Abstract
The aim of the present study is to determine if body mass index (BMI) during childhood is associated with the breast cancer risk factor ‘adult mammographic density adjusted for age and BMI’. In 1968, the Tasmanian Longitudinal Health Study studied every Tasmanian school child born in 1961. We obtained measured heights and weights from annual school medical records across ages 7–15 years and imputed missing values. Between 2009 and 2012, we administered to 490 women a questionnaire that asked current height and weight and digitised at least one mammogram per woman. Absolute and percent mammographic densities were measured using the computer-assisted method CUMULUS. We used linear regression and adjusted for age at interview and log current BMI. The mammographic density measures were negatively associated: with log BMI at each age from 7 to 15 years (all p < 0.05); with the average of standardised log BMIs across ages 7–15 years (p < 0.0005); and more strongly with standardised log BMI measures closer to age 15 years (p < 0.03). Childhood BMI measures explained 7 and 10 % of the variance in absolute and percent mammographic densities, respectively, and 25 and 20 % of the association between current BMI and absolute and percent mammographic densities, respectively. Associations were not altered by adjustment for age at menarche. There is a negative association between BMI in late childhood and the adult mammographic density measures that predict breast cancer risk. This could explain, at least in part, why BMI in adolescence is negatively associated with breast cancer risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
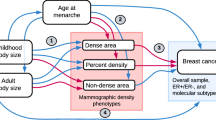
Mammographic density refers to the white and bright regions on a mammogram. The area covered by these regions is referred to as absolute mammographic density, and when presented as a proportion of the total area of the breast image on the mammogram it is referred to as percent mammographic density. Prospective studies of large cohorts of women undertaking mammographic screening have consistently found that, for women of the same age and body mass index (BMI), those with greater absolute or percent mammographic density are at greater risk of breast cancer [1].
Given mammographic density decreases with both age and BMI (i.e. has a negative association), while breast cancer risk increases with both age and BMI (i.e. has a positive association) [2, 3], these studies typically matched for age and adjusted for BMI, as well as other measured breast cancer risk factors. In recognition of this, we use the expression ‘mammographic density measures that predict breast cancer risk’ to describe ‘mammographic density measures adjusted for age and BMI’. This issue is most important when considering percent mammographic density because BMI is highly negatively correlated with that measure (typically r ~ −0.5) but less so for absolute mammographic density (typically r ~ −0.1) [2].
The associations between a particular measure that predicts risk and other risk factors can give insight into how and why that measure is implicated in risk. For example, having a family history of breast cancer is positively associated with age- and BMI-adjusted mammographic density measures [4]. Twin and family studies suggest that about 60 % of the variance in the age- and BMI-adjusted mammographic density measures could be due to genetic factors [2, 5, 6]. From the above, it has been estimated that about 10 % of the genetic factors that cause breast cancer also cause variation in the mammographic density measures that predict breast cancer risk. Empirical evidence to support this has now emerged from studying the common genetic variants recently found to be associated with breast cancer risk [7, 8].
Therefore, studying the determinants of the mammographic density measures that predict breast cancer risk could provide information about breast cancer aetiology. In particular, it might reveal the role of factors in earlier life, especially if those putative predictors were measured at the time rather than relying on retrospective self-report.
We have used the Tasmanian Longitudinal Health Study (TAHS), which studied 7-year-old children in 1968 and collected their subsequent school medical records, to estimate the associations between measured growth at ages 7–15 years and the mammographic density measures of women aged in their late 40 s that predict their subsequent breast cancer risk.
Methods
Subjects
We studied women who participated in the Tasmanian Longitudinal Health Study (TAHS) which commenced in 1968 as a survey of 99 % of all 7-year-old children attending school in Tasmania (i.e. born around 1961). TAHS participants have been followed up regularly and 56 % of the 8583 participants (4191 females) were located 36 years after the initial survey [9, 10]. Between October 2009 and January 2012 (when TAHS participants were aged 47–50), we approached 1967 women who, based on our last contact, might still be living in Tasmania and asked if they would be interested in the study, and if they had a mammogram (or if not, would be willing to have one). While the government-funded BreastScreen Tasmania approaches only women over the age of 50 to have a free mammogram, women in their 40 s can have a mammogram should they wish. BreastScreen Tasmania services are situated in the major population centres, with a mobile service that covers the rural areas once every 2 years. Of those mailed, 1266 (64 %) replied and of those, 401 (32 %) refused or withdrew, leaving 825 participants who completed a questionnaire. Of these, 335 did not have a retrievable mammogram before the study closed, or had at least one mammogram but none were analogue, or had a previous diagnosis of breast cancer. This left a sample of 490 women who gave consent and information to enable us to locate at least one analogue mammogram. At the time of questionnaire administration, they were aged 47–50 years old. This study was approved by the Human Research Ethics Committee of The University of Melbourne. Participants provided written consent.
