Abstract
Detection of disseminated tumour cells (DTCs) in bone marrow by immunocytochemistry (ICC) includes morphological evaluation of cytokeratin immunopositive cells. The aim of this study was to disclose the prognostic significance of different morphological categories of ICC-positive cells according to treatment status and tumour subtype. Bone marrow samples (at surgery) were analysed for the presence of cytokeratin-positive DTCs by a standard immunocytochemical method. The immunopositive cells were classified into the following categories, prior to any analysis of the association between DTCs and clinical outcome: tumour cells (TC), uninterpretable cells (UIC), hematopoietic cells (HC), and questionable HC (QHC). The analysis included 747 early breast cancer patients. Median follow-up was 84 months for relapse, and 99 months for death. The categorisation of the ICC positive cells revealed TC in 13.3 % of the patients, whereas 13.1, 17.8, and 21.4 % of the cases were positive for UIC, QHC, and HC, respectively. Analysing all patients, only TC and UIC predicted systemic relapse. Separate analysis of all patients not receiving adjuvant systemic treatment (No-Adj; n = 389) showed that only QHC were associated with reduced survival (DDFS: p = 0.008; BCSS: p = 0.004, log rank) and the presence of QHC also remained significant in multivariate analysis. Primary tumour subgroup analysis (of all patients) by hormone receptors (HR) and HER2, demonstrated that only TC/UIC had prognostic impact in the HR+/HER2− patients, whereas presence of QHC was associated with unfavourable outcome only in triple negative patients (DDFS: p = 0.004; BCSS: p = 0.024). Patients with ≥3HC had improved outcome compared to those with fewer/no HC (DDFS: p = 0.005; BCSS: p = 0.009). Hence, morphological DTC subgroups may differ in clinical significance according to primary tumour subtype and treatment status. This emphasises the importance of DTC characterisation, and separate analyses of DTC categories according to tumour subtype. Hematopoietic (“false positive”) cells might predict an immune-related favorable clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clinical relevance of disseminated tumour cells (DTCs) in the bone marrow (BM) at diagnosis and during follow-up (FU) has been demonstrated in several early breast cancer studies, including large pooled analyses [1, 2]. So far, the most standardised and validated detection method for DTCs is standard immunocytochemical analysis (ICC) of BM mononuclear cells (MNC) centrifuged onto glass slides (cytospins). The slides are immunostained by anti-cytokeratin monoclonal antibodies and visualised by alkaline phosphatase/monoclonal mouse anti-alkaline phosphatase (APAAP) detection system [3, 4]. In parallel, it has been recommended to stain additional cytospins with a negative control antibody of the same immunoglobulin subtype substituting the specific anti-cytokeratin antibody(ies). Cytospins are screened for immunostained cells by light microscopy, and the presence of DTCs concluded if certain morphological criteria are fulfilled [3, 4]. These criteria for distinction between DTC and occasional false positive hematopoietic cells (HC) have to some extent been clinically validated [5, 6]. However, tumour cells may display different morphological phenotypes, from small, anonymous or HC-like cells to unambigous tumour cell morphology [3].
In a previous study (“Oslo 1 Micrometastasis study”) we classified, prior to any knowledge of clinical outcome, ICC-positive cells in BM into four categories: Tumour cells (TC), HC, probable HC, in addition to cells/elements not possible to evaluate because of disruption/degeneration/poor conservation (uninterpretable cells, UIC) [6–9]. The categories TC and UIC were found to harbour cells significantly associated with reduced survival, whereas neither HC nor probable HC affected patient outcome [6]. However, survival analysis according to adjuvant systemic treatment status was not explored. As breast cancer can be classified into distinct subtypes (and morphological appearances) with different prognosis and treatment options [10, 11], the clinical significance of DTCs with different morphologies, should also be studied in relation to primary tumour subtype. In the present study, the immunomorphological cell categories of “DTCs” were revisited, analysing separately their prognostic impact according to adjuvant systemic treatment status and primary tumour subtype.
Materials and methods
Patients
Totally 920 non-metastatic breast cancer patients were enrolled (Oslo Micrometastasis Project; 1995–1998). Studies of prognostic significance of DTCs have been reported previously [1, 2, 6, 8]. In this study, only the cases with both specific test and negative control analysis of comparable and appropriate technical quality were included. In addition, information about systemic adjuvant treatment and clinical outcome (relapse and/or breast cancer death) was required. Totally 747 patients fulfilled these criteria. For 11 patients no relapse status was available. Systemic treatment followed the Norwegian guidelines for 1995–1998 and was administered to patients with pT2pN0G2–3 or pN+ status, as described in detail previously [8]. Clinico-pathologic data were extracted from the Oslo Micrometastasis Project database. Median FU time was 84 months (range 1–125 months) for relapse. From the Norwegian Death Cause Registry, additional information regarding extended FU time for death was available. Median FU for death was 99 months (range 2–128). The study was approved by the Regional Ethical Committee, and written consent obtained from all patients.
