Abstract
There are no validated predictors of benefit from anthracyclines. We compared cyclophosphamide, methotrexate, 5-fluorouracil (CMF), and epirubicin in different sequences with CMF alone in a phase III trial on operable breast cancers. Outcomes were analyzed in relation to tumor biological profiles to identify potential predictors of the efficacy of different treatments/drug combinations. Patients with N− or 1–3N+ tumors, were randomized to receive (a) epirubicin (4 cycles) followed by CMF (4 cycles); (b) CMF (4 cycles) followed by epirubicin (4 cycles), or (c) CMF (6 cycles) alone. Immunohistochemical assessments of estrogen (ER) and progesterone (PgR) receptors, HER2 and Ki67 were available for 705 patients (arm A/B/C: 276/269/160). Prognostic and predictive relevance was analyzed by log-rank tests and Cox models. Ki67 > 20 % and absent/low expression of ER and PgR were associated with worsen disease-free (DFS) and overall survival (OS). In patients with triple negative tumors (ER−, PgR−, HER2−), epirubicin-containing regimens yielded better DFS (HR 0.33, 95 % CI 0.17–0.62, P = 0.0007) and OS (HR 0.24, 95 % CI 0.10–0.57, P = 0.001) compared with CMF alone, whereas no differences were found in patients with HER2-positive (HER2+, ER−, PgR−) subtype. Treatment by subtype interaction (HER2-positive vs. others) was significant for DFS (χ 2 = 6.72, P = 0.009). In triple unfavorable (ER−, PgR−, Ki67 > 20 %) tumors, the use of epirubicin yielded better DFS (HR 0.45,95 % CI 0.26–0.78, P = 0.005) and OS (HR 0.30, 95 % CI 0.15–0.63, P = 0.001). Epirubicin-containing regimens seem to be superior to CMF alone in patients with highly proliferating, triple negative or triple unfavorable tumors .
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anthracyclines given sequentially with non cross-resistant regimens show higher efficacy than the six cycles of cyclophosphamide, methotrexate, and fluorouracil (CMF) given as adjuvant therapy for early breast cancer [1], but also greater toxicity. It is therefore important to define which patients really need them. Several biomarkers have been assessed as predictors of anthracycline sensitivity [2–4], but none has been introduced into clinical practice to estimate the potential benefit for individual patients [5].
The tumor proliferation rate has a prognostic impact in early breast cancer [6] and is known to predict response to chemotherapy in the neoadjuvant [7] and metastatic [8] settings and to affect results of adjuvant chemotherapy [9, 10]. We previously compared two different sequences of CMF and epirubicin with CMF alone in a phase III randomized trial on rapidly proliferating breast cancer (RPBC), observing no differences in disease-free (DFS) or overall survival (OS) [11] at the intent-to-treat analysis.
The present paper investigated, in a post-hoc analysis, whether the levels of tumor biomarkers (hormone receptors, Ki67 and HER2, considered individually or combined to define “tumor subtypes”) were associated with outcome in the entire patient population and within the cohorts treated with epirubicin plus CMF or with CMF alone.
We also assessed the difference in efficacy between epirubicin-containing regimens and CMF alone on the basis of the expression levels of tumor biomarkers and within the subgroups of patients with different immunohistochemically defined subtypes of breast cancer.
Patients and methods
Study design and patients
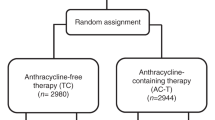
This clinical study enrolled women with completely excised, node-negative >1 cm or 1–3 node-positive invasive breast carcinomas of any size and with no evidence of metastases. From 1997 to 2004, 1,066 patients were randomized to one of three arms: (a) epirubicin (100 mg/m2 i.v. every 3 weeks) for four courses followed by CMF (600/40/600 mg/m2 i.v. days 1 and 8 every 4 weeks) for four courses (440 patients); (b) CMF for four courses followed by epirubicin for four courses (438 patients); (c) CMF for 6 courses (188 patients). Arm C was closed in 1999 following the results of the EBCSG meta-analysis [15].
The present study focuses on a subgroup of 705 (66 %) patients enrolled in eight centers, among the most important recruiters in Italy, up to 2004, for whom information on tumor biological features was fully available. The analysis was conducted on the basis of treatment received by each patient (Fig. 1).
