Abstract
Purpose
The present study evaluated whether morphological-measured stromal and intra-tumour tumour-infiltrating lymphocytes (TILs) levels were associated with gene expression profiles, and whether TILs-associated genomic signature (GS) could be used to predict clinical outcomes and response to therapies in several breast cancer subtypes.
Methods
We retrospectively evaluated haematoxylin eosin (HE)-TILs levels and gene expression profiling data from 40 patients with primary breast cancer and extracted the 22 overexpressed genes in cases with high TILs scores as the TILs-GS. The TILs-GS were compared with breast cancer subtype and were evaluated predictive values for prognosis and response to therapies.
Results
Higher TILs-GS expressions were observed for triple-negative and human epidermal growth factor receptor 2 (HER2) positive (+) breast cancers, compared to the luminal types (P < 0.001). With the exception of HER2+, the TILs-GS had no prognostic value in subtypes of breast cancers. The Wilcoxon test revealed significantly different TILs-GS levels between the cases with pathological complete response (pCR) and residual disease after anthracycline and taxane-based neoadjuvant chemotherapy, with the exception of the luminal-low proliferation subtype. In the multivariate analysis, pCR was independently associated with smaller tumour size, higher histological grade, ER negativity, HER2 positivity and higher TILs-GS scores (OR 2.02, 95% CI 1.30–3.14, P = 0.025).
Conclusions
TILs-GS was associated with stromal and intra-tumour TILs levels, as evaluated using HE, which predicted prognosis and chemotherapy response in several breast cancer subtypes. Further studies are needed to perform stratification according to TILs-GS levels and the conventional breast cancer subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In hormone receptor-positive (HR+) and human epidermal growth factor receptor 2-negative (HER2−) breast cancers, first-generation genomic signatures that are highly associated with proliferation have been widely used to predict prognosis and as secondary markers for predicting chemotherapy response [1, 2]. Several prospective randomized trials are currently evaluating the utility of the first-generation genomic signatures, and several results have recently been reported [3, 4]. For example, genomic markers, especially for HR+ breast cancer, may indicate that some patients cannot benefit from receiving adjuvant chemotherapy, which is also associated with significant side effects. Cost-effectiveness has also been discussed. These reports showed similar advantages to use first-generation signatures from the quality-adjusted life-years compared to conventional clinicopathological markers [5, 6]. However, with the exception of the conventional clinicopathological markers, there are no standardized and clinically available prognostic and predictive markers for HER2+ or HR− breast cancers. Several recent clinical studies have revealed that morphological evaluation for tumour-infiltrating lymphocytes (TILs), using hematoxylin eosin (HE) or immunohistochemistry (IHC) testing, can predict prognosis and chemotherapy response, independent of the effects of age, nodal status and tumour size, in cases of estrogen receptor-negative (ER−), triple-negative (TN) and HER2+ breast cancer [7–9]. A recent meta-analysis also revealed that high levels of TILs were significantly associated with favourable breast cancer outcomes in patients who predominantly had TN cancers [10]. Thus, using morphological-measured TILs in different breast cancer subtypes may provide clinically relevant information regarding chemotherapy response and prognosis.
Despite this information, most panellists at the 2015 St Gallen Consensus Conference did not recommend using TILs as a new prognostic factor, based on the absence of standardized evaluation guidelines and limited information regarding reproducibility and clinical validity [11]. However, a group of professionals who are experienced in TILs evaluation (the International TIL Working Group) recently issued recommendations for improving the consistency of TILs scoring, as well as detailed guidelines for annotating lymphocyte infiltration [12]. These recommendations are important, as HE or IHC testing for morphology is cumbersome and lacks objectivity and reproducibility in many instances. For example, there is broad inconsistency in the IHC evaluation of Ki-67 in moderately differentiated breast cancer, and there is controversy regarding whether Ki-67 is an appropriate biomarker for guiding treatment decisions for patients with breast cancer. Furthermore, previous studies have described inconsistent Ki-67 assessments during the routine diagnosis of breast cancer [13, 14]. Moreover, the inter- and intra-observer variability in Ki-67 assessments remains poor to moderate in cases of breast cancer, especially in the G2 breast cancer group (kappa: 0.2–0.4), despite recommendations from the International Ki-67 in Breast Cancer Working Group [13, 14]. Thus, the absence of standardized methodologies, cut-off values and information regarding inter-/intra-observer agreement for evaluating TILs has limited the use of morphological testing to detect TILs in clinical practice [12, 15].
The problems of reproducibility and consistency may be further exacerbated by the complex testing procedure, as Hida et al. have indicated that the morphological method is too detailed for pathologists to use in clinical practice [16]. Thus, a reproducible and objective method for evaluating TILs, such as gene expression profiles, is needed. Previously published results may provide valuable information regarding the use and logistical implementation of gene expression profiles, as several studies have addressed sample handling, testing reproducibility, quality control and standardization of genomic signatures [2, 17, 18]. However, little is known regarding whether TILs-associated genomic signature (TILs-GS) can predict prognosis and treatment response. Therefore, the present study evaluated whether HE-measured stroma and intra-tumour TILs levels were associated with gene expression profiles, and whether TILs-GS could be used to predict chemotherapy response and prognosis in several breast cancer subtypes.