Primary tumour analyses
Primary tumour analyses were performed as described [7]. Grading was centrally performed on whole sections according to Elston/Ellis [12]. In cases of doubt another pathologist was consulted. In general, one paraffin block was examined per case.
Estrogen-, progesterone- and HER2 analysis
Immunohistochemical staining (IHC) for estrogen (ER) and progesterone (PR) receptors and HER2 was performed on whole paraffin sections as previously described [7]. In addition, tissue micro array (TMA) blocks were analysed for HER2 amplification by FISH (HER2 DNA probe kit; Vysis Inc, USA) [13]. The primary tumour was regarded ER or PR-positive if ≥10 % of TC nuclei were immunostained with the respective antibodies (according to prevailing recommendations when the study was conducted). Tumours were scored as HER2-positive if ≥10 % of the TC showed membranous immunostaining and/or HER2 FISH was positive (HER2/centromere 17 ratio ≥2.2) [13]. FISH was performed on all tumours with tissue available for this purpose.
Bone marrow analyses
Mononuclear cells from BM collected at surgery were analysed for DTCs by the standard ICC method, as described [7]. For each sample 4 cytospins (2 × 106 BM MNC) were immunostained for epithelial cells by anti-cytokeratin monoclonal antibodies AE1/AE3 (Sanbio), visualised by APAAP detection [14], and New Fuchsin. In parallel, negative control slides of 2 × 106 BM MNC were prepared from 605 of the 747 patients and incubated with a control antibody of the same immunoglobulin subtype substituting the specific anticytokeratin antibodies. For 139 patients, only 0.5 × 106 MNC were available for negative control analysis, for three patients 1–1.5 × 106 MNC. The slides were screened in light microscopy (manually or by Ariol SL50 automated screener), and immunostained elements classified according to predefined morphological criteria [3], as TC, UIC, questionable HC (QHC; named probable HC in Naume et al. [6]) or HC. Questionable HC were defined as cells intermediate between TC and HC, and exhibiting some HC characteristics.
A sample was scored as positive for a cell category if no similar positive cells were detected in the corresponding negative control, or if a higher number of cells of the respective cell type were present in AE1AE3-stained slides than in the corresponding negative control slides. The overall analysis of the ICC positive categories included all cases with appropriate negative control quality irrespective of the number of cells included in the control analysis (i.e. 0.5–2.0 × 106 MNC). This was decided in order not to exclude clinically relevant information from the morphological categories, being aware of the possibility for an increase in false positive cases. Still, patients with the same (or lower) number of ICC positive cells in the specific test than in the negative control analysis of only 0.5 × 106 MNC would be concluded as negative for the studied cell category, thereby reducing the rate of false positivity among these 139 patients. A separate analysis including only cases with equal cell number in specific test and negative control was also performed. Where relevant, the manuscript includes the essential elements of the REMARK criteria [15].
Statistical analysis
The SPSS software (version 17/18) was used. Survival time was measured from time of surgery to time of death or first evidence of recurrence. Breast cancer-specific survival (BCSS) was measured from date of surgery to breast cancer-related death, or otherwise censored at time of last follow-up, or at time of non-cancer-related death. Likewise, distant disease free survival (time to systemic relapse) (DDFS) was measured. Metastases to skeleton, liver, lungs, or central nervous system were recorded as systemic relapse. Kaplan–Meier survival curves for DDFS and BCSS were constructed. P values were computed by log-rank test. Cox proportional hazards regression was used for univariate and multivariate (stepwise backward elimination) analyses of prognostic impact of relevant variables. All p values are two-tailed, and p < 0.05 considered significant.
Results
Patients/tumour characteristics and ICC cell category status
Differences in the morphological appearance of ICC positive cells detected in the BM samples are illustrated in Fig. 1. Patient characteristics are presented in Table 1, and the associations between these and the presence of ICC positive cells of TC or UIC morphology and of QHC morphology, are presented in Table 2. Presence of ≥1 positive cells of the respective categories was considered positive. Analysing all patients, 13.3 % had the presence of TC, and 13.1, 17.8, and 21.4 % were positive for UIC, QHC, and HC, respectively. Presence of detected TC/UIC was significantly associated with lymph node status, pT-status, and HER2-status, while no significant association between QHC and clinico-pathological variables was found (Table 2). Considering cases with presence of TC, UIC and/or QHC, 72.5 % had cells from only one category.
