Abstract
Chemotherapy is widely used to treat early stage breast cancer (ESBC). Reductions and delays in dose administered—e.g., due to advanced age or febrile neutropenia (FN)—are generally believed to increase risk of disease progression and reduce survival. Little is known about incidence of reduced chemotherapy dose intensity among women with ESBC in the current era of US clinical practice. This study employed a retrospective cohort design and electronic medical records from >65 community oncology/hematology clinics in >35 states (2004–2010). The study population comprised adult women who received myelosuppressive chemotherapy for ESBC (stages I–IIIA). For each such woman, each unique cycle of chemotherapy within their first observed course was identified. Incidence of chemotherapy dose delays (≥7 days for any drug in ≥1 cycles), chemotherapy dose reductions (≥15% for any drug in ≥1 cycles), and low chemotherapy relative dose intensity (RDI <85% over the course) relative to published reference standards were descriptively analyzed for the seven most-frequently planned regimens in the study database. A total of 2,228 women (70% of the subjects who received chemotherapy for ESBC and met other selection criteria) initiated 1 of the 7 most-frequently planned regimens. Mean age of subjects was 54 years and 69% received primary prophylaxis against FN with a colony-stimulating factor. Incidence of dose delays, dose reductions, and low RDI was 31, 24, and 26%, respectively; low RDI typically was due to premature treatment discontinuation. For patients (n = 626) receiving the most common regimen (dose-dense AC-T: doxorubicin/cyclophosphamide, Q2 × 4 cycles, paclitaxel or docetaxel, Q2 × 4 cycles), incidence of dose delays, dose reductions, and low RDI was 42, 29, and 32%, respectively. In the current era of US clinical practice, chemotherapy dose delays and dose reductions are common among women with ESBC receiving frequently used myelosuppressive dose-dense, as well as conventional, chemotherapy regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy, chiefly as neoadjuvant/adjuvant therapy, is widely used to treat early stage breast cancer (ESBC). A variety of different myelosuppressive chemotherapy regimens have proven to be efficacious and safe in clinical trials, and are commonly used today in US clinical practice [1, 2]. Reductions from published trial-based or reference “standard” dose of chemotherapy among patients with ESBC may occur due to a variety of factors—especially advanced age and hematological adverse events, such as neutropenia and related infections–and are generally believed to result in an increased risk of disease progression and poorer overall survival [3–10].
Relative dose intensity (RDI), or the amount of drug administered per unit of time as a fraction of the standard amount per unit of time, is one of the most commonly used measures of chemotherapy dose intensity [9, 11]. Although other thresholds have been used for specific cancers, an RDI <85% has been found to represent a clinically acceptable threshold for a reduction from standard therapy, below which the effectiveness of chemotherapy may be diminished and patient outcomes—including disease progression and survival—may be worse [7, 9, 11, 12]. In an evaluation of chemotherapy dose intensity among women with breast cancer in US clinical practice—a nationwide study of 20,799 early-stage breast cancer patients from August 1997 to May 2000—56% of the subjects received an RDI <85% and mean RDI among all study subjects was 0.79 [7]. Most subjects (55%) received an anthracycline-based regimen including doxorubicin (e.g., non-dose-dense doxorubicin and cyclophosphamide [AC]; cyclophosphamide, doxorubicin, and fluorouracil [CAF]), while the remainder (45%) received a non-anthracycline regimen including cyclophosphamide, methotrexate, and 5-fluorouracil (CMF).
Over the past decade, the frequency of use of alternative chemotherapy regimens for ESBC has changed considerably, in large part due to accumulating evidence of the superiority of the anthracycline-based regimens and the incorporation of the taxanes into various adjuvant chemotherapy regimens [2]. We therefore undertook an examination of the incidence of chemotherapy dose delays and dose reductions, and reduced chemotherapy RDI, among women with ESBC in the current era of US clinical practice using data from a recent 7-year period.
