Abstract
Purpose
Achieving a higher chemotherapy completion rate is associated with better outcomes in breast cancer patients. We examined the role of exercise and health-related fitness variables in predicting chemotherapy completion in early stage breast cancer patients.
Methods
We pooled data from two large, multicenter, exercise trials that obtained baseline (pre-chemotherapy) measures of exercise and health-related fitness in 543 breast cancer patients initiating adjuvant chemotherapy. Assessments included body composition, cardiovascular fitness, muscular strength, patient-reported physical functioning, and self-reported exercise behavior. Chemotherapy completion was assessed as the average relative dose intensity (RDI) for the originally planned regimen. We used logistic regression analyses with a two-sided p value of < 0.05 to estimate the associations between the predictors and an RDI of ≥ 85%.
Results
Overall, 432 of 543 (79.6%) breast cancer patients received an RDI of ≥ 85%. In logistic regression analyses adjusted for significant covariates, patients in the highest 20% vs. lowest 80% of absolute VO2peak were significantly more likely to complete ≥ 85% RDI (89.0% vs. 77.2%; ORadj 2.06, 95% CI 1.07–3.96, p = 0.031). Moreover, patients in the highest 80% vs. lowest 20% of absolute chest strength were significantly more likely to complete ≥ 85% RDI (81.5% vs. 71.4%; ORadj 1.80, 95% CI 1.09–2.98, p = 0.021).
Conclusions
In these exploratory analyses, higher baseline (pre-chemotherapy) cardiovascular fitness and muscular strength were associated with higher rates of chemotherapy completion in early stage breast cancer patients. Aerobic and/or strength training interventions that increase cardiovascular fitness and muscular strength prior to chemotherapy for breast cancer may improve treatment tolerability and outcomes.
Clinical trial registration
START: NCT00115713, June 24, 2005; CARE: NCT00249015, November 7, 2005 (http://clinicaltrials.gov).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
A lower rate of chemotherapy completion is associated with worse survival in early stage breast cancer patients [1,2,3,4,5]. Previous research has reported a 38% increase in cancer-specific mortality among breast cancer patients completing < 85% of their planned chemotherapy [2]. Interventions that improve chemotherapy completion in early stage breast cancer patients may improve longer-term outcomes.
Exercise and health-related fitness variables (e.g., body composition, cardiovascular fitness, muscular strength, physical functioning) may affect chemotherapy completion [1]. In particular, previous studies in breast cancer have shown that body composition variables, such as greater muscle mass and lower adiposity, are associated with higher chemotherapy completion [2, 3]. Moreover, higher self-reported exercise prior to a breast cancer diagnosis has been associated with a higher chemotherapy completion [4]; and exercise initiated during breast cancer chemotherapy has improved treatment completion [6, 7]. Limited data exist on patient-reported physical functioning [8] and no studies have examined objective physical fitness [1]. Identifying modifiable health-related fitness variables that predict chemotherapy completion may lead to targeted interventions to improve treatment tolerability.
We previously completed two randomized controlled trials investigating exercise during adjuvant chemotherapy in early stage breast cancer patients [6, 9]. Here, we report a pooled analysis from these two trials examining baseline (pre-chemotherapy) exercise and health-related fitness variables as predictors of chemotherapy completion. We hypothesized that higher lean body mass and lower fat mass would be associated with improved chemotherapy completion. We considered the analyses of physical fitness, patient-reported physical functioning, and self-reported exercise behavior to be exploratory.
Materials and methods
Setting and participants
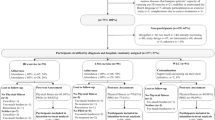
We pooled data from START [Supervised Trial of Aerobic versus Resistance Training (NCT00115713, http://clinicaltrials.gov)] [6] and CARE [Combined Aerobic and Resistance Exercise (NCT00249015, http://clinicaltrials.gov)] [9], which used very similar methods to examine various exercise interventions in breast cancer patients receiving adjuvant chemotherapy. START recruited from 2002 to 2005 and CARE recruited from 2008 to 2011. Both trials were multi-centered, randomized trials conducted in Edmonton, Ottawa, and Vancouver, Canada. In both START and CARE, ethics approval was obtained for all three centers and all participants provided written informed consent. Eligibility criteria for both trials included non-pregnant women ≥ 18 years of age with stage I–IIIa (START) or stage I–IIIc (CARE) breast cancer initiating first-line adjuvant chemotherapy. Exclusion criteria included incomplete axillary surgery, transabdominal rectus abdominis muscle reconstructive surgery, uncontrolled hypertension, cardiac illness, psychiatric illness, or disapproval by the oncologist.