Examples of morphological features of cells categorised into the tumor cell (TC), uninterpretable cell (UIC), questionable hematopoietic (QHC) and hematopoietic cell (HC) group. The classification was performed prospectively according to published guidelines [3]. TC a–c: The appearance in clusters, a nucleus clearly enlarged beyond the size of neighbouring bone marrow nuclei and irregular distribution of the cytoplasmic staining, are typical characteristics of TC (a). But the nucleus is not necessarily enlarged (b, c). Strong immunostaining for cytokeratin, partly covering the nucleus (b, c), with an irregular distribution, sometimes even suggesting a reticular/cytoskeletal network (b), is often seen in TC. Strong staining, partly covering the nucleus, and absence of HC characteristica placed cell C into the TC category. UIC (d–f): These cells/elements are all destroyed/degenerated and with a nucleus not possible to identify, therefore classified in the UIC group. QHC (g–i): Obvious HC characteristics are lacking, the cytoplasmic staining intensity is somewhat variable, and in cell G irregularly distributed, which could indicate TC. But the nuclei are small, resembling neighbouring cells, and the quite regularly dispersed cytoplasm in H resemble HC cytoplasm, and nuclear covering is lacking/limited. HC (j, k): Typical HC features with low nuclear/cytoplasmic ratio, regularly dispersed cytoplasm suggesting microvacuolisation (l), with pin-point vacuoles (j, k), and plasma cell-like morphology with a small, eccentric nucleus. Cytoplasmic staining not covering the nucleus
ICC-positive cell category and clinical outcome
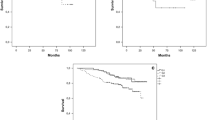
During the median observation time of 84 months (range 1–125 months) for relapse and 99 months (range 2–128) for death, 139 (18.9 %) patients experienced systemic relapse and 111 (14.9 %) died of breast cancer. The association between ICC cell category status and outcome was analysed. When all patients were included in the analysis, only presence of TC and UIC predicted systemic relapse (p = 0.005 and p = 0.030, respectively, Fig. 2). Separate analysis of patients that had not received adjuvant systemic treatment (No-Adj; n = 389) and those that had (Adj; n = 358), showed that among No-Adj patients, only those harbouring QHC experienced reduced survival. In contrast, only TC and UIC predicted DDFS and BCSS in Adj patients (Figs. 2, 3; Table 3).
Distant disease-free survival among patients with (Pos) or without (Neg) ICC-positive cells in the bone marrow within the indicated morphological cell categories; for all, for Adj, and for No-Adj patients. P values were computed by log-rank test. Due to missing data in the database for a few patients, the number of patients included in the various survival analyses differ
Breast cancer-specific survival among patients with (Pos) or without (Neg) ICC-positive cells in the BM within the indicated morphological cell categories; for all, for Adj, and for No-Adj patients. Due to missing data in the database for a few patients, the number of patients included in the various survival analyses differ
For No-Adj patients, QHC status, and primary tumour factors found to be prognostic in univariate analysis (Table 3) were included in a multivariate analysis. The presence of QHC retained independent prognostic significance both for DDFS and BCSS. Additionally, HER2 status was significant for DDFS, while grade and lymph node status were significant for both DDFS and BCSS (Table 4). Multivariate analysis of Adj patients is presented in Supplementary Table 1 (Online Resource 1).
The patients were subgrouped into three categories according to hormone receptor (HR) and HER2 status of the primary tumour. A prognostic impact of TC and UIC were observed only in HR+/HER− subgroup (n = 526) (p ≤ 0.003), but not in the HER2+ (n = 79) or triple negative (TN) subgroup (n = 116). In contrast, presence of QHC was associated with worse outcome in TN patients (p = 0.004 for DDFS, p = 0.024 for BCSS) with no significant prognostic impact in the other two subgroups (Fig. 4; Table 5). In multivariate analyses, the prognostic significance of QHC in TN patients was retained for both DDFS and BCSS (DDFS: Hazard ratio 2.5 (CI 1.2–5.3), p = 0.017; BCSS: Hazard ratio 2.4 (CI 1.1–5.4), p = 0.029), and BCSS was influenced by the TC/UIC status in HR+/HER2− patients (DDFS: Hazard ratio 1.6 (CI 1.0–2.7), p = 0.076; BCSS: Hazard ratio 2.1 (CI 1.2–3.8), p = 0.016) (Supplementary Table 2; Online Resource 2).
Survival analyses (DDFS and BCSS) for patients with (Pos) or without (Neg) the indicated DTC subcategory (TC/UIC versus QHC) detected in the BM; for HR+/HER2− and for HR−/HER2− patients. Due to missing data in the database for a few patients, the number of patients included in the various survival analyses differ
Additional survival analyses were also performed after exclusion of patients with presence of DTCs with TC morphology. As presented in Fig. 5, QHC status had the same impact on clinical outcome. Furthermore, the exclusion of the 140 patient samples from which the negative controls included less than 1.5 × 106 MNC, did not alter the results (Supplementary Fig. 1; Online Resource 3).
A separate analysis of the tumour subgroups according to the morphological categories of DTCs (i.e., TC, UIC, and QHC) in No-Adj patients revealed that TN patients with the presence of QHC had markedly reduced DDFS (p = 0.004) and BCSS (p = 0.002) (Supplementary Figs. 2 and 3; Online Resource 4 and 5). In the same subgroup of patients (No-adj, TN), the presence of TC was associated with reduced DDFS (p = 0.027), but not BCSS (p = 0.224). No association was observed for UIC for any No-Adj subgroup.
