Abstract
Triple-negative breast cancers comprise about 20 % of breast cancers. They have poor prognosis and have no standard therapy. The aim of this study was to evaluate pathologic complete response (pCR), progression-free survival (PFS), and overall survival (OS) in patients with TNBC treated with neoadjuvant platinum-based chemotherapy. This is a retrospective study of one hundred and forty-four women with TNBC treated with neoadjuvant platinum-containing chemotherapy for locally advanced breast cancer at the University of Miami between January 1, 1999, and January 1, 2011. The medical record was reviewed to obtain data on clinical characteristics, including ethnicity, race, age, clinical stage, treatment regimen, and vital status. This study was approved by the University of Miami IRB. All patients had locally advanced breast cancer with at least one of the following features at presentation: T3, T4, N2, and N3. The mean tumor size by palpation was 9.4 cm. The clinical T-stage at presentation was 1.4 % T1, 8.3 % T2, 52.8 % T3, and 37.5 % T4 (19.4 % T4d). The nodal status by physical exam at presentation was 23 % N0, 37.5 % N1, 34 % N2, and 5.5 % N3. pCR in breast and axilla was seen in 31 %. PFS and OS were 55 and 59 %, respectively, at 7 years. Cisplatin offered a survival advantage over carboplatin in both PFS (P = 0.007) and OS (P = 0.018). Node positivity was the most important predictor of survival. Cisplatin/docetaxel neoadjuvant therapy was well tolerated and an effective therapy in locally advanced TNB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is a heterogeneous group of diseases, embracing a number of different entities that vary in their morphology, biological behavior, clinical outcome, and response to therapy [1]. The groundbreaking work of Perou et al. [2, 3] demonstrated that the majority of breast cancers could be divided into five distinct genetic signatures, each with its own prognosis. The HER2 overexpressing and basal-like subtypes were associated with the worst clinical outcomes, with the basal-like group linked to the shortest relapse-free and overall survival times.
The basal-like subgroup expressed CK5/6, CK14, CK17, p53, p63, vimentin, smooth muscle actin (SMA), c-kit, P-cadherin, and epidermal growth factor receptor 1 (EGFR) and was missing estrogen receptor (ER), progesterone receptor (PR), or Her-2 [4–10]. Triple-negative breast cancer (TNBC) is defined by the lack of ER, PR, and HER2 expression on immunohistochemical staining. A majority of the TNBC tumors are of the basal subtype. TNBCs are usually high-grade tumors and frequently associated with the p53 mutation. TNBC is characterized by higher incidence of visceral and cerebral metastases [11–14]. TNBC is more common in African-American, African, and younger women [15]. The risk of distance recurrence appears to peak at 3 years from diagnosis and declines rapidly thereafter [8]. Triple-negative breast cancers are commonly found in women who have germline mutations in BRCA1 or BRCA 2. However, a majority of women with triple-negative tumors do not have germline mutations [16]. Preclinical data suggest that TNBC may be sensitive to interstrand crosslinking agents that damage the DNA such us platinum because of deficiencies in the BRCA-associated DNA repair mechanism [17–23]. Currently, there is no consensus regarding optimal systemic or targeted therapy for TNBC.
The aim of this study was to evaluate pathologic complete response (pCR), progression-free survival (PFS), overall survival (OS), and factors that predict for them in patients with TNBC treated with neoadjuvant platinum-based chemotherapy.
Methods
Study population
This retrospective study was approved by the University of Miami IRB
One hundred and forty-four women with TNBC were treated with neoadjuvant platinum-containing chemotherapy for locally advanced breast cancer at the University of Miami between January 1, 1999, and January 1, 2011. Many of these women were treated on prospective trials evaluating the use of platinum-based chemotherapy in the neoadjuvant setting. The medical record was reviewed to obtain data on clinical characteristics, including ethnicity, race, age, clinical stage, treatment regimen, and vital status.
