Abstract
We examined cardiorespiratory fitness (CRF) levels in early stage breast cancer patients and determined whether CRF differs as a function of adjuvant therapy regimen. A total of 180 early breast cancer patients representing three treatment groups (surgery only, single-, and multi-modality adjuvant therapy) in the Cooper Center Longitudinal Study (CCLS) were studied. A non-cancer control group (n = 180) matched by sex, age, and date of the CCLS visit was included. All subjects underwent an incremental exercise tolerance test to symptom limitation to assess CRF (i.e., peak metabolic equivalents [METs] and time to exhaustion). The mean time from breast cancer diagnosis to exercise tolerance testing was 7.4 ± 6.2 years. In adjusted analyses, time to exhaustion and peak METs were incrementally impaired with the addition of surgery, single-, and multi-modality adjuvant therapy compared to those of matched controls (p = 0.006 and 0.028, respectively). CRF was lowest in the multi-modality group compared to all other groups (all p’s < 0.05). Despite being 7 years post-diagnosis, asymptomatic early breast cancer survivors have marked reductions in CRF. Patients treated with multi-modal adjuvant therapy have the greatest impairment in CRF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Significant improvements in early detection and adjuvant therapy have resulted in substantial reductions in cancer-specific mortality among women diagnosed with early breast cancer [1]. As a result, approximately 2.5 million women are alive today in the US with a history of breast cancer [2], a number that is expected to double over the next two decades. However, women with early breast cancer, particularly those over 65 years of age, now have sufficient survival to be at risk for non-breast cancer-related (competing) mortality, primarily cardiovascular disease (CVD) [3]. The precise etiology of therapy-related CVD late effects in early breast cancer patients remains to be fully elucidated. Women with early breast cancer are subjected to prolonged and aggressive adjuvant therapies (e.g., surgery, radiation, systemic therapy) which are proposed to cause ‘direct’ insults to components of the cardiovascular system [4]. Direct insults in conjunction with ‘indirect’ lifestyle changes (e.g., weight gain, physical inactivity) collectively lead to marked reductions in cardiovascular function (reserve capacity). We have termed this phenomenon the ‘multiple-hit’ hypothesis [3]. As such, the accurate quantification of cardiovascular function is likely to become increasingly important in the management and long-term surveillance of women with early stage breast cancer [5].
In current oncology practice, evaluation of cardiovascular function is commonly determined via resting determination of left ventricular ejection fraction (LVEF), usually prior to the initiation of therapy and before administration of agents with known cardiotoxicity [6]. Global cardiovascular function is not routinely evaluated after the completion of adjuvant therapy, and is only repeated if patients exhibit signs or symptoms of heart failure or in patients receiving trastuzumab therapy. In addition, resting LVEF does not capture global cardiovascular function, which is determined by the integrative capacity of multiple organ systems working in concert to maintain whole-body homeostatic regulation under a variety of physiological conditions [7]. Taken together, global cardiovascular function of women following the completion of primary adjuvant therapy for early breast cancer is poorly characterized.
Incremental exercise tolerance testing to symptom limitation evaluates the ability of the cardiovascular, hematologic, and musculoskeletal systems to transport and utilize oxygen (O2) for ATP resynthesis [8]. The efficiency of O2 transport and utilization determines an individual’s cardiorespiratory fitness (CRF); CRF, as assessed by exercise tolerance testing, is inversely correlated with cardiovascular and all-cause mortality in a broad range of adult populations [9, 10]. Thus, exercise tolerance testing provides an accurate assessment of global cardiovascular function that may, in turn, not only complement current methods used in the oncology setting (prior to the initiation of therapy), but also evaluate cardiovascular reserve capacity after the completion of therapy. Such information may help to identify those patients requiring close or further monitoring and/or therapeutic intervention.
Few studies have examined the clinical utility of exercise tolerance testing to evaluate cardiovascular function in early breast cancer patients following the completion of primary adjuvant therapy and/or evaluate the additive contribution of different components of adjuvant therapy on CRF. Accordingly, we utilized the Cooper Center Longitudinal Study (CCLS) database (1971–2007) [11] to examine CRF levels in early breast cancer patients on average 7 years after primary adjuvant therapy, and determined whether CRF differed as a function of the type of prior local or systemic adjuvant therapy. We hypothesized that breast cancer patients would have significant impairments in CRF compared to matched control women without a history of breast cancer. We further hypothesized that patients treated with multi-modal adjuvant therapy would have the greatest impairment in CRF.