Analysis of number of false positive HC
The presence of ≥1 HC did not negatively affect clinical outcome, compatible with the unequivocal hematopoietic cell morphology of these cells. Comparison of 2 × 106 MNC stained by AE1AE3 with the same number of cells stained by negative control antibody, showed a similar frequency of HC (26.7 and 23.9 %, respectively). Of all patients, 91.4 % had either presence of none (61.4 %) or 1–2 (30.0 %) ICC-positive cells with definite HC morphology in specific test and negative controls added together. In the remaining cases 3–7 cells were detected. As these cells were defined as unspecific, we performed an analysis based on the total number of HC present in all slides analysed (both AE1AE3 and negative control slides). Patients with ≥3 HC had significantly improved DDFS (p = 0.005, log-rank) and BCSS (p = 0.009, log-rank) compared to those with fewer or no HC (Fig. 6). Only 4.8 % of the patients with a total of ≥3 HC experienced metastasis, versus 20.2 % of those with <3 HC. Overlapping survival curves were observed for patients with the presence of 1 HC, 2 HC, or no HC (data not shown).
Survival analyses (DDFS and BCSS) among patients harbouring a total of ≥3 HC versus patients harbouring 0–2 HC, in the bone marrow. Patients with ≥3 HC had significantly improved DDFS (Hazard ratio 0.2, 95 %CI 0.1–0.7, p = 0.010) and BCSS (Hazard ratio 0.2, 95 %CI 0.05–0.8, p = 0.019) compared to those with fewer or no HC
Discussion
We have previously reported morphological cell classification of immunopositive elements to increase the clinical significance of DTCs in BM [6]. Morphological interpretation of detected elements is also part of the standardised method for detection of circulating tumour cells in blood (CTCs) by the Cellsearch system [16]. There is, however, a morphological overlap between real tumour cells and false positive HC, as illustrated by the occasional presence of cells with morphology compatible with tumour cells in negative control specimens and in BM samples from healthy donors [3, 17, 18].
This study shows a clinically significant biological heterogeneity within the DTC population. The results demonstrate that QHC positivity is associated with reduced survival among patients that did not receive systemic adjuvant treatment, indicating presence of DTCs within this cell category. In addition, TN patients (irrespective of treatment status) with presence of QHC had reduced survival, whereas in the HER2+ or HR+/HER2− subgroups, QHC positivity did not affect survival. It cannot be excluded that misclassification of some HC as QHC might have influenced the results, but the contrasting finding of TC/UIC presence associated with reduced survival only for the systemically treated patients, and predominantly for patients with HR+/HER2− status, indicates biological differences. These results show that a definition of DTC positivity based on a combination of different cell morphologies, would have reduced the clinical significance of DTCs. Furthermore, the inclusion of the entire patient population (Adj + No-Adj) in the analyses diminishes the clinical information obtained from DTC analysis. The data indicate that the DTC population is morphologically heterogenous, including cells with clear epithelial tumour cell morphology as well as anonymous cells with some resemblance to HC. Differences in cell biology and possibly in treatment sensitivity between these cell categories, seem to be reflected in their morphological appearance. The interpretation of these results is hampered by the overlap in morphology between ICC false positive cells, as they appear in healthy controls, and tumour cells [3, 17, 18]. Furthermore, the possibility to perform quantitative analysis is restricted because of the low number of these cells in the samples. Analysis of a higher number of BM cells would probably give additional information, if combined with additional characterisation of the cells. Unfortunately, additional cytospins are not available for this purpose. Uninterpretable cells were defined as cells/elements not possible to evaluate because of disruption/degeneration/poor conservation. The finding of prognostic significance for this equivocal ICC positive category is not unique. Analysis for CTCs by the Cellsearch system has also shown that cytokeratin positive cell fragments have prognostic significance [19].
