Abstract
Purpose
Although gene expression profiling provides critical information, knowledge remains limited regarding the differential effects of molecular subtype on clinical course. This study evaluated the impact of molecular status on long-term patterns of failure in patients with non-metastatic breast cancer.
Methods
We analyzed data from 1181 individuals with invasive breast cancer undergoing surgery plus PORT from 2003 to 2011. Molecular subtypes were defined as luminal A (LA), luminal B (LB)-HER2(−), LB-HER2(+), HER2, and triple-negative (TN) based on the 2013 St. Gallen Consensus criteria. Competing risks analysis and baseline hazard rate function plots were used to explore subtype-specific recurrence patterns.
Results
The 10-year overall survival rates of LA, LB-HER2(−), LB-HER2(+), HER2, and TN groups were 96, 93, 94, 84, and 85%, respectively (P < 0.001). Distant metastatic events differed significantly according to molecular subtype (P < 0.001). In competing risks regression analysis, initial development of distant metastasis was the highest with TN tumors, followed by HER2, LB-HER2(−), and LB-HER2(+) subtypes (P = 0.005). Regarding preferential sites of distant metastasis, the risk of initial brain metastasis was significantly higher with HER2 tumors, followed by TN tumors (P = 0.001). A low-level but sustained metastatic risk increment was observed in luminal tumors, whereas TN and HER2 subtypes showed a short-term risk surge within 5 years.
Conclusion
From the significant impact of molecular profile on distant metastasis, subtype-specific individualization of systemic treatment and close surveillance are suggested. The preferential and long-term risk of brain metastasis in the HER2 subtype underlines the importance of alternative anti-HER2 therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a heterogeneous malignancy representing diverse clinical presentation, tumor aggressiveness, treatment responsiveness, and prognosis [1]. In addition to representative clinicopathological factors—including Tumor, Node, and Metastasis (TNM) stage, type of histology, tumor grade, and tumor markers—gene expression profiling has been used to determine the appropriate treatment strategy and predict survival [2, 3]. Above all, immunohistochemistry (IHC) analyses of estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and Ki-67 have been essential in the diagnosis of breast cancer, dividing tumors into luminal A (LA), luminal B (LB)-HER2(−), LB-HER2(+), HER2, and triple-negative (TN) subtypes [4]. These molecular signatures have provided information on the distinct biologic features and response to systemic, targeted, and endocrine treatment, allowing for prediction of differential risks of tumor relapse and mortality [5].
In luminal tumors, selective estrogen receptor modulators (SERMs) or aromatase inhibitors are preferentially considered [6]. The best prognosis occurs with LA tumors. LB tumors, even with the use of endocrine therapy, have been associated with a higher risk of relapse than LA tumors [7]. The basal-like subtype has an aggressive disease course, without a definite targeted modality [8]. The HER2-enriched subtype, representing HER2 amplification and/or overexpression, has a worse prognosis, but the use of trastuzumab, an anti-HER2 agent, has significantly improved survival outcomes [9]. Despite recent advances in systemic treatment, HER2 and TN tumors still exhibit shorter survival than the luminal subtypes [10]. Because of the shortcomings of trastuzumab, such as its limited ability to penetrate the blood–brain barrier and the development of resistance, there are ongoing studies to evaluate treatment efficacy of alternative anti-HER2 agents [11].
Nevertheless, knowledge about the preferential patterns of failure according to molecular subtype is limited. Because of the heterogeneity of study populations and analytic methods, consensus has not been established. In this study, we evaluated long-term survival outcomes and types of recurrences according to molecular status in patients with breast cancer who received postoperative radiotherapy (PORT). Competing risks analysis was used to assess relapse behavior, including identifying potential organ-selective characteristics determined by the molecular profiles. This study revealed a subtype-specific predisposition to metastasis, thus providing useful clinical and prognostic information in the contemporary era.
