Abstract
Higher body mass index (BMI) and diabetes are associated with worse breast cancer prognosis. However, few studies have focused on triple-negative breast cancer (TNBC). The goal of this study is to examine this association in a cohort of patients with TNBC. We retrospectively reviewed 501 consecutive patients with TNBC seen at the Washington University Breast Oncology Clinic. Cox proportional hazard models were used to determine the relationship between BMI and diabetes at diagnosis with overall survival (OS) and disease free survival (DFS). Four hundred and forty-eight patients had BMI recorded and 71 patients had diabetes. The median age at diagnosis was 53 (23–98) years and follow-up was 40.1 months (IQR 25.2–62.9). Baseline BMI and diabetes were not associated with OS or DFS. OS hazard ratios (HRs) for patients who were overweight (BMI 25.0–29.99), with class I obesity (BMI 30–34.99), or BMI ≥35 were 1.22 (CI 0.78–1.91), 0.92 (CI 0.59–1.43), and 1.16 (CI 0.70–1.90), respectively. The HRs for DFS in patients who were overweight, with class I obesity, or BMI ≥35 were 1.01 (CI 0.65–1.56), 0.94 (CI 0.60–1.47), and 0.99 (CI 0.63–1.57), respectively. Similarly, the HRs for diabetics were 1.27 (CI 0.82–1.96) for OS and 0.98 (CI 0.64–1.51) for DFS. Obesity and diabetes did not significantly affect survival for patients with TNBC in this study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over one-third of adults in the United States are obese, defined by a body mass index (BMI) of greater than or equal to 30 [1]. Obesity significantly increases the risk of developing a number of malignancies, one of which is breast cancer [2]. Interestingly, the relationship of obesity and breast cancer risk depends on estrogen receptor (ER) and menopausal status. It is well established that obesity increases the risk of hormone receptor-positive breast cancer in postmenopausal women [3–5]. In contrast, in premenopausal women, recent data suggest that obesity may be associated with a higher incidence of triple-negative breast cancer (TNBC) [6]. The increased risk of breast cancer, in particular the ER positive (ER+) subtype, is explained in part by the higher peripheral estrogen production from adipocytes [7, 8], while the increased levels of insulin and insulin-like growth factor (IGF) [9, 10], adipokines (leptin and adiponectin) [11], and inflammation [12] associated with obesity provide potential explanations for increased risk of ER+ BC as well as TNBC.
In addition, obesity at breast cancer diagnosis has been associated with increased breast cancer-related and overall mortality. However, most studies reported so far included patients with all subtypes of breast cancer or only those with ER+ disease [13–20]. Few studies have focused on the interaction between obesity and survival in the TNBC patient population [21–26].
Similarly, diabetes, which tends to develop in obese patients due to insulin resistance, is associated with increased incidence of malignancy and mortality in breast cancer patients as shown in recent systemic reviews and meta-analysis of controlled trials and cohort studies [27–29]. However, only one prior study has investigated the influence of diabetes on outcomes in TNBC [30]
Since TNBC has limited treatment options, it is important to identify potential modifiable factors such as obesity and diabetes that could contribute to worse prognosis. In an effort to elucidate the relationship between BMI and diabetes with survival outcomes in TNBC, we retrospectively reviewed patients with TNBC treated at the Washington University Breast Oncology Clinic in St. Louis.
Methods
Patient population
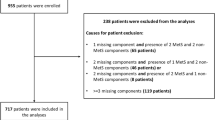
We constructed a database of 505 consecutive women with a diagnosis of TNBC who presented for their first visit to the Breast Oncology Clinic at Washington University in Saint Louis, MO between January 1st 2006 and December 16th 2010. Four patients were excluded due to absence of date of diagnosis or date of last follow-up. The information on BMI and diabetes was collected at initial breast cancer diagnosis. Four hundred and forty-eight patients with BMI data available were included in the analysis, and 71 diabetics were compared to 417 non-diabetics. Those with BMI information were divided into the following groups: normal weight (BMI <25), overweight (BMI 25.0–29.99), class I obesity (BMI 30–34.99), or BMI ≥35.