The patients in this study were selected for adjuvant therapy on the basis of standard risk markers, as tumour size, lymph node metastasis and tumour grade, according to Norwegian guidelines at the time of inclusion. The Adj patients therefore represented higher risk individuals compared to the No-Adj. It might be speculated if the TCs, with their quite recognisable tumour cell morphology, represent dissemination/desquamation from the bulk of tumour, in patients with generally more advanced disease. Indeed the frequency of TC/UIC was clearly higher in lymph node positive patients than in lymph node negative, which was not the case for QHC (Table 2). As only the presence of cells in the TC/UIC group predicted reduced survival among the HR+/HER2− patients (enriched for luminal A patients), the tumour-initiating cells of this tumour subtype might predominate in the TC/UIC subpopulation. It has been proposed that tumor cells all along the differentiation/hierarchical tree in luminal-like breast cancers may have tumour-initiating properties [20]. As the Luminal A subgroup also has the best prognosis, patients at very early stages of this disease (with node negative status, not receiving systemic treatment) would have a reduced chance of developing metastasis, despite presence of a low number of DTCs. The lack of metastasis formation might be explained by unsupportive microenvironment, elimination of tumour cells by the immune system and/or dormancy state of the scarce DTCs [21, 22]. Among the patients with TN tumours, our results indicate that DTCs within the QHC group include tumour-initiating cells. The anonymous, undifferentiated appearance typical of QHC, often with a modest cytokeratin staining compatible with a low/downregulated cytokeratin expression, might signify epithelial-mesenchymal transformation/stemness [23]. This does not exclude presence of tumour-initiating cells within the TC/UIC categories. A separate analysis of the TC group (excluding UIC) showed that TN No-Adj patients with presence of TC actually had reduced DDFS, but BCSS was not significantly affected. Analysis of the No-Adj patients according to QHC status in the TN patients, showed that presence of QHC had the strongest prognostic impact in the TN patients (Supplementary Figs. 2 and 3; Online Resource 4 and 5). The lack of significance of QHC in the entire Adj group (Fig. 2) may in part be explained by the fact that only a smaller fraction of the Adj patients, 53 out of 358, were TN. Furthermore, a better elimination of tumour-initiating, disseminated cells by the adjuvant treatment in TN patients than in the large group of HR+/HER2− patients is also a possible explanation [24, 25]. Outcome comparison of Adj versus No-Adj patients revealed a hazard ratio for systemic relapse of 2.3 for the HR+/HER2− patients (p = 0.001) and 1.9 for the TN patients (p = 0.086).
We have previously identified plasma cells/pre-plasma cells as responsible for false positive reactions in DTC diagnostics [26]. The beneficial outcome for those with ≥3 HC in our study might support an association between the B cell lineage response and inhibition of tumour progression, as part of an immunological response [27]. Cancer progression, as well as the response to anti-cancer therapy, are influenced and modulated by the immune system. Different molecular signatures, signaling patterns and susceptibility loci of importance have been identified [28–30]. It has been reported that cytotoxic T-lymphocytes and natural killer cells exhibit antitumour activity [31]. In a recent study by Kristensen et al. [29], primary tumour immune signatures were shown to predict survival. Although they demonstrated that patients with a Th1-expression profile signature had the most favourable outcome, it has been shown that B-lymphocyte responses may both inhibit and potentiate tumour progression [27, 29, 31].
In addition to morphological classification, further characterisation of single DTCs at the molecular level is desirable. Several methods have been presented for this purpose, although not yet as high-throughput routine analyses. These include array CGH, multiplex immunological and FISH analyses, and analyses of gene expression [32–38]. These techniques are resource demanding and still lack appropriate standardisation and thorough testing on BM samples. Therefore, morphological subclassification of detected elements combined with an optimised interpretation, taking aspects as therapy and primary tumour molecular subtype into account, might serve as an important basic/screening analysis for selection of clinical relevant samples for such additional DTC analyses.
Studies comparing CTCs and DTCs have shown differences in their clinical significance [39, 40], and different prognostic relevance of CTCs versus DTCs according to primary tumour characteristics [41, 42]. Although it cannot be excluded that such differences may partially have methodological reasons, these observations have similarities with our results. It has also been reported that certain primary tumour signatures are associated with presence of DTCs or CTCs [43–45]. Therefore, optimal monitoring of DTCs and CTCs should incorporate information about primary tumour expression profiles (if available) and other clinico-pathological parameters.
In conclusion, this study reveals a biologically and clinically relevant heterogeneity within the DTC population, and highlights the importance of further characterisation of DTC at the single cell level. Studies of DTCs should also take into account the molecular subtype of the primary tumour.