Height and weight data from childhood
School medical records were obtained from the Tasmanian State Archives as has been described previously [11]. These records contained heights and weights measured annually for members of the TAHS from the age of 7 until 15 years. Missing data were imputed; see Statistical methods. BMI was defined as weight divided by height squared.
Questionnaire
A structured questionnaire similar to that used by the Australian Breast Cancer Family Registry [12] was administered to all participants to record: age; self-reported height and weight at interview; and putative breast cancer risk factors including age at menarche, parity, number of children, use of oral contraceptives, use of hormone replacement therapy, alcohol consumption, smoking and family history of breast cancer in first-degree female relatives.
Mammographic density measures
We obtained mammograms through BreastScreen Tasmania, private clinics and from the women themselves. We sought all available mammograms, and used the mammogram closest to the date of interview. Both absolute and percent mammographic densities were measured by three observers (T.L.N., J.S., C.E.) using the computer-assisted thresholding software CUMULUS [13]. We used the average of each mammographic measure across the three observers.
Statistical methods
We imputed missing school records of height and weight separately. We fitted the mean as a double-logistic function of age [14] using existing data and assuming the covariance between repeated measures could be decomposed into an individual-specific component, an autoregressive component and a time-point-specific component [15–17]. Models were fitted under the assumption of multivariate normality using the statistical package FISHER [18]. From the fitted model, we interpolated the missing values based on all measured values for an individual and the estimated mean and covariance structure. Code for this was written and executed in R [19].
The percentages of non-missing values for height and weight were: 76, 6, 6, 5, 89, 10, 6, 5 and 68 % for ages 7–15, respectively (30 % overall). There was very strong tracking in the residuals of measurements about the mean when fitted as a double-logistic function of age. For height, the correlation was 0.87 for measures 1 year apart, and this reduced to 0.72 for measures 9 years apart. For weight, the corresponding correlations were 0.84 and 0.60. It was therefore possible to predict missing values with substantial precision, especially for those women for whom there were two or more measures.
We used linear regression of the mammographic density measures to estimate the strengths of their associations with the recorded or imputed childhood body size measures, adjusting for age and BMI around the time of mammography (current BMI). We transformed the mammographic density measures with the aim that, after adjusting for covariates, the residuals were approximately normally distributed; we found that a cube root transformation was appropriate. We also standardised the outcome and covariate variables to have mean = 0 and variance = 1; as a result, the squares of the regression coefficients, (β *)2, approximate the variance explained by fitting that variable with all other variables in the model held constant [2]. Analyses were conducted using Stata, version 11 [20].
We first estimated smoothed curves using the non-parametric locally weighted regression (LOWESS) procedure and found that the associations of the mammographic density measures with log-transformed BMI measures were approximately linear and the residuals had a constant variance. This can also been seen from Fig. 2a, b. We therefore used log BMI throughout.
We performed a principal components analysis of the log BMI measures at ages 7–5 years, standardised to have mean = 0 and variance = 1. The first principal component applied approximately equal weights to each measure and explained a large proportion of the variance (86 %). The second principal component, for which the weights increased as the age increased, explained a further 5 % of the variance. We, therefore, created two summary measures: (i) the average of the standardised log BMIs across ages 7–15 years, and (ii) a linear combination of the standardised log BMIs in which the weights increased linearly with age.
Results
Table 1 shows that the mean age of participants at the time of the mammogram selected for study were 47 years (all but three were younger than 50 years), 65 % of participants were pre-menopausal and 88 % were parous at the time of interview. Current log BMI was correlated with log BMI in early life, and this correlation increased from 0.31 for log BMI at age 7 years to 0.41 for log BMI at age 15 years.
