Abstract
Male breast cancer (mBC) is a rare entity. As detection of disseminated tumor cells (DTCs) in the bone marrow of females with early stage breast cancer is a promising prognostic marker, we aimed to determine the prevalence and prognostic value of DTCs in mBC. Bone marrow aspirates were collected from male patients undergoing primary surgery for early stage breast cancer (T1–4, N0–2, M0) at Tuebingen University, Germany, between January 2001 and April 2015. DTCs were identified by immunocytochemistry (pancytokeratin antibody A45/B-B3) and cytomorphology. 24 patients with mBC were included into the analysis. DTCs were detected in four of these (17 %). There was no significant association between the DTC status and any other clinicopathological parameter. Also, no significant impact of the DTC status on DFS or OS could be observed. DTCs are detectable in patients with early stage mBC. The detection rate is comparable to that in women. No associations between DTCs and clinicopathological features or prognosis were observed, which is most likely due to the small sample size. The detection of DTCs in male patients with early stage breast cancer emphasizes the transmission of future clinical applications for DTCs from women to men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Male breast cancer (mBC) is a rare malignancy that accounts for less than 1 % of all breast cancers and less than 0.5 % of male cancer deaths in the U.S. [1]. The most frequent type is invasive ductal carcinoma, and only few cases of invasive lobular carcinomas are described in the literature [2]. As compared to female breast cancer (fBC), mBC occurs later in life with higher stages and higher grades [3]. The rate of estrogen receptor (ER) positive mBC is higher than in females, while conversely, HER2 overexpression is a rare event [4].
Risk factors associated with mBC are gynecomastia, obesity, low physical activity, and alcohol use [5]. Moreover, genetic conditions like the Klinefelter syndrome (XXY) or BRCA mutations strongly increase the risk for mBC [6, 7]. In contrast to fBC, BRCA2 mutations are more frequent than BRCA1 mutations, and male BRCA2 mutation carriers have a 6.5 % cumulative risk of developing breast cancer before the age of 70, which is 100-fold higher than the general male population [7].
While some studies have suggested that early stage mBC has a worse prognosis as compared to fBC [3], other reported that male sex is not associated with poor outcome [8]. Similar to fBC, stage, tumor size, and nodal involvement are important prognostic factors [9]. However, there are limited data on other prognostic biomarkers in mBC.
Tewes et al. recently reported on the detection of disseminated tumor cells (DTCs) from the bone marrow in male patients with early stage breast cancer [10]. DTCs are a surrogate biomarker of minimal residual disease, and in fBC, various reports including thousands of patients have shown a strong association between DTCs and poor outcome [11, 12]. The detection rate of DTCs in females with early stage breast cancer is 20–30 %. However, due to the low incidence, no data exist on the detection rate in mBC. In the small study presented by Tewes et al., DTCs were detected in three out of five patients [13], which seem relatively high as compared to fBC.
In the current study, we therefore aimed to determine the prevalence of DTCs in early stage mBC. Moreover, we investigated whether associations between the DTC status and clinicopathological parameters exist and analyzed the prognostic impact of DTCs in mBC.
Patients and methods
Study population
Male patients undergoing primary surgery for early stage breast cancer (T1–4, N0–2, M0) at the Department of Obstetrics and Gynecology at Tuebingen University Hospital, Germany, between January 2001 and April 2015 were eligible for this study. Patients who received (neoadjuvant) systemic therapy prior to bone marrow sampling as well as patients with recurrent or metastatic disease or a previous history of secondary malignancy were excluded. All patients provided written informed consent for BM aspiration. The analysis was approved by the ethics committee of the University of Tuebingen (reference number 560/2012R).
Detection of DTC
BM aspirates (10–20 ml per patient) were collected during primary surgery and processed within 24 h. Briefly, mononuclear cells were isolated by density centrifugation (Ficoll, 1.077 g/ml, Biochrom, Berlin, Germany), spun down onto a glass slide (cytocentrifuge, Hettich, Tuttlingen, Germany), and fixed in 4 % formalin. The presence of DTCs (DTC status) was determined by immunostaining using the DAKO Autostainer (Dako, Glostrup, Denmark), the mouse monoclonal antibody A45-B/B3 directed against pancytokeratin (Micromet, Munich, Germany), and the DAKO-APAA detection kit (Dako, Glostrup, Denmark). Two slides (1 × 106 cells, each) per patient were evaluated, in accordance with consensus recommendations for standardized tumor cell detection [14, 15]. An additional slide was stained with an unspecific isotype-matched antibody. Moreover, each batch of samples was analyzed together with leukocytes from healthy volunteers as negative controls and the human breast cancer cell lines MCF-7 and SKBR-3 as positive controls. To assess the specificity of our method for DTC detection, we analyzed BM samples from 100 patients without evidence of malignant disease, of whom one was DTC positive [16].