Methods
Data source
Data for this study were obtained from a large electronic medical records (EMR) database (SDI Health, Plymouth Meeting, PA) and spanned 2004–2010. Over this 7-year period, the database contains information on approximately 560,000 patients from more than 65 community-based or hospital-affiliated oncology/hematology practices in over 35 states.
Information included in the EMR database is directly entered by clinic staff during patient visits, and includes patient demographics (e.g., age, sex, and body surface area), performance status (Eastern Cooperative Oncology Group [ECOG] and Karnofsky), diagnoses (including type, stage, and grade of cancer), treatments, and date of visit. Treatment data include orders or prescriptions for medications, including information on dose, route, and duration of supply of oral medications, as well as the amount and timing of drugs administered in the clinic. Laboratory findings include the test ordered, the test result, units of measurement, and normal range. Information on planned chemotherapy regimen also is available, and includes the agents, doses, number of cycles, and duration of cycles. Not all participating practices routinely and comprehensively collect and report information on all of the above-noted variables.
All patient-identifying information was encrypted or removed from the study extract prior to their release to the study investigators. The extract, therefore, was fully compliant with the Health Insurance Portability and Accountability Act (HIPAA) of 1996 and federal guidance on Public Welfare and the Protection of Human Subjects. As per the Code of Federal Regulations, Institutional Review Board (IRB) review and approval was not needed for a study of this nature, since “… subjects cannot be identified, directly or through identifiers linked to the subjects…” (45 CFR 46 §46.101).
Study population
The study population included all women, aged 18 years or older, who initiated a new course of myelosuppressive chemotherapy for ESBC (stages I–IIIA) between April 1, 2004 and December 31, 2010. For patients with evidence of receipt of more than one course of chemotherapy during the study period, only the first (observed) course was considered.
Patients were excluded from the study population if: (1) they had evidence of primary breast cancer and a primary cancer in another body site at anytime during the pre-chemotherapy period; (2) they received care from a practice that did not contribute their patient-level data for at least 90 days prior to patients’ earliest observed course of chemotherapy through the end of the course; (3) they had any orders for a chemotherapy medication that is administered orally (since the precise pattern of receipt of such drugs cannot be characterized); (4) they did not have information on planned chemotherapy regimen, including the agents, doses, number of cycles, and duration of cycles; (5) their planned regimen was not consistent with published reference standards (except for planned dose, which was allowed to vary from reference standards) [1]; or (6) the combination of chemotherapy agents delivered in cycle one did not match planned agents. Thus, all patients included in the study population were required to have a planned regimen consistent with published reference standards, and to have received this regimen (i.e., in terms of the agents) during at least the first cycle of their course.
Chemotherapy cycles and regimens
For each patient in the study population, each unique cycle during the first qualifying course of chemotherapy was identified. The first cycle was defined as beginning with the date of (actual) initiation of chemotherapy, and ending with the date of the next administration (i.e., cycle) of chemotherapy, provided that it was at least 12 days––but not more than 59 days––after the date of initiation of chemotherapy. If the second cycle of chemotherapy was found to begin between 7 and 11 days following the date of initiation of chemotherapy, the first cycle of chemotherapy and all subsequent cycles were omitted from the analysis sample (because the interval between administrations of myelosuppressive chemotherapy is typically at least 7 days, agents administered from cycle day 1–6 were used to identify the regimen for that cycle). If there was no evidence of receipt of a second cycle of chemotherapy before day 60, the course of chemotherapy was considered to have ended following the first cycle; the end date for the cycle—and thus the course—was assigned based on published regimen-specific reference standards for cycle duration. The second and all subsequent cycles of chemotherapy, up to a maximum of eight, were defined in similar fashion. Each chemotherapy course thus could comprise as few as one cycle or as many as eight cycles. Delivered chemotherapy agents and doses were ascertained on a cycle-specific basis using data on all parenterally administered myelosuppressive antineoplastic agents.
