Abstract
Animal and in vitro studies suggest that the use of aspirin may be associated with reduced risk for breast cancer, but results from these studies of the association have been inconsistent. The objective of this meta-analysis was to quantitatively summarize the current evidence for such a relationship. We searched MEDLINE for studies of aspirin use and breast cancer risk that were published in any language, from January 1, 1966, to July 1, 2011. A total of 33 studies (19 cohort studies, 13 case–control studies, and 1 randomized controlled trial [RCT]) that included 1,916,448 subjects were identified. We pooled the relative risks from individual studies using a random-effects model, heterogeneity, and publication bias analyses. In a pooled analysis of all studies, aspirin use was associated with reduced risk for breast cancer (odds ratio [OR] = 0.86, 95% confidence interval [CI] = 0.81, 0.92). In the subgroup analysis by study design, results were similar except for RCT (OR = 0.98, 95% CI = 0.87, 1.09). In conclusion, this meta-analysis indicated that regular use of aspirin may be associated with reduced risk of breast cancer. More RCT were needed to confirm this association in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer alone is expected to account for 26% (178,480) of all new cancer cases among women and for 15% (40,460) of all female cancer deaths in the United States of America [1]. Primary prevention of breast cancer is, therefore, very important. The mechanism of breast carcinogenesis is still not fully understood. One of the major risk factors of breast cancer is age [2]. Breast cancer may result from multiple environmental, dietary, hereditary, racial, and socioeconomic risk factors [3].
Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit production of prostaglandins and cyclooxygenase, which comes in two isoforms (COX-1 and COX-2); therefore, aspirin and other NSAIDs are potential agents for chemoprevention of breast cancer. In vitro studies have shown that breast cancers produce prostaglandins in greater amounts than normal breast cells and that aspirin can inhibit growth and decrease the invasiveness of breast cancer cells, reduce cytokines involved in bony metastasis, and stimulate immune responsiveness [4]. Although an association between aspirin use and breast cancer risk is biologically plausible, epidemiologic studies on this relationship have yielded inconsistent results [5–7]. A meta-analysis and meta-regression of observational studies from 2001 to 2005 support that aspirin may reduce breast cancer risk. Moreover, a dose–response-relationship seems to exist [8]. We therefore carried out an exhaustive meta-analysis on aspirin use and risk of breast cancer. Our objective was to provide a more definitive answer about a possible inverse relationship between use of aspirin and risk for breast cancer.
Methods
Publication search
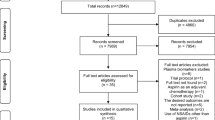
A search of the electronic databases MEDLINE (from January 1, 1966, to July 1, 2011) was performed by the following keywords: (aspirin or NSAIDs or non-steroidal anti-inflammatory drugs) and breast and (cancer or neoplasm or carcinoma or tumor). No restrictions were applied. The References lists of reviews and retrieved articles were hand searched at the same time. If necessary, we attempted to contact the corresponding authors of retrieved articles to require additional information.
Study selection
Studies were included if they met the following criteria: (1) evaluate the association between aspirin and breast cancer; (2) use a randomized controlled trial (RCT) or case–control or cohort study design; (3) provide the odds ratios (OR) or relative risk (RR) with confidence intervals (CI) or data necessary to calculate them.
Data extraction
Data were extracted independently by two investigators according to the prespecified selection criteria. We extracted the following data from each study if available: the last name of the first author, year of publication, study design, study period, the country in which the study was performed, sample size (numbers of case patients and control subjects or cohort size), and the OR or RR with corresponding 95%CI. When several estimates were available, we used the one that was adjusted for the most variables. If more than one article was published by the same author using the same population, we selected the most recent or most informative report.
