Abstract
Purpose
To assess the impact of relative dosing intensity (RDI) on the outcomes of breast cancer patients referred for adjuvant anthracycline–taxane chemotherapy.
Methods
This is a secondary analysis of the outcomes of patients in the comparator arm of the BCIRG005 study who received adjuvant adriamycin/cyclophosphamide (AC)–docetaxel regimen. Overall survival was assessed according to RDI through Kaplan–Meier analysis. Univariate and multivariate analyses of parameters affecting overall survival were then conducted through Cox regression analysis.
Results
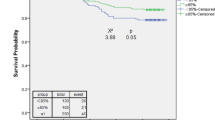
Kaplan–Meier analysis of overall survival according to RDI for the AC–docetaxel regimen (< 90 vs. ≥ 90%) was conducted and it showed that RDI < 90% is associated with worse overall survival (P = 0.006). In univariate Cox regression analysis, the following parameters significantly affected overall survival (P < 0.05): age, T stage, lymph node ratio, hormone receptor status, and grade of the disease and RDI for AC–docetaxel regimen. When these factors were included in multivariate analysis, the following factors were associated with worse overall survival: age less than 40 years (P < 0.0001), greater T stage (P < 0.0001), greater lymph node ratio (P < 0.0001), negative hormone receptor status (P = 0.001), high grade (P < 0.0001) and RDI ≤ 90% (P = 0.015). Formal interaction testing between RDI and hormone receptor status has a non-significant P value (P = 0.794).
Conclusion
Lower RDI for the whole anthracycline–taxane protocol is associated with worse patient survival. Every effort should be exercised to avoid unnecessary dose reductions and/or interruptions among early breast cancer patients receiving adjuvant anthracycline–taxane chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following standard surgery for early-stage breast cancer, adjuvant chemotherapy was proven to improve the outcomes of some patients’ subsets with adverse clinical and pathological parameters [1]. This fact was concluded from numerous clinical trials and meta-analyses which span the past five decades [2,3,4]. Relative dosing intensity (RDI) of adjuvant chemotherapy is an established quality indicator which accounts for both unplanned dose reduction and interruption.
The concept of RDI was first evaluated in a clinical trial program of cyclophosphamide, methotrexate, and fluorouracil (CMF) in 1995 and higher RDI was associated with better survival outcomes (this finding was also shown at 20-year follow-up of the patients in this program) [5]. Since the initial publication of these results, numerous strategic advances in the planning of adjuvant chemotherapy for breast cancer have occurred. These advances include the introduction of anthracyclines and taxanes in the adjuvant treatment of breast cancer as well as the subtyping of breast cancer patients according to biomarkers (estrogen receptor, progesterone receptor, and HER2) [6]. Subsequent studies tried to tackle these new scenarios; however, almost all these studies were retrospective in nature. It was thus deemed necessary to validate the relevance of RDI for anthracycline–taxane regimens in the context of a controlled prospective trial.
The newly established initiative of project data share (PDS) provides an exceptional opportunity to examine raw data of a number of landmark clinical trials [7]. One of these trials is the BCIRG005 (whose control arm is an anthracycline–taxane sequential regimen).
Assessing the real impact of RDI in the context of currently considered standard adjuvant chemotherapy regimens for early breast cancer is of paramount importance and should inform health policy decisions for those patients.
Objective
To assess the impact of RDI on the outcomes of early-stage breast cancer patients referred for adjuvant anthracycline–taxane chemotherapy.
