Abstract
During the past 50 years, breast cancer incidence has increased by 2–3 % annually. Despite many years of testing for estrogen receptors (ER), evidence is scarce on breast cancer incidence by ER status. The aim of this paper was to investigate the increase in breast cancer incidence by ER status. Data were obtained from the clinical database of the Danish Breast Cancer Cooperative Group which holds nationwide data on diagnosis, including pathology, treatment, and follow-up on primary breast cancers since 1977. All Danish women <80 years diagnosed with primary breast cancer 1996–2007 were identified in this prospective register based study. ER status was evaluated using immunohistochemical staining by standardized laboratory methods in the Danish Pathology Departments and reported to the database. From 1996 to 2007, breast cancer incidence increased overall with a tendency to level off after 2002. In all women a significant decrease was found in ER unknown tumors. However, in both pre- and postmenopausal women, significant increases were seen in incidence of ER+ tumors; though the increase levelled off for premenopausal women after 2002. In postmenopausal women, the incidence of ER− breast cancer decreased significantly throughout the period. In women <35 years, we found a minor non-significant increase in both ER+ and ER− tumors. ER unknown decreased in all women and was the most distinct in premenopausal women aged 35+. We found a significant increase in ER+ breast cancer incidence in postmenopausal women whereas the incidence in premenopausal women (aged 35+) levelled off after 2002.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most frequent malignant disease in Danish women. In 1996, 3,495 women were diagnosed with breast cancer. This number increased to 4,189 in 2007 just before national screening was introduced. Through the past 50 years, a 2–3 % annual increase in breast cancer incidence has been observed [1]. The hormone receptor status among the increasing number of breast cancers has not been described. Figure 1 shows age-standardized incidence and mortality rates (ASR) of breast cancer per 100,000 women in the last 65 years. The data were obtained from the Danish Cancer Registry (www.iarc.fr/NORDCAN). The breast cancer incidence increased until 2002 and thereafter levelled off. The mortality peaked in 1994 and has decreased ever since.
In the US, trends in breast cancer incidence rates show conflicting results [2–9]. Studies examining ER status conclude that the increase in incidence was primarily a result of an increase in ER positive (ER+) tumors [2–5]; however, this increase seems to decline over the last decade [6–8]. Use of hormone replacement therapy (HRT) has long been known to increase the risk of breast cancer [10]. The Women Health Initiative [11–13] and the British Million Women Study [14] found the risk especially pronounced to use of combined hormone therapy. It has been suggested that the widespread use of HRT and mammography screening contributed to the increase in breast cancer incidence and the observed plateau or decline in incidence may reflect a decrease in HRT use [12, 13, 15–18]. However, breast cancer incidence fluctuates over time, and known as well as unknown biologic risk factors may also influence the trends [1, 15, 19, 20]; therefore a single etiological explanation seems unlikely. In Denmark, the incidence has increased with a tendency to plateau [19, 21] while an overall reduction in the prescription of HRT after 2002 was registered [15, 22].
The aim of our study was to investigate breast cancer incidence in Denmark in relation to ER status using data from Danish Breast Cancer Group (DBCG). Our analysis was restricted to 1996–2007 to avoid the influence of the prevalence phase of the national mammography screening introduced after 2007.
Materials and methods
Pathology data
ER analyses have been performed in Denmark since 1977, and since 1994 IHC has been employed by all laboratories [23]. Internal control protocols for staining quality and additionally external quality control has been performed by NordiQ as a routine within all participating laboratories in the investigation period. Up to 2011 ER+ in Denmark was defined as positive nuclear staining of 10 % or more of the tumor cells using standardized IHC methods. Nuclear staining of less than 10 % was defined as ER− breast cancer. Presently, however, a cut-off of 1 % is used to match guidelines for adjuvant therapy.
Measures
Data derived from the DBCG which has performed clinical trials and issued national guidelines for treatment since 1977. Data have been collected prospectively on diagnosis, histopathology, and treatment (surgery, radiotherapy, and medical) for all newly diagnosed early stage breast cancer patients in Denmark. The database is nearly complete (95 %) [24]. Completion of data on receptor status and tumor histology was achieved by linking to The Danish Pathology Register and The Danish Cancer Registry using the unique personal identification number held by all inhabitants of Denmark. Women were defined as postmenopausal if they had no menstrual bleeding within one year. Women on HRT were classified as postmenopausal being 55 years or older.