Chemotherapy dose delays, reductions, and intensity
Delays in delivery of chemotherapy were ascertained based on variation in the length of intervals between cycles of chemotherapy from reference standards, and were assessed dichotomously as <7 days vs. ≥7 days based on delays in one or more individual agents. Chemotherapy dose reductions were assessed based on reductions in delivered dosages of agents administered relative to standard values, and were assessed dichotomously as ≥15% versus <15%. For regimens containing multiple agents, dose reductions were based on a reduction in one or more individual agents. Observed dosages (in mgs) were converted to doses in mg/m2 by dividing total dose by body surface area (BSA). For chemotherapy that was planned but never delivered (i.e., based on observed chemotherapy administrations in the study database), and chemotherapy that was not planned but delivered (e.g., due to regimen switch), corresponding drug doses were assumed to be zero in remaining “planned” cycles and corresponding duration of cycles was based on standard values. Patients who received fewer cycles than reference standards were assumed to have experienced a dose reduction ≥15% and dose delay ≥7 days in all missed cycles. Chemotherapy RDI was estimated based on the ratio of delivered dose intensity (DDI) to the reference standard dose intensity (SDI), and was defined as “low” if RDI was <85% (Table 1); [7, 11, 12]. For regimens containing multiple agents, RDI was based on the corresponding mean value of the individual RDIs for each myelosuppressive chemotherapy agent in the regimen. RDI values exceeding 100% were set equal to 100%.
Statistical analyses
Characteristics of study subjects at chemotherapy initiation were described, including age, body surface area, body mass index, performance status (Karnofsky or ECOG scales), cancer stage, and planned chemotherapy regimen; receipt of colony-stimulating factor (CSF) as primary prophylaxis (defined as first administration of a CSF agent by day 5 of the first cycle of the course) also was described. Characteristics were ascertained using the most recent data from the pre-chemotherapy period, unless otherwise noted, and were summarized for all study subjects and regimen-specific subgroups using mean (standard deviations [SD]) and percentages.
Delivered dose of chemotherapy (by agent) and the actual duration of cycles were tallied on a cycle-specific basis for patients in each regimen-specific subgroup, and were summarized using mean and approximate 95% confidence intervals (based on non-parametric bootstrapping); the number of patients receiving a given cycle of chemotherapy—overall and by regimen—also was tallied. Incidence of chemotherapy dose delays and dose reductions in one or more cycles during the chemotherapy course, and the incidence of RDI <85% over the chemotherapy course, were calculated along with corresponding approximate 95% confidence intervals (based on non-parametric bootstrapping). Analyses were limited to chemotherapy regimens that were planned for at least 100 patients (corresponding to the seven most-frequently planned regimens); the eighth most-frequently planned regimen included <70 patients.
Results
Patient characteristics
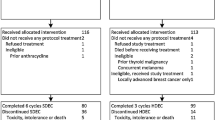
Among the 8,665 adult women in the study database who received chemotherapy for ESBC, 3,204 had planned treatment data consistent with published reference standards, received the planned agents in cycle one, and met all other selection criteria (Table 2). Among these 3,204 patients, 2,228 (70%) received 1 of the 7 most-frequently planned chemotherapy regimens in the study database and thus were considered for analyses. Planned chemotherapy regimens were (in order of frequency):
-
(1)
Dose-dense AC-T: doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2) administered every 14 days for 4 cycles (i.e., Q2 weeks × 4 cycles) followed by paclitaxel (175 mg/m2) or docetaxel (100 mg/m2) Q2 weeks × 4 cycles (n = 626);
-
(2)
TC: docetaxel (75 mg/m2) and cyclophosphamide (600 mg/m2) administered every 21 days for 4 cycles (i.e., Q3 weeks × 4 cycles) (n = 543);
-
(3)
Non-dose-dense AC: doxorubicin (60 mg/m2) and cyclophosphamide (600 mg/m2) Q3 weeks × 4 cycles (n = 415);
-
(4)
TAC: docetaxel (75 mg/m2), doxorubicin (50 mg/m2), and cyclophosphamide (500 mg/m2) Q3 weeks × 6 cycles (n = 293);
-
(5)
TCH: docetaxel (75 mg/m2) and carboplatin (360 mg/m2) Q3 weeks × 6 cycles (n = 136);
-
(6)
Non-dose-dense AC-T: same drugs/doses as regimen #1, but delivered Q3 weeks × 4 cycles (n = 114); and
-
(7)
Dose-dense AC: same drugs/doses as regimen #3, but delivered Q2 weeks × 4 cycles (n = 101).
