Abstract
Concurrent use of tamoxifen and cytochrome P450 2D6 (CYP2D6) inhibitors, such as selective serotonin reuptake inhibitors, has been shown to decrease plasma concentrations of tamoxifen metabolites. However, it is still unclear whether such concurrent use affects tamoxifen’s effectiveness. Thus, the objective of this study is to determine whether concurrent use of tamoxifen with CYP2D6 inhibitors increases the risk of recurrence in patients newly diagnosed with breast cancer. We conducted a nested case–control analysis within a population-based cohort from the UK General Practice Research Database. The cohort included women with a first-ever diagnosis of breast cancer who were prescribed tamoxifen between January 1, 1998 and June 30, 2008. Cases consisted of all patients with a breast cancer recurrence occurring during follow-up. Up to ten controls were matched to each case on year of birth, date of cohort entry, and duration of follow-up. Conditional logistic regression was used to estimate rate ratios (RR) of breast cancer recurrence in patients who concurrently used tamoxifen with CYP2D6 inhibitors, compared to patients who only used tamoxifen. The cohort included 9,209 incident users of tamoxifen, of whom 807 were diagnosed with a breast cancer recurrence. Concurrent use was not associated with an increased incidence of breast cancer recurrence (adjusted RR 1.07, 95% 0.88, 1.30). Type and strength of CYP2D6 inhibitors, as well as duration of concurrent use did not affect breast cancer recurrence. These results remained consistent after performing sensitivity analyses. The results of this large population-based study indicate that concurrent use of tamoxifen with CYP2D6 inhibitors does not increase the risk of recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For nearly three decades, tamoxifen has been used in patients with early breast cancer and estrogen-receptor positive tumors. In the adjuvant setting, a 5-year treatment has been associated with a 40% reduction in breast cancer recurrences, and a 30% reduction in breast cancer-related deaths [1]. While aromatase inhibitors have been shown to have a superior efficacy and good tolerability over tamoxifen in postmenopausal women, tamoxifen remains the only treatment option in premenopausal women [2, 3].
Tamoxifen is metabolized into its more active metabolites, 4-hydroxytamoxifen and 4-hydroxy N-desmethyltamoxifen (endoxifen), by the cytochrome P450 2D6 (CYP2D6) enzyme. With more than 80 known allelic variants, polymorphisms of this enzyme have been associated with different clinical outcomes in several settings [4]. With respect to tamoxifen, several studies have shown that patients with the wild-type (normal) CYP2D6 enzyme have been shown to have a better prognosis such as time to recurrence and disease-free survival, than patients with reduced or absent CYP2D6 enzyme activity [5]. Thus, the metabolic activity of this enzyme is an important predictor of treatment outcome.
Over 25% of commonly prescribed drugs are also metabolized by the CYP2D6 enzyme [4, 6]. These include antidepressants, anti-arrhythmics, antipsychotics, and β-blockers [4]. If taken concurrently with tamoxifen, these drugs can either act as competitive or non-competitive inhibitors, thereby decreasing CYP2D6 activity. In fact, concurrent use of tamoxifen and certain antidepressants has been shown to decrease plasma concentration levels of endoxifen [7, 8], raising the concern that such concurrent use might possibly increase the risk of recurrence in these patients.
To date, only a few observational studies have been conducted to investigate the effects of concurrent use of tamoxifen and CYP2D6 inhibitors on breast cancer recurrence [9–16]. Because of certain methodological limitations, these studies have produced inconclusive results. In one study [10], patients with reduced CYP2D6 function who took inhibitors during their tamoxifen treatment were at a greater risk of breast cancer recurrence and cancer-related death than patients with normal CYP2D6 function who did not take any inhibitors. While this study revealed the overall importance of CYP2D6 function, questions remain as to whether it is the reduced enzyme function or the use of inhibitors that was responsible for the observed results. As for those studies finding null associations [9, 11–16], limitations included small sample sizes, no consideration of latency time windows, and no adjustment for potential confounders such as body mass index (BMI) and smoking.
Given the continued concerns related to the use of tamoxifen with CYP2D6 inhibitors, which include selective serotonin reuptake inhibitors (SSRI) [17], carefully designed, large population-based studies are needed to evaluate the long-term effects of such concurrent use. Thus, the objective of this large population-based study was to determine whether concurrent use of tamoxifen and CYP2D6 inhibitors increase the risk of recurrence in patients with breast cancer.