Materials and methods
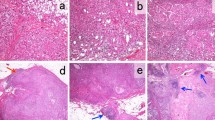
Training dataset and TILs-GS
We retrospectively evaluated haematoxylin and eosin-stained slides and gene expression profiling data (Gene Expression Omnibus dataset: http://www.ncbi.nlm.nih.gov/geo/GSE6367) from 40 patients with primary breast cancer. The slides were evaluated for TILs at low magnification (×2−4) by a single pathologist from the Nihon University School of Medicine. The presence of TILs was evaluated at the edges of the tumour mass, in the tumour mass, and in the stroma surrounding the expanding mammary ducts that were packed with carcinoma cells. The HE-assessed TILs results were scored as 0 (no detected TILs), 1 (sparse TILs; <50% of the area had TILs) or 2 (dense TILs; >50% of the area had TILs). Among the 40 included cases, 11 cases were assigned a score of 0, 18 cases were assigned a score of 1 and 11 cases were assigned a score of 2. Our institutional ethics board approved the use of human tissues for the HE assessments of TILs.
We subsequently selected 29 samples (scores of 0 or 2) that had available TILs information and gene expression profiling data, and identified genes that were differentially expressed in the samples with TILs scores of 0 or 2. To minimize noisy measurements, we removed probe sets that had average expression values of less than or equal to the lowest 15% of the expression distributions, and retained only the probe set with the highest average gene expression. Thus, 7797 genes were included in the analysis.
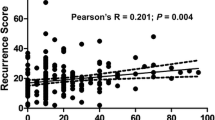
We also performed a class comparison test for mRNA gene expressions using the samples with TILs scores of 0 or 2. In this analysis, we blocked the samples using ER status, in order to analyse randomized experiments. This approach allowed us to adjust for a single covariate (i.e., ER status) while analysing different classes (i.e., TILs scores of 0 or 2) using the BRB Array Tools software, as HE-assessed TILs levels are highly associated with ER status [19]. Parametric P values of <0.001 were considered statistically significant in the training analysis, and the 22 overexpressed genes in cases with TILs scores of 2 were selected as the TILs-GS (Supplementary Table 1). The overall TILs-GS score was calculated using the average unweighted gene expressions for the 22 genes, in order to ensure comparability of results that were obtained using different chip types.
Validation analysis for TILs-GS
During the validation analysis, we retrieved publicly available cDNA microarray data from 2337 primary breast cancers (806 cases without systemic adjuvant therapy from GSE2034, GSE2990, GSE7390 and GSE11121; 625 cancers that received anthracycline and taxane-based neoadjuvant chemotherapy [NAC] from GSE20194, GSE20271, GSE22093, GSE23988 and GSE25066; 780 cases that received tamoxifen from GSE6532, GSE12093, GSE1705 and GSE26971 and 126 cases that received trastuzumab from GSE37946, GSE42822 and GSE50948). These data were annotated using the Affymetrix Human Genome Array (Affymetrix Inc., Santa Clara, CA). Expressions of ER and HER2 were identified based on ER (ESR1) and HER2 (ERBB2) mRNA expression levels, as previously described [20, 21]. All gene expression data were generated using Affymetrix gene chips and normalized using the MAS5 algorithm (http://www.bioconductor.org), with the mean expression centred to 600 and log 2 transformation. Patients with ESR1 mRNA expression levels (probe set: 205225_at) of greater >10.18 were considered ER+ , and patients with HER2 mRNA expression levels (probe set: 216836_s_at) of >12.54 were considered HER2+ [20, 21]. ER+ and HER2− breast cancers were stratified into two groups with luminal A-like low proliferation or luminal B-like high proliferation. The proliferation score was calculated as the average expression of 12 mitotic kinases (Mitotic Kinase Score), as previously described [22]. The cut-off point between luminal-low and -high proliferation was set at a Mitotic Kinase Score of 8.255 [20].
First, we compared the TILs-GS according to breast cancer subtype (luminal-low, luminal-high, HER2+ and TN [ER−/HER2−]) using the Kruskal–Wallis rank sum test. The prognostic analysis was performed using datasets from patients who received no systemic adjuvant therapy or only adjuvant tamoxifen. The outcome of interest was defined as distant event-free survival (DEFS), and was evaluated according to the tertiles of the TILs-GS score. Survival was censored at 10 years. Survival curves were calculated using the Kaplan–Meier method and compared using the log-rank test. Survivals were also evaluated using a proportional hazards model and Cox regression analysis to estimate the hazard ratios (HRs) and 95% confidential intervals (CIs). In the tamoxifen-treated dataset, we only used ER+ and HER2− cases for the predictive analysis.