Recruitment, randomization, and blinding
Eligible patients in both trials were approached by their treating oncologists during a medical visit prior to chemotherapy. The study coordinators followed-up with these patients and scheduled interested patients for baseline testing. After completing baseline assessments, patients were randomly assigned to their various interventions (described later) in a 1:1:1 ratio using a computer-generated program with random blocks of four or six.
Measures of baseline exercise and health-related fitness
In both START and CARE, baseline assessments generally occurred prior to the initiation of chemotherapy. If patients were unable or unwilling to complete all baseline assessments prior to chemotherapy, assessments could occur after the first chemotherapy cycle but always prior to the second chemotherapy cycle.
Body composition
Body weight and height were assessed without shoes using a balance beam scale in both START and CARE. BMI was calculated as weight in kilograms divided by the square of height in meters (kg/m2). In both trials, body composition was assessed using a DEXA scan [Hologic QDR-4500 (Vancouver), General Electric Lunar Expert/Prodigy (Ottawa and Edmonton)]. Body composition variables included lean body mass (kilograms and relative to total body weight), fat mass (kilograms and relative to total body weight), lean-to-fat ratio (total lean mass divided by total fat mass) [10]; and skeletal muscle mass index (lean body mass in kilograms divided by the square of height in meters) [11]. Participants were classified as sarcopenic if their skeletal muscle mass index was more than one standard deviation below age- and sex-based norms [12].
Physical fitness
In both START and CARE, cardiovascular fitness (i.e., VO2peak) was assessed using a maximal incremental treadmill protocol with measurements of expired gas [CPX-D; Medical Graphics, St Paul, MN (START) [6] and Parvo Medics TrueOne 2400, Parvo Medics Inc, Sandy, UT (CARE)] [9]. VO2peak was determined as the highest value over a 15-s period. Both trials used submaximal tests to estimate muscular strength (i.e., one-repetition maximum). In START, muscular strength was estimated from an eight-repetition maximum bench press and leg extension [6]. In CARE, muscular strength was estimated from a seven to ten-repetition maximum bench and leg press [9]. Given the different exercises used to measure lower body strength in each trial (i.e., leg extension vs. leg press), we could not combine them into a single score, and therefore, we only analyzed upper body (chest) strength.
Patient-reported physical functioning
In both trials, patient-reported physical functioning was assessed by the physical well-being (PWB), functional well-being (FWB), and fatigue subscales of the Functional Assessment of Cancer Therapy-Fatigue scale [13]. The PWB, FWB, and fatigue subscales were analyzed separately and combined into the Trial Outcome Index-Fatigue (TOI-F) scale. On all scales, including fatigue, higher scores indicated better functioning.
Self-reported exercise behavior
In both trials, exercise behavior was self-reported using the Godin Leisure Time Exercise Questionnaire [14], which consists of three questions on the average frequency of light (e.g., easy walking), moderate (e.g., fast walking), and vigorous (e.g., running) aerobic exercise during free time in a typical week for the past month. We modified the questionnaire to include the average duration of exercise and added a separate question on strength exercise. We asked patients to report their typical weekly exercise, since their breast cancer diagnosis. Total aerobic exercise time was calculated by multiplying vigorous aerobic exercise time (min/week) by two and adding it to moderate aerobic exercise time (min/week). Participants were categorized as meeting versus not meeting aerobic exercise guidelines (≥ 150 min of total aerobic exercise per week), strength exercise guidelines (≥ 2 resistance training sessions per week), and combined exercise guidelines (neither, aerobic only, strength only, and combined) [15].
Primary outcome measure
The primary outcome was chemotherapy completion, assessed as the average RDI for the originally planned regimen based on standard formulas [16,17,18] in both START and CARE. We used an RDI ≥ 85% as an indicator of chemotherapy completion based on its association with improved survival outcomes [5, 19]. Chemotherapy treatment data were obtained from medical records but we did not collect the reasons for dose reductions, delays, or discontinuations.