Statistical analysis
Associations between categorical variables (DTC status and patient characteristics) were analyzed using Fisher’s exact test. To determine survival, times from BM aspiration to any recurrence of disease (disease-free survival, DFS) and death of any cause (overall survival, OS) were investigated separately. If no event occurred, data were censored at last follow-up. The influence of DTC status on survival was determined in a univariate analysis using the log-rank test. All statistical tests were performed using PASW Statistics 22 (SPSS Inc., Chicago, IL, USA), and all reported p values are two-sided with significance level set to P < 0.05.
Results
Patient characteristics
24 male patients with early stage breast cancer (mean age: 64 years, range 40–82 years) were included into the analysis. Patient characteristics are shown in detail in Table 1. All patients except for one had invasive ductal carcinoma (96 %), and tumors were mostly grade 2 (67 %). The majority was ER positive (96 %), PR positive (79 %) and HER2 negative (96 %).
DTC studies
As displayed in Table 1, DTCs were detected in four out of 24 patients (17 %). There was no significant association between the DTC status and any other clinicopathological parameter.
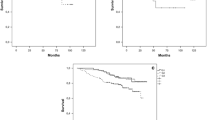
Survival analysis
As shown in Table 2, median follow-up for DFS was 24.89 months and for OS 33.87 months, respectively. Median DFS was 54 months with a 95 % confidence interval from 0 to 109 months. The median OS was not reached. A significant impact of the DTC status on DFS or OS could not be observed.
Discussion
We herein report on the prevalence of DTCs in male patients with early stage breast cancer and found that the detection rate is comparable to that observed in females. Only one small case series, presented by Tewes et al., has addressed this question earlier [13]. In that study, three out of five early stage patients with mBC were DTC positive (60 %). This high DTC detection rate will most notably be explained by chance and the small sample size. However, two other reasons might explain for it. On the one hand, patients were at relatively high tumor stages; tumor size and nodal status had been shown to correlate with the DTC detection rate in fBC [11]. On the other hand, Tewes et al. analyzed eight million mononuclear cells per patients instead of the recommended two million cells [13, 14]. Additionally, one patient had received neoadjuvant systemic treatment before bone marrow sampling, which was shown to interact with the DTC status [17]. Here, we only included treatment naïve patients into the analysis.
We found no significant association between the DTC status and clinicopathological variables. However, our dataset is also limited by its small sample size. Therefore, we cannot rule out that similar correlations as observed in fBC might exist, e.g., the higher DTC detection rate in PR-negative, HER2-positive patients with larger tumors and lymph node involvement [11, 12].
In female patients with early stage breast cancer, the DTC status has a strong and independent prognostic value [11, 12]. However, we could not confirm a significant impact of DTC detection on DFS or OS in male patients. Again, the most notably explanation is the small number of events and the short follow-up of the current analysis. Moreover, adjuvant systemic treatment was shown to eliminate DTCs and might therefore interact with the prognostic information of the DTC status [18, 19]. Earlier studies in fBC have shown that bone marrow sampling during or after adjuvant therapy might help to monitor treatment efficacy and to identify patients that could benefit from additional adjuvant treatment [16].
Due to the invasive character of bone marrow sampling, recent studies have focused on the detection of circulating tumor cells (CTCs) from the peripheral blood [20, 21]. Especially for serial analyses within translational research programs of prospective clinical trials, repeated venous blood sampling is more feasible than bone marrow sampling. However, it is not clear whether DTC detection is associated with CTC detection, as data on this issue are inconclusive among the literature [22–26]. Although CTC detection was shown to predict survival in female patients with early stage breast cancer, low detection rates in the non-metastatic setting make the use of this technology challenging [21, 27]. To the best of our knowledge, the analysis by Tewes et al. is the only published dataset of CTC detection in early stage mBC [13]. The authors found CTCs in one out of five patients, but the small sample size permits to draw conclusions on their prevalence or prognostic value in males.
Next to the prognostic impact of DTC detection, their characterization might reveal biomarkers that are predictive of treatment efficacy. For example, the HER2 status of DTCs might indicate patients that benefit from HER2-targeted treatment [28]. A prospective trial is currently investigating the efficacy of trastuzumab in females with early stage HER2-negative breast cancer but HER2-positive DTCs (NCT01779050). It is unlikely that such questions are to be answered in clinical trials of mBC patients. However, as therapy recommendations for mBC usually derive from lessons learned in females, the clinical implementation of DTC detection and/or characterization in women may also help improve treatment of men.