Response criteria
Pathologic complete response (pCR) is defined as the absence of invasive tumor. A specimen containing only ductal carcinoma in situ or lobular carcinoma in situ would be registered as a pathologic complete response. We have specified pCR in the breast, pCR in the axilla, and pCR in the breast and axilla to facilitate a comparison with other studies. Patients who did not have surgery either because of unresectability or refusal were classified as having no pCR in the breast and as having >4 lymph nodes positive for tumor in the axilla. Progression (PD) during NACT was defined as a lack of clinical response to NACT in the primarily involved disease site(s) or clinical evidence of locoregional progression during NACT. Locoregional recurrence (LR) after NACT and definitive surgery was defined as recurrence in the breast or chest wall (CW) and/or axillary, supraclavicular, or internal mammary lymph nodes.
Treatment
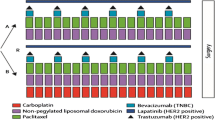
All patients received neoadjuvant platinum salts (either cisplatin or carboplatin) with docetaxel. There were five chemotherapy regimens used. An anthracycline regimen was given to all patients. Doxorubicin and cyclophosphamide (AC) were the most commonly used (96 %) and could be given neoadjuvantly (61 %) or adjuvantly (34 %).
- Regimen 1:
-
Cisplatin 70 mg/m2 + docetaxel 70 mg/m2 every 21 days × 4 → surgery → AC × 4.
- Regimen 2:
-
Cisplatin 70 mg/m2 + docetaxel 70 mg/m2 every 21 days × 4 → AC × 4 → surgery.
- Regimen 3:
-
Carboplatin AUC 2 + docetaxel 35 mg/m2 weekly × 3 repeat every 28 days × 4 → surgery → AC × 4.
- Regimen 4:
-
Carboplatin AUC 5 + docetaxel 75 mg/m2 every 21 days × 4 → surgery → AC × 4.
- Regimen 5:
-
Carboplatin AUC 5 + docetaxel 75 mg/m2 every 21 days × 4 → AC × 4 → surgery.
The surgery offered was modified radical mastectomy or breast conservation with axillary node dissection based on the clinical response and the physician and patient preferences. Based on the fact that all patients had locally advanced breast cancer at presentation, all patients were offered radiation therapy (RT) to the breast or chest wall (CW) ± regional lymph nodes after surgery, and the median total breast/CW dose inclusive of boost was 60.4 Gy. RT was generally delivered using medial and lateral photon tangents; in patients who had mastectomy, a 1-cm bolus was placed over the chest wall every other day. Treatment of the internal mammary nodes with a medial electron field was rarely performed. Some patients received radiation to the supraclavicular nodes; radiation to the SCV was delivered by a standard anterior or anterior oblique field, prescribed to a depth of 3–5 cm.
Statistical analysis
Patient disease and treatment characteristics, and clinical outcomes, were summarized overall and by neoadjuvant chemotherapy (NACT) using descriptive statistics. Fisher’s exact test or χ 2 test for categorical variables and Student t test for quantitative variables were used in comparing cisplatin versus carboplatin NACT. OS was defined as the elapsed time from start NCAT to death. PFS was defined as the elapsed time from start NCAT to date of first evidence of disease progression or recurrence, or date of death, whichever was earlier. Event-free patients were censored at the date of last follow-up. The date of disease progression was selected as the date of radiologic progression. Rates of PD during NACT, LR, and distant metastasis as first failure were estimated by the method of cumulative incidence allowing for competing risks as described by Gray [24] using the “cuminc” procedure in the R statistical package “cmprsk.” The effect of prognostic factors was examined by Gray’s test as part of the cuminc procedure or the test of Fine and Gray [25] based on the competing risk Cox proportional hazards regression method implemented in the “crr” procedure in the “cmprsk” package. PFS and OS were estimated by the Kaplan–Meier method with 95 % confidence intervals (95 % CIs) based on the log–log transform method and Greenwood’s variance. The effects of prognostic factors were examined using the logrank test and Cox proportional hazards regression analysis [26]. Analyses were conducted using the SAS® version 9.3.
Results
Patient demographics
The demographic characteristics of the patients included in the study are shown in Table 1. The median age was 49 (range 27–86). Fifty-eight percent of the patients were premenopausal. The racial and ethnic makeup of our cohort shows that 62 % were Caucasian, 36 % African descent, 2 % Asian, and 58 % were Hispanic. Our patients came from 21 countries on 4 continents.