Statistical analysis
The measure of effect of interest is the OR with 95%CI. Because the absolute risk of breast cancer is low, the OR mathematically approximates the RR in case–control studies; we therefore report all results as OR for simplicity [9]. The statistical heterogeneity between and within groups was measured by using the Q statistic, P < 0.1 was considered statistically significant. The Der-Simonian-Laird method for random effects were used to estimate pooled OR [10]. We calculated pooled estimates and confidence intervals assuming a random-effects model. Publication bias was investigated both visually by using a funnel plot and statistically by Begg funnel plots and Egger’s bias test, which measures the degree of funnel plot asymmetry [11, 12]. P < 0.1 was considered to be representative of statistically significant publication bias. All analysis was performed by using the STATA, version 11.0 (Stata Corporation, College Station, Texas).
Results
A total of 33 studies that included 1,916,448 subjects, published from 1980 through 2011, met the inclusion criteria and were included in the meta-analysis [13–45]. Of those, 19 studies were cohort studies, 8 studies were population-based case–control (PCC) studies, 5 studies were hospital-based case–control (HCC) studies, and 1 study was RCT. Studies were conducted in USA, Denmark, and Canada (Table 1).
When all the studies were combined into the meta-analysis, we found that aspirin use was associated with reduced risk for breast cancer (OR = 0.86, 95% CI = 0.81, 0.92) (Fig. 1). In the subgroup analysis by study design, cohort studies (OR = 0.91, 95% CI = 0.84, 0.98), PCC studies (OR = 0.79, 95% CI = 0.68, 0.90), and HCC studies (OR = 0.75, 95% CI = 0.65, 0.84) yielded similar results, except for RCT (OR = 0.98, 95% CI = 0.87, 1.09) (Fig. 1).
There was significant heterogeneity for all studies (Q = 155.39; P < 0.001; I 2 = 79.4%), and this heterogeneity remained significant for cohort studies (Q = 92.25; P < 0.001; I 2 = 80.5%) and PCC studies (Q = 35.53; P < 0.001; I 2 = 80.3%), but not for HCC studies (Q = 3.83; P = 0.43; I 2 = 0.0%). Publication bias was found for all studies by the Begg rank correlation method (P = 0.02) (Fig. 2) and the Egger weighted regression method (P = 0.003) (Fig. 3).
Discussion
In this meta-analysis of 33 studies that included 1,916,448 subjects, we found that regular use of aspirin may be associated with reduced risk of breast cancer. In the subgroup analysis by study design, results were similar except for RCT.
Many studies have investigated the associations between aspirin use and risk of other cancers. A systematic review and meta-analysis supported a protective association between aspirin and NSAIDs and esophageal cancer and provided evidence for a dose effect [46]. The study by Din et al. [47] demonstrated a protective effect against colorectal cancer associated with the lowest dose of aspirin (75 mg per day) after only 5 years use in the general population. A 20-year follow-up of five randomised trials found that aspirin taken for several years at doses of at least 75 mg daily reduced long-term incidence and mortality because of colorectal cancer [48]. Regular use of aspirin appears to reduce the risk of colorectal cancers that overexpress COX-2 but not the risk of colorectal cancers with weak or absent expression of COX-2 [49]. A meta-analysis by Yang et al. [50] indicated that regular use of aspirin may be associated with reduced risk of noncardia gastric cancer, especially among Caucasians; for H. pylori-infected subjects, the result was similar. Analysis of individual patient data from randomised trials found that daily aspirin reduced deaths because of several common cancers during and after the trials [51]. Many studies have shown that aspirin may have chemopreventive activity against prostate cancer [52–54].
The molecular mechanism by which regular use of aspirin may reduce the risk of breast cancer has been investigated by many experimental studies. Some human breast tumors cause in vitro osteolysis that may be inhibited by aspirin [55]. The aspirin metabolite salicylate inhibits breast cancer cells growth and their synthesis of the osteolytic cytokines interleukins-6 and -11 [56]. The aspirin metabolite, salicylate, inhibits 7,12-dimethylbenz[a]anthracene-DNA adduct formation in breast cancer cells [57]. Aspirin inhibits camptothecin-induced p21CIP1 levels and potentiates apoptosis in human breast cancer cells [58]. Maspin has been shown to inhibit the invasion and metastasis of breast cancer in an animal model. Ingestion of aspirin by breast cancer patients has been reported to restore the systemic synthesis of maspin through the stimulation of systemic nitric oxide production [59].