We chose to investigate the breast cancer incidence from 1996 to 2007, and divided analysis as just before (1996–2002) and after (2003–2007) a major reduction in HRT prescriptions was registered in 2002 [15, 22] and to terminate the study before the National Mammography Screening Programme was implemented in 2008/2009.
Statistical analysis
The DBCG Data Centre undertook central review, querying and analysis of data. Associations between ER status (excluding unknowns) and time periods were analyzed by χ 2 test. Incidence rates were calculated on the observed number of breast cancer and the corresponding number of person years in the Danish female population (from Statistics Denmark) in the same age category and time period. Incidence rates were age standardized to the World Standard Population [ASR(W)]. The analysis of trends over time using joinpoint modeling were done with Joinpoint Regression Program 3.5 [25]. Joinpoint regression models with different lines connected at joinpoints were made for each combination of ER (negative, positive, and unknown) and age/menopausal status (<35 years, premenopausal 35+ years, postmenopausal). Models with 0, 1, and 2 number of joinpoints were investigated. The simplest joinpoint model that the data allowed was fitted. For details, see Ref. [25]. Estimated annual percentage rate change (APC) is the percentage change of the rate of the previous year, and is used to characterize the trends in rates over time. Other statistical analyses were done with the SAS 9.2 program package.
Results
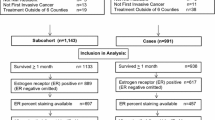
Between 1996 and 2007, 42,119 primary breast cancers were registered in the DBCG database in Danish women. Since ER status was unknown for 19 % of women aged ≥80 years, we excluded 4,575 women leaving 37,544 for further analyses of whom ER status was available for 35,195.
Figure 2 shows the number of primary breast cancers according to ER status in three categories; ER+, ER−, and ER unknown, and year of operation. The number of ER+ tumors increased from 1,854 to 2,628 in the years under investigation and the increase was significant from 1996 to 2002 and then stabilised, whereas the number of ER− tumors decreased significantly from 683 to 609 and ER unknown decreased significantly from 271 to 112 over the entire investigation period.
Table 1 describes the number and percentage of ER+, ER−, and ER unknown breast cancer tumors according to two time periods; 1996–2002 and 2003–2007, respectively. We selected these time periods due to investigations showing 65 % reduction in the prescription of HRT after 2002 [15, 22]. Among 37,544 women <80 years, 27,625 (73.5 %) had an ER+ breast cancer tumor, 7,570 (20.2 %) had an ER− tumor and for 2,349 (6.3 %) ER was unknown. The percentage of ER+ tumors increased with age/menopausal status (P < 0.0001). In all three groups, the percentage of ER+ tumors increased between the two time periods, but the increase was only significant in women aged 35+. More than two-thirds of premenopausal women aged 35+ and postmenopausal women had ER+ tumors (66.9/72.4 vs. 78.7/77.7 % in the latest time period). Young women <35 years differed from the overall pattern with the highest percentage of ER− tumors (41.5/40.3 %) and ER unknown (12.5/6.1 %). The percentage of patients with ER unknown decreased significantly in all women. The distribution of the ER remained significantly different between the time periods whether or not the ER unknowns were included. Subanalysis (not shown) for the oldest women, aged 70–79 years, showed that ER status did not vary between the time periods (P = 0.27) with 82.5 % ER+ tumors in 1996–2002 versus 83.5 % in 2003–2007.
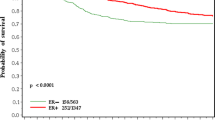
The age-standardized incidence rates [ASR(W)] per 100,000 woman-years for breast cancer by ER status are shown in Figs. 3, 4, and 5 representing women aged <35 years, premenopausal aged 35+, and postmenopausal women. In women aged <35 years, a non-significant annual incidence increase of 2.2 % (95 % CI = −0.4 to 4.8) for ER+ and 1.4 % (95 % CI = −2.8 to 5.7) for ER− were observed while a significant annual decrease of 10.3 % (95 % CI = −15.2 to −5.0) for ER unknown was found (Fig. 3) (N = 50 in 1996–2002 and N = 16 in 2003–2007; Table 1). In premenopausal women aged 35+ years, incidence rates increased significantly 10.4 % (95 % CI = 7.3–13.6) for ER+ until 2002 followed by a borderline significant annual decrease of 3.4 % (95 % CI = −6.6 to −0.1) (Fig. 4). A significant 4.5 % (95 % CI = −6.5 to −2.5) annual incidence decrease in ER− and a 13.3 % (95 % CI = −17.0 to −9.4) annual decrease for ER unknown was found. In the postmenopausal group, a significant 2.0 % (95 % CI = 1.1–2.8) annual incidence increase in ER+ and a significant 3.0 % (95 % CI = −4.3 to −1.7) annual decrease in ER− and a significant 7.9 % (95 % CI = −14.0 to −1.3) decrease in the ER unknown were found (Fig. 5).