Tumor characteristics
All patients had locally advanced breast cancer with at least one of the following features at presentation: T3, T4, N2, and N3. The mean tumor size by palpation was 9.4 cm. The clinical T-stage at presentation was 1.4 % T1, 8.3 % T2, 52.8 % T3, and 37.5 % T4 (19.4 % T4d). The nodal status by physical exam at presentation was 23 % N0, 37.5 % N1, 34 % N2, and 5.5 % N3. Invasive ductal carcinoma accounted for 72.5 % of the histologic types, while 12.5 % were metaplastic, 8.3 % medullary, and 7.7 % other histologies (Table 1).
Progression-free survival
The median follow-up of the 88 alive and progression-free patients is 4.0 years with a range from 0.7 to 11.3 years. PFS is based on 56 events, including 11 progressions during NACT and 45 who relapsed after surgery. Four of the 11 patients who progressed during NACT were alive at 1.2, 1.5, 6.4, and 10 years, three of them with no evidence of disease. Six of the 45 patients who progressed after surgery were alive at last follow-up, but none were disease free.
The PFS by Kaplan–Meier analysis for the whole population and by selected prognostic factors is shown in Fig. 1. The percent of women without progression or relapse at 1 year was 84 %; at 2 years 68 %; at 3 years 60 %; at year 4 57 %; and at years 5, 6, and 7, it was 55 %. Factors affecting PFS in univariate Cox regression analysis were pCR in the breast and axilla versus no pCR (HR 0.22, P = 0.001), cisplatin chemotherapy vs carboplatin (HR 0.49, P = 0.007), >3 lymph nodes involved with tumor after NACT versus none (HR 7.52, P = 0.0001), Stage 3 versus Stage 2 (HR 3.18, P = 0.008), T4 versus T1, 2, 3 (HR 3.69, P < 0.0001), and tumor diameter >8 cm (HR 2.07, P = 0.01). In multivariate analysis, the factors that predicted for PFS were cisplatin chemotherapy (HR 0.55, P = 0.045), >3 lymph nodes involved with tumor (HR 3.55, P < 0.001), and T4 (HR 3.31, P = <0.0001). Race, ethnic group, age, histology, and menopausal status had no significant effect on PFS (Table 2).
Overall survival
The median follow-up of the 98 alive patients was 3.8 years with a range from 0.7 to 11.3 years. There were 46 deaths, including 39 deaths from breast cancer, 6 from other causes, and 1 of unknown cause. The percent of women surviving at one year was 94 %; at two years 78 %; at three years 70 %; at four years 64 %; at five years 61 %; and at 6, 7, and 8 years 59 % (Fig. 2). The OS by Kaplan–Meier analysis for the whole population and by selected prognostic factors is shown in Fig. 2. Factors significantly affecting OS in univariate analysis were pCR in the breast and axilla (HR 0.32, P = 0.009), cisplatin chemotherapy versus carboplatin (HR 0.40, P = 0.002), >3 axillary node involvement after NACT versus none (HR 8.74, P < 0.0001), 1–3 axillary node involvement versus none (HR 2.87 P = 0.007), and T4 versus T1, 2, 3 (HR 3.19, P < 0.0001). In multivariate analysis, cisplatin therapy (HR 0.48, P = 0.018), >3 lymph node residual (HR 5.74, P < 0.0001), and T4 disease (HR 2.59, P = 0.003) remained predictive of OS. There was no difference in OS based on race, ethnic group, age, menopausal status, or histology (Table 2).
Local relapse
There were 56 failure events, including 11 progressions during NACT, and 18 locoregional failures with chest wall involvement (with or without distant failure). The 5-year incidence rate of locoregional failure was 15.1 % (95 % CI 9.2–23.0 %) and of distant failure was 22.2 % (95 % CI 15–30 %), taking into account progression during NACT as a competing risk for the first site of failure. Initial stage, age, race, menopausal status, histology, and T4 status did not predict local relapse. No pCR in the breast and axilla (HR = 7.59, P = 0.047), no pCR in the breast (HR = 4.38, P = 0.047), more than 3 residual axillary nodes’ involvement after neoadjuvant therapy (HR = 6.64, P < 0.001), and age <50 years (HR = 3.07, P = 0.045) predicted local relapse. In the multivariate model, only residual disease in axillary nodes remained significant (HR = 4.39, P = 0.027). 34.1 % of patients with more than 3 nodes relapsed locally by the third year after diagnosis. This contrasts with patients with 1–3 nodes or 0 nodes who had local relapse rates of 12 % and 7 %, respectively (P = 0.001) (Table 3; Fig. 3).