Several limitations needed to be discussed in this meta-analysis. First, although our results are consistent with former meta-analyses [5–8], we did not analyse a dose–response-relationship considering frequency and duration of aspirin use. Second, age is one of the major risk factors of breast cancer, but we cannot conduct stratified analyses adjusted by age because of the lack of enough data from the included studies. Third, as COX-2 expression is a very important factor for chemoprevention of breast cancer, it is reasonable to assume that the effectiveness of aspirin may also differ according to expression of COX-2. But we could not obtain information on the expression of COX-2 from most studies. Fourth, a significant heterogeneity and publication bias must be considered. Finally, all these studies are reported on Caucasians, so more studies were needed in Asians in the future.
In conclusion, this meta-analysis indicated that regular use of aspirin may be associated with reduced risk of breast cancer. More RCT were needed to confirm this association in the future.
References
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007) Cancer statistics, 2007. CA Cancer J Clin 57(1):43–66
Muss HB, Berry DA, Cirrincione CT, Theodoulou M, Mauer AM, Kornblith AB, Partridge AH, Dressler LG, Cohen HJ, Becker HP, Kartcheske PA, Wheeler JD, Perez EA, Wolff AC, Gralow JR, Burstein HJ, Mahmood AA, Magrinat G, Parker BA, Hart RD, Grenier D, Norton L, Hudis CA, Winer EP (2009) Adjuvant chemotherapy in older women with early-stage breast cancer. N Engl J Med 360(20):2055–2065
Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK, Goodman MT, Giuliano AE, Karanja N, McAndrew P, Hudis C, Butler J, Merkel D, Kristal A, Caan B, Michaelson R, Vinciguerra V, Del Prete S, Winkler M, Hall R, Simon M, Winters BL, Elashoff RM (2006) Dietary fat reduction and breast cancer outcome: interim efficacy results from the women’s intervention nutrition study. J Natl Cancer Inst 98(24):1767–1776
Holmes MD, Chen WY, Li L, Hertzmark E, Spiegelman D, Hankinson SE (2010) Aspirin intake and survival after breast cancer. J Clin Oncol 28(9):1467–1472
Zhao YS, Zhu S, Li XW, Wang F, Hu FL, Li DD, Zhang WC, Li X (2009) Association between NSAIDs use and breast cancer risk: a systematic review and meta-analysis. Breast Cancer Res Treat 117(1):141–150
Takkouche B, Regueira-Mendez C, Etminan M (2008) Breast cancer and use of nonsteroidal anti-inflammatory drugs: a meta-analysis. J Natl Cancer Inst 100(20):1439–1447
Khuder SA, Mutgi AB (2001) Breast cancer and NSAID use: a meta-analysis. Br J Cancer 84(9):1188–1192
Mangiapane S, Blettner M, Schlattmann P (2008) Aspirin use, breast cancer risk: a meta-analysis, meta-regression of observational studies from 2001 to 2005. Pharmacoepidemiol Drug Saf 17(2):115–124
Greenland S (1987) Quantitative methods in the review of epidemiologic literature. Epidemiol Rev 9:1–30
Robins J, Greenland S, Breslow NE (1986) A general estimator for the variance of the Mantel-Haenszel odds ratio. Am J Epidemiol 124(5):719–723
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Bardia A, Olson JE, Vachon CM, Lazovich D, Vierkant RA, Wang AH, Limburg PJ, Anderson KE, Cerhan JR (2011) Effect of aspirin and other NSAIDs on postmenopausal breast cancer incidence by hormone receptor status: results from a prospective cohort study. Breast Cancer Res Treat 126(1):149–155