Methodology
Data source
The current analysis represents a secondary analysis of the control arm of the randomized phase III study BCIRG005 (NCT00312208). This study was chosen because it contains all relevant information necessary to conduct the intended analysis. This study randomized node-positive, HER2-negative operable breast cancer patients to either an intervention arm of docetaxel/adriamycin/cyclophosphamide (TAC regimen) every 3 weeks for six cycles versus a control arm of adriamycin in combination with cyclophosphamide (AC regimen) every 3 weeks for four cycles followed by docetaxel every 3 weeks for four cycles. Within the PDS platform, only the raw data of the control arm of this study were available and were obtained from the PDS platform after appropriate approvals. Planned doses of drugs used in the AC–docetaxel arm were as follows: adriamycin 60 mg/m2 as an IV bolus; cyclophosphamide 600 mg/m2 as an IV infusion, docetaxel 100 mg/m2 as a 1 h IV infusion. The primary results of the BCIRG005 study were published before [8]. The control arm (AC–docetaxel) contains 1650 patients, among which 173 patients were excluded because they did not receive the planned full course of chemotherapy (eight cycles) and then 151 patients with incomplete survival data were excluded. Finally, a total of 1326 patients were included in the final analysis (Fig. 1).
Data collection
The following data were collected from the comparator arm dataset; age at diagnosis, body mass index, performance score (Karnofsky scale), T and N stages (pathological), lymph node ratio, status of hormone receptors (estrogen and progesterone receptors), grade, histological subtype, surgery type, whether or not adjuvant radiotherapy was administered, RDI for the whole chemo regimen as well as RDI for anthracycline and taxane parts of the protocol, relapse status, vital status, overall survival and relapse-free survival. RDI was calculated as per the previously published methodology of Bonadonna and coworkers [5]. According to the available protocol of BCIRG005 study, all included patients have satisfactory hepatic, bone marrow, cardiac and renal functions. Definition of overall survival was as follows: “time from randomization till death” (patients were censored if they were alive at the time of database lock). Definition of relapse-free survival was: “time from randomization till local, regional or distant relapse” (patients were censored if they did not have relapse at the time of database lock or if they died without relapse).
Statistical considerations
Overall survival was evaluated according to RDI through Kaplan–Meier analysis and log rank testing. For the sake of the current analysis, cutoff value for RDI was either 85 or 90%.
Univariate and multivariate analyses of parameters predicting overall survival and relapse-free survival were then conducted through Cox regression model. The following factors were included in the univariate analysis: age, T stage, lymph node ratio, hormone receptor status, grade and relative dose intensity. Factors with P < 0.05 in the univariate analysis were incorporated in the multivariate analysis. An additional test of interaction was conducted between RDI and hormone receptor status. Overall, a two-tailed P value < 0.05 equaled statistical significance in the current study. Statistical analyses were conducted through SPSS Statistics 20.0 (IBM, NY).
Results
Baseline characteristics of the 1326 patients were detailed in Table 1. Most of the patients have an age between 40 and 69 years (85.1%), early T stage (T1–2: 92%), ductal carcinoma histology (77.3%) and hormone receptor-positive disease (77.8%). Because all included patients have HER2-negative status, the only breast cancer subtypes represented in the current analysis were luminal breast cancer and triple negative breast cancer. All patients have an N1 disease. 33.5% of patients have a high-grade disease (grade 3). Postmenopausal patients represent 45.6% of the study population. 59.6% of the patients were treated with mastectomy, all patients were treated with adjuvant AC–docetaxel (all patients received full eight cycles) and 75.9% of the patients were treated with adjuvant radiation therapy.
Mean RDI for AC–docetaxel was: 99% (range 75–100%), 0.3% (4 patients) have RDI less than 85%; while 0.9% (12 patients) have RDI less than 90%. Mean RDI for AC part of the protocol was: 99% (range 75–100%); 0.7% of patients have RDI less than 90%. Mean RDI for docetaxel part of the protocol was: 97% (range 63–100%); 11.4% of patients have RDI less than 90%. Because of the very small number of patients with RDI less than 85%, further survival analyses were based on the 90% cutoff value.
Causes of dose reduction included hematological toxicities in 23% of cases, non-hematological toxicities in 63% of cases and other causes in 14% of cases. Median follow-up for the study cohort was 126 months (range 7–155 months).
Survival outcomes according to RDI
Kaplan–Meier analysis of overall survival according to RDI for the AC–docetaxel regimen (< 90 vs. ≥ 90%) was conducted and it showed that RDI < 90% is associated with worse overall survival (P = 0.006) (Fig. 2).