Materials and methods
Population and study design
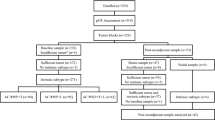
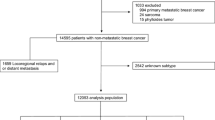
This study reviewed data from a total of 1181 patients with stage I–III breast cancer who underwent postoperative adjuvant radiotherapy in Seoul National University Bundang Hospital between 2003 and 2011. Patients with (1) clinical M1 stage, (2) prior diagnosis of another malignancy, (3) refusal of systemic or endocrine treatment, or (4) insufficient follow-up duration (<1 year) were excluded. After obtaining approval from our Institutional Review Board (B-1505/298-116), patient, tumor, and treatment-related demographic and clinicopathologic data, as well as survival outcomes, were collected from our electronic medical records.
Definition of molecular subtypes
Based on IHC results of ER, PR, HER2, and Ki-67, molecular subtypes were classified into LA, LB-HER2(−), LB-HER2(+), HER2, and TN according to the 2013 St. Gallen Consensus criteria [4]. HER2-positivity was defined by the presence of c-erbB-2 overexpression with an IHC score of 3 or a c-erbB-2 IHC score of 2 with positive HER2 gene amplification on fluorescence in situ hybridization. Ki-67 expression level was divided into low (<14%) or high (≥14%) labeling index. The definitions of molecular subtypes were as follows: LA group for ER(+), PR(+), HER2(−), and low Ki-67 expression; LB-HER2(−) group for ER(+), HER2(−), and at least high Ki-67 expression or PR(−); LB-HER2(+) group for ER(+) and HER2(+); HER2 group for ER(−), PR(−), and HER2(+); and TN group for ER(−), PR(−), and HER2(−).
Patterns of failure events
Initial recurrence events were categorized as ipsilateral breast or chest wall, regional lymphatics, contralateral breast or chest wall, or distant metastasis. Regional lymphatic spread included ipsilateral axillary level I, II, or III, supraclavicular, or internal mammary lymph nodes. Organ-specific sites of distant metastatic failure were categorized as (1) distant lymph nodes (lymphatic spread other than regional lymphatic recurrence), (2) lung and/or pleura, (3) liver, (4) bone, or (5) brain and/or leptomeningeal seeding (LMS).
Statistical analysis
Baseline clinicopathological data were categorized, and differences in variables according to molecular subtypes were evaluated with the χ 2 test. The clinical endpoints of this study were overall survival (OS) and disease-free interval (DFI), defined as the time interval between initiation of treatment and overall death or tumor relapse, respectively. Kaplan–Meier analysis with a log-rank test was used to assess differences in survival outcomes. Incidences of site-specific recurrence events according to molecular subtypes were evaluated using the linear-by-linear association. The 10-year site-specific failure risk rates were estimated using competing risks analysis with the Grey’s test. After adjustment for related prognostic factors identified from Cox proportional hazards regression, the subdistribution hazard ratios (sHRs) and 95% confidence intervals (CIs) were calculated using competing risks regression with the Wald test. Multivariate regression models included variables with P < 0.1 in the univariate analysis. Two-sided P-values less than 0.05 were designated as statistically significant. The statistical analyses were performed using IBM SPSS Statistics 22.0 (IBM, Armonk, NY, USA) and R version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics
Table 1 presents baseline patient-, tumor-, and treatment-related characteristics of the study population. According to the 2013 St. Gallen Consensus definitions, the tumors of 446 (38%), 253 (21%), 131 (11%), 123 (10%), and 228 (19%) patients were classified as LA, LB-HER2(−), LB-HER2(+), HER2, and TN breast cancers, respectively. Significant differences according to molecular subtype were observed for age, T stage, N stage, summarized American Joint Committee on Cancer (AJCC) stage, type of primary surgery, axillary lymph node dissection, and use of chemotherapy (P < 0.001 for all comparisons). Young age (<40 years) was more common in TN tumors (33%) than in other subtypes. Early-stage diseases, such as T1–2 and node-negative tumors, were more commonly observed in the LA subtype (94 and 61%, respectively). The proportion of advanced AJCC stage III tumors was the highest in HER2 tumors (46%), followed by LB-HER2(+) cancers (31%). Considering the type of primary surgery, mastectomy was the most commonly performed in patients with HER2 cancer (42%), followed by the LB (24%) and TN (18%) subtypes. The frequency of axillary lymph node dissection was the highest with the HER2 subtype (61%), and chemotherapy was less commonly administered in patients with an LA (59%) tumor.