Cronin-Fenton DP, Pedersen L, Lash TL, Friis S, Baron JA, Sorensen HT (2010) Prescriptions for selective cyclooxygenase-2 inhibitors, non-selective non-steroidal anti-inflammatory drugs, and risk of breast cancer in a population-based case–control study. Breast Cancer Res 12(2):R15
Brasky TM, Bonner MR, Moysich KB, Ambrosone CB, Nie J, Tao MH, Edge SB, Kallakury BV, Marian C, Trevisan M, Shields PG, Freudenheim JL (2010) Non-steroidal anti-inflammatory drug (NSAID) use and breast cancer risk in the western New York exposures and breast cancer (WEB) study. Cancer Causes Control 21(9):1503–1512
Eliassen AH, Chen WY, Spiegelman D, Willett WC, Hunter DJ, Hankinson SE (2009) Use of aspirin, other nonsteroidal anti-inflammatory drugs, and acetaminophen and risk of breast cancer among premenopausal women in the nurses’ health study II. Arch Intern Med 169(2):115–121 Discussion: 121
Friis S, Thomassen L, Sorensen HT, Tjonneland A, Overvad K, Cronin-Fenton DP, Vogel U, McLaughlin JK, Blot WJ, Olsen JH (2008) Nonsteroidal anti-inflammatory drug use and breast cancer risk: a Danish cohort study. Eur J Cancer Prev 17(2):88–96
Ready A, Velicer CM, McTiernan A, White E (2008) NSAID use and breast cancer risk in the VITAL cohort. Breast Cancer Res Treat 109(3):533–543
Gierach GL, Lacey JV Jr, Schatzkin A, Leitzmann MF, Richesson D, Hollenbeck AR, Brinton LA (2008) Nonsteroidal anti-inflammatory drugs and breast cancer risk in the National Institutes of Health-AARP Diet and Health Study. Breast Cancer Res 10(2):R38
Gill JK, Maskarinec G, Wilkens LR, Pike MC, Henderson BE, Kolonel LN (2007) Nonsteroidal antiinflammatory drugs and breast cancer risk: the multiethnic cohort. Am J Epidemiol 166(10):1150–1158
Jacobs EJ, Thun MJ, Bain EB, Rodriguez C, Henley SJ, Calle EE (2007) A large cohort study of long-term daily use of adult-strength aspirin and cancer incidence. J Natl Cancer Inst 99(8):608–615
Slattery ML, Curtin K, Baumgartner R, Sweeney C, Byers T, Giuliano AR, Baumgartner KB, Wolff RR (2007) IL6, aspirin, nonsteroidal anti-inflammatory drugs, and breast cancer risk in women living in the southwestern United States. Cancer Epidemiol Biomarkers Prev 16(4):747–755
Gallicchio L, Visvanathan K, Burke A, Hoffman SC, Helzlsouer KJ (2007) Nonsteroidal anti-inflammatory drugs and the risk of developing breast cancer in a population-based prospective cohort study in Washington County, MD. Int J Cancer 121(1):211–215
Harris RE, Beebe-Donk J, Alshafie GA (2006) Reduction in the risk of human breast cancer by selective cyclooxygenase-2 (COX-2) inhibitors. BMC Cancer 6:27
Marshall SF, Bernstein L, Anton-Culver H, Deapen D, Horn-Ross PL, Mohrenweiser H, Peel D, Pinder R, Purdie DM, Reynolds P, Stram D, West D, Wright WE, Ziogas A, Ross RK (2005) Nonsteroidal anti-inflammatory drug use and breast cancer risk by stage and hormone receptor status. J Natl Cancer Inst 97(11):805–812
Zhang Y, Coogan PF, Palmer JR, Strom BL, Rosenberg L (2005) Use of nonsteroidal antiinflammatory drugs and risk of breast cancer: the case–control surveillance study revisited. Am J Epidemiol 162(2):165–170
Swede H, Mirand AL, Menezes RJ, Moysich KB (2005) Association of regular aspirin use and breast cancer risk. Oncology 68(1):40–47