Second, therapy sensitivity analysis was performed according to whether the patients had received anthracycline- and taxane-based NAC or a trastuzumab-containing regimen. The outcome of interest was defined as pathological complete response (pCR) in the breast and axilla. The samples for the NAC cohorts had been collected before any treatment using needle biopsy. The Wilcoxon test was used to evaluate the associations between TILs-GS and the responses to NAC or trastuzumab according to breast cancer subtype. Univariate and multivariate logistic regression analyses were also performed to evaluate the values of TILs-GS and clinicopathological variables for predicting NAC response. To avoid optimal cut-off selection bias [23], the univariate and multivariate logistic regression analyses were performed using metagene scores as continuous variables. The multivariate analyses included variables with a univariate P value of <0.1 to avoid overfitting of the data, based on the small number of events in each subgroup.
All statistical analyses were performed using BRB Array Tools software (version 3.9.0a; http://linus.nci.nih.gov/BRB-ArrayTools.html) and R software (version 2.9.0; http://www.r-project.org). Two-sided P values of ≤0.05 were considered statistically significant.
Results
Figure 1 shows the associations between TILs-GS and the breast cancer subtypes in the prognostic dataset. Significantly higher TILs-GS expressions were observed for TN and HER2+ breast cancers, compared to the luminal types (rank sum test P < 0.001). As expected, higher TILs-GS expression levels were associated with the characteristics of more aggressive breast cancers.
Prognostic and predictive values of TILs-GS
The Kaplan–Meier DEFS curves for the TILs-GS tertiles were plotted according to breast cancer subtype using the pooled prognostic datasets from tamoxifen-treated patients and patients without adjuvant treatment (Fig. 2, Supplementary Fig. 1). Among the patients without adjuvant treatment, TILs-GS did not predict prognosis in the luminal cases, regardless of the proliferative level (Fig. 2a, b). Similarly, in the tamoxifen-treated dataset, TILs-GS did not predict prognosis in any of the proliferative subtypes (Supplementary Fig. 1a, b). Among HER2+ cases, a high TILs-GS was significantly associated with a better prognosis, compared to cases with lower expressions (log rank P = 0.001), although this analysis only considered a small number of cases (n = 120) (Fig. 2c). Among TN cases, we observed a similar trend compared to the HER2+ cases, although the trend was not statistically significant (log rank P = 0.729) (Fig. 2d).
The Kaplan–Meier curves according to tumour-infiltrating lymphocytes gene signatures in the dataset without adjuvant treatment. The Kaplan–Meier curves for a luminal-low, b luminal-high, c HER2+ and d triple-negative breast cancers. P-values were calculated using the log-rank test. Hazard ratios (HR) and 95% confidence intervals (CIs) were estimated for distant event-free survival using Cox regression analysis
We also assessed the predictive power of TILs-GS using the NAC-treated cases according to breast cancer subtype. With the exception of the luminal-low proliferation subtype, the Wilcoxon test revealed significantly different TILs-GS levels between the cases with pCR or residual disease. This result indicates that TILs-GS might be a strong marker for predicting chemotherapy response (Fig. 3). In contrast, TILs-GS had no predictive power in the two independent trastuzumab-treated datasets (Supplementary Fig. 2).
Neoadjuvant therapy responses and tumour-infiltrating lymphocytes gene signatures according to breast cancer subtype. The regimens contained anthracycline and taxane. The boxplots show the associations between tumour-infiltrating lymphocytes gene signatures (TILs-GS) and neoadjuvant therapy responses according to breast cancer subtype (A: luminal-low, B: luminal-high, C: HER2+ and D: triple-negative). P values were calculated using Wilcoxon’s test. pCR pathological complete response, RD residual disease
Finally, we performed univariate and multivariate logistic regression analyses to determine whether TILs-GS and the clinicopathological variables could predict pCR (Table 1). In the univariate analyses, pCR was significantly associated with higher histological grade, ER negativity, HER2 positivity and higher TILs-GS scores. In the multivariate analysis, pCR was independently associated with smaller tumour size, higher histological grade, ER negativity, HER2 positivity and higher TILs-GS scores (OR 2.02, 95% CI 1.30–3.14, P = 0.025).
Discussion
The present study revealed that genomic markers were highly associated with TILs levels based on HE. Interestingly, Gu-Trantien et al. evaluated leukocyte infiltration in various breast cancers, and found that 75% of the cells were T lymphocytes, <20% of the cells were B-cells, <10% of the cells were monocytes and <5% of the cells were natural killer cells or natural killer T-cells [24]. Given that our TILs evaluations were based on HE, it is unsurprising that most TILs-associated genes had roles in immune function, especially in T lymphocytes (e.g., ICOS, TCF7, LCK and LCP1). Furthermore, we found that breast cancers with TILs scores of 2 (dense TILs) and 0 (no identified TILs) had distinct gene expression patterns, and that aggressive breast cancer subtypes (e.g., ER− or HER2+) were associated with higher TILs-GS levels. Similar results have been observed in previously studies [19, 25, 26]. However, we investigated the clinical implications of these findings and discovered that TILs-GS was associated with chemotherapy response in several breast cancer subtypes.