Methods
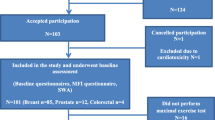
Participants and procedures
The CCLS is a prospective observational cohort study of participants undergoing a preventive health examination including exercise tolerance testing to symptom limitation or volitional exhaustion at the Cooper Clinic in Dallas, Texas. Patients enrolled in CCLS signed an informed consent and the Cooper Institute’s Institutional Review Board approved this study.
An overview of the methods and procedures of CCLS has been described previously [11–13]. In the present study, the CCLS database was queried for individuals reporting a history of non-skin-related cancer. A detailed medical chart review was then conducted to confirm a diagnosis of breast cancer (between 1971 and 2007) as well as to ascertain date of cancer diagnosis and type of local and/or systemic therapy. Among the cases, time from diagnosis to CRF testing were as follows: 18 % (0–2 years), 26 % (>2 to 4 years), 13 % (>4 to 6 years), 19 % (>6 to 10 years), and 24 % (>10 years). A total of 180 participants with a history of early breast cancer were categorized into one of three treatment groups: (i) surgery only (n = 67), (ii) surgery plus radiotherapy or chemotherapy (n = 71) (herein referred to as the single-modality adjuvant therapy group), and (iii) surgery plus chemotherapy and radiation (n = 42) (herein referred to as the multi-modality adjuvant therapy group). Within the single-modality adjuvant therapy group, 55 % received radiation + surgery and 45 % received chemotherapy + surgery. A non-cancer control group (n = 180) individually matched to breast cancer patients by sex, age, and date of the CCLS preventive medical exam was included for comparison purposes.
Cardiorespiratory fitness
CRF was evaluated by a maximal treadmill exercise tolerance test using a modified-Balke protocol. Greater than 97 % of women reached 85 % of their maximal predicted heart rate. Treadmill speed was initially set at 3.3 mph. In the first minute, the grade was set at 0 % followed by a 2 % increase in the second minute and a 1 % increase for every minute thereafter. After 25 min, the grade remained unchanged but the speed was increased 0.3 mph (5.4 m/min) for each additional minute until test termination. The test was terminated by volitional exhaustion reported by the participant or by the physician for medical reasons. Time to exhaustion utilizing this protocol correlates with direct measurement of \( V_{{{\text{O}}_{{2{\text{peak}}}} }} \) (r = 0.92) [14]. Furthermore, using well-characterized regression equations, time to exhaustion from the modified-Balke protocol permits estimation of CRF level in peak metabolic equivalents (METs) (1 MET = 3.5 mL kg−1 min−1) [15]. Continuous electrocardiography (ECG) and heart rate monitoring were performed during exercise and for 10 min following peak stress (recovery) [16]. Abnormal resting and exercise ECG findings were broadly categorized as rhythm and conduction disturbances and ischemic ST-T wave abnormalities as described elsewhere [17].
Other CVD risk factors
Information about age, gender, and health habits was obtained by questionnaires and were physician verified. Body mass index (BMI) was calculated from measured weight and height. Blood pressure was measured with standard auscultatory methods after the participant had been seated for 5 min. Systolic and diastolic blood pressure was recorded as the first and fifth Korotkoff sounds, respectively. Physical activity was assessed by self-report and was used to calculate METs min/week [18]. A 12-h fasting antecubital venous blood sample was obtained and plasma concentrations of glucose and lipids were determined with automated bioassays in the Cooper Clinic Laboratory, which meets quality control standards of the CDC Lipid Standardization Program.
Statistical methods
Descriptive statistics was used to assess patient demographic and clinical parameters. Analysis of covariance (ANCOVA) was used to assess differences in measures of CRF (i.e., time to exhaustion and peak METs) between the overall cohort of breast cancer patients and matched controls with adjustment for age, physical activity, years since breast cancer diagnosis, and cardiovascular risk factors (total cholesterol, glucose, systolic and diastolic blood pressure). To examine differences in CRF between the three patient treatment groups and matched controls, we conducted an overall F test with post hoc (Tukey–Kramer) analysis, as appropriate to control for varying sample sizes between groups. These analyses were also adjusted for the aforementioned covariates. A two-sided significance level of 0.05 was used for all statistical tests. All statistical analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC).