On the other hand, overall survival comparison according to RDI for the docetaxel portion of the protocol (< 90 vs. ≥ 90%) was conducted and it showed no impact on overall survival (P = 0.628); while overall survival comparison according to RDI for the AC portion of the protocol (< 90 vs. ≥ 90%) was conducted and it showed a marginal adverse impact of an RDI < 90% on overall survival (P = 0.051).
In univariate Cox regression analysis, the following parameters significantly affected overall survival (P < 0.05): age, T stage, lymph node ratio, hormone receptor status, grade of the disease and RDI for AC–docetaxel regimen. When these factors were included in multivariate analysis, the following factors were associated with worse overall survival: age less than 40 years (P < 0.0001), greater T stage (P < 0.0001), greater lymph node ratio (P < 0.0001), negative hormone receptor status (P = 0.001), high grade (P < 0.0001) and RDI ≤ 90% (P = 0.015) (Table 2). Formal interaction testing between RDI and hormone receptor has a non-significant P value (P = 0.794) (Table 2).
An additional univariate analysis for RDI for the docetaxel portion of the treatment (< 90 vs. ≥ 90%) did not significantly affect overall survival (P = 0.629). Likewise, univariate analysis for RDI for the AC portion of the treatment (< 90 vs. ≥ 90%) did not significantly affect overall survival (P = 0.060). An additional univariate analysis of RDI for docetaxel portion of treatment (as a continuous variable) failed to show significant impact on overall survival (P = 0.778). Similar assessment of RDI of AC portion as a continuous variable was not reliable statistically (because the majority of patients received 100% RDI of the AC portion). Additionally, univariate analysis for the impact of RDI for AC–docetaxel regimen on relapse-free survival was not statistically significant (P = 0.967).
Discussion
The current study provides an assessment of the impact of RDI on the survival of early breast cancer patients treated with a sequential anthracycline–taxane protocol (in the context of a prospective clinical trial). It shows that lower RDI for the whole anthracycline–taxane protocol is associated with worse patient survival.
Some theories were suggested to interpret the negative impact of a lower RDI. These include the assumption that there might be an increased probability of chemotherapy resistance in micrometastases in case of chemotherapy delay and/or interruption [9].
High-grade toxicities (whether hematological or non-hematological) represent a common cause of dose reduction and/or delay in the current analysis. Appropriate attention to supportive care and prophylactic G-CSF is thus needed when administering myelotoxic regimen to minimize the risk of unplanned dose reduction or delay [10].
Cancer centers and community hospitals who are charged with administering adjuvant treatment for early-stage breast cancer patients should conduct regular audits about their ability to maintain acceptable RDI for the majority of their patients. Regular G-CSF support should be administered to patients at high risk of neutropenic complications to avoid undue treatment delay and/or dose reduction. Moreover, attention should be paid to additional administrative confounders which might lead to unplanned treatment interruptions (e.g., ensuring stable supply and adequate stock of chemotherapy agents) [11]. This is particularly relevant in low resource settings where chemotherapy supply shortages are unfortunately common and which might compromise the survival of early-stage breast cancer patients.
The current analysis has a number of limitations that need to be acknowledged. Foremost, the current analysis represents the outcomes of highly selected clinical trial patients with strict eligibility criteria and minimal comorbid conditions. Consequently, the probability of having suboptimal RDI is expected to be much higher among patients being treated within routine practice settings. This context might also explain the relatively low numbers of patients with RDI less than 85 or 90% compared to previous retrospective studies. The low numbers of patients with RDI less than 85 or 90% has also probably affected the statistical power of many of the comparisons of the current study. Likewise, the current analysis excluded patients with HER2-positive patients as well as patients who received part or all of their chemotherapy before surgery; thus, extrapolation of the current results to these subsets of patients is not warranted. Additionally, the specific nature of the current study as a secondary analysis of a previously published clinical trial might be another source of concern. Moreover, details of hormonal therapy (if applicable) were not available for all patients in the PDS datasets; this might have confounded the survival analyses. On the other hand, there are a number of strengths to be noted in the current analysis. These include most importantly the controlled nature of data collection (including chemotherapy doses and survival outcomes). This means that the reliability of the results of the current analysis would be higher than previously published retrospective studies.