Interventions
Although baseline exercise and health-related fitness variables were assessed prior to the exercise interventions, the collection of the primary outcome of RDI occurred during the interventions. In both trials, participants were asked to perform thrice-weekly supervised exercise, beginning 1–2 weeks after starting chemotherapy and ending 3–4 weeks after completing chemotherapy. In START, participants were randomized to aerobic exercise training, resistance exercise training, or usual care (UC). In CARE, participants were randomized to 25–30 min of vigorous aerobic exercise, 50–60 min of vigorous aerobic exercise, or a combined dose of 50–60 min of vigorous aerobic and resistance exercise. Resistance exercise in both trials consisted of two sets of 8–12 (START) or 10–12 (CARE) repetitions at approximately 60–75% of one repetition maximum for nine different exercises involving major muscle groups. The UC group in START was asked not to exercise during chemotherapy.
Statistical analyses
We analyzed the associations between each continuous predictor variable and chemotherapy completion (< 85% RDI vs. ≥ 85% RDI) using independent t tests and analyses of covariance adjusting for significant covariates in our data set. We further categorized the continuous variables as categorical/ordinal variables based on clinically relevant (e.g., BMI, exercise guidelines, sarcopenia) or statistically determined (quintile) cut-points to identify any non-linear thresholds associated with chemotherapy completion. The potential thresholds in these categorical/ordinal variables were determined based on a criterion of ± 5% difference in the mean proportion of patients completing 85% RDI between adjacent quintiles (Supplementary Tables 1–4, online resource). We then analyzed the association between the identified thresholds (e.g., highest 80% vs. lowest 20%) and chemotherapy completion using unadjusted and adjusted logistic regression. Predictor variables that remained statistically significant (p < 0.05) after adjustment for covariates were analyzed in a multivariate logistic regression model with all significant predictors and covariates. Finally, as a sensitivity analysis, we re-analyzed the data excluding the UC group from START.
Results
Participant flow has been reported elsewhere for both START [6] and CARE [9]. In brief, 242 and 301 participants were randomized in START and CARE, respectively. Baseline characteristics of the combined study participants overall and by chemotherapy completion are described in Table 1. Briefly, 543 participants were included in the analyses with 79.6% (432/543) completing ≥ 85% of their planned RDI. Statistically significant differences in chemotherapy completion were found for trial (START vs. CARE), randomized arm (UC vs. exercise groups), and taxane-based chemotherapy (yes vs. no). These variables were included as covariates in the adjusted analyses.
Associations of predictors with chemotherapy completion
Supplementary Table 1 (online resource) presents the associations between body composition variables and chemotherapy completion. There were no significant associations between any body composition variable and chemotherapy completion. One potential threshold was analyzed comparing a BMI of severely obese vs. not severely obese but it was not significant (Table 2).
Supplementary Table 2 (online resource) presents the associations between physical fitness variables and chemotherapy completion. Breast cancer patients who completed ≥ 85% RDI had significantly higher absolute VO2peak (1.86 L/min vs. 1.78 L/min; p = 0.044) and relative VO2peak (27.0 mL/kg/min vs. 25.6 mL/kg/min; p = 0.050) compared to patients who completed < 85% RDI, but these associations were not significant after adjustment for covariates (p = 0.28 and p = 0.23, respectively). In terms of potential thresholds, there were no significant associations for relative VO2peak or relative chest strength (Table 2). Conversely, patients in the highest 20% vs. lowest 80% for absolute VO2peak were significantly more likely to complete ≥ 85% RDI in unadjusted (89.0% vs. 77.2%; OR 2.39, 95% CI 1.26–4.53, p = 0.008) (Fig. 1a) and adjusted analyses (ORadj 2.06, 95% CI 1.07–3.96, p = 0.031) (Table 2). Similarly, patients in the highest 80% vs. lowest 20% for absolute chest strength were significantly more likely to complete ≥ 85% RDI in unadjusted (81.5% vs. 71.4%; OR 1.76, 95% CI 1.08–2.87, p = 0.023) (Fig. 1b) and adjusted analyses (ORadj 1.80, 95% CI 1.09–2.98, p = 0.021) (Table 2).