Conclusion
In conclusion, DTCs are detectable in male patients with early stage breast cancer, and their detection rate is comparable to that in women. Due to the small sample size of our analysis, no associations between DTCs and clinicopathological features or prognosis could be revealed. Although it is unlikely that clinical implementations of DTCs will be prospectively addressed in mBC, their detection in male patients emphasizes the transmission of future clinical applications from women to men.
References
Siegel RL, Miller KD (2015) Jemal A (2015) Cancer statistics. CA Cancer J Clin 65(1):5–29
Tawil AN, Boulos FI, Chakhachiro ZI, Otrock ZK, Kandaharian L, El Saghir NS, Abi Saad GS (2012) Clinicopathologic and immunohistochemical characteristics of male breast cancer: a single center experience. Breast J 18(1):65–68
Hossain AM, Bobba RK, Kardinal CG, Freter C (2012) Outcomes of male breast cancer in the United States: a SEER database analysis from 1973 to 2008. J Clin Oncol 30:suppl; abstr 1586
Korde LA, Zujewski JA, Kamin L, Giordano S, Domchek S, Anderson WF, Bartlett JM, Gelmon K, Nahleh Z, Bergh J, Cutuli B, Pruneri G, McCaskill-Stevens W, Gralow J, Hortobagyi G, Cardoso F (2010) Multidisciplinary meeting on male breast cancer: summary and research recommendations. J Clin Oncol 28(12):2114–2122
Jain S, Gradishar WJ (2014) Male breast cancer. In: Harris JR, Lippman ME, Morrow M, Osborne CK (eds) Diseases of the breast, 5th edn. Wolters Kluwer, Philadelphia, pp 819–825
Brinton LA, Carreon JD, Gierach GL, McGlynn KA, Gridley G (2010) Etiologic factors for male breast cancer in the U.S. Veterans Affairs medical care system database. Breast Cancer Res Treat 119(1):185–192
Ottini L, Silvestri V, Rizzolo P, Falchetti M, Zanna I, Saieva C, Masala G, Bianchi S, Manoukian S, Barile M, Peterlongo P, Varesco L, Tommasi S, Russo A, Giannini G, Cortesi L, Viel A, Montagna M, Radice P, Palli D (2012) Clinical and pathologic characteristics of BRCA-positive and BRCA-negative male breast cancer patients: results from a collaborative multicenter study in Italy. Breast Cancer Res Treat 134(1):411–418
Kwong A, Visram H, Graham N, Balchin K, Petrcich W, Dent S (2012) Treatment outcomes for early stage male breast cancer: a single centre retrospective case-control study. In: San Antonio breast cancer symposium, abstr P3-11-03
Gnerlich JL, Deshpande AD, Jeffe DB, Seelam S, Kimbuende E, Margenthaler JA (2011) Poorer survival outcomes for male breast cancer compared with female breast cancer may be attributable to in-stage migration. Ann Surg Oncol 18(7):1837–1844
Tewes M, Kasimir-Bauer S, Welt A, Schuler M, Kimmig R, Aktas B (2015) Detection of disseminated tumor cells in bone marrow and circulating tumor cells in blood of patients with early-stage male breast cancer. J Cancer Res Clin Oncol 141(1):87–92
Hartkopf AD, Taran FA, Wallwiener M, Hahn M, Becker S, Solomayer EF, Brucker SY, Fehm TN, Wallwiener D (2014) Prognostic relevance of disseminated tumour cells from the bone marrow of early stage breast cancer patients—results from a large single-centre analysis. Eur J Cancer 50(15):2550–2559
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Pierga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundt G, Strobl B, Fehm T, Wong GY, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353(8):793–802
Tewes M, Aktas B, Welt A, Mueller S, Hauch S, Kimmig R, Kasimir-Bauer S (2009) Molecular profiling and predictive value of circulating tumor cells in patients with metastatic breast cancer: an option for monitoring response to breast cancer related therapies. Breast Cancer Res Treat 115(3):581–590
Fehm T, Braun S, Muller V, Janni W, Gebauer G, Marth C, Schindlbeck C, Wallwiener D, Borgen E, Naume B, Pantel K, Solomayer E (2006) A concept for the standardized detection of disseminated tumor cells in bone marrow from patients with primary breast cancer and its clinical implementation. Cancer 107(5):885–892
Borgen E, Naume B, Nesland JM, Kvalheim G, Beiske K, Fodstad O, Diel I, Solomayer EF, Theocharous P, Coombes RC, Smith BM, Wunder E, Marolleau JP, Garcia J, Pantel K (1999) Standardization of the immunocytochemical detection of cancer cells in BM and blood: I. establishment of objective criteria for the evaluation of immunostained cells. Cytotherapy 1(5):377–388