Discussion
We found a non-significant increase in ER+ and ER− breast cancer in young women <35 years. A significant increase in ER+ breast cancer incidence was found in premenopausal aged 35+ until 2002 and thereafter levelled off and ER unknown decreased significantly. In postmenopausal women a significant increase in ER+ and a significant decrease in ER− were found. For young women <35 years and the oldest women between 70 and 79 years, the distribution of ER+ and ER− changed very little between 1996 and 2007.
Our finding of an increased incidence restricted to ER+ breast cancer tumors is in agreement with other studies [4, 8]. Well-known risk factors for breast cancer are mainly related to the female hormone production and can be described as either intrinsic or external exposures. The risk related to intrinsic hormonal production is measured by proxy variables such as: age of menarche, age at first full-term pregnancy, number of childbirths, age at menopause, and number of menstrual cycles [1, 20]. Examples of exogenous exposure are HRT, alcohol consumption, obesity, and environmental factors [1, 26, 27]. The intrinsic hormonal production reflects changes in hormone production in the lifespan of a fertile woman, where big changes have occurred due to women working outside the home, being educated and as a consequence giving birth later. The exogenous exposures are most often referred to as lifestyle factors such as obesity, alcohol, and HRT [11, 14, 28, 29]. Few risk factors have been studied in relation to the ER and the findings are inconsistent probably due to the lack of results from large population studies or randomised studies [7, 20, 30]. The known genetic risk such as BRACA1 and BRACA2 accounts for a minor part of breast cancer cases in Denmark; however, as a course of the increase in incidence from one decade to the other, genetic evolution is not a plausible explanation [1].
In 2002, findings from the Women Health Initiative studies revealed an increased risk of breast cancer in women using HRT [11], and were later confirmed by British findings from the Million Women Study in 2003 [14]. Recent analyses from the Women Health Initiative trial confirmed a decline in breast cancer risk after discontinuation of combined hormone therapy [12]. As a consequence, reductions in the prescription of HRT was observed and used as an explanation for a decrease in breast cancer incidence found in some countries after 2002 [4, 6–8, 15, 16, 18, 31, 32]. A tendency to a decline or a plateau in incidence rates from late 1990s or early 2000 is believed to be related to the effect of mammography screening programs [7, 9, 21]. In Denmark HRT prescriptions declined from 1995 to 2002 but more than halved after 2002 [15, 22]. In order to elucidate a possible effect on breast cancer incidence, we divided our data into two time periods; before and after 2002. However, for premenopausal women 35+ years the breast cancer incidence levelled off after 2002 (Fig. 4, borderline significant), and for postmenopausal the incidence increased significantly in ER+ tumors after 2002 (Fig. 5). This finding is in contrast to the observed decline in breast cancer incidence in the US [4, 6–8], Canada [16], Belgium [18], Germany [32], and Sweden [17]. Recent analyses from US showed results in agreement with our findings. The decline in breast cancer incidence rates did not continue between 2003 and 2007 and they found a non-significant increase in ER+ in ages 40 to 49 and a decrease in ER− in ages 40 to 49 and 60 to 69 despite decreasing trends in HRT [33]. A national mammography screening program was not implemented from 1996 to 2007. Screening was performed for 20 % of all women in the age group 50–69 years in five counties out of 16. At the end of 2009, Danish national screening was fully implemented.
Determination of the estrogen hormone receptor has important implications for the adjuvant treatment of breast cancer. Hormone status acts as a prognostic and predictive factor for recurrence or mortality [30]. ER testing was introduced in 1977 using different biochemical assays and replaced by IHC in 1994 [23] and further prognostic factors have been implemented since. Human epidermal growth factor receptor 2 (HER2) and topoisomerase II-alpha (TOP2A) are now part of standardized tumor testing, together with lymph node status, tumor size, malignant grading, menopausal status, and age, to allocate women into low-risk and high-risk patients for recurrence and mortality (www.dbcg.dk/Consensus on medical treatment).