For all patients, including those diagnosed elsewhere and those who had received initial medical oncology care prior to subsequent treatments at our institution, data collection, follow-up time, and analysis started from the time of initial diagnosis. Exclusion criteria included ER or progesterone receptor (PR) positivity, HER2/neu over-expression or amplification, unknown date of diagnosis, absence of date of last follow-up, an additional malignancy and male sex. This study was approved by the Washington University Institutional Review Board.
Tumor staging and pathology
Initial pathological stage was determined based on American Joint Committee on Cancer Criteria at the time of diagnosis. Biopsy specimens from other institutions, when available, were reviewed by pathologists at Barnes Jewish Hospital. Histological grade and ER, PR, and HER2 status were recorded from pathology reports. ER and PR were considered negative if immunohistochemistry indicated an Allred score below 3 or less than 1 % of tumor cells staining. HER2 was considered to be negative if non-amplified by FISH or 0 or 1+ on immunohistochemistry. Pathologic complete response (pCR) was defined as absence of residual invasive disease in the breast and axillary lymph nodes.
Clinical parameters
We recorded clinical parameters including race, ethnicity, age, menopausal status, time from imaging to biopsy diagnosis, tumor characteristics, time from biopsy diagnosis to surgery, surgical intervention, pathological stage, receipt of neoadjuvant and/or adjuvant treatment, pathologic response to neoadjuvant therapy, follow-up information, recurrence information, and date of death (obtained from the Social Security Death Index).
Outcome measures
The primary outcomes included overall survival (OS) and disease free survival (DFS). OS was defined as the time from diagnosis to death due to any cause, and survivors were censored at the date of last contact. DFS was defined as time from surgery to any invasive breast recurrence (local or distant) or death, whichever occurred first. Those patients alive and recurrence-free were censored at date of last contact. Patients who presented with stage IV disease at diagnosis or who did not undergo surgery were excluded from DFS analysis.
Statistical analysis
The distributions of demographic and clinical characteristics across groups were compared using Chi-square test, Wilcoxon rank sum test, or ANOVA as appropriate. Survival curves by groups were estimated using the Kaplan–Meier product-limit method and compared by log-rank test. Univariate Cox proportional hazard models were fit to identify factors significantly related to OS or DFS. To assess whether BMI and diabetic status were independent predictors of survival, a multivariate Cox model was constructed to adjust for other demographic and clinical characteristics that were significant in the univariate analyses. All analyses were two-sided and significance was set at a p value of 0.05. Statistical analyses were performed using SAS (SAS Institutes, Cary, NC).
Results
Comparison of patient characteristics among BMI groups
Four hundred and forty-eight TNBC patients with BMI data were divided into the following groups: normal weight (n = 108), overweight (n = 138), class I obesity (n = 111), and BMI ≥35 (n = 91). Table 1 shows the distribution of patient characteristics among the BMI groups. Higher BMI was more prevalent among African American (AA) women. However, there was no significant difference among BMI groups with regards to age at diagnosis, menopausal status, pathological tumor stage or grade. Most patients presented with high grade and early-stage disease in all BMI groups. To investigate whether higher BMI is associated with potential diagnostic and treatment delays, we reviewed the time interval from abnormal breast imaging study to diagnostic biopsy and from the diagnostic biopsy to surgery. No significant differences in these intervals were observed among BMI groups. The percentage of patients who received neoadjuvant or adjuvant chemotherapy was compared to examine potential treatment differences among BMI groups and no differences were observed. In addition, BMI did not influence the pCR rate to neoadjuvant chemotherapy (Table 1).
Among the 52 patients (normal weight: n = 17, overweight: n = 18, class I obesity: n = 7, and BMI ≥35: n = 10) with early-stage disease (Stage I: n = 32, Stage 2: n = 11, Stage 3: n = 9) who did not receive chemotherapy, the most common reasons for not receiving chemotherapy included stage I disease for which chemotherapy was not recommended by the treating physician, age/comorbidities, and patient refusal.