Outcome analysis
Supplementary Fig. 1 represents Kaplan–Meier survival curves of OS and DFI. With a median follow-up duration of 76 months, there were significant differences in OS and DFI according to molecular subtype (P < 0.001 for both comparisons). The 10-year OS rates of patients with HER2 (84.2%) and TN (84.9%) tumors were inferior to those of patients with LA (96.2%), LB-HER2(−) (93.2%), and LB-HER2(+) (93.9%) subtypes. The 10-year DFI rate of patients with an LA tumor was 90.4%, which was higher than that of patients with LB-HER2(−) (81.0%), LB-HER2(+) (87.0%), HER2 (72.6%), and TN (78.4%) subtypes.
Recurrence events
Supplementary Table 1 lists the incidence of initial site-specific recurrences in relation to molecular subtype, counting simultaneous events involving different organs separately. The recurrence events were categorized as ipsilateral breast or chest wall, regional lymphatics, contralateral breast or chest wall, and distant metastasis, and the sites of distant metastatic failure were bone, lung and/or pleura, distant lymph nodes, liver, and brain and/or LMS. Ipsilateral breast or chest wall recurrence was the highest in the TN subtype (16%). Regional lymphatic failure was the highest with the HER2 (22%) and TN (19%) subtypes, followed by LB-HER2(−) (15%), LB-HER2(+) (14%), and LA (7%) cancers. Higher proportions of bone metastasis were observed for luminal tumors, occurring in 21% of LB and 18% of LA subtypes, compared with HER2 (9%) and TN (8%) cancers. The frequency of initial tumor spread with brain metastasis and/or LMS was the highest with HER2 (9%) tumors, followed by TN (3%) cancers. The overall distributions of recurrence events according to different molecular subtypes were not significantly different (P = 0.548).
Patterns of recurrence
Table 2 shows the 10-year failure risk rates for different types of recurrences based on competing risks analysis. When the events were classified into ipsilateral breast or chest wall, regional lymphatic, contralateral breast or chest wall, and distant metastasis, significant differences in relation to molecular subtypes were observed in distant metastasis (P < 0.001). In univariate analysis, the 10-year failure risk rates of distant metastatic failure were the highest with the HER2 (13.4%) and TN (11.5%) subtypes, followed by LB-HER2(−) (9.0%), LB-HER2(+) (8.6%), and LA (3.2%) tumors. There was no significant difference in ipsilateral breast or chest wall recurrence according to molecular subtype (P = 0.435). For regional lymphatic and contralateral breast or chest wall recurrence, trends that did not reach statistical significance were observed (P = 0.072 and 0.085, respectively).
To evaluate the impact of molecular subtypes on patterns of recurrence, other potentially associated covariates, such as age and/or TN stage, were adjusted in the competing risks regression analysis. Statistical significance was not achieved in the multivariate analysis of patterns of regional lymphatic and contralateral breast or chest wall recurrences according to subtype (P = 0.270 and 0.130, respectively), whereas an independent effect of subtype on distant metastatic failure was observed (P = 0.005) (Table 3). Compared with the LA subtype, the metastatic risk was the highest with TN (sHR 3.74, 95% CI 1.79–7.81) tumors, followed by HER2 (sHR 3.05, 95% CI 1.37–6.78), LB-HER2(−) (sHR 2.64, 95% CI 1.29–5.40), and LB-HER2(+) (sHR 1.55, 95% CI 0.64–3.74) subtypes. When metastatic events were subcategorized according to specific organ sites, the 10-year failure risk rate of brain metastasis was the highest with HER2 tumors (3.5%), followed by the TN (0.9%) subtype (P = 0.001) (Table 4). No statistically significant differences were observed in other sites, including distant lymph nodes, lung and/or pleura, liver, or bone (P = 0.173, 0.104, 0.099, and 0.197, respectively).