The strength of the study is the highly validated data of the DBCG database and its completeness covering 95 % of all breast cancers in Denmark. All breast cancer cases in Denmark must be reported to the Danish Cancer Registry and the DBCG database. Clinical data on treatment and follow-up are reported electronically to the DBCG database.
The limitation of the study is lack of data for the progesterone receptor. Future studies can provide more extensive analyses using other prognostic factors. Incompleteness of receptor status in the database was improved during the time of investigation (Table 1). We identified a majority of the hormone receptor data to be missing in older women (80+ years) and therefore excluded women aged 80 or older from analyses. Another important limitation is the categorical analysis using 2002 as a cut point for high HRT prescription versus low HRT prescription. Breast cancer risk estimates would be more accurate if HRT use on the individual level was used.
In summary, an increase in breast cancer incidence was seen in Denmark until 2002 and then levelled off. The increase was restricted to ER+ breast cancer in postmenopausal women whereas ER− breast cancer decreased. Until 2002 an increase in ER+ breast cancer was found in premenopausal women aged 35+. No decline in breast cancer incidence was observed in postmenopausal women from 2003 to 2007 despite a 65 % reduction in HRT prescription after 2002.
Abbreviations
- ER:
-
Estrogen receptor
- DBCG:
-
Danish Breast Cancer Group
- IHC:
-
Immunohistochemical staining
- HRT:
-
Hormone replacement therapy
- APC:
-
Annual percentage rate change
References
Lidegaard O, Kroman N (2005) The epidemiology of breast cancer. Eur Clin Obstet Gynaecol 1:24–28
Pujol P, Hilsenbeck SG, Chamness GC, Elledge RM (1994) Rising levels of estrogen receptor in breast cancer over 2 decades. Cancer 74(5):1601–1606
Li CI, Daling JR, Malone KE (2003) Incidence of invasive breast cancer by hormone receptor status from 1992 to 1998. J Clin Oncol 21(1):28–34
Glass AG, Lacey JV Jr, Carreon JD, Hoover RN (2007) Breast cancer incidence, 1980–2006: combined roles of menopausal hormone therapy, screening mammography, and estrogen receptor status. J Natl Cancer Inst 99(15):1152–1161
Anderson WF, Katki HA, Rosenberg PS (2011) Incidence of breast cancer in the United States: current and future trends. J Natl Cancer Inst 103(18):1397–1402
Ravdin PM, Cronin KA, Howlader N, Berg CD, Chlebowski RT, Feuer EJ, Edwards BK, Berry DA (2007) The decrease in breast-cancer incidence in 2003 in the United States. N Engl J Med 356(16):1670–1674
Jemal A, Ward E, Thun MJ (2007) Recent trends in breast cancer incidence rates by age and tumor characteristics among U.S. women. Breast Cancer Res 9(3):R28
Cronin KA, Ravdin PM, Edwards BK (2009) Sustained lower rates of breast cancer in the United States. Breast Cancer Res Treat 117(1):223–224
Anderson WF, Reiner AS, Matsuno RK, Pfeiffer RM (2007) Shifting breast cancer trends in the United States. J Clin Oncol 25(25):3923–3929
Collaborative Group on Hormonal Factors in Breast Cancer (1997) Breast cancer and hormone replacement therapy: collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Lancet 350(9084):1047–1059
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford AA, Howard BV, Johnson KC, Katchen JM (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA 288(3):321–333
Chlebowski RT, Kuller LH, Prentice RL, Stefanick ML, Manson JE, Gass M, Aragaki AK, Ockene JK, Lane DS, Sarto GE, Rajkovic A, Schenken R et al (2009) Breast cancer after use of estrogen plus progestin in postmenopausal women. N Engl J Med 360(6):573–587
Chlebowski RT, Anderson GL, Gass M, Lane DS, Aragaki AK, Kuller LH, Manson JE, Stefanick ML, Ockene J, Sarto GE, Johnson KC, Wactawski-Wende J et al (2010) Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA 304(15):1684–1692
Beral V (2003) Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet 362(9382):419–427
von Euler-Chelpin M (2011) Breast cancer incidence and use of hormone therapy in Denmark 1978–2007. Cancer Causes Control 22(2):181–187