Results
Participant characteristics
Participant characteristics are described in Table 1. The mean and median time from breast cancer diagnosis to CRF assessment was 7.4 ± 6.2 years. Breast cancer patients and matched controls mean age and BMI were 55 ± 9 years and 25 ± 5 kg/m2 and 55 ± 10 years and 24 ± 5 kg/m2, respectively (both p = NS). There were no significant between group differences in any cardiovascular risk factors including the proportion of subjects presenting with ECG abnormalities (all p’s < 0.05). All patients underwent surgical resection, while 22, 18, and 23 % received adjuvant radiotherapy, chemotherapy, or both, respectively. No participants had evidence of recurrent or metastatic disease and all were asymptomatic at the time of examination.
Differences between the overall breast cancer patients and matched controls
Differences in CRF are presented in Table 2. Adjusted analyses indicated that measures of CRF were lower in breast cancer patients compared to matched controls but these differences did not reach statistical significance. Specifically, mean time to exhaustion was 723 ± 259 s (range 150–1,587 s) in patients compared to 781 ± 287 s (range 77–1,710 s) in matched controls (mean difference −51 s, p = 0.136; Fig. 1a). Mean peak METs was 8.9 ± 2.1 (range 4–15) in patients compared to 9.3 ± 2.4 (range 4–18) in controls (mean difference −0.4, p = 0.114; Fig. 1b). Results were similar to the overall results when stratifying on median time from diagnosis and testing (5 years). For example, women >5 years from diagnosis have a mean peak METs of 8.8 (2.2) compared to women <5 years from diagnosis [9.0 METs (1.9)] and controls [9.3 METs (2.4)] (p = 0.06). Peak heart rates were 165 ± 18 and 167 ± 18 beats min−1 in patients and controls, respectively (p = 0.915). There were no between group differences in heart rate recovery (p trend = 0.365).
Differences between breast cancer patients by prior adjuvant therapy and matched controls
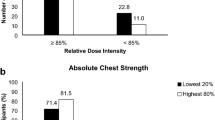
In comparison to matched controls, time to exhaustion and peak METs were incrementally lower with the addition of surgery, single-, and multi-modality adjuvant therapy in patients (p trend = 0.006 and 0.028, respectively) (Table 3). Specifically, time to exhaustion was 758 ± 301 s in the surgery only (mean difference from controls: −23 s), 737 ± 228 s in the single-modality adjuvant therapy group (mean difference from controls: −44 s), and 645 ± 226 s in the multi-modality adjuvant therapy group (mean difference from controls: −136 s) (p trend = 0.006; Fig. 2a). Post hoc analysis indicated that time to exhaustion was lowest in the multi-modality adjuvant therapy group compared to all other groups (all p’s <0.05).
Differences in CRF between breast cancer patients by prior adjuvant therapy for a time to exhaustion (*significantly different from controls, surgery only, single-modality adjuvant therapy, and multi-modal adjuvant therapy) and b peak METs (*significantly different from matched controls). Statistical tests: *p < 0.05
Similarly, peak METs was 9.2 ± 2.3 s in the surgery only group (mean difference from controls: −0.1), 9.0 ± 1.8 s in the single-modality adjuvant therapy group (mean difference from controls: −0.3), and 8.3 ± 1.9 s in the multi-modality adjuvant therapy group (mean difference: −1.0) (p trend = 0.028; Fig. 2b). Post hoc analysis indicated that peak METs was lowest in the multi-modality adjuvant therapy group compared to matched controls (p = 0.021). There were no between group differences in resting or peak heart rate, the proportion of ECG abnormalities at peak exercise, or heart rate recovery (p trend = 0.944).
Discussion
The principal finding of this study was that patients treated with multi-modality adjuvant therapy had a significant impairment in CRF compared to women of similar age without a history of breast cancer. To our knowledge, this is the first study to evaluate the additive contribution of different components of adjuvant therapy (i.e., surgery, chemotherapy, radiation) on CRF in early breast cancer survivors. Furthermore, the additive nature of the observed impairment is consistent with the tenets of the ‘multiple-hit’ hypothesis [3]. Finally, our findings demonstrate the feasibility and safety of maximal exercise tolerance testing in the post-therapy breast cancer survivorship setting. From a clinical perspective, our findings provide support for exercise tolerance testing as an assessment tool that could identify a sub-group of patients with diminished CRF, and hence high-risk of therapy-induced cardiovascular late effects that likely requires close monitoring, further evaluation, and therapeutic intervention.