pCR (breast and axilla)
Pathologic complete response in the breast and axilla occurred in 45 of the 144 patients (31 %, 95 % CI 24–39 %). Initial stage and T-stage were significant predictors of pCR in the breast and axilla, with corresponding rates of 39.3 % in stage II/IIIA versus 20.0 % in IIIB–C (P = 0.014), and 37.8 % in T1–3 versus 20.4 % in T4 (P = 0.029). Patients with a pCR in the breast and axilla had a longer OS, PFS, and time to local relapse than women without a pCR (P = 0.006, 0.002 and 0.047).
The median PFS has not yet been reached in the subgroup of patients that achieved pCR, whereas the median PFS for non-pCR was 3.1 years (P = 0.002 by logrank test). The 5-year PFS rates were 81.6 % in pCR versus 44.7 % in no pCR (Fig. 1). Median overall survival was not reached for women who achieved a pCR in the breast and axilla, who had a survival rate of 84 % at 3 years and 79.4 % at year 4 and thereafter. For those with residual invasive disease in the breast or axilla, median overall survival was 8.4 years. OS at 5 years was 79.4 versus 53.2 % for women with a pCR in the breast and axilla vs no pCR (P = 0.006 by logrank test) (Fig. 2).
pCR (axilla/node negative)
The PFS and OS curves diverge quickly for women with positive axillary nodes after neoadjuvant therapy. Median progression-free and overall survival was not reached for 87 (60.4 %) women who were node negative after receiving neoadjuvant chemotherapy. Women who had 1–3 axillary nodes had a median PFS and OS of 4.6 and 5.0 years, respectively, while women with 4 or more axillary nodes had PFS and OS of 1.0 and 1.7 years (log rank P value <0.0001 for OS and PFS), respectively. Only 22 % of women with >3 residual lymph nodes after neoadjuvant therapy were alive at 5 years. The existence of multiple positive axillary nodes after neoadjuvant therapy is the single worst prognostic factor and predicts for markedly shortened overall survival (Figs. 1, 2).
Significant predictors of pCR in the axilla were cisplatin versus carboplatin 68 versus 44.7 % (P = 0.007), initial clinical stage (pCR in axilla of 87.5 % in stage II vs. 52.7 % in stage III, P = 0.0004; 75 % in stage II/IIIA vs. 40 % in stage IIIB–C, P < 0.0001), T-stage (71.1 % in T1–3 vs. 42.6 % in T4, P = 0.0007; 66.4 % in “not T4” vs. 35.7 % in T4, P = 0.003), and N-stage (81.8 % in N0, 72.2 % in N1 and 36.8 % in N2–3, P < 0.0001) (Table 4). Race was a marginally significant predictor of pCR in the axilla with corresponding rates of 50 % in Blacks versus 66.3 % in other races (P = 0.055).
Cisplatin versus carboplatin
Sixty-seven percent of the patients received cisplatin chemotherapy, while the remaining 33 % received carboplatin. The cisplatin-based regimens were superior to the carboplatin-based regimens in OS and PFS (univariate HR 0.49 and 0.40, P = 0.007 and P = 0.018, respectively) (Figs. 1, 2). The median OS for carboplatin-based regimens was 3.8 years, while the OS for cisplatin-based regimens has not been reached. This is regardless of whether AC was given preoperatively or postoperatively.
The group of patients that received cisplatin achieved a pCR rate in the breast and axilla of 36 %, compared to the group that received carboplatin which had a pCR rate of 21. % (P = 0.072). The node-negative rate was 70 % for the women receiving cisplatin and 49 % for those receiving carboplatin (P = 0.004). Eleven patients progressed on initial neoadjuvant chemotherapy, 4 (4 %) from the cisplatin group versus 7 (15 %) from the carboplatin group (P = 0.04). The two groups were well balanced in terms of demographics and tumor characteristics. Multivariate analysis confirms that the improvement in PFS and OS was due to the drug itself and not due to patient selection factors (Tables 1, 2, 4).
