Abstract
The detection of circulating tumor cells (CTCs) in the peripheral blood of metastatic breast cancer (MBC) patients is an independent marker of prognosis. This large prospective multicenter study aimed to assess the impact of CTCs on overall survival (OS) and progression free survival (PFS) in patients with predefined molecular subgroups of MBC. To this end, 468 MBC patients were divided into three subgroups based on immunohistochemical staining of the primary tumor: (1) hormone receptor-positive/HER2-negative (HorR+/HER2−), (2) HER2-positive (HER2+), and (3) HorR-negative/HER2-negative (HorR−/HER2−) patients. CTC status (<5 CTCs/7.5 ml blood (CTC-negative) vs. ≥5 CTCs/7.5 ml blood (CTC-positive)) was determined using the CellCearch® system before patients started a new line of therapy. At baseline, 205 (42 %) patients were CTC-positive. On multivariate analysis, CTC-positivity was an independent prognostic factor for shorter PFS and OS. In HorR+/HER2− patients, median PFS [95 % CI] of CTC-negative versus CTC-positive patients was 8.60 [5.93–11.27] versus 4.33 [3.29–5.38] months (p < 0.001), in HER2+ patients 7.60 [5.40–9.79] versus 6.60 [4.20–9.00] months (p = 0.477) and in HorR−/HER2− patients 5.83 [5.09–6.78] versus 3.05 [1.81–4.29] months (p < 0.001), respectively. Median OS [95 % CI] of CTC-negative versus CTC-positive patients was as follows: not reached by either in the HorR+/HER2− subgroup (p < 0.001), not reached versus 18.07 [11.10–25.05] months (p = 0.001) in the HER2+ subgroup, and not reached versus 8.57 [4.07–13.07] months in the HorR−/HER2− subgroup (p = 0.001). In conclusion, our results strongly confirm the independent prognostic value of CTC enumeration in MBC patients. In contrast to recent reports, there was no association between primary tumor-based molecular subgroups and the impact of CTC status on OS. Hence, CTC status may help to identify patients who require aggressive therapy, especially among those with triple-negative MBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastatic breast cancer (MBC) remains an incurable disease. However, women with MBC represent a heterogeneous group with respect to their life expectancy and response to therapy. Better prognostic and predictive markers are needed to prevent patients from receiving unnecessary and/or ineffective treatment but experiencing the treatment-related side effects. Circulating tumor cells (CTCs) in the peripheral blood of breast cancer patients are attractive candidates in this context. Their detection, characterization, and clinical role as predictive and prognostic markers of treatment response and survival are currently the subject of intensive research [1].
Tumor cell spread into the blood circulation plays a key role during cancer progression. In recent years, highly sensitive methods have been developed to detect single CTCs. One such method is utilized by the CellSearch® system (Veridex, LLC, Warren, NJ, USA), a device approved by the FDA in 2004 for the detection of CTCs in the peripheral blood of patients with MBC. The number of CTCs detected with CellSearch® has been shown to be an independent prognostic marker of MBC [2–9]. Moreover, a substantial decrease in CTC count is an early marker of individual response to treatment and thus CTC enumeration provides an easy-to-perform alternative method to monitor therapy [10, 11].
Recently, Giuliano et al. [6] suggested that targeted therapy directed against the human epidermal growth factor receptor 2 (HER2) might improve outcome in MBC patients with high levels of CTCs. Another study, however, stated that CTCs had less prognostic value in a subgroup of patients with HER2-positive (HER2+) MBC, possibly due to selective effectiveness of HER2 directed therapy against CTCs [7]. Accordingly, Pierga et al. [8] reported that CTC levels appeared to decrease more markedly in patients who received first-line chemotherapy plus targeted therapy (bevacizumab or trastuzumab). The present large multicenter study was, therefore, conducted to assess the prognostic impact of CTCs in predefined subgroups of MBC patients as determined by immunohistochemical staining of the primary tumor.