Biological marker determination
Estrogen (ER) and progesterone (PgR) receptors were assessed at each participating center by immunohistochemistry. Tumors with >10 % immunopositive cells were considered positive, as in most studies published in the period when the present study was carried out [12, 13, 14]. For the 23 cases only that were assessed using the dextran-coated charcoal method, the cut off values were set at ≥10 and ≥25 fmol/mg of protein for ER and PgR positivity, respectively. Ki67 was assessed with MIB 1 monoclonal antibody (Dako Corporation) in all tumors and quantified as the ratio (%) of immunoreactive to total number of tumor cells.
HER2 was determined using HercepTest (DAKO Corporation) in 536 cases and CB11 monoclonal antibody (Biogenex, San Ramon, CA) in 169 cases. With the first test, positivity was assessed by considering the percentage of immunoreactive neoplastic cells where we measured the intensity and completeness of membrane staining, using a 0–3+ scale as recommended by the Dako criteria. The cases scored as 3+ were considered HER2-positive. For the cases processed with the CB11 antibody, tumors were classified as positive if any grade of immunostaining was present in more than 10 % of tumor cells. Finally, because of the potentially confounding effects of inter- and intra-center sources of variation in the data, based on our experience as members of the National Quality Control Program run by the National Research Council [14], a final check was performed on 200 cases. In this sample, an agreement of results by two independent observers of IRST in more than 90 % of cases was observed.
Definition of biomarker classes and tumor subtypes
The predictive and prognostic relevance of each biomarker was assessed by dichotomizing variables as positive or negative for ER, PgR, and HER2 and as low or high for Ki67 using a cut-off of 20 %. Tumor subtypes were defined as: hormone receptor-positive (ER-positive and/or PgR-positive with any HER2 status), HER-2 positive (HER2-positive and hormone receptor-negative), and triple negative (ER- , PgR- and HER2-negative).
Statistical considerations
The primary and secondary endpoints were OS (time from randomization to the date of last contact or of death from any cause), and DFS (time from randomization to the date of locoregional or distant recurrence, second invasive breast carcinoma, second primary cancer, and/or death without evidence of breast cancer), respectively. DFS and OS probabilities and 95 % confidence intervals (95 % CI) were computed by the product-limit method and the absolute effect of treatment was assessed by the log rank test.
Estimated hazard ratios (HR) and their 95 % CI were calculated from Cox regression models in univariate analyses performed for each biomarker. Ki67, HER2, ER, and PgR were entered as individual markers in a multivariate Cox model adjusted for age (>50 vs. ≤50 years), lymph node status (positive vs. negative), tumor size (as continuous variable), grade (3 vs. 1 + 2), treatment, and treatment-by marker interaction. The predictive value of each biomarker was evaluated with a test of interaction between treatment effect and biomarker expression using Cox models including the biomarker, treatment, and treatment-by-marker interaction.
No correction for multiple comparisons was made because of the exploratory nature of this study. All P values were based on two-sided testing, and statistical analyses were performed with SAS (version 9.3, SAS Institute).
Results
Patient and tumor characteristics are presented in Table 1 and are representative of the entire study population [11]. At a median follow-up of 69 months, there were no significant differences in the DFS and OS of the entire population or of any subgroup between patients receiving epirubicin followed by CMF and those administered CMF followed by epirubicin [11]. Unless otherwise specified, data from the two arms (A and B) were merged and compared with arm C (CMF alone). In the entire population of 705 patients the epirubicin-containing regimens were superior to CMF alone in terms of both DFS (HR 0.54, 95 % CI 0.39–0.77; P = 0.0006) and OS (HR 0.44, 95 % CI 0.27–0.71; P = 0.0009).
An analysis restricted to patients enrolled until the data of CMF arm closure confirmed the results, in terms of HR, that emerged from the main analyses of the present study (data not shown).
Prognostic impact of tumor biomarkers
Overall, Ki67 > 20 % and ER/PgR negativity were associated with worse DFS and OS (Table 2). The effects of ER and PgR were essentially maintained within the different treatment arms. A high Ki67, although generally detrimental, was only significant for DFS in the epirubicin arm. HER2 overexpression had a non-significant detrimental effect on DFS and OS in the epirubicin arm only.
Within the epirubicin-treated group, the prognostic impact of negative ER/PgR and HER2 overexpression was statistically significant in arm A (epirubicin followed by CMF) but not in arm B (CMF followed by epirubicin) [11].
Prognostic impact of tumor subtypes
A triple negative phenotype was associated with worse DFS and OS compared with the combination of other subtypes after CMF alone (Table 2). Conversely, the HER2-positive subtype was associated with worse outcome in the entire patient population and in the epirubicin-treated cohort. The hormone receptor-positive subtype was always associated with a better outcome.