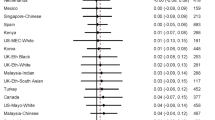
Table 2 shows that transformed absolute mammographic density was negatively associated with the log BMI measurements at all of the ages from 7 to 15 years (all p < 0.05). In terms of absolute values of the β * estimates, for which the standard errors were all about 0.04, the strength of the associations increased with the age at the BMI measure from 0.11 at 7 years to 0.19 at 15 years. In absolute terms, the association with current log BMI decreased after adjustment for the early-life log BMIs, and by greater amounts as the age increased from 7 to 15 years. The correlation between the association with childhood log BMI and current log BMI went from −0.3 at age 7 years to −0.4 at age 15 years. The associations in Table 2 are plotted in Fig. 1a and are seen to vary linearly with age.
For each of the different ages in childhood and adolescence (growth), plots of the regression coefficients for transformed and adjusted absolute mammographic density (a), and percent mammographic density (b), against the standardised measured log BMI at that age (continuous line) and the corresponding association with the log BMI at age of mammogram (dashed line), when fitted concurrently
Using the two principal components, we found that the transformed absolute mammographic density was negatively associated with the average of the standardised log BMIs (−0.17 per standard deviation; p = 0.0005) and with the linear combination of the standardised log BMIs (−0.14 per standard deviation; p = 0.03). When those two factors were fitted together, standardised transformed absolute mammographic density decreased by −0.19 per standard deviation of the average of the standardised log BMIs, and by −0.18 per standard deviation of the linear combination of the standardised log BMIs; together they explained 7 % of the variance (p < 0.001). After fitting these two parameters together, the absolute strength of the association with current log BMI decreased by about 25 %, from −0.35 to −0.26.
Figure 2a shows that standardised, transformed and adjusted absolute mammographic density was linearly associated with the standardised measured log BMIs across childhood and adolescence. The fitted straight lines and the LOWESS fitted smoothed lines of fit are almost identical through the main section of these plots.
For transformed and standardised percent mammographic density, the regression coefficients shown in Table 3 were very similar for the associations with log BMI in childhood and adolescence, but the associations with current log BMI were stronger. After adjusting for age and BMI, absolute and percent density measures were highly correlated; r = 0.97. As in Table 2, in absolute terms, the association with current log BMI decreased after adjustment for the childhood log BMIs, and by greater amounts as the age increased from 7 to 15 years. The correlation between the association with childhood log BMI and current log BMI went from −0.3 at age 7 years to −0.4 at age 15 years. The associations shown in Table 3 are plotted in Fig. 1b and are seen to vary linearly with age.
Using the two principal components, we found that transformed percent mammographic density decreased by −0.22 per standard deviation of the average of the log BMIs (p = 0.00005) and by −0.23 per standard deviation of the linear combination (p = 0.03), and together explained 10 % of the variance (p < 0.00001). When these two parameters were estimated together, the association with current log BMI decreased by about 20 %, from 0.54 to 0.44. Figure 2b shows that the standardised, transformed and adjusted percent mammographic density was linearly associated with the standardised measured log BMIs across childhood and adolescence.
The above associations were unaltered by further adjustments for age at menarche or number of live births, the two other measured factors that were at best marginally associated with the outcome measures. They also did not differ by menopausal status (data not shown).
Discussion
From this prospective study, we found that the mammographic density measures that predict breast cancer risk in the fifth decade of life were negatively associated with BMI measured between the ages of 7 and 15 years. This association was strongest for the BMI measures taken later in adolescence. BMI in childhood was modestly correlated with BMI in mid-life, but because the mammographic density measures that predict breast cancer risk are adjusted for current BMI (due to negative confounding; see “Introduction”), this did not have an impact on our conclusions.
After adjusting for early-life BMI, the correlation between the age-adjusted mammographic density measures and current log BMI decreased by 20–25 %. Therefore, a substantial proportion of the negative association of current BMI with mammographic density is explained, in the statistical sense, by the association of mammographic density measures with BMI in early life. Moreover, the absolute strengths of the associations with childhood BMI increased after adjusting for current BMI, and they also increased the later the age at which childhood BMI was measured.