Comparison of patient characteristics between diabetics and non-diabetics
Among the 488 patients with known diabetic status, 71 were diabetic and 417 were non-diabetic. Table 2 shows the distribution of patient characteristics. Diabetics were older at breast cancer diagnosis, with a median age of 56 years compared to 53 years in non-diabetics (p = 0.03). Diabetes occurred more frequently in AA patients than in Caucasians (25.5 vs. 9.9 %, p < 0.0001) and more frequently in postmenopausal than in premenopausal women (18.3 vs. 8.3 %, p = 0.01) at breast cancer diagnosis. There was no significant difference between diabetics and non-diabetics in regards to pathological tumor stage or grade. Diabetics and non-diabetics did not differ for measures of either diagnostic or treatment delays, the receipt of neoadjuvant or adjuvant chemotherapy, nor the pCR rate to neoadjuvant chemotherapy (Table 2). Thirteen (18.8 %) of diabetics and 48 (12.2 %) of non-diabetics with early-stage disease (Stage I: n = 36, Stage II: n = 16, Stage III: n = 9) did not receive chemotherapy (Table 2). This difference was not statistically significant.
Comparison of survival outcomes among BMI groups
The median follow-up time was 40.1 months (IQR 25.2–62.9 months) for all patients. Follow-up time did not differ significantly among the BMI groups (Table 1). There were a total of 154 deaths and 136 recurrences. There was no significant relationship between BMI and OS (p = 0.82) (Fig. 1), with 5-year OS of 57, 62, 65, and 65 % for normal weight, overweight, class I obesity, and BMI ≥35, respectively. On multivariate analysis, the OS hazard ratio (HR) for overweight patients was 1.22 (CI 0.78–1.91), for class I obesity 0.92 (CI 0.59–1.43), and for BMI ≥35 it was 1.16 (CI 0.70–1.90). Similarly, there was no relationship between BMI and DFS (p = 0.84), with 5-year DFS of 46, 57, 54, and 52 % for normal weight, overweight, class I obesity, and BMI ≥35, respectively (Fig. 1). HR for DFS on multivariate analysis was 1.01 (CI 0.65–1.56) for overweight patients, 0.94 (CI 0.60–1.47) for class I obesity, and 0.99 (CI 0.63–1.57) for BMI ≥35.
The interaction between menopausal status and BMI on survival
Menopausal status did not affect the relationship between BMI and outcomes of patients with TNBC for either OS (p = 0.73) or DFS (p = 0.53). HRs for OS for postmenopausal compared to premenopausal women for the different BMI groups were 0.97 (CI 0.50–1.89), 0.88 (CI 0.45–1.74), 1.26 (CI 0.63–2.52), and 0.70 (CI 0.33–1.50) for normal weight, overweight, class I obesity, and BMI ≥35, respectively. Similarly, the HRs for DFS for postmenopausal compared to premenopausal women for the different BMI groups were 0.94 (CI 0.49–1.82), 0.54 (CI 0.29–1.01), 1.00 (CI 0.53–1.91), and 0.77 (CI 0.38–1.56) for normal weight, overweight, class I obesity, and BMI ≥35, respectively.
Comparison of survival outcomes between diabetics and non-diabetics
The median follow-up time was not significantly different between diabetics and non-diabetics (37.0 vs. 41.8 months, p = 0.27) (Table 2). There were a total of 177 deaths and 155 recurrences. There was no significant relationship between diabetes and OS (Fig. 2): 5-year OS was 62 % for both diabetics and non-diabetics. On multivariate analysis, the OS HR for diabetics was 1.27 (CI 0.82–1.96). Similarly, there was no relationship between diabetes and DFS (Fig. 2): 5-year DFS for diabetics was 50 % and for non-diabetics was 58 %. The DFS HR for diabetics on multivariate analysis was 0.98 (CI 0.64–1.51).
Relationship between BMI and diabetes
There were increased rates of diabetes with increasing BMI (p ≤ 0.0001). There were 7 (6.5 %) diabetics in the normal weight group, 15 (10.9 %) in the overweight group, 8 (7.2 %) in those with class I obesity, and 31 (34.1 %) in those with BMI ≥35. While significant for increasing BMI as a whole, the increased incidence of diabetes was only significantly greater for those with BMI ≥35.
Univariate and multivariate analysis of other variables on survival outcomes
In univariate analysis, only pathological stage and response to neoadjuvant chemotherapy predicted survival. Stage II or III disease predicted significantly worse DFS, while stages IIB, III, or IV disease at diagnosis predicted significantly worse OS. Those who did not achieve a pCR to neoadjuvant chemotherapy experienced significantly worse DFS and OS compared to those who achieved a pCR to neoadjuvant chemotherapy (Table 3). Because pathological stage and response to neoadjuvant chemotherapy were strongly correlated, pathological stage was the only adjusted predictor of survival in the multivariate analyses for BMI or diabetes.
