2 demonstrate that ribociclib plus letrozole provides a valuable first-line treatment option for postmenopausal women with HR+ , HER2− ABC.
References
Gnant M (2012) The role of mammalian target of rapamycin (mTOR) inhibition in the treatment of advanced breast cancer. Curr Oncol Rep 15:14–23. https://doi.org/10.1007/s11912-012-0277-1
Gnant M (2012) Overcoming endocrine resistance in breast cancer: importance of mTOR inhibition. Expert Rev Anticancer Ther 12:1579–1589. https://doi.org/10.1586/era.12.138
Cardoso F, Costa A, Norton L, Senkus E, Aapro M, André F, Barrios CH, Bergh J, Biganzoli L, Blackwell KL, Cardoso MJ, Cufer T, El Saghir N, Fallowfield L, Fenech D, Francis P, Gelmon K, Giordano SH, Gligorov J, Goldhirsch A, Harbeck N, Houssami N, Hudis C, Kaufman B, Krop I, Kyriakides S, Lin UN, Mayer M, Merjaver SD, Nordström EB, Pagani O, Partridge A, Penault-Llorca F, Piccart MJ, Rugo H, Sledge G, Thomssen C, van’t Veer L, Vorobiof D, Vrieling C, West N, Xu B, Winer B (2014) ESO-ESMO 2nd international consensus guidelines for advanced breast cancer (ABC2). Ann Oncol 25:1871–1888. https://doi.org/10.1093/annonc/mdu385
National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology – Breast Cancer version 2.2017
Fox EM, Arteaga CL, Miller TW (2012) Abrogating endocrine resistance by targeting ERalpha and PI3K in breast cancer. Front Oncol 2:145. https://doi.org/10.3389/fonc.2012.00145
Osborne CK, Schiff R (2011) Mechanisms of endocrine resistance in breast cancer. Annu Rev Med 62:233–247. https://doi.org/10.1146/annurev-med-070909-182917
Mayer IA, Arteaga CL (2016) The PI3K/AKT pathway as a target for cancer treatment. Annu Rev Med 67:11–28. https://doi.org/10.1146/annurev-med-062913-051343
Miller TW, Balko JM, Fox EM, Ghazoui Z, Dunbier A, Anderson H, Dowsett M, Jiang A, Smith RA, Maira SM, Manning HC, Gonzalez-Angulo AM, Mills GB, Higham C, Chanthaphaychith S, Kuba MG, Miller WR, Shyr Y, Arteaga CL (2011) ERalpha-dependent E2F transcription can mediate resistance to estrogen deprivation in human breast cancer. Cancer Discov 1:338–351. https://doi.org/10.1158/2159-8290.CD-11-0101
Cancer Genome Atlas N (2012) Comprehensive molecular portraits of human breast tumours. Nature 490:61–70. https://doi.org/10.1038/nature11412
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im S-A, Masuda N, Colleoni M, DeMichele A, Loi S, Verma S, Iwata H, Harbeck N, Zhang K, Theall KP, Jiang Y, Bartlett CH, Koehler M, Slamon D (2016) Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol 17:425–439. https://doi.org/10.1016/s1470-2045(15)00613-0
Finn RS, Crown JP, Lang I, Boer K, Bondarenko IM, Kulyk SO, Ettl J, Patel R, Pinter T, Schmidt M, Shparyk Y, Thummala AR, Voytko NL, Fowst C, Huang X, Kim ST, Randolph S, Slamon DJ (2015) The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol 16:25–35. https://doi.org/10.1016/s1470-2045(14)71159-3
Finn RS, Martin M, Rugo HS, Jones SE, Im S-A, Gelmon KA, Harbeck N, Lipatov ON, Walshe JM, Moulder SL, Gauthier ER, Lu D, Randolph S, Diéras V, Slamon DJ (2016) PALOMA-2: primary results from a phase III trial of palbociclib (P) with letrozole (L) compared with letrozole alone in postmenopausal women with ER+/HER2− advanced breast cancer (ABC). J Clin Oncol 34:507. https://doi.org/10.1200/JCO.2016.34.15_suppl.507
Turner NC, Ro J, André F, Loi S, Verma S, Iwata H, Harbeck N, Loibl S, Huang Bartlett C, Zhang K, Giorgetti C, Randolph S, Koehler M, Cristofanilli M (2015) Palbociclib in hormone-receptor–positive advanced breast cancer. N Engl J Med 373:209–219. https://doi.org/10.1056/nejmoa1505270