Several other studies have considered childhood growth as a predictor of mammographic density measures in adulthood, and in general, have found negative associations even though most used retrospective self-reported anthropometric data; see summary in Andersen et al., 2014. In particular, McCormack et al. [21] measured Wolfe patterns from the mammograms of 1,287 women (average age at mammogram 51.5 years) for whom they had previous anthropometric measures taken at one or more of ages 2, 4, 7, 11, 15, 26, 36, 43 and 53. They found that “higher BMI at any age during childhood or adult life was associated with a reduction in the odds of higher Wolfe grade after controlling for breast size and BMI at mammography” [21]. They did not present findings from multivariable analyses to try to determine whether BMI at any particular age(s) best predicted mammographic density in mid-life. Nevertheless, in absolute terms, their associations were strongest for the BMI measures at ages 11 and 15 years (see their Table 4).
Recently, a prospective Danish study measured high versus low mammographic density for 13,572 women (aged 50–69 years) in the Copenhagen mammography screening program for whom childhood anthropometric measurements were available from the Copenhagen School Health Records Register [22]. They analysed mammographic density as a binary trait and found that childhood BMI at all ages was negatively associated with having ‘mixed or dense breasts’, although they did not adjust for current BMI.
Greater BMI in late adolescence has been found by multiple studies to be negatively associated with risk of breast cancer, independent of current BMI [22–35]. Therefore, our and others’ findings are consistent with the hypothesis that the negative association of BMI in late adolescence with adult mammographic density measures that predict breast cancer risk explains at least in part why BMI in late adolescence is negatively associated with risk of breast cancer.
Findings from the prospective Copenhagen study [23] support this hypothesis, despite using a binary measure of mammographic density. They studied the risk factors for breast cancer diagnosed after the age of 50 years (716 cases) and found that childhood BMI was negatively associated with risk. Importantly, after adjusting for mammographic density, the associations between childhood BMI and breast cancer diminished to become negligible and were not significant; see in particular the top panels in their Fig. 2. They concluded that “childhood body fatness was inversely (i.e. negatively) associated with the breast cancer risk, possibly via a mechanism mediated by (mammographic density), at least partially” [22].
Harris et al. [23] conducted a US study with some similarities to the Danish study, and found an attenuation of the breast cancer risk association with BMI at age 18 after adjusting for percent mammographic density, and a smaller attenuation after adjusting for average body fatness at young ages. Their negative association between childhood and adolescent body size and breast cancer risk remained significant after adjusting for mammographic density. Anderson et al. [22] discussed this study and the implications of their use of recall for exposures and smaller and younger sample size. Neither study adjusted for current BMI.
Interestingly, the associations we found were not influenced by age at menarche, despite it being associated with BMI around the time of menarche, and later age at menarche being associated with greater mammographically dense area at around the same age of the women we have studied [36]. This suggests that the pathway(s) through which greater BMI during the growth period impacts on the amount of mammographically dense area is not implicated in the timing of growth.
Our study has strengths, including the use of measures of body size taken in childhood and adolescence and use of the well-established measure of mammographic density, CUMULUS. It will be interesting to revisit this study should better predictors of breast cancer risk based on mammograms, such as by defining the density at higher pixel brightness thresholds, be confirmed [37]. We also considered women of the same age, to minimise age effects on the outcomes of interest, but in this regard it is important to note that the mammographic density measures that predict breast cancer risk, which adjust for age and BMI, track strongly with age and have correlations over 10 year intervals in excess of 0.8 [38]. Consequently, our results apply in general to the mammographic density measures that predict breast cancer risk, at least across the usual screening age range.
One potential weakness of our study was the incompleteness of body size measurements. We addressed this by modelling the strong tracking in height and weight of girls as they aged and imputed the missing values. Tables 2 and 3 show that the conclusions of our study also held true when based alone on the BMI measures at ages 7, 11 and 15 years when the proportion of missing values was least. Also, it is possible that the aspects of growth we have measured (height and weight) are surrogates for other causal factors not measured for this cohort, and candidates might include the age and rate of growth of breast tissue. Given that a proportion of women in the original population-complete cohort were lost to follow-up or did not agree to be in the study, there is the potential that if participation depended on key factors this could influence our findings. While we cannot exclude differential participation, given that our findings are about associations between BMI during early-life growth (exposure) and mammographic density in later life (outcome), it would have to involve both exposure and outcome to bias these association estimates.