Patients and methods
Study design and population
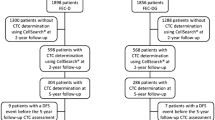
This prospective study was performed at nine German university breast cancer centers. In total, 486 women with progressive MBC starting a new line of systemic therapy between 12/2007 and 06/2011 were included in the analysis. CTC enumeration was carried out at baseline, i.e., before initiation of the new therapy, using the CellSearch® system (Veridex, LLC, Warren, NJ, USA). Other inclusion criteria were radiologically measurable or clinically evaluable metastatic disease and written informed consent. Response to treatment was determined according to the Response Evaluation Criteria in Solid Tumors (RECIST) criteria [12]. Patients with malignancies other than breast cancer were excluded from this study. The analysis was approved by the local ethics committees (reference number S-295/2009, Heidelberg).
Patient subgroups by primary tumor receptor status
Patients were divided into three subgroups according to their primary tumor receptor status: (1) positive for estrogen and/or progesterone (hormone receptor-positive, HorR+) and negative for HER2 (HER2−), (2) HER2+, or (3) HorR−/HER2− (triple negative). Details of the primary tumor’s HorR and HER2 status were extracted from the patient records. At all participating centers, HER2 status was determined using the HercepTest™ (Dako, Glostrup, Denmark) and/or the Pathvysion® Kit (Vysis, Downers Grove, IL, USA). All pathology laboratories had participated in round robin tests and were certified for HER2 testing. Hence there was no central review of primary tumor HER2 status. The cut-off level for HER2 positivity was based on the guideline recommendations published by the American Society of Clinical Oncology and College of American Pathologists [13]. HorR+ was defined as ER and/or PgR positivity of the primary tumor according to local pathology standards.
CTC studies
Enrichment and enumeration of CTCs using the CellSearch® technology was essentially performed as described elsewhere [14]. Briefly, samples of 7.5 ml of peripheral blood were drawn into CellSave tubes (Veridex LLC, Warren, NJ, USA), maintained at room temperature, and processed within 72 h. Epithelial cells were immunomagnetically enriched using anti-EpCAM-coated ferrofluid. EpCAM-positive cells were labeled with the nuclear dye 4′,6-diamidino-2-phenylindole (DAPI) and monoclonal antibodies specific for the leukocyte common antigen C45. CD45-negative, cytokeratin-positive cells with an intact nucleus were defined as CTCs and were enumerated by trained operators. A blood sample was considered CTC-positive (CTC+) if it contained ≥5 CTCs/7.5 ml blood, as published previously [2].
Statistical analysis
Chi squared and Fisher’s exact tests were used to determine differences in CTC status (<5 CTCs vs. ≥5 CTCs/7.5 ml blood) among patient subgroups. For univariate analysis, survival with respect to CTC status was calculated by the Kaplan–Meier method and curves were compared using the log-rank test. Multivariate Cox proportional hazard regression analysis was performed to assess the independent prognostic value of CTC status in comparison with other prognostic factors, including age (<55 vs. ≥55 years), number of metastatic sites (one vs. multiple sites), site of metastasis (bone metastasis vs. visceral metastasis vs. both sites), line of therapy (first-line vs. second-line vs. third or further lines), and receptor status (HorR+/HER2− vs. HER2+ vs. HorR−/HER2−). Variables were entered stepwise backward and a significance level of 0.1 was used to exclude a variable from the model. The CTC status was not forced to be included in the model. The effect of each variable was evaluated using the Wald test and described by the hazard ratio (HR) and the corresponding 95 % confidence interval (CI). PFS was calculated from the date of CTC blood sampling to the date of progressive disease as determined by RECIST criteria. Overall survival (OS) was defined as the time from the date of CTC blood draw to the date of death. To determine PFS and OS, patients without disease progression and living patients, respectively, were censored at last follow-up. All statistical tests were two-sided with significance levels set at p < 0.05 and were carried out using PASW Statistics 20 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
A total of 486 patients with a median age of 55 (range: 23–91) years were eligible for this study. Further details of patient demographics, tumor characteristics, and CTC status are presented in Table 1. Of all 486 patients, 251 (52 %) were HorR+/HER2−, 117 (24 %) were HER2+, and 88 (18 %) were HorR−/HER2−; 347 (71 %) had multiple metastatic sites, 83 (17 %) had bone metastases only, 175 (36 %) had visceral metastases only, and 228 (47 %) had both bone and visceral metastases; 183 (38 %) received first-line, 115 (24 %) second-line, and 188 (39 %) third- or further line treatment for MBC.