Supplementary Table 3 (online resource) presents the associations between patient-reported physical functioning and chemotherapy completion. Breast cancer patients who completed ≥ 85% RDI had significantly higher PWB (21.9 vs. 20.3; p = 0.027) and TOI-F (79.1 vs. 74.4; p = 0.023) compared to patients who completed < 85% RDI, but these associations were not significant after adjustment for covariates (p = 0.08 and p = 0.11, respectively). In terms of potential thresholds, there were no significant differences for FWB or TOI-F (Table 2). Conversely, patients in the highest 80% vs. lowest 20% for PWB were significantly more likely to complete ≥ 85% RDI (81.6% vs. 71.3%; OR 1.79, 95% CI 1.10–2.89, p = 0.018) (Table 2; Fig. 2a). Moreover, patients in the highest 80% (less fatigue) vs. lowest 20% (more fatigue) for fatigue were significantly more likely to complete ≥ 85% RDI (81.3% vs. 71.3%; OR 1.75, 95% CI 1.06–2.90, p = 0.030) (Table 2; Fig. 2b). Neither of these associations remained significant after adjustment for significant covariates (Table 2).
Supplementary Table 4 (online resource) shows the associations between self-reported exercise behavior and chemotherapy completion. There were no significant associations between any of the self-reported exercise variables and chemotherapy completion. One potential threshold was analyzed comparing the combined exercise guideline vs. other guidelines but it was not significant (Table 2).
In a final multivariate model that included the two significant fitness predictors and four covariates, absolute VO2peak (ORadj 1.87, 95% CI 0.96–3.63, p = 0.07) and absolute chest strength (ORadj 1.65, 95% CI 0.99–2.74, p = 0.05) were borderline significantly associated with chemotherapy completion (Table 3).
In sensitivity analyses excluding the UC group (n = 461), there were no substantive differences in the results although the associations of the fitness variables with chemotherapy completion became slightly stronger. Specifically, the HR for absolute VO2peak (highest 20% vs. lowest 80%) increased from 2.06 (95% CI 1.07–3.96; p = 0.031) with the UC group to 2.45 (95% CI 1.12–5.35; p = 0.024) without the UC group. The HR for absolute chest strength (highest 80% vs. lowest 20%) increased from 1.80 (95% CI 1.09–2.98; p = 0.021) with the UC group to 1.94 (95% CI 1.11–3.41; p = 0.021) without the UC group. Finally, in the multivariate analyses (with both fitness variables in the model), the HR for absolute VO2peak increased from 1.87 (95% CI 0.96–3.63; p = 0.07) with the UC group to 2.19 (95% CI 0.99–4.84; p = 0.05) without the UC group; and for absolute chest strength the HR increased from 1.65 (95% CI 0.99–2.74; p = 0.05) with the UC group to 1.73 (95% CI 0.98–3.07; p = 0.06) without the UC group.
Discussion
To our knowledge, our study is the first to report a comprehensive set of exercise and health-related fitness predictors of chemotherapy completion in early stage breast cancer patients. We found that higher baseline (pre-chemotherapy) cardiovascular fitness and muscular strength were independently associated with a greater likelihood of completing ≥ 85% of the planned chemotherapy regimen. Patient-reported physical functioning variables were associated with chemotherapy completion in unadjusted but not adjusted analyses. Neither self-reported exercise behavior nor body composition variables were associated with chemotherapy completion in our data set. Our results may have important implications for the management of breast cancer patients.
Contrary to our hypotheses, body composition variables did not predict chemotherapy completion. Previous research has shown that breast cancer patients with higher BMI, greater fat mass, and lower lean mass are less likely to complete their chemotherapy [2, 20,21,22]. The majority of previous studies have assessed body composition through computed tomography [2, 21, 22]; however, similar associations have been reported using DEXA [20]. It is unclear why body composition variables did not predict chemotherapy completion in our study. One possible explanation is that our study population was healthier and fitter than the general population of breast cancer patients, because they participated in an exercise trial. For example, compared to previous studies, our study participants were 2–3 years younger [4, 8, 23, 24], had a lower BMI by 2–3 kg/m2 [2, 4, 20,21,22], and were 10–20% more likely to complete ≥ 85% of their chemotherapy [2, 4, 20,21,22]. Moreover, our study did not address the issue of chemotherapy dosing based on body composition, which is an important topic for future research.