Abbreviations
- DTCs:
-
Disseminated tumour cells
- BM:
-
Bone marrow
- FU:
-
Follow-up
- ICC:
-
Immunocytochemical analysis
- MNC:
-
Mononuclear cells
- APAAP:
-
Alkaline phosphatase/monoclonal mouse anti-alkaline phosphatase
- HC:
-
Hematopoietic cells
- TC:
-
Tumour cells
- UIC:
-
Uninterpretable cells
- pT:
-
Histopathological primary tumor size status
- pN:
-
Histopathological lymph node status
- G1, 2, 3:
-
Histopathological grade 1–3
- IHC:
-
Immunohistochemical staining
- ER:
-
Estrogen receptor(s)
- PR:
-
Progesteron receptor(s)
- HER2:
-
Human epidermal growth factor receptor 2
- TMA:
-
Tissue microarray
- FISH:
-
Fluorescence in situ hybridization
- QHC:
-
Questionable hematopoietic cells
- BCSS:
-
Breast cancer-specific survival
- DDFS:
-
Distant disease-free survival
- HR:
-
Hormone receptor(s)
- TN:
-
Triple negative
- CTCs:
-
Circulating tumour cells
References
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Pierga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundt G, Strobl B, Fehm T, Wong GY, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353:793–802
Janni W, Vogl FD, Wiedswang G, Synnestvedt M, Fehm T, Juckstock J, Borgen E, Rack B, Braun S, Sommer H, Solomayer E, Pantel K, Nesland J, Friese K, Naume B (2011) Persistence of disseminated tumor cells in the bone marrow of breast cancer patients predicts increased risk for relapse–a European pooled analysis. Clin Cancer Res 17:2967–2976
Borgen E, Naume B, Nesland JM, Kvalheim G, Beiske K, Fodstad O, Diel I, Solomayer EF, Theocharous P, Coombes RC, Smith BM, Wunder E, Marolleau JP, Garcia J, Pantel K (1999) Standardization of the immunocytochemical detection of cancer cells in BM and blood: I. Establishment of objective criteria for the evaluation of immunostained cells. Cytotherapy 1:377–388
Fehm T, Braun S, Muller V, Janni W, Gebauer G, Marth C, Schindlbeck C, Wallwiener D, Borgen E, Naume B, Pantel K, Solomayer E (2006) A concept for the standardized detection of disseminated tumor cells in bone marrow from patients with primary breast cancer and its clinical implementation. Cancer 107:885–892
Bidard FC, Vincent-Salomon A, Gomme S, Nos C, de Rycke Y, Thiery JP, Sigal-Zafrani B, Mignot L, Sastre-Garau X, Pierga JY (2008) Disseminated tumor cells of breast cancer patients: a strong prognostic factor for distant and local relapse. Clin Cancer Res 14:3306–3311
Naume B, Wiedswang G, Borgen E, Kvalheim G, Karesen R, Qvist H, Janbu J, Harbitz T, Nesland JM (2004) The prognostic value of isolated tumor cells in bone marrow in breast cancer patients: evaluation of morphological categories and the number of clinically significant cells. Clin Cancer Res 10:3091–3097
Naume B, Borgen E, Kvalheim G, Karesen R, Qvist H, Sauer T, Kumar T, Nesland JM (2001) Detection of isolated tumor cells in bone marrow in early-stage breast carcinoma patients: comparison with preoperative clinical parameters and primary tumor characteristics. Clin Cancer Res 7:4122–4129
Wiedswang G, Borgen E, Karesen R, Kvalheim G, Nesland JM, Qvist H, Schlichting E, Sauer T, Janbu J, Harbitz T, Naume B (2003) Detection of isolated tumor cells in bone marrow is an independent prognostic factor in breast cancer. J Clin Oncol 21:3469–3478
Wiedswang G, Borgen E, Karesen R, Qvist H, Janbu J, Kvalheim G, Nesland JM, Naume B (2004) Isolated tumor cells in bone marrow three years after diagnosis in disease-free breast cancer patients predict unfavorable clinical outcome. Clin Cancer Res 10:5342–5348
Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, Speed D, Lynch AG, Samarajiwa S, Yuan Y, Graf S, Ha G, Haffari G, Bashashati A, Russell R, McKinney S, Langerod A, Green A, Provenzano E, Wishart G, Pinder S, Watson P, Markowetz F, Murphy L, Ellis I et al (2012) The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486:346–352
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ (2011) Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, Van d V, Wheeler TM, Hayes DF (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Arch Pathol Lab Med 131:18–43
Cordell JL, Falini B, Erber WN, Ghosh AK, Abdulaziz Z, MacDonald S, Pulford KA, Stein H, Mason DY (1984) Immunoenzymatic labeling of monoclonal antibodies using immune complexes of alkaline phosphatase and monoclonal anti-alkaline phosphatase (APAAP complexes). J Histochem Cytochem 32:219–229
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235
Kraan J, Sleijfer S, Strijbos MH, Ignatiadis M, Peeters D, Pierga JY, Farace F, Riethdorf S, Fehm T, Zorzino L, Tibbe AG, Maestro M, Gisbert-Criado R, Denton G, de Bono JS, Dive C, Foekens JA, Gratama JW (2011) External quality assurance of circulating tumor cell enumeration using the Cell Search® system: a feasibility study. Cytometry B Clin Cytom 80:112–118