In conclusion, using a prospective design with previously measured exposures and quantitative measurement of mammographic density, we found evidence of a negative association between aspects of growth in late adolescence and the mammographic density measures that predict breast cancer risk in adulthood. There are several novel aspects to our study. We used measured rather than recalled BMI in childhood, We had BMI measurements across childhood and adolescence and enhanced the dataset by taking advantage of the observed strong tracking of BMI during growth to impute missing values and thereby have more information and power without inducing bias. We used the continuous measure of mammographic density and we adjusted this for age and BMI at measurement to focus on the aspect of mammographic density that is the actual risk factor for breast cancer. Given the concordance of our findings with those reported by a large prospective Danish study, even though it only used a binary measure of mammographic density unadjusted for BMI, this observation could explain, in part, why BMI in late adolescence has been widely reported to be negatively associated with risk of breast cancer.
References
McCormack VA, dos Santos Silva I (2006) Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev 15:1159–1169
Nguyen TL, Schmidt DF, Makalic E et al (2013) Explaining variance in the cumulus mammographic measures that predict breast cancer risk: a twins and sisters study. Cancer Epidemiol Biomarkers Prev 22:2395–2403
Huo CW, Chew GL, Britt KL et al (2014) Mammographic density-a review on the current understanding of its association with breast cancer. Breast Cancer Res Treat 144:479–502
Martin LJ, Melnichouk O, Guo H et al (2010) Family history, mammographic density, and risk of breast cancer. Cancer Epidemiol Biomarkers Prev 19:456–463
Boyd NF, Dite GS, Stone J et al (2002) Heritability of mammographic density, a risk factor for breast cancer. N Engl J Med 347:886–894
Stone J, Dite GS, Gunasekara A et al (2006) The heritability of mammographically dense and nondense breast tissue. Cancer Epidemiol Biomarkers Prev 15:612–617
Odefrey F, Stone J, Gurrin LC et al (2010) Common genetic variants associated with breast cancer and mammographic density measures that predict disease. Cancer Res 70:1449–1458
Stone J, Thompson DJ, dos-Santos-Silva I et al (2015) Large International Study reveals novel associations between common breast cancer susceptibility variants and risk-predicting mammographic density measures. Cancer Res 75:2457–2467
Matheson M, Abramson MJ, Burgess JA, Giles GG, Hopper JL, Jenkins M, Johns DP, Perret JL, Walters EH, Lowe A, Thompson BR, Pretto JJ, Markos J, Morrison S, Thomas PS, McDonald CF, Wood-Baker R, Svanes C, Dharmage SC for the TAHS investigator group. Tasmanian Longitudinal Health Study (TAHS)—cohort profile. Int J Epidemiol
Wharton C, Dharmage S, Jenkins M et al (2006) Tracing 8,600 participants 36 years after recruitment at age seven for the Tasmanian Asthma Study. Aust N Z J Public Health 30:105–110
Nakajima K, Dharmage SC, Carlin JB et al (2007) Is childhood immunisation associated with atopic disease from age 7 to 32 years? Thorax 62:270–275
Milne RL, John EM, Knight JA et al (2011) The potential value of sibling controls compared with population controls for association studies of lifestyle-related risk factors: an example from the Breast Cancer Family Registry. Int J Epidemiol 40:1342–1354
Byng JW, Boyd NF, Fishell E et al (1994) The quantitative analysis of mammographic densities. Phys Med Biol 39:1629–1638
Preece MA, Baines MJ (1978) A new family of mathematical models describing the human growth curve. Ann Hum Biol 5:1–24
Diggle PJ, Zeger SL, Lian K-Y (1994) Analysis of longitudinal data. Oxford University Press, New York
Hopper JL, Mathews JD (1994) A multivariate normal model for pedigree and longitudinal data, and the statistical package “FISHER”. Aust J Stat 36:153–176
Stone J, Dite GS, Giles GG et al (2012) Inference about causation from examination of familial confounding: application to longitudinal twin data on mammographic density measures that predict breast cancer risk. Cancer Epidemiol Biomarkers Prev 21:1149–1155