Interestingly, cardiovascular fitness and muscular strength predicted chemotherapy completion in unadjusted and adjusted analyses. Specifically, patients in the highest 20% vs. lowest 80% of absolute VO2peak were twice as likely to complete an RDI ≥ 85%; and patients in the highest 80% vs. lowest 20% for absolute chest strength were 1.8 times more likely to complete an RDI ≥ 85%. In multivariate analyses, both variables were borderline significant, suggesting the possibility that aerobic fitness and muscular strength may have independent associations with chemotherapy completion. No previous studies have examined if objective physical fitness predicts chemotherapy completion.
Cardiovascular fitness is a robust measure of physical health that may influence chemotherapy completion through various mechanisms including improved heart function, cardiac output, left ventricular ejection fraction, blood pressure, blood volume, hemoglobin levels, and muscle metabolism. An improved cardiovascular system may affect dose-limiting toxicities such as cardiotoxicity, low blood counts, febrile neutropenia, peripheral neuropathy, and fatigue. Cardiovascular fitness declines significantly during chemotherapy [23]; therefore, patients with the highest VO2 reserve (top 20%) may be more buffered against declines associated with dose-limiting toxicities.
Muscular strength is important for improved physical functioning but its association with chemotherapy completion has not been documented. In one small study, a quicker sit-to-stand time and faster gait speed predicted chemotherapy completion in 26 lung cancer patients [24]. The obvious explanation for an association between muscular strength and chemotherapy completion would be greater muscle mass [25]; however, that explanation is not supported by our data. It is important to note, however, that DEXA does not measure actual skeletal muscle mass but rather lean soft tissue (body water, total protein, carbohydrates, non-fat lipids, and soft tissue) [26]. Moreover, although muscle mass is an important component of muscular strength, factors related to muscle quality (e.g., composition, metabolism, aerobic capacity, insulin resistance, fat infiltration, fibrosis, and neural factors) may also play an important role in muscular strength and physical functioning [27]. It is plausible that factors affecting muscle quality are also implicated in the body’s ability to metabolize drugs, thereby, reducing dose-limiting toxicities. Finally, it is also possible that the association between upper body strength and chemotherapy completion may be confounded by surgical factors (type of surgery, complications, and recovery); however, breast conserving surgery was not associated with improved chemotherapy completion in our study.
Although objectively measured physical fitness variables predicted chemotherapy completion, patient-reported physical functioning variables did not predict chemotherapy completion in adjusted models. One previous study reported that patient-reported physical functioning and fatigue severity were not associated with chemotherapy completion in 385 advanced breast cancer patients participating in a randomized reflexology trial [8]. The role of patient-reported physical functioning versus objectively measured physical functioning in predicting chemotherapy completion requires further research.
In our study, higher volumes of self-reported exercise were not associated with higher chemotherapy completion. In contrast, Usiskin et al. [4] reported that breast cancer patients who exercised ≥ 7.5 metabolic equivalent task-hour per week in the year before their diagnosis had a 7.6 times higher rate of chemotherapy completion. Usiskin et al.’s study has notable differences from our study including the timing of assessment (i.e., 1 year prior to diagnosis vs. since diagnosis) and exercise intensity (i.e., any vs. moderate-to-vigorous). Moreover, our study was restricted to breast cancer patients who were not currently doing structured exercise training which may have reduced variability in the measures. Finally, our study intervened on exercise behavior after the self-report assessment which may have altered any associations. Future research using observational cohort designs is needed to investigate the relationship between objectively measured exercise behavior at different pre-chemotherapy time points and chemotherapy completion.