The current analysis did not show a significant interaction between hormone receptor status and RDI. This indicates that the impact of RDI is independent of breast cancer subtype. This is in line with previously published data and calls for more caution regarding RDI among all patients regardless of hormone receptor status [12].
Previous studies evaluating RDI for first-generation regimens for early breast cancer suggested 85% as a cutoff value for RDI [13]. The current analysis, however, suggests that 90% can also work as a discriminatory cutoff value in settings where very few patients received less than 85% (like in the controlled clinical trial settings).
It has to be remembered that the majority of the patients (92%) have a T1–2 disease. Moreover, all patients have an N1 disease and only one-third of patients have high-grade disease. This is combined with the observation that only 16% have hormone receptor-negative disease. With the absence of an adjunctive genomic evaluation, a predominance of low-risk disease (with no absolute indication of chemotherapy) cannot be excluded. These factors might have downplayed the true impact of a lower RDI in the studied cohort.
Different forms exist for anthracycline–taxane sequential regimens [14]. The current study evaluates only one form of them. The tendency of these regimens to induce high-grade toxicities and thus dose reduction and/or delay is variable. This is particularly relevant with regards to the variable tendencies of the taxane part of the protocol to induce hematological toxicities. Docetaxel, in the dose of 100 mg/m2 every 3 weeks, is particularly notorious for a higher incidence of hematological side effects compared to commonly used weekly or three weekly paclitaxel regimens [15]. Thus, extrapolation of the results of the current analysis to other anthracycline–taxane sequential regimens needs to be done with caution.
It is notable also in the current analysis that the probability of a compromised RDI in the docetaxel part of the protocol was far higher than the probability of a compromised RDI in the AC part of the protocol. Additionally, while lower RDI for the docetaxel part of the protocol did not affect survival, lower RDI for the anthracycline part of the protocol was associated with a marginal impact on survival (its full potential was probably concealed by the lower number of events in the anthracycline part of the protocol). This is consistent with previous retrospective studies evaluating FEC/docetaxel adjuvant chemotherapy which showed that reductions in RDI of FEC chemotherapy compared with reductions in RDI of docetaxel are correlated with inferior survival [16].
In conclusion, lower RDI for the whole anthracycline–taxane protocol is associated with worse patient survival. Every effort should be exercised to avoid unnecessary dose reductions and/or interruptions among early breast cancer patients receiving adjuvant anthracycline–taxane chemotherapy.
References
Senkus E, Kyriakides S, Ohno S, et al. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol. 2015;26(suppl_5):v8–30. https://doi.org/10.1093/annonc/mdv298.
Shannon C, Ashley S, Smith IE. Does timing of adjuvant chemotherapy for early breast cancer influence survival? J Clin Oncol. 2003;21(20):3792–7. https://doi.org/10.1200/jco.2003.01.073.
Lohrisch C, Paltiel C, Gelmon K, et al. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006;24(30):4888–94. https://doi.org/10.1200/jco.2005.01.6089.
Cold S, During M, Ewertz M, et al. Does timing of adjuvant chemotherapy influence the prognosis after early breast cancer? Results of the Danish Breast Cancer Cooperative Group (DBCG). Br J Cancer. 2005;93(6):627–32. https://doi.org/10.1038/sj.bjc.6602734.
Bonadonna G, Valagussa P, Moliterni A, et al. Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer: the results of 20 years of follow-up. N Engl J Med. 1995;332(14):901–6. https://doi.org/10.1056/nejm199504063321401.