Methods
Data source
This study was conducted using the General Practice Research Database (GPRD), a primary care database from the United Kingdom (UK) [18]. The GPRD is the world’s largest computerized database of longitudinal records from primary care. It contains the complete primary care medical record for more than 9.9 million people (corresponding to around 7.4% of the UK population) enrolled in more than 545 general practices. The geographic distribution of the practices participating in the GPRD has been shown to be representative of the UK population, and age and sex distributions of patients in the GPRD are similar to those reported by the National Population Census [19]. Participating general practitioners have been trained to record medical information including demographic data, medical diagnoses, details of hospital stays, and deaths using a standardized form. Prescriptions written by GPRD physicians are automatically transcribed into the computer record. In addition, the GPRD collects information regarding lifestyle variables such as BMI, and quantitative and qualitative data pertaining to smoking and excessive alcohol use. The READ classification is used to enter medical diagnoses and procedures, and a coded drug dictionary based on the UK Prescription Pricing Authority Dictionary is used for recording prescriptions. The recorded information on drug exposures and diagnoses has been validated and proven to be of high quality [20–23]. The study protocol was approved by the Scientific and Ethical Advisory Group of the GPRD.
Study population
We conducted a population-based cohort study using a nested case–control analysis within the GPRD population. We identified all female patients, at least 18 years of age, diagnosed with breast cancer for the first time and who were prescribed at least one tamoxifen prescription between January 1, 1998 and June 30, 2008. All patients were required to have at least 1 year of follow-up after their first tamoxifen prescription. This was to ensure that all cohort members would have a minimum potential exposure period of at least 1 year. This was also shown to be the required time for tamoxifen to exert its beneficial effects [1]. Cohort entry corresponded to the year after the first tamoxifen prescription.
We excluded patients with less than 1 year of up-to-standard medical history in the GPRD prior to the first tamoxifen prescription, those prescribed tamoxifen before January 1, 1998, those prescribed tamoxifen more than 3 months prior to the primary diagnosis, those prescribed a first tamoxifen prescription more than 12 months after the primary diagnosis, and women receiving concurrent prescriptions of tamoxifen and aromatase inhibitors.
All patients were followed from cohort entry until a breast cancer recurrence, death from any cause, end of registration with the general practice, or end of the study period (June 30, 2008), whichever came first.
Study design
This was a retrospective cohort study using nested case–control analysis. This approach was used because of the time-varying nature of the exposure, the size of the cohort, and the long duration of follow-up [24]. Thus, in comparison to a time-dependent survival analysis, a nested case–control analysis is computationally more efficient [25], while producing odds ratios that are unbiased estimators of incidence rate ratios (RR), with little or no loss in precision [24–26].
Case–control selection
From the cohort of patients described above, we identified all cases with medical diagnoses of local, regional, and distant recurrences of breast cancer occurring during follow-up. This definition included contralateral breast cancers, secondary primaries, and evidence of metastatic disease. The calendar date of each case’s breast cancer recurrence was defined as the index date. Up to 10 controls were randomly selected from the case’s risk set, after matching on year of birth (±1 year), date of cohort entry (±1 year), and duration of follow-up. As a result of the sampling scheme, all controls were alive, never diagnosed with a recurrence, and registered with their general practice when matched to a given case, and thus had equal duration of follow-up at the risk set date.
Exposure assessment
For each case and control, we obtained all prescription information between cohort entry and index date. Exposures in the year prior to index date were excluded to take into account a biologically meaningful latency time window. Furthermore, exclusion of exposures in this time period minimizes the possibility that exposure to certain CYP2D6 inhibitors, such as codeine, might have been influenced by early signs or symptoms of a breast cancer recurrence (protopathic bias), as well as detection bias, where the initiation of a new treatment may lead to an increase in diagnostic investigations leading to an increase in the probability of identifying a recurrence.
A tamoxifen treatment was defined as the time between the first and the last prescription in a patient’s record plus the specified duration of the last prescription to which an additional 70 days were added, corresponding to the five half-life elimination period of the metabolites [27]. In the UK, tamoxifen is mainly used in the adjuvant setting for non-metastatic incident breast cancer [28].
Concurrent users were defined as those who were ever prescribed at least one CYP2D6 inhibitor during their tamoxifen treatment. Consequently, non-concurrent users were those who were ever prescribed a CYP2D6 inhibitor either before or after, but never during their tamoxifen treatment. The CYP2D6 enzyme has no known inducers [6]. A total of 51 CYP2D6 inhibitors of varying binding affinities were considered in this study. These are listed in the appendix.
Statistical analysis
Descriptive statistics were used to summarize the characteristics of the cohort, along with the most frequently concurrently prescribed CYP2D6 inhibitors. Person-time at risk was measured from cohort entry (the year after the first tamoxifen prescription) to time of event or end of follow-up. Thus, the crude rate of recurrence, along with confidence intervals based on the Poisson distribution, was calculated by dividing the number of patients with recurrences over the person-time at risk.