Our finding that TILs-GS was highly associated with stromal and intra-tumour TILs status may be reasonable and reproducible. International TILs Working Group recommends evaluating stromal TILs as the principle parameter, rather than intra-tumour TILs, because intra-tumour TILs do not provide the same information that is provided by stromal TILs [12]. However, recent evidence from the neoadjuvant setting suggests that both stromal and intra-tumour TILs can predict NAC response [27]. In addition, Dieci et al. reported that intra-tumour and stromal TILs strongly predicted overall survival (intra-tumour TILs, HR 0.85, P = 0.003; stromal TILs, HR 0.89, P = 0.005) [8]. Nevertheless, it is impractical to consider only stromal TILs during clinical practice, as genome signature samples are usually obtained using core needle biopsy which contain tumour cells (50%), lymphocytes (20%) and stromal cells (30%) [17], or surgical samples, those composition is usually similar to core needle biopsy. Thus, without microdissection to separate the stromal and intra-tumour components, gene expression profiling inevitably involves intra-tumour components. Moreover, microdissection is a complex procedure that cannot be routinely performed during clinical practice, and our goal was to develop TILs-GS as a clinically useful tool. Therefore, the TILs-GS was developed using the signatures that were associated with both intra-tumour and stromal TILs, which allowed us to directly examine and compare TILs-GS with the morphological-evaluated TILs levels.
The present study also revealed that TILs-GS predicted chemotherapy response in most breast cancer subtypes, with the exception of the luminal-low proliferative subtype. Several previous reports have also revealed that immune-related genomic signatures have predictive value, especially in non-luminal breast cancers [22, 28, 29]. There are several possible explanations for the absence of predictive value in the luminal-low proliferative subtype. First, chemotherapy itself may not be effective for low-proliferative breast cancers [30–32]. Second, the pCR outcome after NAC may not be suitable for evaluating efficacy in luminal cases [33]. Third, it is possible that our analyses were underpowered, given the sample size and number of events.
Interestingly, our results revealed that TILs-GS had prognostic value in only HER2+ cases. Previous studies have evaluated the prognostic value of TILs in the context of randomized adjuvant trials for breast cancer. The results indicate that baseline TILs were associated with high-proliferative, high-grade and ER− breast cancers, and strongly predicted prognosis for specific breast cancer subtypes, especially TN cancers [7, 19]. However, these trials only considered patients who received adjuvant chemotherapy and/or targeted therapy, and the prognostic value of TILs in untreated patients remains unclear. In the present study, the untreated dataset included retrospectively evaluated outcomes in patients with stage I–II disease and without lymph node metastasis. Thus, the clinical and biological significances of TILs may be distinct in early and advanced breast cancers, and it might be useful to identify patients with a poor prognosis (who should not receive adjuvant therapy) and patients who are expected to experience a good response to therapy. This type of evaluation would require patients with advanced cancers who have not received adjuvant therapy, although it would be difficult to prospectively collect samples in this subgroup, given the related ethical issues.
To address this issue, we tested the predictive value of TILs-GS among trastuzumab-treated cases, as TILs can predict long-term survival in these cases [8, 34], as well as the efficacy of trastuzumab [26, 35]. In addition, trastuzumab treatment results in the activation or recruitment of multiple immune cell lineages, and increases the susceptibility of tumour cells to antibody-dependent cytotoxicity [36]. However, the N9831 trial revealed that TILs were not associated with prognosis among patients who received chemotherapy plus trastuzumab [37]. Nevertheless, patients who receive trastuzumab are a unique subgroup, as they typically receive trastuzumab combined with multiple chemotherapeutic agents, which can induce immunogenic cell death, carcinoma differentiation and inhibit TILs mitosis [38–40]. Thus, data from patients who received only a single agent are needed to evaluate a single marker’s predictive power (the “one agent needs one predictive marker” concept). In the present study, TILs-GS did not have prognostic value when we only considered the tamoxifen-treated dataset, and this result was independent of the proliferative level, which indicates that TILs may have distinct roles in cases that received hormone therapy or chemotherapy. Interestingly, Dowsett et al. reported that higher immune-related genes were associated with poorer response to aromatase inhibitor [41], although these associations were opposite to chemotherapy response. The immune system has conflicting potential role in both suppressing tumour growth and carcinogenesis through the production of cytokines and growth factors [42]. Therefore, the absence of predictive value in chemotherapy-treated luminal-low proliferative cases might be related to the distinct roles of TILs in different breast cancer subtypes. Additional studies are needed to validate our findings and address these issues.