In the present data (for the overall cohort), patients’ mean CRF was 8.9 METs or an estimated \( V_{{{\text{O}}_{{2{\text{peak}}}} }} \) of 31.1 mL kg−1 min−1, the equivalent to ~5 % below matched women without a history of breast cancer. The level of CRF impairment in the present study is lower than that observed in our prior study. Specifically, we previously found that despite ‘normal’ resting cardiac function (i.e., LVEF ≥50 %), CRF, as measured by peak oxygen consumption (\( V_{{{\text{O}}_{{2{\text{peak}}}} }} \)) was, on average, 18.4 mL kg−1 min−1, the equivalent to 22 % below that of age-matched sedentary women, a mean of 27 months following the completion of primary adjuvant therapy [19]. Several important study methodological differences may explain these divergent findings including: (1) measurement of CRF (maximal ‘stress’ test vs. direct measurement of \( V_{{{\text{O}}_{{2{\text{peak}}}} }} , \) which may have resulted in over-estimation of CRF in the present study [15, 20]), (2) exercise test modality (treadmill vs. cycle ergometer; CRF is typically 5–10 % higher on a treadmill [21], and (3) timing of CRF assessment following cancer diagnosis (~3 years in prior study vs. ~7 years in the current study).
The CCLS data provided a unique opportunity to investigate the additive contribution of adjuvant therapies on CRF impairment. As hypothesized, CRF levels became increasingly impaired with the addition of single or multi-modal adjuvant therapy to surgery, with multi-modality adjuvant therapy conferring the greatest impairment in CRF. These data provide further support for the major tenets of the ‘multiple-hit’ hypothesis, contending that as a patient progresses through diagnosis and adjuvant therapy, they are subjected to a series of sequential or concurrent direct perturbations in one or more organs that govern O2 transport and utilization, which collectively deplete cardiovascular reserve capacity [3]. Indeed, compared to matched controls, the impact of surgery alone was associated with a ~3 % reduction in CRF; the addition of radiation or chemotherapy to surgery was associated with a further 3 % reduction; whereas the addition of both radiation and chemotherapy was associated with a further 15 % reduction in CRF (a total CRF reduction of 21 %). The mean CRF in the multi-modality adjuvant therapy group was 8.3 METs (equivalent to a \( V_{{{\text{O}}_{{2{\text{peak}}}} }} \) of ~29.0 mL kg−1 min−1), the equivalent to ~12.4 % (−3.5 mL kg−1 min−1) below matched controls, and ~9 to ~12 % (−2.5 to −3.0 mL kg−1 min−1) below that of the other breast cancer treatment groups. The magnitude of CRF impairment in the multi-modality adjuvant therapy, compared with matched controls, is similar to that observed in our prior study (−18.4 vs. −22 %) [19].
Gupta et al. [9] reported that a single assessment of CRF significantly improved the discrimination and reclassification of all-cause and cardiovascular mortality risk prediction at 10 and 25 years, even after controlling for traditional cardiovascular risk factors (e.g., systolic blood pressure, diabetes mellitus) in 66,371 asymptomatic individuals participating in the CCLS. Given emerging data indicating that early breast cancer patients have heightened risk for therapy-induced CVD late effects [3] tools such as exercise tolerance testing that improve CVD mortality risk prediction may also have utility in the oncology setting. Furthermore, exercise tolerance testing can facilitate the design of intervention strategies to prevent and/or mitigate therapy-induced fitness impairments. Further study evaluating the clinical importance of CRF impairments in post-therapy breast cancer as well as other cancer populations appears warranted.