The primary analysis consisted of determining whether concurrent use of tamoxifen and any CYP2D6 inhibitor increased the risk of recurrence. Thus, cases and controls were categorized into three mutually exclusive groups based on the following exposure patterns: (1) tamoxifen only, (2) concurrent use of tamoxifen with at least one CYP2D6 inhibitor, and (3) non-concurrent use of a CYP2D6 inhibitor. The reference category for this analysis consisted of patients who only used tamoxifen between cohort entry and index date.
We also conducted three secondary analyses based on a priori hypotheses. In the first, patients deemed to be ever concurrent users were further categorized according to duration of concurrent use. Their duration of concurrent use was categorized into quartiles based on the distribution of concurrent use in the controls (<30, 30–90, 90–365, and ≥365 days).
In the second analysis, we investigated whether drugs with different binding affinities to the CYP2D6 enzyme also differed in their association with respect to breast cancer recurrence. Given the fact that tamoxifen has a moderate binding affinity to the CYP2D6 enzyme, it was hypothesized that CYP2D6 inhibitors with strong or moderate binding affinities would be more likely to affect tamoxifen’s effectiveness, and as a result, lead to a higher breast cancer recurrence risk than drugs with weak binding affinities. To investigate this hypothesis, concurrent users were categorized according into five mutually exclusive groups of patients: inhibitors only, strong substrates only, moderate substrates only, weak substrates only, and combinations of any of these categories.
Finally, it was of interest to conduct a separate analysis on antidepressants, as these represent the most frequently prescribed drug class in this population, often used to treat tamoxifen-related side effects, such as hot flashes [29]. Thus, concurrent users were categorized into three mutually exclusive groups: those who used moderate/strong CYP2D6 antidepressants (bupropion, doxepin, duloxetine, fluoxetine, maprotiline, paroxetine, and sertraline), weak CYP2D6 antidepressants (citalopram, escitalopram, fluvoxamine, mirtazapine, and venlafaxine), and combinations of moderate/strong and weak antidepressants. For all the secondary analyses described above, the reference category consisted of patients who only used tamoxifen between cohort entry and index date.
Conditional logistic regression was used to estimate RRs, along with 95% CIs. In addition to age and date of cohort entry on which the logistic regression was conditioned, we adjusted for the following potential baseline confounders: lifestyle variables (measured in the year prior to cohort entry), which consisted of smoking (ever vs. never), excessive alcohol use and obesity (BMI ≥ 30), as well as history of oophorectomy. We also adjusted the models for the previous use of the following drugs: hormone replacement therapy, antidepressants (other than CYP2D6 substrates), anti-diabetic agents, NSAIDs (other than CYP2D6 substrates), benzodiazepines, antipsychotic drugs (other than CYP2D6 substrates), and statins. All analyses were conducted with SAS version 9.2 (SAS Institute, Cary, NC).
Sensitivity analyses
We conducted two sensitivity analyses to assess the robustness of the results. In the first sensitivity analysis, we repeated the analyses after considering tamoxifen metabolite elimination periods of different lengths. Specifically, we conducted one analysis which ignored an elimination period and one assuming a 90-day elimination period. In the second sensitivity analysis, we assessed the impact of excluding the year prior to index date, by repeating the analyses using a 6-month lag period.
Results
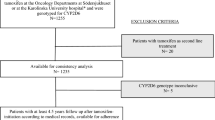
A total of 9,209 women were diagnosed with breast cancer and were prescribed at least one tamoxifen prescription during the study period (Fig. 1). The mean (SD) age at cohort entry was 61.7 (13.5) years, and the mean (SD) duration of follow-up was 4.5 (2.5) years. The mean (SD) duration of a tamoxifen treatment was 3.1 (1.8) years.
A total of 807 patients experienced a breast cancer recurrence during 32,682 person-years of follow-up, yielding a crude recurrence rate of 24.7/1000 persons per year (95% CI 23.0, 26.4). These cases were matched to 7,941 controls. Compared to controls, cases were likely to have been prescribed antidepressants, antipsychotics, and benzodiazepines at baseline (Table 1).
The five most frequently prescribed CYP2D6 inhibitors among controls consisted of codeine (26.8%), fluoxetine (5.1%), citalopram (4.3%), ranitidine (4.0%), and metoclopramide (3.6%). Overall, 3,473 (43.7%) controls were prescribed at least one CYP2D6 inhibitor concurrently with tamoxifen. Of those, 2,201 (63.4%) were prescribed only one, 796 (22.9%) were prescribed two, while 476 (13.7%) were prescribed three or more different drugs at any time during their tamoxifen treatment. The mean (SD) duration of concurrent use of tamoxifen and at least one CYP2D6 inhibitor was 289.0 (397.9) days.