Kim S, Loo A, Chopra R, Caponigro G, Huang A, Vora S, Parasuraman S, Howard S, Keen N, Sellers W, Brain C (2013) Abstract PR02: LEE011: An orally bioavailable, selective small molecule inhibitor of CDK4/6− reactivating Rb in cancer. Molecular Cancer Therapeutics 12:PR02-PR02. https://doi.org/10.1158/1535-7163.targ-13-pr02
O’Brien NA, Tomaso ED, Ayala R, Tong L, Issakhanian S, Linnartz R, Finn RS, Hirawat S, Slamon DJ (2014) Abstract 4756: in vivo efficacy of combined targeting of CDK4/6, ER and PI3K signaling in ER+ breast cancer. Cancer Res 74:4756. https://doi.org/10.1158/1538-7445.am2014-4756
Juric D, Munster PN, Campone M, Ismail-Khan R, García-Estevez L, Hamilton EP, Becerra C, Boer RHD, Hui R, Goncalves A, Wang Y, Dhuria SV, Kalimi GH, Lorenc KCR, Mayer IA (2016) Ribociclib (LEE011) and letrozole in estrogen receptor-positive (ER+), HER2-negative (HER2−) advanced breast cancer (aBC): phase Ib safety, preliminary efficacy and molecular analysis. J Clin Oncol 34:568. https://doi.org/10.1200/JCO.2016.34.15_suppl.568
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, Campone M, Blackwell KL, Andre F, Winer EP, Janni W, Verma S, Conte P, Arteaga CL, Cameron DA, Petrakova K, Hart LL, Villanueva C, Chan A, Jakobsen E, Nusch A, Burdaeva O, Grischke EM, Alba E, Wist E, Marschner N, Favret AM, Yardley D, Bachelot T, Tseng LM, Blau S, Xuan F, Souami F, Miller M, Germa C, Hirawat S, O’Shaughnessy J (2016) Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N Engl J Med 375:1738–1748. https://doi.org/10.1056/NEJMoa1609709
Hortobagyi GN, Stemmer SM, Burris HA, Yap YS, Sonke GS, Paluch-Shimon S, Campone M, Petrakova K, Blackwell KL, Winer EP, Janni W, Verma S, Conte PF, Arteaga CL, Cameron DA, Xuan F, Miller MK, Germa C, Hirawat S, O’Shaughnessy J (2017) Updated results from MONALEESA-2, a phase 3 trial of first-line ribociclib + letrozole in hormone receptor-positive (HR+), HER2-negative (HER2−), advanced breast cancer (ABC). J Clin Oncol 35:1038. https://doi.org/10.1200/JCO.2017.35.15_suppl.1038
Nahleh ZA (2008) Residual cancer burden in locally advanced breast cancer: a superior tool. Curr Oncol. https://doi.org/10.3747/co.v15i6.242
Gregorc V, Ghio D, Sallemi C, Bulotta A, Rossoni G, Viganò MG, Fontana F, Rossoni G, Colombi S, Lambiase A, Bordignon C (2015) Treatment-free interval (TFI) after first-line therapy as a prognostic and predictive factor in malignant pleural mesothelioma (MPM): findings from the NGR015 phase III trial with NGR-hTNF plus best investigator choice (BIC) versus placebo plus BIC. J Clin Oncol 33:7557. https://doi.org/10.1200/jco.2015.33.15_suppl.7557
Goetz MP, Toi M, Campone M, Sohn J, Paluch-Shimon S, Huober J, Park IH, Tredan O, Chen SC, Manso L, Freedman OC, Garnica Jaliffe G, Forrester T, Frenzel M, Barriga S, Smith IC, Bourayou N, Di Leo A (2017) MONARCH 3: Abemaciclib as initial therapy for advanced breast cancer. J Clin Oncol. https://doi.org/10.1200/jco.2017.75.6155
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16:139–144. https://doi.org/10.1200/jco.1998.16.1.139
Verma S, O’Shaughnessy J, Burris HA, Campone M, Alba E, Chandiwana D, Manson S, Sutradhar SC, Monaco M, Janni W (2017) Health-related quality of life (HRQoL) of postmenopausal women with hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2−) advanced breast cancer (ABC) treated with ribociclib + letrozole: results from MONALEESA-2. J Clin Oncol 35:1020. https://doi.org/10.1200/JCO.2017.35.15_suppl.1020
Finn RS, Martin M, Rugo HS, Jones S, Im S-A, Gelmon K, Harbeck N, Lipatov ON, Walshe JM, Moulder S, Gauthier E, Lu DR, Randolph S, Diéras V, Slamon DJ (2016) Palbociclib and Letrozole in advanced breast cancer. N Engl J Med 375:1925–1936. https://doi.org/10.1056/NEJMoa1607303