The combination of negative ER and PgR with Ki67 > 20 % (herein called “triple unfavorable” tumors) showed a worse DFS and OS in the entire patient cohort and in the subgroup treated with CMF alone. A slightly lower negative impact was noted after the addition of epirubicin to the regimen.
Predictive value of tumor biomarkers and tumor subtypes
We compared the efficacy of epirubicin-containing regimens and CMF alone within subgroups of patients defined by the expression levels of single biomarkers or by tumor subtypes (Table 3). When considering individual biomarkers, although benefit from epirubicin was higher in patients with high Ki67, negative HER2 or negative hormone receptors, the treatment by marker interaction was never significant (data not shown).
Among patients with triple negative subtype, epirubicin-containing regimens yielded better DFS and OS compared with CMF (Table 3; Fig. 2a, b). In patients with hormone receptor-positive subtype, epirubicin yielded better DFS, but the impact on OS was not significant. No significant benefit from epirubicin emerged in patients with HER2-positive subtype. The interaction between treatment and subtype (HER2-positive vs. others) was highly significant for DFS (χ 2 = 6.72, P = 0.009), with a trend toward significance for OS (χ 2 = 3.46, P = 0.063).
DFS and OS in triple negative (a, b) and triple unfavorable (c, d) breast cancer patients according to treatment. TN triple negative tumor (ER-negative, PgR-negative, and HER2-negative), TU triple unfavorable tumor (ER-negative, PgR-negative, and Ki67 > 20 %), Other other tumor type (not TN or not TU), CMF cyclophosphamide, methotrexate, and fluorouracil, E → CMF/CMF → E epirubicin followed by CMF or CMF followed by epirubicin
Among patients with “triple unfavorable” tumors, the epirubicin-containing regimens yielded significantly better DFS and OS compared with CMF (Fig. 2c, d); treatment by tumor type (triple unfavorable vs. others) interaction was not significant.
Multivariate analysis
Multivariate Cox regression models were built including the biological markers, the main conventional prognostic factors, the treatment variable and the treatment by tumor subtype (HER2-positive vs. others) interaction (Table 4). Tumor size, histologic grade, treatment, and treatment-by tumor subtype interaction were independent predictors of DFS. Tumor size, PgR status, treatment, and treatment-by tumor subtype interaction were independent predictors of OS.
Discussion
The present exploratory study identified a benefit from the addition of epirubicin to CMF in patients with highly proliferating triple negative tumor and a lack of benefit in women with the HER2-positive tumor subtype. Up to now the search for strong predictors of anthracycline benefit has been elusive. Most research has focused on HER2 overexpression or gene amplification and topoisomerase IIα expression or gene (TOP2A) amplification or deletion. However, a large meta-analysis of individual patient data concluded that, while HER2 amplification and TOP2A alterations are predictive of response to anthracyclines, the possibility of patients with normal HER2 and TOP2A tumors also benefitting cannot be ruled out [4]. Chromosome 17 centromere enumeration probe (Ch17CEP) duplication has been associated with improved outcome from treatment with anthracyclines [16, 17]. Ch17CEP duplication is a marker of chromosomal instability (CIN), which has also been associated with benefit from anthracyclines [18]. Nonetheless, CIN has also been correlated with sensitivity to other drugs, such as carboplatin [19], and this mechanism may therefore not be anthracycline-specific.
Most potential predictors of response to anthracyclines are related to tumor proliferation. Topoisomerase IIα expression is closely related to the cell cycle phase [4]. Although Ch17CEP duplication is not associated with Ki67 [16], CIN correlates with high histological grade [18] and is more frequent in ER-negative and triple negative tumors, which are often highly proliferating. Thus, it is not surprising that highly proliferating, triple negative tumors benefit in particular from anthracyclines. In our study, an advantage from epirubicin was not significant in HER2-positive tumors and was absent in the HER2-positive subtype (ER−, PgR−, HER2+). Although several studies have hypothesized an increased benefit from anthracyclines compared to CMF in patients with HER2-positive tumors [3, 4], a formal statistically significant interaction between HER2 status and treatment has rarely been reported [20, 21]. A meta-analysis of individual patient data showed a significant interaction in relation to event-free survival but not to OS [4]. Other studies did not highlight any benefit from anthracyclines in patients with HER2-positive tumors [22, 23]. In particular, the BR9601 study, a study similar to ours that compared four cycles of epirubicin followed by four cycles of CMF with eight cycles of CMF, only showed a benefit from anthracyclines in HER1/HER2/HER3-negative tumors [23]. There is no clear rationale for a relationship between HER2 overexpression and benefit from anthracyclines, and preclinical studies have not found any differences in sensitivity to CMF compared with CEF in breast cancer cells overexpressing HER2 [24].