Figure 1 represents baseline hazard function plots for distant metastasis. For the LA subtype, the hazard rate was estimated at a relatively low level, which was maintained until 7–8 years of follow-up. There was an initial risk increase within 5 years with LB tumors; an additional late peak was observed after 7 years with LB-HER2(+) but not LB-HER2(−) tumors. Although non-luminal tumors commonly showed early peaks of risk surge within 3–4 years, the HER2 subtype showed a distinctive late risk increment that appeared beyond 5 years of follow-up. For brain metastasis in the HER2 subgroup, an initial peak around 3 years of follow-up was observed. However, an additional second peak after 5 years of follow-up was observed in trastuzumab-treated tumors (Fig. 2).
Discussion
We explored the long-term prognosis and patterns of recurrence according to molecular subtype in Korean patients with breast cancer. Significant outcome differences in OS and DFI were observed in relation to the LA, LB-HER2(−), LB-HER2(+), HER2, and TN subtypes. When recurrence events were classified into ipsilateral breast or chest wall, regional lymphatic, contralateral breast or chest wall, and distant metastasis, the TN and HER2 subtypes were associated with significantly greater distant metastatic failure risks in competing risks analysis. In organ-specific evaluation, the 10-year failure risk rate of initial brain metastasis and/or LMS was the highest with the HER2 subtype, followed by TN tumors. Considering the subtype-specific time course of distant metastatic failure, we observed a low-level but sustained long-term risk with LA tumors and a short-term early risk surge with the TN and HER2 subtypes. In addition, HER2-positive tumors, including both LB-HER2(+) and pure HER2-enriched cancers, commonly showed second late peaks after 7 years of follow-up.
In this study, competing risks analysis was used to analyze detailed patterns of initial tumor spread of patients with recurrence. This method considers other types of events as competing risks while calculating conditional probabilities of the event of interest [12, 13]. In competing risks regression, the independent effect of the molecular status on tumor relapse was elucidated, adjusting for potentially related covariates [14]. Because of the relatively long-term survival of patients with breast cancer in general, evaluation of recurrence profiles is crucial to predict prognosis. Since the systemic and/or endocrine therapy of analyzed patients was recommended based on their IHC findings, our results are representative of failure patterns in current routine clinical practice.
Competing risks regression demonstrated that molecular status did not affect ipsilateral breast or chest wall or regional lymphatic recurrences. Nevertheless, TN and HER2 tumors exhibited greater risks of distant metastatic failure, compared with LA tumors. In an analysis of tumors treated with breast-conservation surgery (n = 1177) and mastectomy (n = 1512), the LA subtype was associated with significantly lower probabilities of local or regional relapse (P = 0.005 and < 0.001 for local; P < 0.001 and < 0.001 for regional, respectively) [15]. A Korean study also demonstrated significant differences in local and nodal failure risk rates favoring the LA subtype (P = 0.026 and 0.004, respectively) [16]. However, the current study was unique in that we exclusively analyzed a study population who completed PORT, while prior investigations included a significant proportion of non-PORT patients [15–18]. In Haffty et al.’s analysis of 482 patients who underwent PORT after breast-conserving surgery, the TN subtype (n = 117) was associated with a significantly lower 5-year distant metastasis-free rate (P = 0.002) but no significant differences in breast (P = 0.823) or nodal (P = 0.05) relapse-free rates [19]. In another study (n = 498), neither ER-positivity nor PR-positivity was significantly associated in a Cox proportional hazards model with ipsilateral breast tumor recurrence after breast-conserving therapy (P = 0.754 and 0.798, respectively) [20]. Taken together, in this study, the potentially enhanced tumor control at the ipsilateral local or regional sites after completion of PORT might contribute to the weak association between molecular subtypes and locoregional recurrence risks. Meanwhile, it was notable that the contribution of molecular subtypes to the risk of metastatic failure remained even after adjusting for age and tumor stage. Importantly, this study revealed the subtype-based differential susceptibility to distant metastasis in the contemporary era of breast cancer treatment.