Mean (±SD) age ranged from 51 (±10) to 56 (±11) years across regimens, and receipt of CSF primary prophylaxis (i.e., receipt in first cycle of course) ranged from 30% (non-dose-dense AC-T) to 94% (dose-dense AC) (Table 3).
Among patients receiving non-dose-dense AC-T, 54% received all planned cycles of chemotherapy, while the percentage for other regimens ranged from 76 to 87% (Table 4). Actual mean dose and mean duration of cycles among patients receiving a given cycle of chemotherapy were comparable—with few exceptions—to corresponding planned/standard values. Mean RDI was 0.86 (95% CI: 0.86–0.87) on an overall basis, and was lowest for non-dose-dense AC-T (0.74 [0.69–0.79]) and was highest for non-dose-dense AC (0.89 [0.88–0.91)) and TC (0.89 [0.87–0.91]) (Fig. 1).
The incidence of chemotherapy dose delays in ≥1 cycles during the chemotherapy course among all study subjects was 31% (29–33); the corresponding incidence of dose reductions was 24% (22–26). The overall incidence of low RDI (<85%) over the chemotherapy course was 26% (24–28) (Fig. 2). Incidence rates of dose delays and dose reductions were highest for non-dose-dense AC-T (43% [34–53] and 49% [40–59]), and were lowest for TC (dose delay, 22% [19–26]) and non-dose-dense AC (dose reduction, 16% [13–20]) and TAC (dose reduction, 16% [12–21]). Incidence of RDI <85% was highest for non-dose-dense AC-T (51% [41–60]) and was lowest for non-dose-dense AC (17% [14–21]).
Discussion
During the past decade, there has been a considerable change in the types of chemotherapy regimens used to treat ESBC, due–in large part–to the increasing popularity of the newer, more effective anthracycline-based (especially those including a taxane agent) and taxane-based regimens, as well as those regimens administered in dose-dense fashion [2]. Of the regimens commonly employed nationwide during the period 1997–2000 [7], only non-dose-dense AC (doxorubicin and cyclophosphamide, Q3 weeks × 4 cycles) remained 1 of the 7 most-frequently planned chemotherapy regimens during the period of our study (2004–2010). It appears that not only have the preferred chemotherapy regimens changed, but that administration of the newer, more effective regimens is less likely to deviate from that planned compared with the regimens preferred in prior years. Because the toxicity of some of the new regimens, especially those that are dose dense, is almost certainly greater than that of earlier regimens, this improvement in dose intensity over time is presumably due in large part to increased use of (and perhaps better) treatments to prevent or control the symptoms of toxicity, especially increased use of CSFs.
For example, in the aforementioned 1997–2000 survey, 56% of the patients had an RDI <85 versus 26% in our study, and for none of the seven regimens in our study was the percentage of patients with RDI <85% as high as 56% [7]. Among patients receiving the only regimen common to both studies (non-dose-dense AC), the incidence of RDI <85%—relative to standard—in the earlier study was 30%, versus 17% in our study. Use of CSF primary prophylaxis among all patients was about 3% in the Lyman study, compared with 69% in our study (range across regimens 30–94%) [7]. We note, however, that while increased use of CSFs may partially explain the declining incidence of low RDI over time, the profile of other important predictors also may have changed over this period, and thus the precise attribution for the improved delivery of chemotherapy is unknown. Notwithstanding the above comparison and what appears to be a declining incidence of reduced chemotherapy dose intensity over time, nearly a third of the patients receiving the most common chemotherapy regimen (dose-dense AC-T) in the study database had a low RDI.