De P, Neutel CI, Olivotto I, Morrison H (2010) Breast cancer incidence and hormone replacement therapy in Canada. J Natl Cancer Inst 102(19):1489–1495
Lambe M, Wigertz A, Holmqvist M, Adolfsson J, Bardage C, Fornander T, Karlsson P, Odlind V, Persson I, Ahlgren J, Bergkvist L (2010) Reductions in use of hormone replacement therapy: effects on Swedish breast cancer incidence trends only seen after several years. Breast Cancer Res Treat 121(3):679–683
Renard F, Vankrunkelsven P, Van EL, Henau K, Boniol M, Autier P (2010) Decline in breast cancer incidence in the Flemish region of Belgium after a decline in hormonal replacement therapy. Ann Oncol 21(12):2356–2360
Ewertz M, Duffy SW (1994) Incidence of female breast cancer in relation to prevalence of risk factors in Denmark. Int J Cancer 56(6):783–787
Althuis MD, Fergenbaum JH, Garcia-Closas M, Brinton LA, Madigan MP, Sherman ME (2004) Etiology of hormone receptor-defined breast cancer: a systematic review of the literature. Cancer Epidemiol Biomarkers Prev 13(10):1558–1568
Fuglede N, Langballe O, Svendsen AL, Tjonneland A, Dalton SO, Johansen C (2006) Development in incidence of breast cancer in non-screened Danish women, 1973–2002—a population-based study. Int J Cancer 118(9):2366–2369
Lokkegaard E, Lidegaard O, Moller LN, Agger C, Andreasen AH, Jorgensen T (2007) Hormone replacement therapy in Denmark, 1995–2004. Acta Obstet Gynecol Scand 86(11):1342–1351
Talman ML, Rasmussen BB, Andersen J, Christensen IJ (2008) Estrogen Receptor analyses in the Danish Breast Cancer Cooperative Group. History, methods, prognosis and clinical implications. Acta Oncol 47(4):789–794
Moller S, Jensen MB, Ejlertsen B, Bjerre KD, Larsen M, Hansen HB, Christiansen P, Mouridsen HT (2008) The clinical database and the treatment guidelines of the Danish Breast Cancer Cooperative Group (DBCG); its 30-years experience and future promise. Acta Oncol 47(4):506–524
Kim HJ, Fay MP, Feuer EJ, Midthune DN (2000) Permutation tests for joinpoint regression with applications to cancer rates. Stat Med 19(3):335–351
MacMahon B (2006) Epidemiology and the causes of breast cancer. Int J Cancer 118(10):2373–2378
Reeves GK, Pirie K, Green J, Bull D, Beral V (2009) Reproductive factors and specific histological types of breast cancer: prospective study and meta-analysis. Br J Cancer 100(3):538–544
Lahmann PH, Hoffmann K, Allen N, van Gils CH, Khaw KT, Tehard B, Berrino F, Tjonneland A, Bigaard J, Olsen A, Overvad K, Clavel-Chapelon F et al (2004) Body size and breast cancer risk: findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Int J Cancer 111(5):762–771
Schutze M, Boeing H, Pischon T, Rehm J, Kehoe T, Gmel G, Olsen A, Tjonneland A-M, Dahm CC, Overvad K, Clavel-Chapelon F, Boutron-Ruault MC et al (2011) Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ 342:d1584
Yang XR, Chang-Claude J, Goode EL, Couch FJ, Nevanlinna H, Milne RL, Goudet M, Schmidt MK, Broeks A, Cox A, Fasching PA, Hein R et al (2011) Associations of breast cancer risk factors with tumor subtypes: a pooled analysis from the Breast Cancer Association Consortium studies. J Natl Cancer Inst 103(3):250–263
Ma H, Bernstein L, Pike MC, Ursin G (2006) Reproductive factors and breast cancer risk according to joint estrogen and progesterone receptor status: a meta-analysis of epidemiological studies. Breast Cancer Res 8(4):R43
Katalinic A, Rawal R (2008) Decline in breast cancer incidence after decrease in utilisation of hormone replacement therapy. Breast Cancer Res Treat 107(3):427–430
DeSantis C, Howlader N, Cronin KA, Jemal A (2011) Breast cancer incidence rates in U.S. women are no longer declining. Cancer Epidemiol Biomarkers Prev 20(5):733–739
Conflict of interest
These authors declare that they have no conflict of interest.
Ethical standards
This study was performed in agreement with the Ethical Committees on Human Studies.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bigaard, J., Stahlberg, C., Jensen, MB. et al. Breast cancer incidence by estrogen receptor status in Denmark from 1996 to 2007. Breast Cancer Res Treat 136, 559–564 (2012). https://doi.org/10.1007/s10549-012-2269-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2269-0