Discussion
TNBC is associated with few treatment options. It is therefore important to identify potential modifiable factors to improve patient outcomes. Increasing BMI and diabetes have been associated with worse breast cancer survival. However, the majority of the studies included all subtypes of breast cancer or focused mainly on patients with ER+ breast cancer. Few studies specifically examine the TNBC population. In this study, we investigated the impact of obesity and diabetes at breast cancer diagnosis on clinicopathologic characteristics and survival outcomes in 501 patients with TNBC treated in a single academic medical oncology practice. Neither BMI nor diabetes affected DFS or OS in this patient population.
The results of our study are consistent with several reports in the literature which suggest that BMI does not impact survival in TNBC [21–23, 25]. Similar to our analysis, most of these studies were retrospective in nature. In a single center study of 418 patients with TNBC, BMI was not associated with relapse free survival or OS at a median follow-up of 37.2 months [21]. Similar findings were observed in a smaller retrospective analysis of 183 patients, which had a median follow-up of 42.5 months [23]. Both of these studies included a smaller sample size compared to our study. The largest retrospective analysis was recently reported by Dawood et al., in which 2,311 patients with stage I-III TNBC from a single institution were included in the analysis. With a median follow-up of 39 months, no difference in distant DFS, DFS, or OS was observed among different BMI groups [22]. The impact of BMI on breast cancer outcome has also been investigated by Sparano et al. in patients enrolled in a previous adjuvant chemotherapy trial (E1199). In this trial, increasing BMI was associated with inferior DFS and OS only in hormone receptor-positive and HER2-negative disease, but not in HER2-positive or TNBC [25].
Turkoz et al. [26] suggested that obesity was associated with worse DFS and OS for premenopausal patients with TNBC. However, Dawood et al. [22] found no relationship between menopausal status and BMI on distant DFS in patients with TNBC. This was consistent with our finding that menopausal status had no effect on the relationship between BMI and survival outcomes in patients with TNBC.
To our knowledge, there was only one prior clinical study that examined whether diabetes influences survival outcomes in TNBC. This study also suggested that diabetes was not associated with TNBC survival [30]. Our data provided critical additional evidence for this finding.
Our study has several limitations. One is the relatively short follow-up time. However, this is not felt to have affected the outcomes of the study because recurrence tends to occur within the first 2–3 years for patients with TNBC. In addition, we took a time-to-event analysis approach in the assessment of OS and DFS, which automatically accounted for the length of follow-up among groups. In such a time-to-event analysis, the statistical power is determined primarily by the number of events and there have been a considerable number of events detected in our study. Another limitation of our study was its retrospective nature. In addition, there exists a possibility of selection bias in our study as patients referred to our practice could be more homogeneous in access to care, diagnostic, treatment, and follow-up approaches as reflected in the results. Because of the small sample size, we did not distinguish between type I and type II diabetes and whether insulin or metformin was administered for glucose control. We did not evaluate whether changes in BMI or glycemic control after cancer diagnosis influence survival outcomes in TNBC.
The differential effects of BMI and diabetes on the survival of patients with ER+ versus TNBC are not fully understood. One explanation is that growth of ER+ BC is dependent on estrogen, the level of which is increased with higher BMI. Increased BMI has also been associated with elevated insulin which has anti-apoptotic and mitogenic properties. However, the pre-clinical evidence on the effect of insulin and IGF on TNBC growth and survival is conflicting compared to that in ER+ BC [31–35].
In summary, our study suggests that BMI and diabetes do not influence survival outcomes in women with TNBC treated at a single academic medical center. These results are in agreement with other clinical studies [21–23, 25, 30]. Future studies examining whether changes in BMI and/or glycemic control after breast cancer diagnosis influence TNBC survival outcomes are needed.