The number of detected CTCs ranged from 0 to 6.380 CTCs/7.5 ml blood (median: 2 CTCs/7.5 ml blood). Out of 486 patients, 205 (42 %) were CTC+ with counts ≥5 CTCs/7.5 ml blood. CTC-positivity was significantly more frequent in estrogen receptor-positive (ER+) than in ER− patients (p = 0.030) and in patients with both bone and visceral metastases compared with those with either bone or visceral metastases (p < 0.001). The CTC status did not differ significantly among subtypes of MBC (p = 0.116). CTC status was positive in 116/251 (46 %) HorR+/HER2− patients, 43/117 (37 %) HER2+ patients, and 32/88 (36 %) HorR −/HER2− patients.
Univariate and multivariate analyses of survival in CTC− versus CTC+ MBC patients
Median follow-up was 10.10 months for PFS and 11.13 months for OS. Follow-up data for PFS were not available for 41 patients. On univariate analysis, CTC status had a significant prognostic impact on PFS and OS (Fig. 1a). Median PFS was significantly lower in CTC+ patients [4.77 (95 % CI: 3.92–5.61) months] than in CTC− patients [7.60 (95 % CI: 5.93–9.27) months, p < 0.001]. Median OS was not reached in CTC− patients and was 18.01 months in CTC+ patients (p < 0.001). The independent prognostic factors of PFS as identified by multivariate analysis (Table 2) were CTC status, site of metastasis, line of therapy, and receptor status of the primary tumor. Independent prognostic factors of OS were CTC status, line of therapy, and receptor status of the primary tumor. The HRs for progression and death in patients with ≥5 CTCs versus <5 CTCs were 1.82 (95 % CI: 1.41–2.34) and 4.79 (95 % CI: 2.95–7.79), respectively (p < 0.001).
Kaplan–Meier plots of progression free (PFS) and overall (OS) survival according to CTC status and the primary tumor hormone receptor/HER2 status. a Median PFS of CTC− (<5 CTCs) patients was 7.60 (95 % CI: 5.93–9.27) versus 4.77 (95 % CI: 3.92–5.61) months in CTC+ (≥5 CTCs) patients (p < 0.001). Median OS was not reached in CTC− patients and was 18.01 months in CTC+ patients (p < 0.001). b Median PFS of HorR+/HER2− patients was 8.60 (95 % CI: 5.93–11.27) versus 4.33 (95 % CI: 3.29–5.38) months (p = 0.001). Median OS was not reached in either CTC− or CTC+ patients (p < 0.001). c Median PFS of HorR−/HER2− patients was 5.83 (5.09–6.56) versus 3.05 (1.81–4.29) months (p = 0.001). Median OS was not reached in CTC− patients and was 8.57 (95 % CI: 4.07–13.07) months in CTC+ patients (p < 0.001). d Median PFS of HER2+ patients was 7.60 (95 % CI: 5.40–9.79) versus 6.60 (95 % CI: 4.20–9.00) months (p = 0.477). Median OS was not reached in CTC− patients and was 18.07 (95 % CI: 11.10–25.05) months in CTC+ patients (p = 0.001)
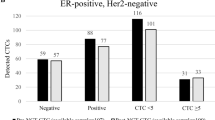
Survival analysis of CTC− versus CTC+ patients according to tumor subtypes
In the survival analysis of predefined subgroups, CTC status was a prognostic factor for PFS and OS in HorR+/HER2− and HorR−/HER2− patients. As illustrated in Fig. 1b, HorR+/HER2− patients had a median PFS of 8.60 (95 % CI: 5.93–11.27) months if CTC− versus 4.33 (95 % CI: 3.29–5.38) months if CTC+ (p = 0.001). OS was significantly decreased in CTC+ patients (p < 0.001), although median OS was not reached in either CTC− or CTC+ patients. In the subgroup of HorR−/HER2− patients (Fig. 1c), median PFS was 5.83 (5.09–6.78) months in CTC− versus 3.05 (1.81–4.29) months in CTC+ patients (p < 0.001). Median OS was not reached in CTC− patients and was 8.57 (95 % CI: 4.07–13.07) months in CTC+ patients (p = 0.001).