Interestingly, 98% of the patients in the Lyman study completed at least 4 cycles of chemotherapy, versus 89% in our study; among patients for whom 8 cycles of chemotherapy was planned, the percentage completing the course was substantially lower. Among patients who actually received a planned cycle of chemotherapy, however, most were administered planned/standard doses of agents as scheduled. Premature discontinuation of chemotherapy, as opposed to dose reductions or delays, thus appears to be primarily responsible for reduced levels of RDI among subjects in our study population. Missed planned cycles of chemotherapy, and the consequences therein vis-a-vis patient outcomes, are an important component of the calculation of RDI and—as pointed out by Kuderer et al. [5]—not considering patients who prematurely discontinued treatment results in a significant overestimation of RDI.
Several of our study’s limitations are inherent in retrospective studies based on electronic medical records. All such databases contain errors of omission and commission in coding. Moreover, information often is not available for one or more clinically important parameters—either because it is not routinely collected, or because collection occurs only at healthcare encounters—and pertinent medical history can be left-censored (e.g., receipt of chemotherapy occurring before the time period of the study database is unobservable, and thus one cannot be certain whether the first observed chemotherapy course is a patient’s actual first, second, or later course).
In addition to these fundamental limitations of electronic medical records, several limitations specific to our study should be noted. First, although the large majority of patients in the study database had a diagnosis of a single primary cancer (i.e., breast cancer), some patients (<10%) had evidence of multiple primary cancers. Because we could not group these patients by primary cancer site, they were excluded from analyses. Second, patients with evidence of prescriptions for oral chemotherapy agents were excluded from the analyses, as identifying their precise patterns of use may be infeasible. Third, it was assumed that CSF administered within the 5-day period following initiation of chemotherapy in a given cycle constituted prophylaxis. Although the veracity of this assumption is uncertain, we note that other retrospective studies of CSF prophylaxis employed similar definitions [8, 13–16]. Fourth, although patient records in the study database have been extracted from more than 65 community-based or hospital-affiliated oncology/hematology practices in more than 35 states, study results may not be generalizable to other ESBC populations. Finally, our analyses focused attention on the subgroup of patients for whom planned treatment data were available in the study database and were consistent with published reference standards. This restriction was necessary for identifying appropriate benchmarks against which to compare actual receipt of chemotherapy, and for an unbiased assignment of patients to dose-dense versus non-dose-dense versions of a given chemotherapeutic regimen (e.g., AC) and to regimens with versus without a planned switch in agents (i.e., AC vs AC-T). The alternative approach (i.e., using reference standards for planned number and duration of cycles, and using observed data for agents and dose) would undoubtedly lead to misclassification of patients who received only a single cycle and those with an apparent non-dose-dense cycle length (e.g., for those who may have been scheduled to receive a dose-dense regimen but experienced a toxicity-related delay in the second cycle). It also would lead to upwardly biased estimates of dose intensity for patients receiving sequential regimens (e.g., AC-T) since they—by definition—would have to complete the first five cycles to be classified into the corresponding regimen. We acknowledge, however, that the exclusion of a substantial number of patients may bias and/or limit the generalizability of study results. We also conducted analyses considering all patients, and using first cycle data to inform planned agents and dose, and standard reference data to inform the planned number and duration of cycles. Results of these analyses were largely similar.
In conclusion, despite the popularity of newer dose-dense regimens that tend to be more toxic, the incidence of reduced chemotherapy dose intensity appears to have declined over the past decade, presumably due—at least in part—to increased use of (and perhaps better) treatments to prevent or control the symptoms of toxicity. Chemotherapy dose delays and dose reductions are, however, still common in patients with ESBC, among those receiving dose-dense as well as conventional anthracycline- and taxane-based regimens. Research examining the causes of these delays and reductions, and possible treatments for these causes, is warranted, as is continued research on the contemporaneous use of alternative chemotherapy regimens—and the implications of such use—in ESBC.