Rahme E, Ghosn J, Dasgupta K, Rajan R, Hudson M (2005) Association between frequent use of nonsteroidal anti-inflammatory drugs and breast cancer. BMC Cancer 5:159
Cook NR, Lee IM, Gaziano JM, Gordon D, Ridker PM, Manson JE, Hennekens CH, Buring JE (2005) Low-dose aspirin in the primary prevention of cancer: the women’s health study: a randomized controlled trial. JAMA 294(1):47–55
Garcia Rodriguez LA, Gonzalez-Perez A (2004) Risk of breast cancer among users of aspirin and other anti-inflammatory drugs. Br J Cancer 91(3):525–529
Terry MB, Gammon MD, Zhang FF, Tawfik H, Teitelbaum SL, Britton JA, Subbaramaiah K, Dannenberg AJ, Neugut AI (2004) Association of frequency and duration of aspirin use and hormone receptor status with breast cancer risk. JAMA 291(20):2433–2440
Ratnasinghe LD, Graubard BI, Kahle L, Tangrea JA, Taylor PR, Hawk E (2004) Aspirin use and mortality from cancer in a prospective cohort study. Anticancer Res 24(5B):3177–3184
Moorman PG, Grubber JM, Millikan RC, Newman B (2003) Association between non-steroidal anti-inflammatory drugs (NSAIDs) and invasive breast cancer and carcinoma in situ of the breast. Cancer Causes Control 14(10):915–922
Harris RE, Chlebowski RT, Jackson RD, Frid DJ, Ascenseo JL, Anderson G, Loar A, Rodabough RJ, White E, McTiernan A (2003) Breast cancer and nonsteroidal anti-inflammatory drugs: prospective results from the women’s health initiative. Cancer Res 63(18):6096–6101
Johnson TW, Anderson KE, Lazovich D, Folsom AR (2002) Association of aspirin and nonsteroidal anti-inflammatory drug use with breast cancer. Cancer Epidemiol Biomarkers Prev 11(12):1586–1591
Cotterchio M, Kreiger N, Sloan M, Steingart A (2001) Nonsteroidal anti-inflammatory drug use and breast cancer risk. Cancer Epidemiol Biomarkers Prev 10(11):1213–1217
Harris RE, Kasbari S, Farrar WB (1999) Prospective study of nonsteroidal anti-inflammatory drugs and breast cancer. Oncol Rep 6(1):71–73
Coogan PF, Rao SR, Rosenberg L, Palmer JR, Strom BL, Zauber AG, Stolley PD, Shapiro S (1999) The relationship of nonsteroidal anti-inflammatory drug use to the risk of breast cancer. Prev Med 29(2):72–76
Neugut AI, Rosenberg DJ, Ahsan H, Jacobson JS, Wahid N, Hagan M, Rahman MI, Khan ZR, Chen L, Pablos-Mendez A, Shea S (1998) Association between coronary heart disease and cancers of the breast, prostate, and colon. Cancer Epidemiol Biomarkers Prev 7(10):869–873
Egan KM, Stampfer MJ, Giovannucci E, Rosner BA, Colditz GA (1996) Prospective study of regular aspirin use and the risk of breast cancer. J Natl Cancer Inst 88(14):988–993
Harris RE, Namboodiri KK, Farrar WB (1996) Nonsteroidal antiinflammatory drugs and breast cancer. Epidemiology 7(2):203–205
Schreinemachers DM, Everson RB (1994) Aspirin use and lung, colon, and breast cancer incidence in a prospective study. Epidemiology 5(2):138–146
Thun MJ, Namboodiri MM, Calle EE, Flanders WD, Heath CW Jr (1993) Aspirin use and risk of fatal cancer. Cancer Res 53(6):1322–1327
Paganini-Hill A, Chao A, Ross RK, Henderson BE (1989) Aspirin use and chronic diseases: a cohort study of the elderly. BMJ 299(6710):1247–1250
Friedman GD, Ury HK (1980) Initial screening for carcinogenicity of commonly used drugs. J Natl Cancer Inst 65(4):723–733