Borgen E, Pantel K, Schlimok G, Muller P, Otte M, Renolen A, Ehnle S, Coith C, Nesland JM, Naume B (2006) A European interlaboratory testing of three well-known procedures for immunocytochemical detection of epithelial cells in bone marrow. Results from analysis of normal bone marrow. Cytom B Clin Cytom 70:400–409
Krag DN, Kusminsky R, Manna E, Weaver D, Harlow SP, Covelli M, Stanley MA, McCahill L, Ittleman F, Leavitt B, Krag M, Amarante P (2009) Cytokeratin-positive cells in the bone marrow of breast cancer patients and noncancer donors. Appl Immunohistochem Mol Morphol 17:403–408
Coumans FA, Doggen CJ, Attard G, de Bono JS, Terstappen LW (2010) All circulating EpCAM+ CK+. Ann Oncol 21:1851–1857
Kim C, Paik S (2010) Gene-expression-based prognostic assays for breast cancer. Nat Rev Clin Oncol 7:340–347
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Meng S, Tripathy D, Frenkel EP, Shete S, Naftalis EZ, Huth JF, Beitsch PD, Leitch M, Hoover S, Euhus D, Haley B, Morrison L, Fleming TP, Herlyn D, Terstappen LW, Fehm T, Tucker TF, Lane N, Wang J, Uhr JW (2004) Circulating tumor cells in patients with breast cancer dormancy. Clin Cancer Res 10:8152–8162
Jordan NV, Johnson GL, Abell AN (2011) Tracking the intermediate stages of epithelial-mesenchymal transition in epithelial stem cells and cancer. Cell Cycle 10:2865–2873
Hall C, Krishnamurthy S, Lodhi A, Mosalpuria K, Kuerer HM, Meric-Bernstam F, Bedrosian I, Hunt KK, Lucci A (2010) Disseminated tumor cells in biologic subtypes of stage I–III breast cancer patients. Ann Surg Oncol 17:3252–3258
von Minckwitz G, Martin M (2012) Neoadjuvant treatments for triple-negative breast cancer (TNBC). Ann Oncol 23 Suppl 6:vi35–vi39
Borgen E, Beiske K, Trachsel S, Nesland JM, Kvalheim G, Herstad TK, Schlichting E, Qvist H, Naume B (1998) Immunocytochemical detection of isolated epithelial cells in bone marrow: non-specific staining and contribution by plasma cells directly reactive to alkaline phosphatase. J Pathol 185:427–434
Schmidt M, Hellwig B, Hammad S, Othman A, Lohr M, Chen Z, Boehm D, Gebhard S, Petry I, Lebrecht A, Cadenas C, Marchan R, Stewart JD, Solbach C, Holmberg L, Edlund K, Kultima HG, Rody A et al (2012) A comprehensive analysis of human gene expression profiles identifies stromal immunoglobulin kappa C as a compatible prognostic marker in human solid tumors. Clin Cancer Res 18:2695–2703
Blankenstein T, Coulie PG, Gilboa E, Jaffee EM (2012) The determinants of tumour immunogenicity. Nat Rev Cancer 12:307–313
Kristensen VN, Vaske CJ, Ursini-Siegel J, Van LP, Nordgard SH, Sachidanandam R, Sorlie T, Warnberg F, Haakensen VD, Helland A, Naume B, Perou CM, Haussler D, Troyanskaya OG, Borresen-Dale AL (2012) Integrated molecular profiles of invasive breast tumors and ductal carcinoma in situ (DCIS) reveal differential vascular and interleukin signaling. Proc Natl Acad Sci USA 109:2802–2807
Stevens KN, Fredericksen Z, Vachon CM, Wang X, Margolin S, Lindblom A, Nevanlinna H, Greco D, Aittomaki K, Blomqvist C, Chang-Claude J, Vrieling A, Flesch-Janys D, Sinn HP, Wang-Gohrke S, Nickels S, Brauch H, Ko YD, Fischer HP, Schmutzler RK, Meindl A, Bartram CR, Schott S, Engel C, Godwin AK et al (2012) 19p13.1 is a triple-negative-specific breast cancer susceptibility locus. Cancer Res 72:1795–1803
DeNardo DG, Coussens LM (2007) Inflammation and breast cancer. Balancing immune response: crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res 9:212
Balic M, Rapp N, Stanzer S, Lin H, Strutz J, Szkandera J, Daidone MG, Samonigg H, Cote RJ, Dandachi N (2011) Novel immunofluorescence protocol for multimarker assessment of putative disseminating breast cancer stem cells. Appl Immunohistochem Mol Morphol 19:33–40
Fehm T, Muller V, Alix-Panabieres C, Pantel K (2008) Micrometastatic spread in breast cancer: detection, molecular characterization and clinical relevance. Breast Cancer Res 10(Suppl 1):S1
Mathiesen RR, Fjelldal R, Liestol K, Due EU, Geigl JB, Riethdorf S, Borgen E, Rye IH, Schneider IJ, Obenauf AC, Mauermann O, Nilsen G, Christian LO, Borresen-Dale AL, Pantel K, Speicher MR, Naume B, Baumbusch LO (2011) High-resolution analyses of copy number changes in disseminated tumor cells of patients with breast cancer. Int J Cancer 131:E405–E415
Riethdorf S, Pantel K (2008) Disseminated tumor cells in bone marrow and circulating tumor cells in blood of breast cancer patients: current state of detection and characterization. Pathobiology 75:140–148
Pierga JY, Bonneton C, Magdelenat H, Vincent-Salomon A, Nos C, Boudou E, Pouillart P, Thiery JP, de CP (2005) Real-time quantitative PCR determination of urokinase-type plasminogen activator receptor (uPAR) expression of isolated micrometastatic cells from bone marrow of breast cancer patients. Int J Cancer 114:291–298