Discussion
Platinum-based neoadjuvant chemotherapy coupled with docetaxel and AC rendered a high rate of pCR in the breast and axilla (31 %) in this high-risk group of women with triple-negative breast cancer. Despite an initial mean tumor size of 9.4 cm, the overall survival was 59 % at 7 years.
pCR in the breast and axilla continues to be a strong predictor of long-term survival in patients treated with neoadjuvant therapy [27–29]. In our series, the median survival for patients with a pCR in the breast, in the axilla, or in the breast and axilla was not reached, while those not achieving these landmarks had median overall survival of 3.8, 2.4, and 4.1 years, respectively. However, pCR in the axilla was by far the strongest predictor for overall survival. Only thirty percent of the women who had any nodal involvement went on to survive 5 years and, tragically, only 15 % of those with over three nodes survived 5 years.
Women with triple-negative breast cancer consistently have a higher rate of response to chemotherapy, but a worse overall survival than women with other types of breast cancer [30, 31], and no specific chemotherapy regimen has proved to be superior. Historically, anthracycline/taxanes-based regimens are the most commonly used (Table 5). Carey et al. [30] reported a 27 % pCR rate for 34 triple-negative breast tumors [Stage II (35 %), Stage III (65 %)] treated with neoadjuvant AC. Seventy-six percent of these patients also received neoadjuvant taxanes. The 4-year DDFS was 71 %. In the MD Anderson experience [31, 32], 471 patients with triple-negative breast cancer [Stage II (52 %), Stage III (45 %)] were treated with an anthracycline-based regimen. Eighty-seven percent also received neoadjuvant taxane therapy. The pCR rate for Caucasian patients was 25 % and for patients of African descent was 17 %. The OS was 71 % at 3 years.
Regimens that are not based on anthracyclines plus taxanes are less commonly used. Falo et al. [33] reported a pCR rate of 65 % in 57 women treated with three cycles of CMF as neoadjuvant therapy. Egawa et al. [34] reported that patients with decreased BRCA2 expression had a favorable response to docetaxel.
Because of the recent identification of TNBC as a unique subtype and its association with BRCA-induced breast cancer, there has been increasing interest in the use of platinum-based therapy in these tumors. Eight weekly doses of cisplatin, epirubicin, and paclitaxel (PET) were given by Frasci et al. [35] to 74 women with moderate-risk TNBC. The patients received either CMF or FEC as adjuvant therapy. The pCR rate was 62 % and the estimated 5-year PFS and OS were 76 and 84 %, respectively. Sirohi et al. [36] treated 62 high-risk patients with TNBC with neoadjuvant epirubicin, cisplatin, and infusional 5FU for 18 weeks (ECisF). Many of the patients with good clinical response underwent radical radiotherapy instead of surgery, so no pCR rates were reported. The 5-year PFS and OS were 57 and 64 %, respectively, while the 10-year OS was 53 %. Yerushalmi et al. [37] treated 20 women with locally advanced TNBC with eight cycles of sequential cisplatin/paclitaxel and adriamycin/paclitaxel for a pCR rate of 35 % and an OS of 49.5 % at 5 years. Bryski et al. [38] reported a pCR rate of 90 % in ten women with TNBC and a BRCA mutation with single-agent cisplatin. Silver et al. [39] reported a pCR rate of 21 % in twenty-eight patients with TNBC treated with single-agent cisplatin as neoadjuvant therapy. Two of the six women with a pCR had a BRCA mutation, so that the pCR rate for women with TNBC without a BRCA mutation in this series is actually 15 %, while the pCR rate for women with a BRCA mutation was 100 %. BRCA1 promoter methylation and low BRCA1 mRNA expression did not reliably predict pCR in the patients who did not have a germline mutation in BRCA1. No survival data are reported in either of these studies.