The present study has an important limitation as the training and validation datasets were relatively small, and therefore some are true but weaker prognostic and predictive variables may not have been detected as significance in our study. Also, our TILs-GS findings should be compared to the predictive powers of previously published immune-related signatures [43]. Nevertheless, we believe that our findings are generalizable and consistent with predictive results that were observed in datasets treated using homogeneous chemotherapy regimens. Furthermore, our methods for gene expression profiling using stromal and intra-tumour components, and our unweighted calculations of the gene expression profiles, should be relatively easy to validate using other datasets.
In conclusion, TILs-GS was associated with stromal and intra-tumour TILs levels, as evaluated using HE, which predicted chemotherapy response in several breast cancer subtypes. Further studies are needed to perform stratification according to TILs-GS levels and the conventional breast cancer subtypes.
Abbreviations
- HR:
-
Hormone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- IHC:
-
Immunohistochemistry
- TILs:
-
Tumour-infiltrating lymphocytes
- HE:
-
Hematoxylin eosin
- ER:
-
Estrogen receptor
- NAC:
-
Neoadjuvant chemotherapy
- TN:
-
ER−/HER2−
- DEFS:
-
Distant event-free survival
- pCR:
-
Pathological complete response
- RD:
-
Residual disease
References
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M, Baehner FL, Walker MG, Watson D, Park T, Hiller W, Fisher ER, Wickerham DL, Bryant J, Wolmark N (2004) A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 351(27):2817–2826. doi:10.1056/NEJMoa041588
Sotiriou C, Pusztai L (2009) Gene-expression signatures in breast cancer. N Engl J Med 360(8):790–800. doi:10.1056/NEJMra0801289
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Perez EA, Olson JA Jr, Zujewski J, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Ravdin P, Keane MM, Gomez Moreno HL, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Atkins JN, Berenberg JL, Sledge GW (2015) Prospective validation of a 21-gene expression assay in breast cancer. N Engl J Med 373(21):2005–2014. doi:10.1056/NEJMoa1510764
Cardoso F, van’t Veer LJ, Bogaerts J, Slaets L, Viale G, Delaloge S, Pierga JY, Brain E, Causeret S, DeLorenzi M, Glas AM, Golfinopoulos V, Goulioti T, Knox S, Matos E, Meulemans B, Neijenhuis PA, Nitz U, Passalacqua R, Ravdin P, Rubio IT, Saghatchian M, Smilde TJ, Sotiriou C, Stork L, Straehle C, Thomas G, Thompson AM, van der Hoeven JM, Vuylsteke P, Bernards R, Tryfonidis K, Rutgers E, Piccart M, Investigators M (2016) 70-Gene signature as an aid to treatment decisions in early-stage breast cancer. N Engl J Med 375(8):717–729. doi:10.1056/NEJMoa1602253
Kondo M, Hoshi SL, Ishiguro H, Yoshibayashi H, Toi M (2008) Economic evaluation of 21-gene reverse transcriptase-polymerase chain reaction assay in lymph-node-negative, estrogen-receptor-positive, early-stage breast cancer in Japan. Breast Cancer Res Treat 112(1):175–187. doi:10.1007/s10549-007-9842-y
Tsoi DT, Inoue M, Kelly CM, Verma S, Pritchard KI (2010) Cost-effectiveness analysis of recurrence score-guided treatment using a 21-gene assay in early breast cancer. Oncologist 15(5):457–465. doi:10.1634/theoncologist.2009-0275
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, Martino S, Wang M, Jones VE, Saphner TJ, Wolff AC, Wood WC, Davidson NE, Sledge GW, Sparano JA, Badve SS (2014) Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol 32(27):2959–2966. doi:10.1200/JCO.2013.55.0491
Dieci MV, Mathieu MC, Guarneri V, Conte P, Delaloge S, Andre F, Goubar A (2015) Prognostic and predictive value of tumor-infiltrating lymphocytes in two phase III randomized adjuvant breast cancer trials. Ann Oncol 26(8):1698–1704. doi:10.1093/annonc/mdv239
West NR, Milne K, Truong PT, Macpherson N, Nelson BH, Watson PH (2011) Tumor-infiltrating lymphocytes predict response to anthracycline-based chemotherapy in estrogen receptor-negative breast cancer. Breast Cancer Res 13(6):R126. doi:10.1186/bcr3072