Fehm T, Solomayer EF, Meng S, Tucker T, Lane N, Wang J, Gebauer G (2005) Methods for isolating circulating epithelial cells and criteria for their classification as carcinoma cells. Cytotherapy 7:171–185
Payne RE, Wang F, Su N, Krell J, Zebrowski A, Yague E, Ma XJ, Luo Y, Coombes RC (2012) Viable circulating tumour cell detection using multiplex RNA in situ hybridisation predicts progression-free survival in metastatic breast cancer patients. Br J Cancer 106:1790–1797
Bidard FC, Vincent-Salomon A, Sigal-Zafrani B, Dieras V, Mathiot C, Mignot L, Thiery JP, Sastre-Garau X, Pierga JY (2008) Prognosis of women with stage IV breast cancer depends on detection of circulating tumor cells rather than disseminated tumor cells. Ann Oncol 19:496–500
Pierga JY, Bonneton C, Vincent-Salomon A, de CP, Nos C, Blin N, Pouillart P, Thiery JP, Magdelenat H (2004) Clinical significance of immunocytochemical detection of tumor cells using digital microscopy in peripheral blood and bone marrow of breast cancer patients. Clin Cancer Res 10:1392–1400
Molloy TJ, Bosma AJ, Baumbusch LO, Synnestvedt M, Borgen E, Russnes HG, Schlichting E, van’t Veer LJ, Naume B (2011) The prognostic significance of tumour cell detection in the peripheral blood versus the bone marrow in 733 early-stage breast cancer patients. Breast Cancer Res 13:R61
Ignatiadis M, Perraki M, Apostolaki S, Politaki E, Xenidis N, Kafousi M, Stathopoulos E, Lianidou E, Sotiriou C, Georgoulias V, Mavroudis D (2007) Molecular detection and prognostic value of circulating cytokeratin-19 messenger RNA-positive and HER2 messenger RNA-positive cells in the peripheral blood of women with early-stage breast cancer. Clin Breast Cancer 7:883–889
Molloy TJ, Roepman P, Naume B, van’t Veer LJ (2012) A prognostic gene expression profile that predicts circulating tumor cell presence in breast cancer patients. PLoS ONE 7:e32426
Naume B, Zhao X, Synnestvedt M, Borgen E, Russnes HG, Lingjaerde OC, Stromberg M, Wiedswang G, Kvalheim G, Karesen R, Nesland JM, Borresen-Dale AL, Sorlie T (2007) Presence of bone marrow micrometastasis is associated with different recurrence risk within molecular subtypes of breast cancer. Mol Oncol 1:160–171
Woelfle U, Cloos J, Sauter G, Riethdorf L, Janicke F, van Diest P, Brakenhoff R, Pantel K (2003) Molecular signature associated with bone marrow micrometastasis in human breast cancer. Cancer Res 63:5679–5684
Acknowledgments
We thank the staff at The Micrometastasis Laboratory, Department of Pathology, Radiumhospitalet, for their excellent technical assistance. The study was supported by The Research Council of Norway, South-Eastern Norway Regional Health Authority, The Norwegian Cancer Society, K. G. Jebsen Centre for Breast Cancer Research, and the European Commission within the 7th Framework Programme (The Miracle project).
Conflict of interest
The authors declare no conflicts of interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Synnestvedt and Borgen contributed equally to the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
Cox multivariate analysis in patients receiving adjuvant systemic treatment (Adj). (DOC 35 kb)
Supplementary Table 2
Cox multivariate analysis. Prognostic significance of DTC categories according to primary tumour subgroups. (DOC 60 kb)
Supplementary Fig. 1
Survival analyses (DDFS and BCSS) for patients with (Pos) or without (Neg) QHC detected in the BM; for all No-Adj patients, and for all TN patients; only patient samples including ≥1.5x106 cells in the negative control included. P values were computed by log-rank test. (TIFF 510 kb)
Supplementary Fig. 2
Distant disease-free survival among No-Adj patients with (Pos) or without (Neg) the indicated DTC subcategory (TC versus UIC versus QHC) detected in the BM; for No-Adj HR +/HER2- patients, for No-Adj HER2 + patients (HR- or +) and for No-Adj TN patients. Due to missing data in the database for a few patients, the number of patients included in the various survival analyses differ. (TIFF 747 kb)
Supplementary Fig. 3
Breast cancer-specific survival among No-Adj patients with (Pos) or without (Neg) the indicated DTC subcategory (TC versus UIC versus QHC) detected in the BM; for No-Adj HR +/HER2- patients, for No-Adj HER + patients (HR- or +) and for No-Adj TN patients. Due to missing data in the database for a few patients, the number of patients included in the various survival analyses differ. (TIFF 721 kb)
Rights and permissions
About this article
Cite this article
Synnestvedt, M., Borgen, E., Schlichting, E. et al. Disseminated tumour cells in the bone marrow in early breast cancer: morphological categories of immunocytochemically positive cells have different impact on clinical outcome. Breast Cancer Res Treat 138, 485–497 (2013). https://doi.org/10.1007/s10549-013-2439-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-013-2439-8