Janni W, Vogl FD, Wiedswang G, Synnestvedt M, Fehm T, Juckstock J, Borgen E, Rack B, Braun S, Sommer H, Solomayer E, Pantel K, Nesland J, Friese K, Naume B (2011) Persistence of disseminated tumor cells in the bone marrow of breast cancer patients predicts increased risk for relapse—a European pooled analysis. Clin Cancer Res 17(9):2967–2976
Hartkopf AD, Taran FA, Wallwiener M, Hagenbeck C, Melcher C, Krawczyk N, Hahn M, Wallwiener D, Fehm T (2013) The presence and prognostic impact of apoptotic and nonapoptotic disseminated tumor cells in the bone marrow of primary breast cancer patients after neoadjuvant chemotherapy. Breast Cancer Res 15(5):R94
Gruber I, Fehm T, Taran FA, Wallwiener M, Hahn M, Wallwiener D, Krawzyck N, Hoffmann J, Hartkopf AD (2014) Disseminated tumor cells as a monitoring tool for adjuvant therapy in patients with primary breast cancer. Breast Cancer Res Treat 144(3):531–538
Naume B, Synnestvedt M, Falk RS, Wiedswang G, Weyde K, Risberg T, Kersten C, Mjaaland I, Vindi L, Sommer HH, Saetersdal AB, Rypdal MC, Bendigtsen Schirmer C, Wist EA, Borgen E (2014) Clinical outcome with correlation to disseminated tumor cell (DTC) status after DTC-guided secondary adjuvant treatment with docetaxel in early breast cancer. J Clin Oncol 32(34):3848–3857
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351(8):781–791
Rack B, Schindlbeck C, Juckstock J, Andergassen U, Hepp P, Zwingers T, Friedl TW, Lorenz R, Tesch H, Fasching PA, Fehm T, Schneeweiss A, Lichtenegger W, Beckmann MW, Friese K, Pantel K, Janni W, Group SS (2014) Circulating tumor cells predict survival in early average-to-high risk breast cancer patients. J Natl Cancer Inst 106(5):1–11
Krishnamurthy S, Cristofanilli M, Singh B, Reuben J, Gao H, Cohen EN, Andreopoulou E, Hall CS, Lodhi A, Jackson S, Lucci A (2010) Detection of minimal residual disease in blood and bone marrow in early stage breast cancer. Cancer 116(14):3330–3337
Molloy TJ, Bosma AJ, Baumbusch LO, Synnestvedt M, Borgen E, Russnes HG, Schlichting E, Veer LJ, Naume B (2011) The prognostic significance of tumour cell detection in the peripheral blood versus the bone marrow in 733 early-stage breast cancer patients. Breast Cancer Res 13(3):R61
Benoy IH, Elst H, Philips M, Wuyts H, Van Dam P, Scharpe S, Van Marck E, Vermeulen PB, Dirix LY (2006) Real-time RT-PCR detection of disseminated tumour cells in bone marrow has superior prognostic significance in comparison with circulating tumour cells in patients with breast cancer. Br J Cancer 94(5):672–680
Wiedswang G, Borgen E, Schirmer C, Karesen R, Kvalheim G, Nesland JM, Naume B (2006) Comparison of the clinical significance of occult tumor cells in blood and bone marrow in breast cancer. Int J Cancer 118(8):2013–2019
Hartkopf AD, Wallwiener M, Hahn M, Fehm TN, Brucker SY, Taran FA (2015) Simultaneous detection of disseminated and circulating tumor cells in primary breast cancer patients. Cancer Res Treat. doi:10.4143/crt.2014.287 (Epub ahead of print)
Lucci A, Hall CS, Lodhi AK, Bhattacharyya A, Anderson AE, Xiao L, Bedrosian I, Kuerer HM, Krishnamurthy S (2012) Circulating tumour cells in non-metastatic breast cancer: a prospective study. Lancet Oncol 13(7):688–695
Hartkopf AD, Banys M, Meier-Stiegen F, Hahn M, Rohm C, Hoffmann J, Helms G, Taran FA, Wallwiener M, Walter C, Neubauer H, Wallwiener D, Fehm T (2013) The HER2 status of disseminated tumor cells in the bone marrow of early breast cancer patients is independent from primary tumor and predicts higher risk of relapse. Breast Cancer Res Treat 138(2):509–517
Acknowledgments
We are grateful to Silke Duerr-Störzer, Ingrid Teufel, Sabine Hofmeister, Angelika Amman, and Brigitte Neth for excellent technical assistance.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hartkopf, A.D., Taran, FA., Walter, C.B. et al. Detection and prevalence of disseminated tumor cells from the bone marrow of early stage male breast cancer patients. Breast Cancer Res Treat 152, 51–55 (2015). https://doi.org/10.1007/s10549-015-3440-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3440-1