A subgroup analysis of the Canadian MA5 study assessing results in intrinsic subtypes defined by gene expression profiling reported the greatest benefit from CEF (vs. CMF) in the HER2 subtype, and no added benefit for CEF in basal-like tumors [25]. Differences in the definition of tumor subgroups (based on gene profiling vs. immunohistochemistry), in treatment schedules (CMF with oral vs. intravenous cyclophosphamide), number of cycles (6 with epirubicin vs. 4 with epirubicin plus 4 without) and cumulative dose of anthracycline could explain these findings. Although epirubicin was present in both sequential arms of our study (epirubicin followed by CMF and CMF followed by epirubicin), the lack of benefit from this anthracycline was more evident in the former sequence (data not shown).
Thus, other factors, such as initiating treatment with polychemotherapy rather than a single agent, or the timing of anthracycline administration, may also play a role. This study has the main limitation that the arm with CMF alone was closed in advance for ethical reasons, thus reducing the power of the analyses. Meanwhile, the study has a major merit in the severe and strict validation of biological determinations.
In conclusion, the retrospective nature and multiplicity of the tests we conducted indicate that our analyses can be considered exploratory and hypotheses-generating ones. The results we presented suggest that patients with triple negative, highly proliferating tumors show a better outcome when treated with an association of epirubicin and CMF rather than with intravenous CMF alone. Conversely, we could find no evidence that the epirubicin–CMF sequence improves prognosis of patients with HER2-positive, hormone receptor-negative tumors.
Abbreviations
- CEF:
-
Cyclophosphamide, epirubicin, fluorouracil
- CIN:
-
Chromosomal instability
- Ch17CEP:
-
Chromosome 17 centromere enumeration probe
- CMF:
-
Cyclophosphamide, methotrexate, and fluorouracil
- DFS:
-
Disease-free
- ER:
-
Estrogen receptor
- HR:
-
Hazard ratio
- OS:
-
Overall survival
- PgR:
-
Progesterone receptor
- RPBC:
-
Rapidly proliferating breast cancer
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG), Peto R, Davies C, Godwin J, Gray R, Pan HC, Clarke M, Cutter D, Darby S, McGale P, Taylor C, Wang YC, Bergh J, Di Leo A, Albain K, Swain S, Piccart M, Pritchard K (2012) Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100,000 women in 123 randomised trials. Lancet 379(9814):432–444. doi:10.1016/S0140-6736(11)61625-5
Munro AF, Cameron DA, Bartlett JM (2010) Targeting anthracyclines in early breast cancer: new candidate predictive biomarkers emerge. Oncogene 29(38):5231–5240. doi:10.1038/onc.2010.286
Gennari A, Sormani MP, Pronzato P, Puntoni M, Colozza M, Pfeffer U, Bruzzi P (2008) HER2 status and efficacy of adjuvant anthracyclines in early breast cancer: a pooled analysis of randomized trials. J Natl Cancer Inst 100(1):14–20
Di Leo A, Desmedt C, Bartlett JM, Piette F, Ejlertsen B, Pritchard KI, Larsimont D, Poole C, Isola J, Earl H, Mouridsen H, O’Malley FP, Cardoso F, Tanner M, Munro A, Twelves CJ, Sotiriou C, Shepherd L, Cameron D, Piccart MJ, Buyse M, HER2/TOP2A Meta-analysis Study Group (2011) HER2 and TOP2A as predictive markers for anthracycline-containing chemotherapy regimens as adjuvant treatment of breast cancer: a meta-analysis of individual patient data. Lancet Oncol 12(12):1134–1142. doi:10.1016/S1470-2045(11)70231-5
Gianni L, Norton L, Wolmark N, Suter TM, Bonadonna G, Hortobagyi GN (2009) Role of anthracyclines in the treatment of early breast cancer. J Clin Oncol 27(28):4798–4808. doi:10.1200/JCO.2008.21.4791