Abdel-Rahman O. Assessment of the prognostic and discriminating value of the novel bioscore system for breast cancer; a SEER database analysis. Breast Cancer Res Treat. 2017. https://doi.org/10.1007/s10549-017-4244-2.
https://www.projectdatasphere.org/projectdatasphere/html/home. Last accessed on 7 Oct 2017.
Eiermann W, Pienkowski T, Crown J, et al. Phase III study of doxorubicin/cyclophosphamide with concomitant versus sequential docetaxel as adjuvant treatment in patients with human epidermal growth factor receptor 2-normal, node-positive breast cancer: BCIRG-005 trial. J Clin Oncol. 2011;29(29):3877–84. https://doi.org/10.1200/jco.2010.28.5437.
Goldie JH, Coldman AJ. A mathematic model for relating the drug sensitivity of tumors to their spontaneous mutation rate. Cancer Treat Rep. 1979;63(11–12):1727–33.
Zhu X, Bouganim N, Vandermeer L, et al. Use and delivery of granulocyte colony–stimulating factor in breast cancer patients receiving neoadjuvant or adjuvant chemotherapy—single-centre experience. Curr Oncol. 2012;19(4):e239–43. https://doi.org/10.3747/co.19.948.
Becker DJ, Talwar S, Levy BP, et al. Impact of oncology drug shortages on patient therapy: unplanned treatment changes. J Oncol Pract. 2013;9(4):e122–8. https://doi.org/10.1200/JOP.2012.000799.
Zhang L, Yu Q, Wu X-C, et al. Impact of chemotherapy relative dose intensity on cause-specific and overall survival for stage I-III breast cancer: ER+/PR+, HER2- vs. triple-negative. Breast Cancer Res. 2018. https://doi.org/10.1007/s10549-017-4646-1.
Chirivella I, Bermejo B, Insa A, et al. Optimal delivery of anthracycline-based chemotherapy in the adjuvant setting improves outcome of breast cancer patients. Breast Cancer Res Treat. 2009;114(3):479–84. https://doi.org/10.1007/s10549-008-0018-1.
Bines J, Earl H, Buzaid AC, et al. Anthracyclines and taxanes in the neo/adjuvant treatment of breast cancer: does the sequence matter? Ann Oncol. 2014;25(6):1079–85. https://doi.org/10.1093/annonc/mdu007.
Sparano JA, Wang M, Martino S, et al. Weekly paclitaxel in the adjuvant treatment of breast cancer. N Engl J Med. 2008;358(16):1663–71. https://doi.org/10.1056/NEJMoa0707056.
Veitch ZWN, Khan OF, Tilley D, et al. Adjustments in relative dose intensity (RDI) for FECD chemotherapy in breast cancer: a population analysis. J Clin Oncol. 2017;35(15_suppl):547. https://doi.org/10.1200/jco.2017.35.15_suppl.547.
Acknowledgements
This publication is based on research using information obtained from http://www.projectdatasphere.org, which is maintained by Project Data Sphere, LLC. Neither Project Data Sphere, LLC nor the owner(s) of any information from the website have contributed to, approved or are in any way responsible for the contents of this publication.
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The current study is fully compliant with all applicable ethical and legal standards. It complies fully with the Declaration of Helsinki.
Conflict of interest
None.
Ethical approval
This article does not contain any studies with human participants or animals performed by the author. The original study was approved by appropriate ethics committees of the participating institutes (as detailed in the published clinical trial report and clinicaltrials.gov report of this trial).
Informed consent
As this study is based on a publicly available dataset without identifying patient information, informed consent was not needed. Informed consent was, however, obtained from each of the participants of the original study (as detailed in the published clinical trial report and clinicaltrials.gov report of this trial).
Rights and permissions
About this article
Cite this article
Abdel-Rahman, O. Outcomes of early-stage breast cancer patients treated with sequential anthracyclines–taxanes in relationship to relative dosing intensity: a secondary analysis of a randomized controlled trial. Clin Transl Oncol 21, 239–245 (2019). https://doi.org/10.1007/s12094-018-1915-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-018-1915-3