Tate SC, Andre V, Enas N, Ribba B, Gueorguieva I (2016) Early change in tumour size predicts overall survival in patients with first-line metastatic breast cancer. Eur J Cancer 66:95–103. https://doi.org/10.1016/j.ejca.2016.07.009
Harbeck N, Iyer S, Turner N, Cristofanilli M, Ro J, André F, Loi S, Verma S, Iwata H, Bhattacharyya H, Puyana Theall K, Bartlett CH, Loibl S (2016) Quality of life with palbociclib plus fulvestrant in previously treated hormone receptor-positive, HER2-negative metastatic breast cancer: patient-reported outcomes from the PALOMA-3 trial. Ann Oncol 27:1047–1054. https://doi.org/10.1093/annonc/mdw139
Boye M, Houghton K, Stull DE, Ainsworth C, Price GL (2017) Estimating the effects of patient-reported outcome (PRO) diarrhea and pain measures on PRO fatigue: data analysis from a phase II study of abemaciclib monotherapy, a CDK4 and CDK6 inhibitor, in patients with HR+/HER2- breast cancer after chemotherapy for metastatic disease—MONARCH 1. J Clin Oncol 35:1060. https://doi.org/10.1200/JCO.2017.35.15_suppl.1060
Acknowledgments
We thank the patients who participated in this trial and their families, as well as staff members at individual trial centers who provided support; Avinash Yerramsetti and Amol Hosing (Novartis Healthcare Pvt Ltd) for providing medical editorial assistance with this manuscript. Ribociclib was discovered by Novartis Institutes for BioMedical Research in collaboration with Astex Pharmaceuticals.
Funding
The study was initiated, funded, and sponsored by Novartis Pharmaceuticals Corporation. The study was designed by the investigators and the sponsor. Design and conduct of the study was undertaken by the sponsor in collaboration with investigators. The study investigators and their respective research teams collected the data; Novartis Pharmaceuticals Corporation compiled the data for summation and analysis. All authors were responsible for data interpretation. The article was prepared by Dr Janni in conjunction with all the authors, including employees of the sponsor. The corresponding author had final responsibility for the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Janni reports grants and personal fees from Novartis during the conduct of the study and outside the submitted work. Dr. Alba reports advisory board fees from Roche, Pfizer, and Novartis outside the submitted work. Dr. Bachelot reports personal fees from AstraZeneca, Roche, Novartis, and Pfizer; research grants from Roche, Novartis, and Pfizer outside the submitted work. Dr. Esteva reports consulting fee and research funding to his institution. Dr. Pluard reports advisory board fees from Novartis. Mr. Sutradhar is an employee of Novartis Pharmaceutical Corporation. Dr. Miller is employee of Novartis Pharmaceutical Corporation and hold Novartis stock options. Prof. Campone reports fees for advisory boards from Novartis, during the conduct of the study; and fees for advisory boards from Lilly, Sanofi, Pfizer, and AstraZeneca outside the submitted work. Dr. Diab, Dr. Gil, Dr. Beck, Ryvo, Dr. Tsai, Dr. Aunon, Dr. Kral, Dr. Ward, and Dr. Richards have nothing to disclose.
Rights and permissions
About this article
Cite this article
Janni, W., Alba, E., Bachelot, T. et al. First-line ribociclib plus letrozole in postmenopausal women with HR+ , HER2− advanced breast cancer: Tumor response and pain reduction in the phase 3 MONALEESA-2 trial. Breast Cancer Res Treat 169, 469–479 (2018). https://doi.org/10.1007/s10549-017-4658-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4658-x