Lange K, Weeks D, Boehnke M (1988) Programs for pedigree analysis: MENDEL, FISHER, and dGENE. Genet Epidemiol 5:471–472
Core Team R (2012) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
StatCorp (2009) Stata statistical software: release 11. StataCorp LP, College Station
McCormack V, dos Santos Silva I, De Stavola BL et al (2003) Life-course body size and perimenopausal mammographic parenchymal patterns in the MRC 1946 British birth cohort. Br J Cancer 89:852–859
Andersen ZJ, Baker JL, Bihrmann K et al (2014) Birth weight, childhood body mass index, and height in relation to mammographic density and breast cancer: a register-based cohort study. Breast Cancer Res 20:R4
Harris HR, Tamimi RM, Willett WC et al (2011) Body size across the life course, MD, and risk of breast cancer. Am J Epidemiol 174:909–918
Colditz GA, Bohlke K, Berkey CS (2014) Breast cancer risk accumulation starts early: prevention must also. Breast Cancer Res Treat 145:567–579
Baer HJ, Colditz GA, Rosner B et al (2005) Body fatness during childhood and adolescence and incidence of breast cancer in premenopausal women: a prospective cohort study. Breast Cancer Res 7:R314–R325
Baer HJ, Tworoger SS, Hankinson SE et al (2010) Body fatness at young ages and risk of breast cancer throughout life. Am J Epidemiol 171:1183–1194
Bardia A, Vachon CM, Olson JE et al (2008) Relative weight at age 12 and risk of postmenopausal breast cancer. Cancer Epidemiol Biomarkers Prev 17:374–378
Berkey CS, Frazier AL, Gardner JD et al (1999) Adolescence and breast carcinoma risk. Cancer 85:2400–2409
Le Marchand L, Kolonel LN, Earle ME et al (1988) Body size at different periods of life and breast cancer risk. Am J Epidemiol 128:137–152
London SJ, Colditz GA, Stampfer MJ et al (1989) Prospective study of relative weight, height, and risk of breast cancer. JAMA 262:2853–2858
Magnusson CM, Roddam AW, Pike MC et al (2005) Body fatness and physical activity at young ages and the risk of breast cancer in premenopausal women. Br J Cancer 93:817–824
Palmer JR, Adams-Campbell LL, Boggs DA et al (2007) A prospective study of body size and breast cancer in black women. Cancer Epidemiol Biomarkers Prev 16:1795–1802
Michels KB, Terry KL, Willett WC (2006) Longitudinal study on the role of body size in premenopausal breast cancer. Arch Intern Med 166:2395–2402
Sangaramoorthy M, Phipps AI, Horn-Ross PL et al (2013) Early-life factors and breast cancer risk in Hispanic women: the role of adolescent body size. Cancer Causes Control 24:1771–1778
Bandera EV, Chandran U, Zirpoli G et al (2013) Body size in early life and breast cancer risk in African American and European American women. Breast Cancer Res Treat 138:601–610
Jordan HL, Hopper JL, Thomson RJ et al (2010) Influence of high-dose estrogen exposure during adolescence on mammographic density for age in adulthood. Cancer Epidemiol Biomarkers Prev 19:121–129
Nguyen TL, Aung YK, Evans CF et al (2015) Mammographic density defined by higher than conventional brightness threshold better predicts breast cancer risk for full-field digital mammograms. Breast Cancer Res 17:142
Stone J, Dite GS, Giles GG et al (2012) Inference about causation from examination of familial confounding: application to longitudinal twin data on mammographic density measures that predict breast cancer risk. Cancer Epidemiol Biomarkers Prev 21:1149–1155
Acknowledgments
We would like to thank the participants in the TAHS, the study interviewers and the Tasmanian State Archives for providing access to school medical records.
Funding
This study was funded by the National Health and Medical Research Council of Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
No potential conflicts of interest were disclosed.
Rights and permissions
About this article
Cite this article
Hopper, J.L., Nguyen, T.L., Stone, J. et al. Childhood body mass index and adult mammographic density measures that predict breast cancer risk. Breast Cancer Res Treat 156, 163–170 (2016). https://doi.org/10.1007/s10549-016-3719-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3719-x