Ibrahim EM, Al-Foheidi ME, Al-Mansour MM, Kazkaz GA (2014) The prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancer: a meta-analysis. Breast Cancer Res Treat 148(3):467–476. doi:10.1007/s10549-014-3185-2
Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, Thurlimann B, Senn HJ, Panel M (2015) Tailoring therapies–improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol 26(8):1533–1546. doi:10.1093/annonc/mdv221
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S, International TWG (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26(2):259–271. doi:10.1093/annonc/mdu450
Varga Z, Diebold J, Dommann-Scherrer C, Frick H, Kaup D, Noske A, Obermann E, Ohlschlegel C, Padberg B, Rakozy C, Sancho Oliver S, Schobinger-Clement S, Schreiber-Facklam H, Singer G, Tapia C, Wagner U, Mastropasqua MG, Viale G, Lehr HA (2012) How reliable is Ki-67 immunohistochemistry in grade 2 breast carcinomas? A QA study of the Swiss Working Group of Breast- and Gynecopathologists. PLoS ONE 7(5):e37379. doi:10.1371/journal.pone.0037379
Polley MY, Leung SC, McShane LM, Gao D, Hugh JC, Mastropasqua MG, Viale G, Zabaglo LA, Penault-Llorca F, Bartlett JM, Gown AM, Symmans WF, Piper T, Mehl E, Enos RA, Hayes DF, Dowsett M, Nielsen TO, International Ki67 in Breast Cancer Working Group of the Breast International G, North American Breast Cancer G (2013) An international Ki67 reproducibility study. J Natl Cancer Inst 105(24):1897–1906. doi:10.1093/jnci/djt306
Swisher SK, Wu Y, Castaneda CA, Lyons GR, Yang F, Tapia C, Wang X, Casavilca SA, Bassett R, Castillo M, Sahin A, Mittendorf EA (2016) Interobserver agreement between pathologists assessing tumor-infiltrating lymphocytes (TILs) in breast cancer using methodology proposed by the International TILs Working Group. Ann Surg Oncol. doi:10.1245/s10434-016-5173-8
Hida AI, Ohi Y (2015) Evaluation of tumor-infiltrating lymphocytes in breast cancer; proposal of a simpler method. Ann Oncol 26(11):2351. doi:10.1093/annonc/mdv363
Symmans WF, Ayers M, Clark EA, Stec J, Hess KR, Sneige N, Buchholz TA, Krishnamurthy S, Ibrahim NK, Buzdar AU, Theriault RL, Rosales MF, Thomas ES, Gwyn KM, Green MC, Syed AR, Hortobagyi GN, Pusztai L (2003) Total RNA yield and microarray gene expression profiles from fine-needle aspiration biopsy and core-needle biopsy samples of breast carcinoma. Cancer 97(12):2960–2971. doi:10.1002/cncr.11435
Pusztai L, Ayers M, Stec J, Clark E, Hess K, Stivers D, Damokosh A, Sneige N, Buchholz TA, Esteva FJ, Arun B, Cristofanilli M, Booser D, Rosales M, Valero V, Adams C, Hortobagyi GN, Symmans WF (2003) Gene expression profiles obtained from fine-needle aspirations of breast cancer reliably identify routine prognostic markers and reveal large-scale molecular differences between estrogen-negative and estrogen-positive tumors. Clin Cancer Res 9(7):2406–2415
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, Rouas G, Francis P, Crown JP, Hitre E, de Azambuja E, Quinaux E, Di Leo A, Michiels S, Piccart MJ, Sotiriou C (2013) Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol 31(7):860–867. doi:10.1200/JCO.2011.41.0902
Gong Y, Yan K, Lin F, Anderson K, Sotiriou C, Andre F, Holmes FA, Valero V, Booser D, Pippen JE Jr, Vukelja S, Gomez H, Mejia J, Barajas LJ, Hess KR, Sneige N, Hortobagyi GN, Pusztai L, Symmans WF (2007) Determination of oestrogen-receptor status and ERBB2 status of breast carcinoma: a gene-expression profiling study. Lancet Oncol 8(3):203–211. doi:10.1016/S1470-2045(07)70042-6
Iwamoto T, Bianchini G, Booser D, Qi Y, Coutant C, Shiang CY, Santarpia L, Matsuoka J, Hortobagyi GN, Symmans WF, Holmes FA, O’Shaughnessy J, Hellerstedt B, Pippen J, Andre F, Simon R, Pusztai L (2011) Gene pathways associated with prognosis and chemotherapy sensitivity in molecular subtypes of breast cancer. J Natl Cancer Inst 103(3):264–272. doi:10.1093/jnci/djq524
Bianchini G, Iwamoto T, Qi Y, Coutant C, Shiang CY, Wang B, Santarpia L, Valero V, Hortobagyi GN, Symmans WF, Gianni L, Pusztai L (2010) Prognostic and therapeutic implications of distinct kinase expression patterns in different subtypes of breast cancer. Cancer Res 70(21):8852–8862. doi:10.1158/0008-5472.CAN-10-1039