Although a significant predictor of OS in patients with a HER2+ primary tumor, CTC status had no demonstrable impact on PFS (Fig. 1d). Median PFS was 7.60 (95 % CI: 5.40–9.79) months in CTC− versus 6.60 (95 % CI: 4.20–9.00) months in CTC+ patients (p = 0.477). Median OS was not reached in CTC− patients and was 18.07 (95 % CI: 11.10–25.05) months in CTC+ patients (p = 0.001).
Survival analysis of CTC− versus CTC+ patients with HER2+ primary tumor according to previous treatment with trastuzumab
CTC status also had no impact on PFS in HER2+ patients who had or had not been treated with trastuzumab before CTC enumeration (Fig. 2). Median PFS of HER2+ patients without previous trastuzumab treatment (Fig. 2a) was 8.57 (95 % CI: 6.46–10.68) if they were CTC− versus 6.66 (95 % CI: 5.63–7.69) months if they were CTC+ (p = 0.378). Median PFS of HER2+ patients who had been pretreated with trastuzumab (Fig. 2b) was 4.85 (95 % CI: 3.55–6.15) if they were CTC− versus 4.69 (95 % CI: 0.13–9.25) months if they were CTC+ (p = 0.706). The CTC status of HER2+ patients without previous trastuzumab treatment was, however, prognostic of OS (Fig. 2a). Median OS was not reached in CTC− patients and was 18.07 (95 % CI: 11.97-24.16) months in CTC+ patients (p = 0.002). In contrast, CTC status had no impact on OS in HER2+ patients who had previously received trastuzumab treatment (Fig. 2b). Median OS was not reached in either CTC− or CTC+ patients (p = 0.426).
Kaplan–Meier plots of progression free (PFS) and overall survival (OS) of HER2+ MBC patients according to CTC status and trastuzumab pretreatment. a Median PFS of HER2+ patients who had not been treated with trastuzumab was 8.57 (95 % CI: 6.46–10.68) if CTC− versus 6.66 (95 % CI: 5.63–7.69) months if CTC+ (p = 0.378). Median OS was not reached in CTC− patients and was 18.07 (95 % CI: 11.97–24.16) months in CTC+ patients (p = 0.002). b Median PFS of HER2+ patients who had been treated with trastuzumab was 4.85 (95 % CI: 3.55–6.15) if CTC− versus 4.69 (95 % CI: 0.13–9.25) months if CTC+ (p = 0.706). Median OS was not reached in either CTC− or CTC+ patients (p = 0.426)
Discussion
This prospective study was conducted to determine the influence of CTCs on prognosis in predefined subgroups of progressive MBC. To this end, we divided a large cohort of patients into subgroups based on immunohistochemical staining of the primary tumor and compared survival in CTC− (<5 CTCs/7.5 ml peripheral blood) versus CTC+ (≥5 CTCs/7.5 ml peripheral blood) patients.