Several previous reports have explored the subtype-related preferential sites of distant metastasis [16, 21–26]. However, their results were inconsistent. Although a potential bone-seeking phenotype of luminal tumors has been suggested [21–24], some reports could not verify this tendency [16, 25]. In the study by Sihto et al. of 234 patients diagnosed with distant metastasis as the first site of failure, the authors found higher frequencies of liver (27.1%) and lung (22.9%) metastases in patients with HER2 tumors and higher frequencies of lung (20.8%) and brain (9.5%) metastases in patients with basal-like tumors [21]. In a recent Chinese analysis, patients with hormone receptor-positive/HER2(+) and hormone receptor-negative/HER2(+) tumors were more prone to abdominal or pelvic metastasis, compared to patients with a hormone receptor-positive/HER2(−) tumor [adjusted odds ratio (aOR) 1.665, 95% CI 1.096–2.530; aOR 1.971, 95% CI 1.244–3.124, respectively] [26]. An early bioinformatics study found an association of Wnt signaling and focal adhesion factors with molecular subtypes and relapsed organs [27]. Given these diverse clinical results and the molecular complexity of this issue [28], current understanding of the metastatic behavior for specific organ sites according to molecular subtypes is incomplete.
Our results demonstrated a significantly higher risk of initial brain metastasis in patients with the HER2 subtype but no significant subtype-related tendency in other distant sites. Musolino et al. showed that HER2-positive molecular status and use of trastuzumab were significantly associated with an increased initial [hazard ratio (HR) 15, 95% CI 6.6–20.5; P < 0.001] or cumulative (HR 4.3, 95% CI 1.5–11.8; P = 0.005) brain metastatic failure [29]. Some studies have reported a relatively higher incidence of brain metastasis in patients with the HER2 subtype [30–32], and biological evidence has demonstrated the HER2-related predisposition to brain metastatic failure [33, 34]. When we additionally evaluated the time course of brain metastasis in patients with the HER2 subtype, trastuzumab-treated patients presented an additional risk increment at approximately 7 years of follow-up, compared with the short-term risk only within 5 years in those patients not treated with trastuzumab. Although the widespread use of trastuzumab, an anti-HER2 agent, has reduced disease-specific mortality associated with the HER2 subtype [35], its molecular weight is too high to penetrate the blood–brain barrier [36]. Our results reflect the limited function of trastuzumab in preventing tumor spread to the central nervous system, thus underlining the need for alternative anti-HER2 strategies. A recent ongoing trial of lapatinib plus whole brain radiotherapy should provide insight into a possible targeted approach to overcome the blood–brain barrier (NCT01622868) [37].
The baseline hazard rate function plots demonstrated the time-course patterns of distant metastasis according to intrinsic molecular subtypes. In the study of Ribelles et al., the risk associated with luminal tumors was maintained for a prolonged time at a relatively low level, whereas TN and HER2 subtypes commonly exhibited short-term risk peaks [38]. Nevertheless, the results were inconclusive because a large number of patients who did not complete the treatment (systemic or targeted regimen) were included in the analysis. Under contemporary treatment recommendations in our clinic, we verified several time-course characteristics of the different subtypes of tumors, such as a low-level but sustained risk for LA tumors, a short-term risk increment with the LB subtype, an early high-level risk surge with TN and HER2 tumors, and late second peaks commonly observed with both LB-HER2(+) and pure HER2-enriched tumors. We thus hypothesize that HER2 overexpression and/or amplification might be a factor related to the development of late metastatic behavior. More customized approaches of systemic treatment and close surveillance taking into consideration the gene expression profile should be established to prevent potential metastatic tumor spread. Further investigations are required to determine the clinical and biological implications of HER2-positivity.