Altman DG, Lausen B, Sauerbrei W, Schumacher M (1994) Dangers of using “optimal” cutpoints in the evaluation of prognostic factors. J Natl Cancer Inst 86(11):829–835
Gu-Trantien C, Loi S, Garaud S, Equeter C, Libin M, de Wind A, Ravoet M, Le Buanec H, Sibille C, Manfouo-Foutsop G, Veys I, Haibe-Kains B, Singhal SK, Michiels S, Rothe F, Salgado R, Duvillier H, Ignatiadis M, Desmedt C, Bron D, Larsimont D, Piccart M, Sotiriou C, Willard-Gallo K (2013) CD4(+) follicular helper T cell infiltration predicts breast cancer survival. J Clin Invest 123(7):2873–2892. doi:10.1172/JCI67428
Bianchini G, Qi Y, Alvarez RH, Iwamoto T, Coutant C, Ibrahim NK, Valero V, Cristofanilli M, Green MC, Radvanyi L, Hatzis C, Hortobagyi GN, Andre F, Gianni L, Symmans WF, Pusztai L (2010) Molecular anatomy of breast cancer stroma and its prognostic value in estrogen receptor-positive and -negative cancers. J Clin Oncol 28(28):4316–4323. doi:10.1200/JCO.2009.27.2419
Loi S, Michiels S, Salgado R, Sirtaine N, Jose V, Fumagalli D, Kellokumpu-Lehtinen PL, Bono P, Kataja V, Desmedt C, Piccart MJ, Loibl S, Denkert C, Smyth MJ, Joensuu H, Sotiriou C (2014) Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol 25(8):1544–1550. doi:10.1093/annonc/mdu112
Vinayak S, Gray R, Adams S (2014) Association of increased tumor-infiltrating lymphocytes (TILs) with immunomodulatory (IM) triple-negative breast cancer (TNBC) subtype and response to neoadjuvant platinum-based therapy in PrECOG0105. J Clin Oncol. doi:10.1200/JCO.2015.65.6595
Denkert C, von Minckwitz G, Brase JC, Sinn BV, Gade S, Kronenwett R, Pfitzner BM, Salat C, Loi S, Schmitt WD, Schem C, Fisch K, Darb-Esfahani S, Mehta K, Sotiriou C, Wienert S, Klare P, Andre F, Klauschen F, Blohmer JU, Krappmann K, Schmidt M, Tesch H, Kummel S, Sinn P, Jackisch C, Dietel M, Reimer T, Untch M, Loibl S (2015) Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol 33(9):983–991. doi:10.1200/JCO.2014.58.1967
Callari M, Cappelletti V, D’Aiuto F, Musella V, Lembo A, Petel F, Karn T, Iwamoto T, Provero P, Daidone MG, Gianni L, Bianchini G (2016) Subtype-specific metagene-based prediction of outcome after neoadjuvant and adjuvant treatment in breast cancer. Clin Cancer Res 22(2):337–345. doi:10.1158/1078-0432.CCR-15-0757
Hayes DF, Thor AD, Dressler LG, Weaver D, Edgerton S, Cowan D, Broadwater G, Goldstein LJ, Martino S, Ingle JN, Henderson IC, Norton L, Winer EP, Hudis CA, Ellis MJ, Berry DA, Cancer, Leukemia Group BI (2007) HER2 and response to paclitaxel in node-positive breast cancer. N Engl J Med 357(15):1496–1506. doi:10.1056/NEJMoa071167
Penault-Llorca F, Andre F, Sagan C, Lacroix-Triki M, Denoux Y, Verriele V, Jacquemier J, Baranzelli MC, Bibeau F, Antoine M, Lagarde N, Martin AL, Asselain B, Roche H (2009) Ki67 expression and docetaxel efficacy in patients with estrogen receptor-positive breast cancer. J Clin Oncol 27(17):2809–2815. doi:10.1200/JCO.2008.18.2808
Nitz U, Gluz O, Huober J, Kreipe HH, Kates RE, Hartmann A, Erber R, Scholz M, Lisboa B, Mohrmann S, Mobus V, Augustin D, Hoffmann G, Weiss E, Bohmer S, Kreienberg R, Du Bois A, Sattler D, Thomssen C, Kiechle M, Janicke F, Wallwiener D, Harbeck N, Kuhn W (2014) Final analysis of the prospective WSG-AGO EC-Doc versus FEC phase III trial in intermediate-risk (pN1) early breast cancer: efficacy and predictive value of Ki67 expression. Ann Oncol 25(8):1551–1557. doi:10.1093/annonc/mdu186
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, Swain SM, Prowell T, Loibl S, Wickerham DL, Bogaerts J, Baselga J, Perou C, Blumenthal G, Blohmer J, Mamounas EP, Bergh J, Semiglazov V, Justice R, Eidtmann H, Paik S, Piccart M, Sridhara R, Fasching PA, Slaets L, Tang S, Gerber B, Geyer CE Jr, Pazdur R, Ditsch N, Rastogi P, Eiermann W, von Minckwitz G (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384(9938):164–172. doi:10.1016/S0140-6736(13)62422-8