Our results confirm the strong and independent impact on PFS and OS of ≥5 CTCs/7.5 ml blood, as determined by the CellSearch® system. CTC count was a prognostic marker for OS in all predefined subgroups but failed to predict PFS in the subgroup of HER2+ patients. Detection of CTCs also had an impact on OS in HER2+ patients. This is in contrast to recent findings by Giordano et al. [7], who found that the detection of CTCs has no impact on outcome in MBC patients with HER2+ primary tumors. As most patients with HER2+ breast cancer received HER2 targeting therapy, the authors concluded that this highly effective treatment eliminates CTCs with HER2 amplification, thus impairing the prognostic value of CTCs in HER2+ patients. Accordingly, other studies demonstrated a marked decrease in CTC count at follow-up if MBC patients had received biological therapies such as trastuzumab or bevacizumab [8, 15]. Georgoulias et al. [16] showed that trastuzumab eliminates chemotherapy-resistant CTCs and reduces the risk of disease recurrence in early breast cancer patients. In our study, however, the number of patients treated with trastuzumab was considerably low. Moreover, CTC detection was a predictor of OS only in the subgroup of initially HER2+ patients who had not been treated with trastuzumab. Conversely, CTC detection had no impact on survival if patients had already received trastuzumab treatment. This supports the suggestion that HER2 directed therapy reduces the prognostic value of CTC enumeration. However, these observations should be interpreted with caution due to the small number of patients in our study who had already received trastuzumab therapy. Moreover, there was no association between trastuzumab pretreatment and CTC-positivity.
In contrast to our study in the study by Giordano et al. [7] most patients received first-line therapy. Giuliano et al. [6] recently demonstrated that the CTC status before initiation of HER2 directed first-line therapy is not associated with survival. Additionally, HER2 directed treatment combined with chemotherapy reduced the number of CTCs in all patients with a high baseline CTC count. As the gold standard to decide whether a patient is likely to benefit from HER2 targeted drugs, predictive determination of the HER2 status is generally performed on primary tumor tissue [13]. However, the phenotype of breast cancer, including the HER2 status, may change during disease progression [17, 18]. Various studies have shown that the HER2 status of the primary tumor does not necessarily represent that of peripheral metastasis, micrometastatic spread, or CTCs [19–27]. Moreover, breast cancer treatment will exert selective pressure on different tumor cell clones, resulting in cumulative differences between the primary tumor and advanced disease. The fact that most of our patients had already received multiple lines of therapy may also have contributed to our finding that the prognostic value of CTCs was independent of primary tumor phenotype.
Interestingly, HorR−/HER2− (i.e., triple-negative) patients had a relatively good prognosis if no CTCs were detected. Conversely, OS was markedly decreased if the CTC status was positive. In this subgroup, in particular, the determination of CTC status may, therefore, be helpful in identifying patients who need more aggressive treatment regimes. As early studies demonstrated that bevacizumab has the potential to eradicate CTCs, the inclusion of this targeted drug in treatment regimes for CTCs positive triple-negative patients promises to be a valuable option.
It is reasonable to assume that therapy directed specifically at CTCs is more effective if the targets are features of the CTCs rather than features of the primary tumor. Meng et al. [17] determined the HER2 status of CTCs and treated four patients with initially HER2− breast cancer but HER2+ CTCs with a trastuzumab-containing regimen; one patient had a rapid and complete remission whereas two patients showed a partial response. Thus, the enumeration and characterization of CTCs might serve as a “liquid real time biopsy” of metastatic disease which would allow clinicians to noninvasively predict and monitor response to treatment [28]. Moreover, the possibility to follow phenotypic changes in breast cancer phenotype in real time would provide a excellent opportunity to gain insight into the principles underlying disease progression.
Further prospective trials should be conducted to investigate the clinical value of CTC enumeration and its relationship to phenotypic subtypes. Currently, the prospective SWOG S0500 trial is investigating whether or not therapy for MBC should be changed if CTCs are still elevated at first follow-up (www.clinicaltrials.gov/ct2/show/NCT00382018). Next to the detection of CTCs, their characterization could provide valuable additional predictive and prognostic information. As the clinical value of targeting CTCs remains unclear, the German DETECT study group aims to answer the question as to whether patients with a HER2− primary tumor but HER2+ CTCs might benefit from lapatinib treatment (www.detect-studien.de).