Corley DA, Kerlikowske K, Verma R, Buffler P (2003) Protective association of aspirin/NSAIDs and esophageal cancer: a systematic review and meta-analysis. Gastroenterology 124(1):47–56
Din FV, Theodoratou E, Farrington SM, Tenesa A, Barnetson RA, Cetnarskyj R, Stark L, Porteous ME, Campbell H, Dunlop MG (2010) Effect of aspirin and NSAIDs on risk and survival from colorectal cancer. Gut 59(12):1670–1679
Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, Meade TW (2010) Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet 376(9754):1741–1750
Chan AT, Ogino S, Fuchs CS (2007) Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N Engl J Med 356(21):2131–2142
Yang P, Zhou Y, Chen B, Wan HW, Jia GQ, Bai HL, Wu XT (2010) Aspirin use and the risk of gastric cancer: a meta-analysis. Dig Dis Sci 55(6):1533–1539
Rothwell PM, Fowkes FG, Belch JF, Ogawa H, Warlow CP, Meade TW (2011) Effect of daily aspirin on long-term risk of death due to cancer: analysis of individual patient data from randomised trials. Lancet 377(9759):31–41
Dhillon PK, Kenfield SA, Stampfer MJ, Giovannucci EL (2011) Long-term aspirin use and the risk of total, high-grade, regionally advanced and lethal prostate cancer in a prospective cohort of health professionals, 1988–2006. Int J Cancer 128(10):2444–2452
Salinas CA, Kwon EM, FitzGerald LM, Feng Z, Nelson PS, Ostrander EA, Peters U, Stanford JL (2010) Use of aspirin and other nonsteroidal antiinflammatory medications in relation to prostate cancer risk. Am J Epidemiol 172(5):578–590
Jacobs EJ, Rodriguez C, Mondul AM, Connell CJ, Henley SJ, Calle EE, Thun MJ (2005) A large cohort study of aspirin and other nonsteroidal anti-inflammatory drugs and prostate cancer incidence. J Natl Cancer Inst 97(13):975–980
Powles TJ, Clark SA, Easty DM, Easty GC, Neville AM (1973) The inhibition by aspirin and indomethacin of osteolytic tumor deposits and hypercalcaemia in rats with Walker tumour, and its possible application to human breast cancer. Br J Cancer 28(4):316–321
Sotiriou C, Lacroix M, Lagneaux L, Berchem G, Body JJ (1999) The aspirin metabolite salicylate inhibits breast cancer cells growth and their synthesis of the osteolytic cytokines interleukins-6 and -11. Anticancer Res 19(4B):2997–3006
Abbadessa G, Spaccamiglio A, Sartori ML, Nebbia C, Dacasto M, Di Carlo F, Racca S (2006) The aspirin metabolite, salicylate, inhibits 7, 12-dimethylbenz[a]anthracene-DNA adduct formation in breast cancer cells. Int J Oncol 28(5):1131–1140
Alfonso LF, Srivenugopal KS, Arumugam TV, Abbruscato TJ, Weidanz JA, Bhat GJ (2009) Aspirin inhibits camptothecin-induced p21CIP1 levels and potentiates apoptosis in human breast cancer cells. Int J Oncol 34(3):597–608
Bhattacharyya M, Girish GV, Ghosh R, Chakraborty S, Sinha AK (2010) Acetyl salicylic acid (aspirin) improves synthesis of maspin and lowers incidence of metastasis in breast cancer patients [corrected]. Cancer Sci 101(10):2105–2109
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The author Hua-Mei Yan contributed equally to the work.
Rights and permissions
About this article
Cite this article
Luo, T., Yan, HM., He, P. et al. Aspirin use and breast cancer risk: a meta-analysis. Breast Cancer Res Treat 131, 581–587 (2012). https://doi.org/10.1007/s10549-011-1747-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1747-0