Our findings may have clinical implications. Our data suggest that both aerobic fitness and muscular strength may be independently associated with chemotherapy completion. Nevertheless, the relative thresholds for benefit are quite distinct. Breast cancer patients would need to be in the top 20% of aerobic fitness to gain benefit, whereas they would only need to be in the top 80% of muscular strength to gain benefit. Practically speaking, it may be more realistic for breast cancer patients to improve their muscular strength from the bottom 20% to the top 80% than to improve their cardiovascular fitness from the bottom 80% to the top 20%. Consequently, modest strength training interventions in relatively weak women may be more likely to improve RDI than high intensity aerobic exercise interventions in relatively fit women. Moreover, absolute thresholds may have more clinical utility than relative thresholds. Based on our data, the top 20% of absolute VO2peak corresponds to a score of 2.22 L/min, whereas the top 80% of absolute chest strength corresponds to a score of 16.4 kg. If these absolute thresholds are supported in future research, they may be used to guide clinical exercise programs designed to improve RDI.
Our study has strengths and limitations. Most notably, our study is the first to examine a comprehensive set of exercise and health-related fitness predictors of chemotherapy completion in any cancer patient group. We had a large sample size, multicenter recruitment, no loss to follow-up, and high quality measures of body composition, cardiovascular fitness, muscular strength, patient-reported physical functioning, and chemotherapy completion. Limitations of our study include the data-driven exploratory approach, no adjustment for multiple testing, no measure of lower body strength, the self-report measure of exercise behavior, and the lack of information on reasons for chemotherapy modifications. Perhaps the main shortcoming is that we used baseline data from a randomized exercise trial which resulted in a select sample of healthier breast cancer patients, and also provided exercise interventions that occurred during the collection of the primary outcome. We did, however, adjust for randomization arm in the main analyses and also conducted sensitivity analyses excluding the UC group from START. Moreover, the select sample of healthier breast cancer patients may have worked against our hypotheses. Nevertheless, future studies using observational cohort designs are needed to recruit a more representative sample of breast cancer patients and provide an unaltered test of baseline exercise and fitness measures as predictors of chemotherapy completion.
In summary, we examined exercise and health-related fitness predictors of completing adjuvant chemotherapy for early stage breast cancer. Our results suggest that patients who are fitter and stronger may complete more of their planned chemotherapy. Further research is warranted to understand if and how exercise and health-related fitness variables may influence chemotherapy completion. Ultimately, randomized trials of exercise interventions prior to chemotherapy (prehabilitation) are needed to determine if there are causal effects of exercise and health-related fitness on chemotherapy tolerability and outcomes.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Abbreviations
- BMI:
-
Body Mass Index
- DEXA:
-
Dual energy X-ray absorptiometry
- PWB:
-
Physical well-being
- START:
-
Supervised Trial of Aerobic versus Resistance Training
- UC:
-
Usual care
- CARE:
-
Combined Aerobic and Resistance Exercise
- FWB:
-
Functional well-being
- RDI:
-
Relative dose intensity
- TOI-F:
-
Trial Outcome Index-Fatigue
References
Bland KA, Zadravec K, Landry T, Weller S, Meyers L, Campbell KL (2019) Impact of exercise on chemotherapy completion rate: a systematic review of the evidence and recommendations for future exercise oncology research. Crit Rev Oncol Hematol 136:79–85. https://doi.org/10.1016/j.critrevonc.2019.02.005
Cespedes Feliciano EM, Chen WY, Lee V, Albers KB, Prado CM, Alexeeff S, Xiao J, Shachar SS, Caan BJ (2020) Body composition, adherence to anthracycline and taxane-based chemotherapy, and survival after nonmetastatic breast cancer. JAMA Oncol 6(2):264–270. https://doi.org/10.1001/jamaoncol.2019.4668