Conclusion
In conclusion, this large prospective multicenter study confirms the strong and independent impact of CTCs on prognosis in patients with progressive MBC. Molecular subtypes, including HER2-positive and triple-negative tumors, did not influence the prognostic value of CTC enumeration on OS. Interestingly, HorR−/HER2− (i.e., triple-negative) patients had a comparatively good prognosis if they were CTC-negative. Especially in this subgroup, evaluation of the CTC status might, therefore, help to decide whether patients require more or less aggressive therapy. In the HER2+ positive subgroup, pretreatment with trastuzumab seems to impair the prognostic value of CTC enumeration. This supports the suggested role of targeted therapies to effectively hit CTCs.
Abbreviations
- CI:
-
Confidence interval
- CTC(s):
-
Circulating tumor cell(s)
- CTC−:
-
CTC-negative
- CTC+:
-
CTC-positive
- EpCam:
-
Epithelial cell adhesion molecule
- ER:
-
Estrogen receptor
- FDA:
-
Food and drug administration (USA)
- HER2:
-
Human epidermal growth factor receptor 2
- HorR:
-
Hormone receptor
- MBC:
-
Metastatic breast cancer
- OS:
-
Overall survival
- PFS:
-
Progression free survival
- PgR:
-
Progesterone receptor
- RECIST:
-
Response evaluation criteria in solid tumors
References
Fehm T, Muller V, Alix-Panabieres C, Pantel K (2008) Micrometastatic spread in breast cancer: detection, molecular characterization and clinical relevance. Breast Cancer Res 10(Suppl 1):S1. doi:10.1186/bcr1869
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351(8):781–791
Maestro LM, Sastre J, Rafael SB, Veganzones SB, Vidaurreta M, Martin M, Olivier C, De La Orden VB, Garcia-Saenz JA, Alfonso R, Arroyo M, Diaz-Rubio E (2009) Circulating tumor cells in solid tumor in metastatic and localized stages. Anticancer Res 29(11):4839–4843
Liu MC, Shields PG, Warren RD, Cohen P, Wilkinson M, Ottaviano YL, Rao SB, Eng-Wong J, Seillier-Moiseiwitsch F, Noone AM, Isaacs C (2009) Circulating tumor cells: a useful predictor of treatment efficacy in metastatic breast cancer. J Clin Oncol 27(31):5153–5159. doi:10.1200/JCO.2008.20.6664
Nakamura S, Yagata H, Ohno S, Yamaguchi H, Iwata H, Tsunoda N, Ito Y, Tokudome N, Toi M, Kuroi K, Suzuki E (2010) Multi-center study evaluating circulating tumor cells as a surrogate for response to treatment and overall survival in metastatic breast cancer. Breast Cancer 17(3):199–204. doi:10.1007/s12282-009-0139-3
Giuliano M, Giordano A, Jackson S, Hess KR, De Giorgi U, Mego M, Handy BC, Ueno NT, Alvarez RH, De Laurentiis M, De Placido S, Valero V, Hortobagyi GN, Reuben JM, Cristofanilli M (2011) Circulating tumor cells as prognostic and predictive markers in metastatic breast cancer patients receiving first-line systemic treatment. Breast Cancer Res 13(3):R67. doi:10.1186/bcr2907
Giordano A, Giuliano M, De Laurentiis M, Arpino G, Jackson S, Handy BC, Ueno NT, Andreopoulou E, Alvarez RH, Valero V, De Placido S, Hortobagyi GN, Reuben JM, Cristofanilli M (2012) Circulating tumor cells in immunohistochemical subtypes of metastatic breast cancer: lack of prediction in HER2-positive disease treated with targeted therapy. Ann Oncol 23(5):1144–1150. doi:10.1093/annonc/mdr434