de Azambuja E, Cardoso F, de Castro G Jr, Colozza M, Mano MS, Durbecq V, Sotiriou C, Larsimont D, Piccart-Gebhart MJ, Paesmans M (2007) Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12,155 patients. Br J Cancer 96(10):1504–1513
Jones RL, Salter J, A’Hern R, Nerurkar A, Parton M, Reis-Filho JS, Smith IE, Dowsett M (2009) The prognostic significance of Ki67 before and after neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat 116(1):53–68. doi:10.1007/s10549-008-0081-7
Amadori D, Volpi A, Maltoni R, Nanni O, Amaducci L, Amadori A, Giunchi DC, Vio A, Saragoni A, Silvestrini R (1997) Cell proliferation as a predictor of response to chemotherapy in metastatic breast cancer: a prospective study. Breast Cancer Res Treat 43(1):7–14
Penault-Llorca F, André F, Sagan C, Lacroix-Triki M, Denoux Y, Verriele V, Jacquemier J, Baranzelli MC, Bibeau F, Antoine M, Lagarde N, Martin AL, Asselain B, Roché H (2009) Ki67 expression and docetaxel efficacy in patients with estrogen receptor-positive breast cancer. J Clin Oncol 27(17):2809–2815. doi:10.1200/JCO.2008.18.2808
Hugh J, Hanson J, Cheang MC, Nielsen TO, Perou CM, Dumontet C, Reed J, Krajewska M, Treilleux I, Rupin M, Magherini E, Mackey J, Martin M, Vogel C (2009) Breast cancer subtypes and response to docetaxel in node-positive breast cancer: use of an immunohistochemical definition in the BCIRG 001 trial. J Clin Oncol 27(8):1168–1176. doi:10.1200/JCO.2008.18.1024
Amadori D, Silvestrini R, De Lena M, Boccardo F, Rocca A, Scarpi E, Schittulli F, Brandi M, Maltoni R, Serra P, Ponzone R, Biglia N, Gianni L, Tienghi A, Valerio MR, Bonginelli P, Amaducci L, Faedi M, Baldini E, Paradiso A (2011) Randomized phase III trial of adjuvant epirubicin followed by cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) versus CMF followed by epirubicin in patients with node-negative or 1–3 node-positive rapidly proliferating breast cancer. Breast Cancer Res Treat 125(3):775–784. doi:10.1007/s10549-010-1257-5
Early Breast Cancer Trialists’ Collaborative Group (1998) Polychemotherapy for early breast cancer: an overview of the randomised trials. Lancet 352(9132):930–942
Ellis MJ, Suman VJ, Hoog J, Lin L, Snider J, Prat A, Parker JS, Luo J, DeSchryver K, Allred DC, Esserman LJ, Unzeitig GW, Margenthaler J, Babiera GV, Marcom PK, Guenther JM, Watson MA, Leitch M, Hunt K, Olson JA (2010) Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptor-rich stage 2 to 3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype ACOSOG Z1031. J Clin Oncol 29(17):2342–2349. doi:10.1200/JCO.31.6950
Huober J, Fasching PA, Barsoum M, Petruzelka L, Wallwiener D, Thomssen C, Reimer T, Paepke S, Azim HA, Ragosch V, Kubista E, Baumgärtner AK, Beckmann MW, May C, Nimmrich I, Harbeck N (2012) Higher efficacy of letrozole in combination with trastuzumab compared to letrozole monotherapy as first-line treatment in patients with HER2-positive, hormone-receptor-positive metastatic breast cancer e results of the eLEcTRA trial. Breast 21(1):27–33. doi:10.1016/j.breast.2011.07.006
Paradiso A, Volpe S, Iacobacci A, Marubini E, Verderio P, Costa A, Daidone MG, Marchetti A, Mottolese M, Amadori D, De Paola F, Saragoni L, Medri L, Nenci I, Querzoli P, Gion M, Dittadi R, Plebani M, Orlando C, Bevilacqua G, Silvestrini R, Italian Network for Quality Assessment of Tumor Biomarkers (2002) Quality control for biomarker determination in oncology: the experience of the Italian Network for Quality Assessment of Tumor Biomarkers (INQAT). Int J Biol Markers 17(3):201–214
Bartlett JM, Munro AF, Dunn JA, McConkey C, Jordan S, Twelves CJ, Cameron DA, Thomas J, Campbell FM, Rea DW, Provenzano E, Caldas C, Pharoah P, Hiller L, Earl H, Poole CJ (2010) Predictive markers of anthracycline benefit: a prospectively planned analysis of the UK National Epirubicin Adjuvant Trial (NEAT/BR9601). Lancet Oncol 11(3):266–274. doi:10.1016/S1470-2045(10)70006