As in non-cancer clinical populations, the mechanisms underlying impaired CRF in breast cancer patients are likely multi-factorial with pulmonary, cardiovascular, and/or musculoskeletal limitations playing central roles [4]. Clearly, in cancer patients, normal, age-related mechanisms of exercise limitation are dramatically compounded by the adverse effects of conventional and modern anti-cancer therapies. Most adjuvant therapies used in the treatment of breast cancer are associated with unique and varying degrees of injury to the different organ components that govern the transport and utilization of oxygen that collectively determine CRF (i.e., pulmonary, cardiac, blood-vascular, and skeletal muscle function) [4]. The acute effects of radiation, chemotherapy, and other anti-cancer therapies used in the management of early breast cancer (i.e., endocrine therapy, HER-2 directed therapy) on components of the cardiovascular system, particularly cardiac function, have been described previously [22–24]. It is important to note that we were unable to obtain information on the use of adjuvant endocrine therapy or adjuvant trastuzumab therapy, which are also hypothesized to potentially impair global cardiovascular function. Similarly, information on molecular or clinical breast cancer subtypes was unavailable. While tumor subtype is not likely to impact fitness per se, it may correlate with selection of therapy. Clearly, understanding the mechanisms of injury as well as the contribution of each component of adjuvant therapy to the observed impairments in CRF is an important goal of future research. Nevertheless, and of equal importance, varying degrees of cardiovascular impairment appear to persist for years following the completion of primary adjuvant therapy. The establishment of large cohort studies is required to elucidate the physiological mechanisms of therapy-induced cardiovascular late effects in women with early breast cancer. This approach would parallel studies being conducted in adult survivors of childhood cancers [25]. Such studies will dramatically improve our understanding of the prevalence, incidence, severity, and mechanisms of therapy-induced impaired CRF as well as related cardiovascular toxicities/symptoms in cancer survivors.
The strengths and limitations of this study require consideration. Lack of data on use of other adjuvant therapies (e.g., endocrine therapy, trastuzumab), type of chemotherapy prescribed and therapy dose, as well as the cross-sectional study design is an important limitation. Prospective studies evaluating the trajectory of change in CRF across patient cohorts receiving different adjuvant therapy regimens are required to fully elucidate the relative contribution and potential synergistic or additive effects of modern adjuvant therapies, including endocrine and HER-2 targeted agents on CRF. Data were obtained on women attending a private preventive health visit and thus are more likely to be following healthy lifestyle recommendations and experiencing less treatment-related complications. In addition, data pertaining to specific treatment-related characteristics including type and length/dose of adjuvant therapy were not available. As such, the generalizability of our findings to the larger cohort of population of breast cancer patients receiving adjuvant chemotherapy is limited. A major strength of our study was that breast cancer patients and controls were matched on age and date of preventive health visit. In our prior study, the ‘healthy’ control comparison data were obtained from population-based normative data as opposed to investigator-derived data [19]. Here, CRF testing in both patients and controls was conducted using the identical procedures and equipment, at the same institute, with groups comparable in CVD risk factor profile.
In conclusion, the addition of each form of adjuvant therapy to surgical resection is associated with step-wise reductions in CRF in women with early breast cancer. Women treated with multi-modal adjuvant therapy have the greatest impairment in CRF. Although the prognostic and clinical importance of these findings remains to be determined, breast cancer patients have marked reductions in CRF that persists years after the completion of therapy.
Abbreviations
- CVD:
-
Cardiovascular disease
- CCLS:
-
Cooper Center Longitudinal Study
- METs:
-
Metabolic equivalents
- LVEF:
-
Left ventricular ejection fraction
- CRF:
-
Cardiorespiratory fitness
- ECG:
-
Electrocardiogram
- ANCOVA:
-
Analysis of covariance
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62(1):10–29
Jemal A, Siegel R, Ward E, Murray T, Xu J, Smigal C, Thun MJ (2006) Cancer statistics, 2006. CA Cancer J Clin 56(2):106–130
Jones LW, Haykowsky MJ, Swartz JJ, Douglas PS, Mackey JR (2007) Early breast cancer therapy and cardiovascular injury. J Am Coll Cardiol 50(15):1435–1441