Perez EA, Thompson EA, Ballman KV, Anderson SK, Asmann YW, Kalari KR, Eckel-Passow JE, Dueck AC, Tenner KS, Jen J, Fan JB, Geiger XJ, McCullough AE, Chen B, Jenkins RB, Sledge GW, Winer EP, Gralow JR, Reinholz MM (2015) Genomic analysis reveals that immune function genes are strongly linked to clinical outcome in the North Central Cancer Treatment Group n9831 Adjuvant Trastuzumab Trial. J Clin Oncol 33(7):701–708. doi:10.1200/JCO.2014.57.6298
Salgado R, Denkert C, Campbell C, Savas P, Nuciforo P, Aura C, de Azambuja E, Eidtmann H, Ellis CE, Baselga J, Piccart-Gebhart MJ, Michiels S, Bradbury I, Sotiriou C, Loi S (2015) Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO TRIAL. JAMA Oncol 1(4):448–454. doi:10.1001/jamaoncol.2015.0830
Dushyanthen S, Beavis PA, Savas P, Teo ZL, Zhou C, Mansour M, Darcy PK, Loi S (2015) Relevance of tumor-infiltrating lymphocytes in breast cancer. BMC Med 13:202. doi:10.1186/s12916-015-0431-3
Perez EA, Ballman KV, Tenner KS, Thompson EA, Badve SS, Bailey H, Baehner FL (2016) Association of stromal tumor-Infiltrating lymphocytes with recurrence-free survival in the N9831 adjuvant trial in patients with early-stage HER2-positive breast cancer. JAMA Oncol 2(1):56–64. doi:10.1001/jamaoncol.2015.3239
Ghiringhelli F, Apetoh L, Tesniere A, Aymeric L, Ma Y, Ortiz C, Vermaelen K, Panaretakis T, Mignot G, Ullrich E, Perfettini JL, Schlemmer F, Tasdemir E, Uhl M, Genin P, Civas A, Ryffel B, Kanellopoulos J, Tschopp J, Andre F, Lidereau R, McLaughlin NM, Haynes NM, Smyth MJ, Kroemer G, Zitvogel L (2009) Activation of the NLRP3 inflammasome in dendritic cells induces IL-1beta-dependent adaptive immunity against tumors. Nat Med 15(10):1170–1178. doi:10.1038/nm.2028
Umansky V, Sevko A (2012) Overcoming immunosuppression in the melanoma microenvironment induced by chronic inflammation. Cancer Immunol Immunother 61(2):275–282. doi:10.1007/s00262-011-1164-6
Ma Y, Adjemian S, Mattarollo SR, Yamazaki T, Aymeric L, Yang H, Portela Catani JP, Hannani D, Duret H, Steegh K, Martins I, Schlemmer F, Michaud M, Kepp O, Sukkurwala AQ, Menger L, Vacchelli E, Droin N, Galluzzi L, Krzysiek R, Gordon S, Taylor PR, Van Endert P, Solary E, Smyth MJ, Zitvogel L, Kroemer G (2013) Anticancer chemotherapy-induced intratumoral recruitment and differentiation of antigen-presenting cells. Immunity 38(4):729–741. doi:10.1016/j.immuni.2013.03.003
Dunbier AK, Ghazoui Z, Anderson H, Salter J, Nerurkar A, Osin P, A’Hern R, Miller WR, Smith IE, Dowsett M (2013) Molecular profiling of aromatase inhibitor-treated postmenopausal breast tumors identifies immune-related correlates of resistance. Clin Cancer Res 19(10):2775–2786. doi:10.1158/1078-0432.CCR-12-1000
Schreiber RD, Old LJ, Smyth MJ (2011) Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 331(6024):1565–1570. doi:10.1126/science.1203486
Fan C, Oh DS, Wessels L, Weigelt B, Nuyten DS, Nobel AB, van’t Veer LJ, Perou CM (2006) Concordance among gene-expression-based predictors for breast cancer. N Engl J Med 355(6):560–569. doi:10.1056/NEJMoa052933
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2017_4502_MOESM1_ESM.pptx
Supplementry Fig. 1. Kaplan-Meier curves according to tumour-infiltrating lymphocytes gene signatures in the tamoxifen-treated data set. Kaplan-Meier curves for (a) luminal-low and (b) luminal-high breast cancer were compared using the log-rank test. Hazard ratios (HR) and 95% confidence intervals (CIs) for distant event-free survival were estimated using Cox regression analysis. Supplementry Fig. 2. Neoadjuvant therapy responses and tumour-infiltrating lymphocytes gene signatures among HER2 + cases in the trastuzumab-treated data set. The boxplots show the associations between tumour-infiltrating lymphocytes gene signatures (TILs-GS) and neoadjuvant therapy response. P-values were calculated using Wilcoxon’s test. pCR pathological complete response, RD residual disease. Supplementary material 1 (PPTX 86 kb)
Rights and permissions
About this article
Cite this article
Kochi, M., Iwamoto, T., Niikura, N. et al. Tumour-infiltrating lymphocytes (TILs)-related genomic signature predicts chemotherapy response in breast cancer. Breast Cancer Res Treat 167, 39–47 (2018). https://doi.org/10.1007/s10549-017-4502-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4502-3