Pierga JY, Hajage D, Bachelot T, Delaloge S, Brain E, Campone M, Dieras V, Rolland E, Mignot L, Mathiot C, Bidard FC (2012) High independent prognostic and predictive value of circulating tumor cells compared with serum tumor markers in a large prospective trial in first-line chemotherapy for metastatic breast cancer patients. Ann Oncol 23(3):618–624. doi:10.1093/annonc/mdr263
Dawood S, Broglio K, Valero V, Reuben J, Handy B, Islam R, Jackson S, Hortobagyi GN, Fritsche H, Cristofanilli M (2008) Circulating tumor cells in metastatic breast cancer: from prognostic stratification to modification of the staging system? Cancer 113(9):2422–2430. doi:10.1002/cncr.23852
Hartkopf AD, Wagner P, Wallwiener D, Fehm T, Rothmund R (2011) Changing levels of circulating tumor cells in monitoring chemotherapy response in patients with metastatic breast cancer. Anticancer Res 31(3):979–984. doi:31/3/979
Hayes DF, Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Miller MC, Matera J, Allard WJ, Doyle GV, Terstappen LW (2006) Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin Cancer Res 12(14 Pt 1):4218–4224
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. doi:10.1016/j.ejca.2008.10.026
Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, McShane LM, Paik S, Pegram MD, Perez EA, Press MF, Rhodes A, Sturgeon C, Taube SE, Tubbs R, Vance GH, van de Vijver M, Wheeler TM, Hayes DF (2007) American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol 25(1):118–145. doi:10.1200/JCO.2006.09.2775
Riethdorf S, Fritsche H, Muller V, Rau T, Schindlbeck C, Rack B, Janni W, Coith C, Beck K, Janicke F, Jackson S, Gornet T, Cristofanilli M, Pantel K (2007) Detection of circulating tumor cells in peripheral blood of patients with metastatic breast cancer: a validation study of the cell search system. Clin Cancer Res 13(3):920–928
Bidard FC, Mathiot C, Degeorges A, Etienne-Grimaldi MC, Delva R, Pivot X, Veyret C, Bergougnoux L, de Cremoux P, Milano G, Pierga JY (2010) Clinical value of circulating endothelial cells and circulating tumor cells in metastatic breast cancer patients treated first line with bevacizumab and chemotherapy. Ann Oncol 21(9):1765–1771. doi:10.1093/annonc/mdq052
Georgoulias V, Bozionelou V, Agelaki S, Perraki M, Apostolaki S, Kallergi G, Kalbakis K, Xyrafas A, Mavroudis D (2012) Trastuzumab decreases the incidence of clinical relapses in patients with early breast cancer presenting chemotherapy-resistant CK-19mRNA-positive circulating tumor cells: results of a randomized phase II study. Ann Oncol 23(7):1744–1750. doi:10.1093/annonc/mds020
Meng S, Tripathy D, Shete S, Ashfaq R, Haley B, Perkins S, Beitsch P, Khan A, Euhus D, Osborne C, Frenkel E, Hoover S, Leitch M, Clifford E, Vitetta E, Morrison L, Herlyn D, Terstappen LW, Fleming T, Fehm T, Tucker T, Lane N, Wang J, Uhr J (2004) HER-2 gene amplification can be acquired as breast cancer progresses. Proc Natl Acad Sci USA 101(25):9393–9398. doi:10.1073/pnas.0402993101
Hartkopf AD, Banys M, Fehm T (2012) HER2-positive DTCs/CTCs in breast cancer. Recent Results Cancer Res 195:203–215. doi:10.1007/978-3-642-28160-0_19
Tanner M, Jarvinen P, Isola J (2001) Amplification of HER-2/neu and topoisomerase II alpha in primary and metastatic breast cancer. Cancer Res 61(14):5345–5348