Cisplatin is part of the curative regimens in all solid tumors. It forms the backbone of the treatment of testicular cancer, lung cancer (both small cell and non-small cell), and ovarian cancer. It is part of the organ-sparing regimens for head and neck cancer, sarcomas, and bladder cancer. The superiority of cisplatin over carboplatin has been demonstrated in multiple solid tumors in the curative setting [40, 41]. In this study, we demonstrated the superiority of cisplatin-based chemotherapy to carboplatin-based chemotherapy in the curative setting of triple-negative breast cancer. Despite the fact that there was no difference in the pCR rates in the breast and axilla for cisplatin versus carboplatin chemotherapy, there was a statistically significant improvement in overall survival in patients treated with cisplatin. This may be accounted for by the higher rate of primary failure and the higher rate of node positivity in the carboplatin-containing regimen than the cisplatinum regimen.
The average pCR rate for standard anthracycline- and taxane-containing regimens is reliably in the 20 % range. The pCR rate of 62 % in response to therapy with CMF must be taken in the context of a 39.7 % pCR rate of ER-positive tumors to CMF in the same study. The response rate of platinum-based regimens is spread over a wide range from 15 to 90 % and is influenced heavily by the presence of germline mutations in BRCA1, the addition of taxanes/anthracyclines to the platinum base, and the stage distribution of the patients included in each study. What seems apparent is that, although there is a wide range of response measured by pCR in TNBC, combination therapy with a cisplatin backbone is highly active and well tolerated, while single-agent cisplatin is probably inadequate therapy except in women with a BRCA mutation.
Platinum salts/docetaxel chemotherapy used as neoadjuvant therapy for locally advanced triple-negative breast cancer yielded a high pCR rate of 31 % and was both safe and well tolerated. The use of cisplatin conferred a survival advantage over carboplatin-based therapy. The most significant predictor of survival is the amount of residual axillary nodal involvement. The discovery and the addition of targeted therapy to the platinum/docetaxel backbone should be the next step.
References
EBCTCG (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365:1687–1717
Perou CM, Sorlie T, Elsen MB et al (2000) Molecular portraits of human breast tumors. Nature 406:747–752
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Fulford LG, Easton DF, Reis-Filho JS et al (2008) Specific morphologic features predictive for the basal phenotype in grade 3 invasive ductal carcinoma of the breast. Histopathology 49:22–34
Rahka E, Reis-Filho J, Ellis I (2008) Basal-like breast cancer: a critical review. J Clin Oncol 26(15):2568–2581
Banerjee S, Reis-Filho JS, Ashley S et al (2006) Basal-like breast carcinomas: clinical outcome and response to chemotherapy. J Clin Pathol 59:729–735
Van de Rijn M, Perou CM, Tibshirani R et al (2002) Expression of cytokeratins 17 and 5 identifies a group of breast carcinomas with poor clinical outcome. Am J Pathol 161:1991–1996
Abd El-Rehim DM, Pinder SE, Paish CE et al (2004) Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 203:661–671
Livasy CA, Karaca G, Nanda R et al (2006) Phenotypic evaluation of the basal-like subtype of invasive breast carcinoma. Mod Pathol 19:264–271
Nielsen TO, Hsu FD, Jensen K et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5537
Carey L, Winer E, Viale G et al (2010) Triple-negative breast cancer: disease entitiy or title of convenience. Nat Rev Clin Oncol 7:683–692
Dent R, Trudeau M, Pritchard K et al (2007) Triple negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13(15):4429–4434
Gluz O, Liedtke C, Gottschalk N et al (2009) Triple-negative breast cancer—current status and future directions. Ann Oncol 20(12):1913–1927
Schneider B, Winer E, Foulkes W et al (2008) Triple-negative breast cancer: risk factors to potential targets. Clin Cancer Res 14(24):8010–8018
Carey L, Perou C, Livasy C et al (2006) Race, breast cancer subtypes, and survival in the Carolina breast cancer study. JAMA 295(21):2492–2502
Nanda Rita (2011) “Targeting” triple-negative breast cancer: the lessons learned from BRCA1-associated breast cancers. Semin Oncol 38(2):254–262