Lakoski SG, Eves ND, Douglas PS, Jones LW (2012) Exercise rehabilitation in patients with cancer. Nat Rev Clin Oncol 9(5):288–296
Ewer MS, Lippman SM (2005) Type II chemotherapy-related cardiac dysfunction: time to recognize a new entity. J Clin Oncol Off J Am Soc Clin Oncol 23(13):2900–2902
Jannazzo A, Hoffman J, Lutz M (2008) Monitoring of anthracycline-induced cardiotoxicity. Ann Pharmacother 42(1):99–104
Hsia CC, Ramanathan M, Estrera AS (1992) Recruitment of diffusing capacity with exercise in patients after pneumonectomy. Am Rev Respir Dis 145(4 Pt 1):811–816
Jones LW, Eves ND, Haykowsky M, Joy AA, Douglas PS (2008) Cardiorespiratory exercise testing in clinical oncology research: systematic review and practice recommendations. Lancet Oncol 9(8):757–765
Gupta S, Rohatgi A, Ayers CR, Willis BL, Haskell WL, Khera A, Drazner MH, de Lemos JA, Berry JD (2011) Cardiorespiratory fitness and classification of risk of cardiovascular disease mortality. Circulation 123(13):1377–1383
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE (2002) Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346(11):793–801
Blair SN, Kohl HW III, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW (1989) Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 262(17):2395–2401
Blair SN, Kohl HW III, Barlow CE, Paffenbarger RS Jr, Gibbons LW, Macera CA (1995) Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA 273(14):1093–1098
Lakoski SG, Barlow CE, Farrell SW, Berry JD, Morrow JR Jr, Haskell WL (2011) Impact of body mass index, physical activity, and other clinical factors on cardiorespiratory fitness (from the Cooper Center Longitudinal Study). Am J Cardiol 108(1):34–39
Pollock ML, Foster C, Schmidt D, Hellman C, Linnerud AC, Ward A (1982) Comparative analysis of physiologic responses to three different maximal graded exercise test protocols in healthy women. Am Heart J 103(3):363–373
Pollock ML, Bohannon RL, Cooper KH, Ayres JJ, Ward A, White SR, Linnerud AC (1976) A comparative analysis of four protocols for maximal treadmill stress testing. Am Heart J 92(1):39–46
Ho JS, Fitzgerald SJ, Barlow CE, Cannaday JJ, Kohl HW III, Haskell WL, Cooper KH (2010) Risk of mortality increases with increasing number of abnormal non-ST parameters recorded during exercise testing. Eur J Cardiovasc Prev Rehabil Off J Eur Soc Cardiol Work Groups Epidemiol Prev Cardiac Rehabil Exerc Physiol 17(4):462–468
Peel JB, Sui X, Adams SA, Hebert JR, Hardin JW, Blair SN (2009) A prospective study of cardiorespiratory fitness and breast cancer mortality. Med Sci Sports Exerc 41(4):742–748
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO et al (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32(9 Suppl):S498–S504
Jones LW, Courneya KS, Mackey JR, Muss H, Pituskin EN, Scott JM, Hornsby WE, Coan AD, Herndon JE II, Douglas PS et al (2012) Cardiopulmonary function and age-related decline across the breast cancer survivorship continuum. J Clin Oncol 30(20):2530–2537
Froelicher VF Jr, Thompson AJ Jr, Davis G, Stewart AJ, Triebwasser JH (1975) Prediction of maximal oxygen consumption. Comparison of the Bruce and Balke treadmill protocols. Chest 68(3):331–336
Hermansen L, Saltin B (1969) Oxygen uptake during maximal treadmill and bicycle exercise. J Appl Physiol 26(1):31–37
Khakoo AY, Yeh ET (2008) Therapy insight: management of cardiovascular disease in patients with cancer and cardiac complications of cancer therapy. Nat Clin Pract Oncol 5(11):655–667
Darby SC, Cutter DJ, Boerma M, Constine LS, Fajardo LF, Kodama K, Mabuchi K, Marks LB, Mettler FA, Pierce LJ et al (2010) Radiation-related heart disease: current knowledge and future prospects. Int J Radiat Oncol Biol Phys 76(3):656–665
Yeh ET, Tong AT, Lenihan DJ, Yusuf SW, Swafford J, Champion C, Durand JB, Gibbs H, Zafarmand AA, Ewer MS (2004) Cardiovascular complications of cancer therapy: diagnosis, pathogenesis, and management. Circulation 109(25):3122–3131
Hudson MM, Ness KK, Nolan VG, Armstrong GT, Green DM, Morris EB, Spunt SL, Metzger ML, Krull KR, Klosky JL et al (2011) Prospective medical assessment of adults surviving childhood cancer: study design, cohort characteristics, and feasibility of the St. Jude Lifetime Cohort Study. Pediatr Blood Cancer 56(5):825–836
Acknowledgments
LWJ is supported in part by Research Grants from the National Cancer Institute (CA143254, CA142566, CA138634, CA133895, CA164751).
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lakoski, S.G., Barlow, C.E., Koelwyn, G.J. et al. The influence of adjuvant therapy on cardiorespiratory fitness in early-stage breast cancer seven years after diagnosis: the Cooper Center Longitudinal Study. Breast Cancer Res Treat 138, 909–916 (2013). https://doi.org/10.1007/s10549-013-2478-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2478-1