Gancberg D, Di Leo A, Cardoso F, Rouas G, Pedrocchi M, Paesmans M, Verhest A, Bernard-Marty C, Piccart MJ, Larsimont D (2002) Comparison of HER-2 status between primary breast cancer and corresponding distant metastatic sites. Ann Oncol 13(7):1036–1043
Edgerton SM, Moore D 2nd, Merkel D, Thor AD (2003) erbB-2 (HER-2) and breast cancer progression. Appl Immunohistochem Mol Morphol 11(3):214–221
Pestrin M, Bessi S, Galardi F, Truglia M, Biggeri A, Biagioni C, Cappadona S, Biganzoli L, Giannini A, Di Leo A (2009) Correlation of HER2 status between primary tumors and corresponding circulating tumor cells in advanced breast cancer patients. Breast Cancer Res Treat 118(3):523–530. doi:10.1007/s10549-009-0461-7
Fehm T, Becker S, Duerr-Stoerzer S, Sotlar K, Mueller V, Wallwiener D, Lane N, Solomayer E, Uhr J (2007) Determination of HER2 status using both serum HER2 levels and circulating tumor cells in patients with recurrent breast cancer whose primary tumor was HER2 negative or of unknown HER2 status. Breast Cancer Res 9(5):R74. doi:10.1186/bcr1783
Tewes M, Aktas B, Welt A, Mueller S, Hauch S, Kimmig R, Kasimir-Bauer S (2009) Molecular profiling and predictive value of circulating tumor cells in patients with metastatic breast cancer: an option for monitoring response to breast cancer related therapies. Breast Cancer Res Treat 115(3):581–590. doi:10.1007/s10549-008-0143-x
Fehm T, Muller V, Aktas B, Janni W, Schneeweiss A, Stickeler E, Lattrich C, Lohberg CR, Solomayer E, Rack B, Riethdorf S, Klein C, Schindlbeck C, Brocker K, Kasimir-Bauer S, Wallwiener D, Pantel K (2010) HER2 status of circulating tumor cells in patients with metastatic breast cancer: a prospective, multicenter trial. Breast Cancer Res Treat 124(2):403–412. doi:10.1007/s10549-010-1163-x
Ignatiadis M, Rothe F, Chaboteaux C, Durbecq V, Rouas G, Criscitiello C, Metallo J, Kheddoumi N, Singhal SK, Michiels S, Veys I, Rossari J, Larsimont D, Carly B, Pestrin M, Bessi S, Buxant F, Liebens F, Piccart M, Sotiriou C (2011) HER2-positive circulating tumor cells in breast cancer. PLoS ONE 6(1):e15624. doi:10.1371/journal.pone.0015624
Meng S, Tripathy D, Shete S, Ashfaq R, Saboorian H, Haley B, Frenkel E, Euhus D, Leitch M, Osborne C, Clifford E, Perkins S, Beitsch P, Khan A, Morrison L, Herlyn D, Terstappen LW, Lane N, Wang J, Uhr J (2006) uPAR and HER-2 gene status in individual breast cancer cells from blood and tissues. Proc Natl Acad Sci USA 103(46):17361–17365. doi:10.1073/pnas.0608113103
Alix-Panabieres C, Pantel K (2012) Circulating tumor cells: liquid biopsy of cancer. Clin Chem. doi:10.1373/clinchem.2012.194258
Acknowledgments
We are grateful to the patients who participated in this study. We also wish to acknowledge the medical and nursing staff at the participating centers.
Conflict of interest
KP, BR and WJ has received funding from Veridex. The other authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Markus Wallwiener, Andreas Daniel Hartkopf, Andreas Schneeweiss, and Tanja Natascha Fehm are joint authors.
Rights and permissions
About this article
Cite this article
Wallwiener, M., Hartkopf, A.D., Baccelli, I. et al. The prognostic impact of circulating tumor cells in subtypes of metastatic breast cancer. Breast Cancer Res Treat 137, 503–510 (2013). https://doi.org/10.1007/s10549-012-2382-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2382-0