Several limitations exist in this study. Our data should be interpreted with caution because of the potential selection bias induced by its retrospective design. Although uniform inclusion criteria were applied to identify eligible patients, heterogeneity of clinicopathological characteristics was inevitable. Since this study represents long-term outcomes, changes in systemic treatment regimens or indications during the time course of the study could not be fully considered. However, the strategy for each patient was based on contemporary guidelines, excluding patients who refused recommended treatment. Failure events were classified in detail, considering the chronological order.
In this study, we identified preferential relapse patterns of different molecular subtypes, analyzing a large cohort of breast cancer patients who completed PORT. In addition to observing a strong association between IHC profiles and distant metastatic failure, we also found that the HER2 subtype was associated with the greatest risk of initial brain metastasis. Subtype-specific time-course patterns of distant metastasis were notable, thus suggesting the need for further individualization of systemic treatment and close surveillance. Since the use of trastuzumab in the HER2 tumors did not achieve long-term prevention of distant failure in the brain, other possible anti-HER2 strategies should be established.
Conclusions
We confirmed the differential predisposition to distant metastasis according to molecular subtype of breast cancer. Among multiple organ sites, the preferential behavior of initial brain metastasis was observed with the HER2 subtype. By calculating the baseline hazard rate of each subgroup, we identified subtype-specific time-course patterns of metastatic failure. These findings suggest the need for individualized systemic treatment strategies and long-term close surveillance taking into consideration the molecular profiles. Further large-scale or multi-institutional studies are necessary to confirm and expand our findings.
References
Weigelt B, Baehner FL, Reis-Filho JS (2010) The contribution of gene expression profiling to breast cancer classification, prognostication and prediction: a retrospective of the last decade. J Pathol 220:263–280
van de Vijver MJ, He YD, van’t Veer LJ et al (2002) A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 347:1999–2009
Sotiriou C, Neo SY, McShane LM et al (2003) Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci USA 100:10393–10398
Goldhirsch A, Winer EP, Coates AS et al (2013) Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol 24:2206–2223
Yersal O, Barutca S (2014) Biological subtypes of breast cancer: prognostic and therapeutic implications. World J Clin Oncol 5:412–424
National Comprehensive Cancer Network® (2016) Breast Cancer. Version 2.2016. In: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 10 Mar 2017
Tran B, Bedard PL (2011) Luminal-B breast cancer and novel therapeutic targets. Breast Cancer Res 13:221
Anders C, Carey LA (2008) Understanding and treating triple-negative breast cancer. Oncology 22:1233–1239
Ross JS, Slodkowska EA, Symmans WF et al (2009) The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist 14:320–368
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Loibl S, Gianni L (2016) HER2-positive breast cancer. Lancet. doi:10.1016/S0140-6736(16)32417-5
Satagopan JM, Ben-Porat L, Berwick M (2004) A note on competing risks in survival data analysis. Br J Cancer 91:1229–1235
Scrucca L, Santucci A, Aversa F (2007) Competing risk analysis using R: an easy guide for clinicians. Bone Marrow Transplant 40:381–387
Scrucca L, Santucci A, Aversa F (2010) Regression modeling of competing risk using R: an in depth guide for clinicians. Bone Marrow Transplant 45:1388–1395
Voduc KD, Cheang MC, Tyldesley S et al (2010) Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 28:1684–1691
Lee Y, Kang E, Lee AS et al (2015) Outcomes and recurrence patterns according to breast cancer subtypes in Korean women. Breast Cancer Res Treat 151:183–190
Hennigs A, Riedel F, Gondos A et al (2016) Prognosis of breast cancer molecular subtypes in routine clinical care: a large prospective cohort study. BMC Cancer 16:734