Miyoshi Y, Murase K, Oh K (2008) Basal-like subtype and BRCA1 dysfunction in breast cancer. Int J Clin Oncol 13:395–400
Quinn J, Kennedy RD, Mullan P et al (2003) BRCA1 functions as a differential modulator of chemotherapy-induced apoptosis. Cancer Res 63:6221–6228
Shafee N, Smith C, Wie S et al (2008) Cancer stem cells contribute to cisplatin resistance in BRCA1/p53-mediated mouse mammary tumors. Cancer Res 68(9):3243–3250
Bhattacharyya A, Ear U, Kollers B et al (2000) The breast cancer susceptibility gene BRCA1 is required for subnuclear assembly of Rad51 and survival following treatment with the DNA cross-linking agent cisplatin. J Biol Chem 275(31):23899–23903
Kennedy RD, Quinn J, Mullan PB et al (2004) The role of BRCA1 in the cellular response to chemotherapy. JNCI 96(22):1659–1669
Farmer H, McCabe N, Lord C et al (2005) Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434:917–920
Foulkes W (2006) BRAC1 and BRCA2: chemosensitivity, treatment outcomes and prognosis. Fam Cancer 5:135–142
Gray R (1988) A class of K-sample tests for comparing the cumulative incidence of competing risk. Ann Stat 16:1141–1154
Fine JP, Gray R (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Parmar MKB, Machin D (1995) Survival analysis: a practical approach. Wiley, Cambridge
Fisher B, Brown A, Mamounas E et al (1997) Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol 15:2483–2493
Kuerer HM, Newman LA, Smith TL et al (1999) Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol 17:460–469
Morrell L, Lee Y, Hurley J et al (1998) A Phase II trial of neoadjuvant methotrexate, vinblastine, doxorubicin and cisplatin in the treatment of patients with locally advanced breast cancer. Cancer 82:503–511
Carey L, Dees C, Sawyer L et al (2007) The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 13(8):2329–2334
Liedtke C, Mazouni C, Hess K et al (2008) Response to neoadjuvant therapy and long-term survival in patients with triple negative breast cancer. J Clin Oncol 26(8):1275–1281
Dawood S, Briglio K, Kau S et al (2009) Triple negative breast cancer: the effect of race on response to primary systemic treatment and survival outcomes. J Clin Oncol 27(2):220–226
Falo C, Moreno A, Varela M et al (2007) HER-2/neu status and response to CMF: retrospective study in a series of operable breast cancer treated with primary CMF. J Cancer Res Clin Oncol 133:423–429
Egawa C, Miyoshi Y, Takamura Y et al (2001) Decreased expression of BRCA2 mRNA predicts favorable response to docetaxel in breast cancer. Int J Cancer 95:255–259
Frasci G, Comella P, Rinaldo M et al (2009) Preoperative weekly cisplatin–epirubicin–paclitaxel with G-CSF support in triple negative large operable breast cancer. Ann Oncol 20:1185–1192
Sirohi B, Arnedos M, Popat S et al (2008) Platinum based chemotherapy in triple-negative breast cancer. Ann Oncol 19:1847–1852
Yerulshalmi R, Hayes MM, Gelmon K et al (2009) A phase II trial of a neoadjuvant platinum regimen for locally advanced breast cancer: pathologic response, long-term follow-up, and clinical correlation with biomarkers. Clin Breast Cancer 9(3):166–171
Byrski T, Huzarski T, Dent R et al (2008) Response to neoadjuvant therapy with cisplatin an BRCA1 positive breast cancer. Breast Cancer Res Treat 115(2):359–363
Silver D, Richardson AL, Ecklung A et al (2010) Efficacy of neoadjuvant cisplatin in triple negative breast cancer. J Clin Oncol 28(7):1145–1153
Rosell R, Gatzemeier U, Betticher DC et al (2002) Phase III randomized trial comparing paclitaxel/carboplatin with paclitaxel/cisplatin in patients with advanced non-small cell lung cancer: a cooperative multinational trial. Ann Oncol 13:1539–1549
Ardizzoni A, Boni L, Tiseo M et al (2007) Cisplatin versus carboplatin-based chemotherapy in first-line treatment of advanced non-small cell lung cancer: an individual patient data meta-analysis. J Natl Cancer Inst 99(11):847–857
Acknowledgments
This research was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice and was approved by the Institutional Review Board of the University of Miami.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hurley, J., Reis, I.M., Rodgers, S.E. et al. The use of neoadjuvant platinum-based chemotherapy in locally advanced breast cancer that is triple negative: retrospective analysis of 144 patients. Breast Cancer Res Treat 138, 783–794 (2013). https://doi.org/10.1007/s10549-013-2497-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2497-y