References
Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311(8):806–814
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH (2009) The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC public health 9:88
Eliassen AH, Colditz GA, Rosner B, Willett WC, Hankinson SE (2006) Adult weight change and risk of postmenopausal breast cancer. JAMA 296(2):193–201
Suzuki R, Orsini N, Saji S, Key TJ, Wolk A (2009) Body weight and incidence of breast cancer defined by estrogen and progesterone receptor status–a meta-analysis. Int J Cancer 124(3):698–712
van den Brandt PA, Spiegelman D, Yaun SS, Adami HO, Beeson L, Folsom AR, Fraser G, Goldbohm RA, Graham S, Kushi L et al (2000) Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am J Epidemiol 152(6):514–527
Pierobon M, Frankenfeld CL (2013) Obesity as a risk factor for triple-negative breast cancers: a systematic review and meta-analysis. Breast Cancer Res Treat 137(1):307–314
Key TJ, Appleby PN, Reeves GK, Roddam A, Dorgan JF, Longcope C, Stanczyk FZ, Stephenson HE Jr, Falk RT, Miller R et al (2003) Body mass index, serum sex hormones, and breast cancer risk in postmenopausal women. J Natl Cancer Inst 95(16):1218–1226
Li CI, Malone KE, Daling JR (2006) Interactions between body mass index and hormone therapy and postmenopausal breast cancer risk (United States). Cancer Causes Control 17(5):695–703
Endogenous Hormones and Breast Cancer Collaborative Group, Key TJ, Appleby PN, Reeves GK, Roddam AW (2010) Insulin-like growth factor 1 (IGF1), IGF binding protein 3 (IGFBP3), and breast cancer risk: pooled individual data analysis of 17 prospective studies. Lancet Oncol 11(6):530–542
Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE, Manson JE, Li J, Ho GY, Xue X, Anderson GL et al (2009) Insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 101(1):48–60
Tworoger SS, Eliassen AH, Kelesidis T, Colditz GA, Willett WC, Mantzoros CS, Hankinson SE (2007) Plasma adiponectin concentrations and risk of incident breast cancer. J Clin Endocrinol Metab 92(4):1510–1516
Lorincz AM, Sukumar S (2006) Molecular links between obesity and breast cancer. Endocr Relat Cancer 13(2):279–292
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 348(17):1625–1638
Conroy SM, Maskarinec G, Wilkens LR, White KK, Henderson BE, Kolonel LN (2011) Obesity and breast cancer survival in ethnically diverse postmenopausal women: the Multiethnic Cohort Study. Breast Cancer Res Treat 129(2):565–574
Imkampe AK, Bates T (2010) Impact of a raised body mass index on breast cancer survival in relation to age and disease extent at diagnosis. Breast J 16(2):156–161
Jiralerspong S, Kim ES, Dong W, Feng L, Hortobagyi GN, Giordano SH (2013) Obesity, diabetes, and survival outcomes in a large cohort of early-stage breast cancer patients. Ann Oncol 24(10):2506–2514
Kamineni A, Anderson ML, White E, Taplin SH, Porter P, Ballard-Barbash R, Malone K, Buist DS (2013) Body mass index, tumor characteristics, and prognosis following diagnosis of early-stage breast cancer in a mammographically screened population. Cancer Causes Control 24(2):305–312
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123(3):627–635
Sestak I, Distler W, Forbes JF, Dowsett M, Howell A, Cuzick J (2010) Effect of body mass index on recurrences in tamoxifen and anastrozole treated women: an exploratory analysis from the ATAC trial. J Clin Oncol 28(21):3411–3415
Xing P, Li JG, Jin F, Zhao TT, Liu Q, Dong HT, Wei XL (2013) Prognostic significance of body mass index in breast cancer patients with hormone receptor-positive tumours after curative surgery. Clini Invest Med 36(6):E297–E305
Ademuyiwa FO, Groman A, O’Connor T, Ambrosone C, Watroba N, Edge SB (2011) Impact of body mass index on clinical outcomes in triple-negative breast cancer. Cancer 117(18):4132–4140
Dawood S, Lei X, Litton JK, Buchholz TA, Hortobagyi GN, Gonzalez-Angulo AM (2012) Impact of body mass index on survival outcome among women with early stage triple-negative breast cancer. Clin Breast Cancer 12(5):364–372
Mowad R, Chu QD, Li BD, Burton GV, Ampil FL, Kim RH (2013) Does obesity have an effect on outcomes in triple-negative breast cancer? J Surg Res 184(1):253–259