References
National Comprehensive Cancer Network (2011) NCCN clinical practice guidelines in oncology: myeloid growth factors, v1 2011. Available at http://www.nccn.org/professionals/physician_gls/pdf/myeloid_growth.pdf. Accessed 4 Aug 2011
Dang CT (2006) Drug treatments for adjuvant chemotherapy in breast cancer: recent trials and future directions. Expert Rev Anticancer Ther 6:427–436
Lyman GH, Michels SL, Reynolds MW, et al (2010) Risk of mortality in patients with cancer who experience febrile neutropenia. Cancer 116(23):5555–5563
Rajan SS, Lyman GH, Carpenter WR, Stearns SC (2010) Chemotherapy characteristics are important predictors of primary prophylactic CSF administration in older patients with breast cancer. Breast Cancer Res Treat 127(2):511–520
Kuderer NM, Dale DC, Crawford J, Lyman GH (2007) Impact of primary prophylaxis with granulocyte colony-stimulating factor on febrile neutropenia and mortality in adult cancer patients receiving chemotherapy: a systematic review. J Clin Oncol 25:3158–3167
Bonadonna G, Moliterni A, Zambetti M et al (2005) 30 years’ follow up of randomised studies of adjuvant CMF in operable breast cancer: Cohort study. BMJ 330:217
Lyman GH, Dale DC, Crawford J (2003) Incidence and predictors of low dose-intensity in adjuvant breast cancer chemotherapy: a nationwide study of community practices. J Clin Oncol 21:4524–4531
Smith TJ, Khatcheressian J, Lyman GH (2006) 2006 update of recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J Clin Oncol 24:1–19
Foote MA (1998) The importance of planned dose of chemotherapy on time: do we need to change our clinical practice? Oncologist 3:365–368
Kwak LW, Halpern J, Olshen RA, Horning SJ (1990) Prognostic significance of actual dose intensity in diffuse large-cell lymphoma: results of a tree-structured survival analysis. J Clin Oncol 8:963–977
Lyman GH (2009) Impact of chemotherapy dose intensity on cancer patient outcomes. J Natl Compr Canc Netw 7:88–108
Bonadonna G, Valagussa P, Moliterni A, Zambetti M, Brambilla C (1995) Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer: the results of 20 years of follow-up. N Engl J Med 332:901–906
Weycker D, Malin J, Barron R, Edelsberg J, Kartashov A, Oster G (2011) Comparative effectiveness of filgrastim, pegfilgrastim, and sargramostim as prophylaxis against hospitalization for neutropenic complications in cancer chemotherapy patients. Am J Clin Oncol. doi:10.1097/COC.0b013e31820dc075
Weycker D, Malin J, Kim J, Barron R, Edelsberg J, Kartashov A et al (2009) Risk of hospitalization for neutropenic complications of chemotherapy in patients with primary solid tumors receiving pegfilgrastim or filgrastim prophylaxis: a retrospective cohort study. Clin Ther 31(5):1069–1081
Morrison VA, Wong M, Hershman D, Campos LT, Ding B, Malin J (2007) Observational study of the prevalence of febrile neutropenia in patients who received filgrastim or pegfilgrastim associated with 3–4 week chemotherapy regimens in community oncology practices. J Manag Care Pharm 13(4):337–348
Weycker D, Hackett J, Edelsberg JS, Oster G, Glass AG (2006) Are shorter courses of prophylaxis associated with increased risk of hospitalization? Ann Pharmacother 40:402–407
Acknowledgements
Funding for this research was provided by Amgen Inc. to Policy Analysis Inc. (PAI).
Conflict of interest
Derek Weycker, John Edelsberg, and Alex Kartashov are employed by PAI. Gary Lyman is employed by Duke University School of Medicine, Center for Clinical Health Policy Research. Rich Barron is employed by Amgen Inc. Gary H. Lyman is a principal investigator on a research grant to Duke University from Amgen. Amgen Inc. reviewed and approved the study research plan and study manuscript; data management, processing, and analyses were conducted by PAI, and all final analytic decisions were made by study authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weycker, D., Barron, R., Edelsberg, J. et al. Incidence of reduced chemotherapy relative dose intensity among women with early stage breast cancer in US clinical practice. Breast Cancer Res Treat 133, 301–310 (2012). https://doi.org/10.1007/s10549-011-1949-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1949-5