Prado CM, Baracos VE, McCargar LJ, Reiman T, Mourtzakis M, Tonkin K, Mackey JR, Koski S, Pituskin E, Sawyer MB (2009) Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res 15(8):2920–2926. https://doi.org/10.1158/1078-0432.CCR-08-2242
Usiskin I, Li F, Irwin ML, Cartmel B, Sanft T (2019) Association between pre-diagnosis BMI, physical activity, pathologic complete response, and chemotherapy completion in women treated with neoadjuvant chemotherapy for breast cancer. Breast Cancer 26(6):719–728. https://doi.org/10.1007/s12282-019-00974-3
Zhang L, Yu Q, Wu XC, Hsieh MC, Loch M, Chen VW, Fontham E, Ferguson T (2018) Impact of chemotherapy relative dose intensity on cause-specific and overall survival for stage I-III breast cancer: ER+/PR+, HER2− vs. triple-negative. Breast Cancer Res Treat 169(1):175–187. https://doi.org/10.1007/s10549-017-4646-1
Courneya KS, Segal RJ, Mackey JR, Gelmon K, Reid RD, Friedenreich CM, Ladha AB, Proulx C, Vallance JK, Lane K, Yasui Y, McKenzie DC (2007) Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol 25(28):4396–4404. https://doi.org/10.1200/JCO.2006.08.2024
van Waart H, Stuiver MM, van Harten WH, Geleijn E, Kieffer JM, Buffart LM, de Maaker-Berkhof M, Boven E, Schrama J, Geenen MM, Meerum Terwogt JM, van Bochove A, Lustig V, van den Heiligenberg SM, Smorenburg CH, Hellendoorn-van Vreeswijk JA, Sonke GS, Aaronson NK (2015) Effect of low-intensity physical activity and moderate- to high-intensity physical exercise during adjuvant chemotherapy on physical fitness, fatigue, and chemotherapy completion rates: results of the PACES randomized clinical trial. J Clin Oncol 33(17):1918–1927. https://doi.org/10.1200/JCO.2014.59.1081
Wyatt G, Sikorskii A, Tesnjak I, Victorson D, Srkalovic G (2015) Chemotherapy interruptions in relation to symptom severity in advanced breast cancer. Support Care Cancer 23(11):3183–3191. https://doi.org/10.1007/s00520-015-2698-5
Courneya KS, McKenzie DC, Mackey JR, Gelmon K, Friedenreich CM, Yasui Y, Reid RD, Cook D, Jespersen D, Proulx C, Dolan LB, Forbes CC, Wooding E, Trinh L, Segal RJ (2013) Effects of exercise dose and type during breast cancer chemotherapy: multicenter randomized trial. J Natl Cancer Inst 105(23):1821–1832. https://doi.org/10.1093/jnci/djt297
Eisner MD, Blanc PD, Sidney S, Yelin EH, Lathon PV, Katz PP, Tolstykh I, Ackerson L, Iribarren C (2007) Body composition and functional limitation in COPD. Respir Res 8:7. https://doi.org/10.1186/1465-9921-8-7
Adams SC, Segal RJ, McKenzie DC, Vallerand JR, Morielli AR, Mackey JR, Gelmon K, Friedenreich CM, Reid RD, Courneya KS (2016) Impact of resistance and aerobic exercise on sarcopenia and dynapenia in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. Breast Cancer Res Treat 158(3):497–507. https://doi.org/10.1007/s10549-016-3900-2
Kelly TL, Wilson KE, Heymsfield SB (2009) Dual energy X-ray absorptiometry body composition reference values from NHANES. PLoS ONE 4(9):e7038. https://doi.org/10.1371/journal.pone.0007038
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E (1997) Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manag 13(2):63–74
Godin G, Shephard RJ (1985) A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 10(3):141–146
Schmitz KH, Courneya KS, Matthews C, Demark-Wahnefried W, Galvao DA, Pinto BM, Irwin ML, Wolin KY, Segal RJ, Lucia A, Schneider CM, von Gruenigen VE, Schwartz AL, American College of Sports Medicine (2010) American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc 42(7):1409–1426. https://doi.org/10.1249/MSS.0b013e3181e0c112
Hryniuk W, Bush H (1984) The importance of dose intensity in chemotherapy of metastatic breast cancer. J Clin Oncol 2(11):1281–1288. https://doi.org/10.1200/JCO.1984.2.11.1281
Hryniuk WM, Figueredo A, Goodyear M (1987) Applications of dose intensity to problems in chemotherapy of breast and colorectal cancer. Semin Oncol 14(4 Suppl 4):3–11
Longo DL, Duffey PL, DeVita VT Jr, Wesley MN, Hubbard SM, Young RC (1991) The calculation of actual or received dose intensity: a comparison of published methods. J Clin Oncol 9(11):2042–2051. https://doi.org/10.1200/JCO.1991.9.11.2042