Pritchard KI, Munro A, O’Malley FP, Tu D, Li X, Levine MN, Shepherd L, Chia S, Bartlett JM (2012) Chromosome 17 centromere (CEP17) duplication as a predictor of anthracycline response: evidence from the NCIC Clinical Trials Group (NCIC CTG) MA.5 Trial. Breast Cancer Res Treat 131(2):541–551. doi:10.1007/s10549-011-1840-4
Munro AF, Twelves C, Thomas JS, Cameron DA, Bartlett JM (2012) Chromosome instability and benefit from adjuvant anthracyclines in breast cancer. Br J Cancer 107(1):71–74. doi:10.1038/bjc.2012.232
Swanton C, Nicke B, Schuett M, Eklund AC, Ng C, Li Q, Hardcastle T, Lee A, Roy R, East P, Kschischo M, Endesfelder D, Wylie P, Kim SN, Chen JG, Howell M, Ried T, Habermann JK, Auer G, Brenton JD, Szallasi Z, Downward J (2009) Chromosomal instability determines taxane response. Proc Natl Acad Sci USA 106(21):8671–8676. doi:10.1073/pnas.0811835106
Pritchard KI, Shepherd LE, O’Malley FP, Andrulis IL, Tu D, Bramwell VH, Levine MN, National Cancer Institute of Canada Clinical Trials Group (2006) HER2 and responsiveness of breast cancer to adjuvant chemotherapy. N Engl J Med 354(20):2103–2111
Paik S, Bryant J, Park C, Fisher B, Tan-Chiu E, Hyams D, Fisher ER, Lippman ME, Wickerham DL, Wolmark N (1998) erbB-2 and response to doxorubicin in patients with axillary lymph node-positive, hormone receptor-negative breast cancer. J Natl Cancer Inst 90(18):1361–1370
Knoop AS, Knudsen H, Balslev E, Rasmussen BB, Overgaard J, Nielsen KV, Schonau A, Gunnarsdóttir K, Olsen KE, Mouridsen H, Ejlertsen B, Danish Breast Cancer Cooperative Group (2005) Retrospective analysis of topoisomerase IIa amplifications and deletions as predictive markers in primary breast cancer patients randomly assigned to cyclophosphamide, methotrexate, and fluorouracil or cyclophosphamide, epirubicin, and fluorouracil: Danish Breast Cancer Cooperative Group. J Clin Oncol 23(30):7483–7490
Bartlett JM, Munro A, Cameron DA, Thomas J, Prescott R, Twelves CJ (2008) Type 1 receptor tyrosine kinase profiles identify patients with enhanced benefit from anthracyclines in the BR9601 adjuvant breast cancer chemotherapy trial. J Clin Oncol 26(31):5027–5035. doi:10.1200/JCO.2007.14.6597
Konecny G, Fritz M, Untch M, Lebeau A, Felber M, Lude S, Beryt M, Hepp H, Slamon D, Pegram M (2001) HER-2/neu overexpression and in vitro chemosensitivity to CMF and FEC in primary breast cancer. Breast Cancer Res Treat 69(1):53–63
Cheang MC, Voduc KD, Tu D, Jiang S, Leung S, Chia SK, Shepherd LE, Levine MN, Pritchard KI, Davies S, Stijleman IJ, Davis C, Ebbert MT, Parker JS, Ellis MJ, Bernard PS, Perou CM, Nielsen TO (2012) Responsiveness of intrinsic subtypes to adjuvant anthracycline substitution in the NCIC.CTG MA.5 randomized trial. Clin Cancer Res 18(8):2402–2412. doi:10.1158/1078-0432.CCR-11-2956
Acknowledgments
The authors thank Granato Anna Maria and Roagna Riccardo for technical support, Federica Zumaglini, Alessandra Piancastelli, Emanuela Montanari, Britt Rudnas, Ilaria Massa, Patrizia Serra, Monia Dall’Agata and Chiara Tison for data management, and Ursula Elbling for editing the manuscript.
Conflict of interest
The authors have declared no conflicts of interest.
Ethical standards
All patients provided written informed consent before participating in the trial.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rocca, A., Bravaccini, S., Scarpi, E. et al. Benefit from anthracyclines in relation to biological profiles in early breast cancer. Breast Cancer Res Treat 144, 307–318 (2014). https://doi.org/10.1007/s10549-013-2819-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2819-0