Pajares B, Pollán M, Martín M, Mackey JR, Lluch A, Gavila J, Vogel C, Ruiz-Borrego M, Calvo L, Pienkowski T et al (2013) Obesity and survival in operable breast cancer patients treated with adjuvant anthracyclines and taxanes according to pathological subtypes: a pooled analysis. Breast Cancer Res 15(6):R105
Sparano JA, Wang M, Zhao F, Stearns V, Martino S, Ligibel JA, Perez EA, Saphner T, Wolff AC, Sledge GW Jr et al (2012) Obesity at diagnosis is associated with inferior outcomes in hormone receptor-positive operable breast cancer. Cancer 118(23):5937–5946
Turkoz FP, Solak M, Petekkaya I, Keskin O, Kertmen N, Sarici F, Arik Z, Babacan T, Ozisik Y, Altundag K (2013) The prognostic impact of obesity on molecular subtypes of breast cancer in premenopausal women. J BUON 18(2):335–341
De Bruijn KM, Arends LR, Hansen BE, Leeflang S, Ruiter R, van Eijck CH (2013) Systematic review and meta-analysis of the association between diabetes mellitus and incidence and mortality in breast and colorectal cancer. Br J Surg 100(11):1421–1429
Gold HT, Makarem N, Nicholson JM, Parekh N (2014) Treatment and outcomes in diabetic breast cancer patients. Breast Cancer Res Treat 143(3):551–570
Peairs KS, Barone BB, Snyder CF, Yeh HC, Stein KB, Derr RL, Brancati FL, Wolff AC (2011) Diabetes mellitus and breast cancer outcomes: a systematic review and meta-analysis. J Clin Oncol 29(1):40–46
Bayraktar S, Hernadez-Aya LF, Lei X, Meric-Bernstam F, Litton JK, Hsu L, Hortobagyi GN, Gonzalez-Angulo AM (2012) Effect of metformin on survival outcomes in diabetic patients with triple receptor-negative breast cancer. Cancer 118(5):1202–1211
Bartucci M, Morelli C, Mauro L, Andò S, Surmacz E (2001) Differential insulin-like growth factor I receptor signaling and function in estrogen receptor (ER)-positive MCF-7 and ER-negative MDA-MB-231 breast cancer cells. Cancer Res 61(18):6747–6754
Hartog H, Horlings HM, van der Vegt B, Kreike B, Ajouaou A, van de Vijver MJ, Marike Boezen H, de Bock GH, van der Graaf WT, Wesseling J (2011) Divergent effects of insulin-like growth factor-1 receptor expression on prognosis of estrogen receptor positive versus triple negative invasive ductal breast carcinoma. Breast Cancer Res Treat 129(3):725–736
Law JH, Habibi G, Hu K, Masoudi H, Wang MY, Stratford AL, Park E, Gee JM, Finlay P, Jones HE et al (2008) Phosphorylated insulin-like growth factor-i/insulin receptor is present in all breast cancer subtypes and is related to poor survival. Cancer Res 68(24):10238–10246
Litzenburger BC, Creighton CJ, Tsimelzon A, Chan BT, Hilsenbeck SG, Wang T, Carboni JM, Gottardis MM, Huang F, Chang JC et al (2011) High IGF-IR activity in triple-negative breast cancer cell lines and tumorgrafts correlates with sensitivity to anti-IGF-IR therapy. Clin Cancer Res 17(8):2314–2327
Peiró G, Adrover E, Sánchez-Tejada L, Lerma E, Planelles M, Sánchez-Payá J, Aranda FI, Giner D, Gutiérrez-Aviñó FJ (2011) Increased insulin-like growth factor-1 receptor mRNA expression predicts poor survival in immunophenotypes of early breast carcinoma. Mod Pathol 24(2):201–208
Acknowledgments
We would like to thank patients who participated in this study and physicians, nurses, and research coordinators at Washington University Breast Oncology Clinic for their care of these patients. The authors also wish to acknowledge the support of the Biostatistics Core, Siteman Cancer Center and National Cancer Institute Cancer Center Support Grant P30 CA091842.
Conflicts of Interest
All the authors of this manuscript have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was partly presented at the 2014 Annual Meeting of the American Society of Clinical Oncology, May 30–June 3, 2014, Chicago, IL, USA
S. Tait and J. M. Pacheco have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Tait, S., Pacheco, J.M., Gao, F. et al. Body mass index, diabetes, and triple-negative breast cancer prognosis. Breast Cancer Res Treat 146, 189–197 (2014). https://doi.org/10.1007/s10549-014-3002-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-014-3002-y