Bonadonna G, Valagussa P, Moliterni A, Zambetti M, Brambilla C (1995) Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer: the results of 20 years of follow-up. N Engl J Med 332(14):901–906. https://doi.org/10.1056/NEJM199504063321401
van den Berg MM, Kok DE, Posthuma L, Kamps L, Kelfkens CS, Buist N, Geenen M, Haringhuizen A, Heijns JB, van Lieshout RH (2019) Body composition is associated with risk of toxicity-induced modifications of treatment in women with stage I–IIIB breast cancer receiving chemotherapy. Breast Cancer Res Treat 173(2):475–481
Gouerant S, Leheurteur M, Chaker M, Modzelewski R, Rigal O, Veyret C, Lauridant G, Clatot F (2013) A higher body mass index and fat mass are factors predictive of docetaxel dose intensity. Anticancer Res 33(12):5655–5662
Shachar SS, Deal AM, Weinberg M, Williams GR, Nyrop KA, Popuri K, Choi SK, Muss HB (2017) Body composition as a predictor of toxicity in patients receiving anthracycline and taxane-based chemotherapy for early-stage breast cancer. Clin Cancer Res 23(14):3537–3543. https://doi.org/10.1158/1078-0432.CCR-16-2266
Jones LW, Liang Y, Pituskin EN, Battaglini CL, Scott JM, Hornsby WE, Haykowsky M (2011) Effect of exercise training on peak oxygen consumption in patients with cancer: a meta-analysis. Oncologist 16(1):112–120. https://doi.org/10.1634/theoncologist.2010-0197
Collins JT, Noble S, Chester J, Davies HE, Evans WD, Farewell D, Lester JF, Parry D, Pettit R, Byrne A (2018) The value of physical performance measurements alongside assessment of sarcopenia in predicting receipt and completion of planned treatment in non-small cell lung cancer: an observational exploratory study. Support Care Cancer 26(1):119–127. https://doi.org/10.1007/s00520-017-3821-6
Prado CM, Cushen SJ, Orsso CE, Ryan AM (2016) Sarcopenia and cachexia in the era of obesity: clinical and nutritional impact. Proc Nutr Soc 75(2):188–198. https://doi.org/10.1017/S0029665115004279
Prado CMM, Heymsfield SB (2014) Lean tissue imaging: a new era for nutritional assessment and intervention. JPEN 38(8):940–953. https://doi.org/10.1177/0148607114550189
McGregor RA, Cameron-Smith D, Poppitt SD (2014) It is not just muscle mass: a review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev Healthspan 3(1):9–9. https://doi.org/10.1186/2046-2395-3-9
Funding
START and CARE were funded by the Canadian Breast Cancer Research Alliance. K.S. Courneya is supported by the Canada Research Chairs Program. D.W. Kang was supported by an Alberta Innovates Graduate Studentship. C.M. Friedenreich was supported by a Health Senior Scholar award from Alberta Innovates Health Solution and the Alberta Cancer Foundation Weekend to End Women’s Cancers Breast Cancer Chair.
Author information
Authors and Affiliations
Contributions
KYA: Conceptualization, formal analyses, visualization, writing the original draft, and writing review and editing. FZA, DWK, ARM, and SMN: Formal analyses, visualization, writing the original draft, and writing review and editing. CMF, DCM, KG, and JRM: Conceptualization, data curation, funding acquisition, methodology, project administration, resources, supervision, and writing review and editing. KSC: Conceptualization, data curation, formal analyses, funding acquisition, methodology, project administration, resources, supervision, visualization, writing the original draft, and writing review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict interests.
Ethics approval
In both START and CARE, ethics approval was obtained for all three sites (i.e., the Cross Cancer Institute in Edmonton, Alberta; the Ottawa Hospital Integrated Cancer Program and Cancer Center in Ottawa, Ontario; and the British Columbia Cancer Agency in Vancouver, British Columbia, Canada). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all participants in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
An, KY., Arthuso, F.Z., Kang, DW. et al. Exercise and health-related fitness predictors of chemotherapy completion in breast cancer patients: pooled analysis of two multicenter trials. Breast Cancer Res Treat 188, 399–407 (2021). https://doi.org/10.1007/s10549-021-06205-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06205-8