Shim HJ, Kim SH, Kang BJ et al (2014) Breast cancer recurrence according to molecular subtype. Asian Pac J Cancer Prev 15:5539–5544
Haffty BG, Yang Q, Reiss M et al (2006) Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol 24:5652–5657
Millar EK, Graham PH, O’Toole SA et al (2009) Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol 27:4701–4708
Sihto H, Lundin J, Lundin M et al (2011) Breast cancer biological subtypes and protein expression predict for the preferential distant metastasis sites: a nationwide cohort study. Breast Cancer Res 13:R87
Soni A, Ren Z, Hameed O et al (2015) Breast cancer subtypes predispose the site of distant metastases. Am J Clin Pathol 143:471–478
Alqaisi A, Chen L, Romond E et al (2014) Impact of estrogen receptor (ER) and human epidermal growth factor receptor-2 (HER2) co-expression on breast cancer disease characteristics: implications for tumor biology and research. Breast Cancer Res Treat 148:437–444
Kaplan MA, Arslan UY, Isikdogan A et al (2016) Biological subtypes and distant relapse pattern in breast cancer patients after curative surgery (Study of anatolian society of medical oncology). Breast Care 11:248–252
Park HS, Kim S, Kim K et al (2012) Pattern of distant recurrence according to the molecular subtypes in Korean women with breast cancer. World J Surg Oncol 10:4
Wu SG, Sun JY, Yang LC et al (2016) Patterns of distant metastasis in Chinese women according to breast cancer subtypes. Oncotarget 7:47975–47984
Smid M, Wang Y, Zhang Y et al (2008) Subtypes of breast cancer show preferential site of relapse. Cancer Res 68:3108–3114
Kimbung S, Loman N, Hedenfalk I (2015) Clinical and molecular complexity of breast cancer metastases. Semin Cancer Biol 35:85–95
Musolino A, Ciccolallo L, Panebianco M et al (2011) Multifactorial central nervous system recurrence susceptibility in patients with HER2-positive breast cancer: epidemiological and clinical data from a population-based cancer registry study. Cancer 117:1837–1846
Kennecke H, Yerushalmi R, Woods R et al (2010) Metastatic behavior of breast cancer subtypes. J Clin Oncol 28:3271–3277
Gaedcke J, Traub F, Milde S et al (2007) Predominance of the basal type and HER-2/neu type in brain metastasis from breast cancer. Mod Pathol 20:864–870
Gabos Z, Sinha R, Hanson J et al (2006) Prognostic significance of human epidermal growth factor receptor positivity for the development of brain metastasis after newly diagnosed breast cancer. J Clin Oncol 24:5658–5663
Palmieri D, Bronder JL, Herring JM et al (2007) Her-2 overexpression increases the metastatic outgrowth of breast cancer cells in the brain. Cancer Res 67:4190–4198
Yonemori K, Tsuta K, Ono M et al (2010) Disruption of the blood brain barrier by brain metastases of triple-negative and basal-type breast cancer but not HER2/neu-positive breast cancer. Cancer 116:302–308
Romond EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Koo T, Kim IA (2016) Brain metastasis in human epidermal growth factor receptor 2-positive breast cancer: from biology to treatment. Radiat Oncol J 34:1–9
Whole-brain radiation therapy or stereotactic radiosurgery with or without lapatinib ditosylate in treating patients with brain metastasis from HER2-positive breast cancer. In: ClinicalTrials.gov. National Institutes of Health. https://clinicaltrials.gov/ct2/show/NCT01622868?term=01622868&rank=1. Accessed 10 Mar 2017
Ribelles N, Perez-Villa L, Jerez JM et al (2013) Pattern of recurrence of early breast cancer is different according to intrinsic subtype and proliferation index. Breast Cancer Res 15:R98
Acknowledgements
This work supported by grants from the Korean Ministry of Health and Welfare and to Kim IA (No. 0820010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Institutional Review Board (B-1505/298-116). The retrospective design exempted this study from the requirement to obtain written informed consent from the patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lim, Y.J., Lee, SW., Choi, N. et al. Failure patterns according to molecular subtype in patients with invasive breast cancer following postoperative adjuvant radiotherapy: long-term outcomes in contemporary clinical practice. Breast Cancer Res Treat 163, 555–563 (2017). https://doi.org/10.1007/s10549-017-4206-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4206-8