The results of the primary analysis are presented in Table 2. Patients concurrently using tamoxifen with a CYP2D6 inhibitor were not at an increased risk of breast cancer recurrence, when compared to patients who only used tamoxifen during follow-up (adjusted RR 1.07, 95% 0.88, 1.30).
The results of the secondary analyses produced results similar to those of the primary analysis. Specifically, the incidence of breast cancer recurrence did not increase with duration of concurrent use (Table 3). Furthermore, the type or strength of CYP2D6 molecules did not have an effect on recurrence (Table 4). Finally, concurrent use of moderate or strong CYP2D6 antidepressants enzyme did not increase the incidence of breast cancer recurrence (Table 5).
Sensitivity analyses
All sensitivity analyses yielded results consistent with those of the primary analysis. The first sensitivity analysis consisted of considering different durations of tamoxifen treatment based on varying the length of the metabolite elimination period. Ignoring an elimination period altogether and considering one of 90 days had no material effect on the point estimates (adjusted RR 1.04, 95% CI 0.86, 1.27 and adjusted RR 1.08, 95% CI 0.89, 1.31, respectively). The second sensitivity analysis consisted of excluding exposures in the 6 months prior to index date. This analysis also yielded comparable results (adjusted RR 1.17, 95% CI 0.96, 1.41).
Discussion
The results of this large population-based study indicate that tamoxifen-treated patients were frequently prescribed CYP2D6 inhibitors during their treatment. This concurrent use did not appear to increase their risk of recurrence. The results remained unchanged after investigating the effects of duration of use, and type of CYP2D6 inhibitor used. Furthermore, all sensitivity analyses yielded results consistent with those of the primary analysis.
The results of this study provide further evidence that CYP2D6 inhibitors do not increase the risk of recurrence in patients with breast cancer. Indeed, they are concordant with nearly all observational studies that have specifically investigated this outcome [9, 11–16]. However, they differ from those of a recently published study, which found that regular use of paroxetine during tamoxifen treatment nearly doubled the risk of breast cancer-related deaths (hazard ratio 1.91, 95% CI 1.26–2.89) [30]. As part of the inclusion criteria, the authors restricted their study to patients who had used only one SSRI during tamoxifen treatment. Therefore, patients who had never used SSRIs concurrently with tamoxifen and those had switched from one SSRI to another were excluded from the analysis. Thus, patients meeting the inclusion criteria represented 10% of those initially prescribed tamoxifen (2,430 of 24,430 of tamoxifen-treated patients), and had an exceptionally high overall mortality rate (1,074 (44%) deaths after a mean of 2.4 years of follow-up). Questions remain as to whether these restrictive inclusion criteria may have affected the generalisability of the results. Furthermore, the authors limited their analysis to mortality and did not investigate recurrence. We conducted a separate analysis on antidepressants, which included not only moderate and strong SSRIs, but also other antidepressants known to have strong affinities to the CYP2D6 enzyme. This analysis did not reveal any association between the concurrent use of tamoxifen and these drugs. Taken together with the results of previous published studies [9, 11–16], the use of these drugs do not appear to affect tamoxifen’s effectiveness, and thus do not increase the risk of recurrence in patients with breast cancer.
While there is evidence to suggest that CYP2D6 inhibitors do indeed decrease plasma concentration levels of endoxifen [7, 8], there is accumulating evidence that lower doses of tamoxifen may confer the same protective effect on recurrence, with the advantage of reducing serious adverse events such as venous thrombosis [31, 32]. Randomized controlled trials have shown that doses as low as 1 and 5 mg/day have similar efficacy as the standard 20 mg/day treatment regimen [31, 32]. This indicates that the standard tamoxifen dose of 20 mg/day may exceed what is needed for maximal anti-proliferative activity [31]. Given this evidence, it is likely that CYP2D6 inhibitors decrease plasma concentration levels of tamoxifen metabolites [7, 8], but these reductions may not be sufficient to significantly affect tamoxifen’s overall effectiveness.
This population-based study has a number of strengths. First, we have assembled one the largest population-based cohort of tamoxifen-treated breast cancer patients followed for up to 10 years. Second, we compiled an exhaustive list of over 50 drugs that were available in the UK market during the study period, known to be metabolized the CYP2D6 enzyme. This list included both non-competitive and competitive inhibitors (substrates) of the CYP2D6 enzyme. These were distinguished in terms of type and strength in secondary analyses. Third, we applied lag periods of 6 months and 1 year to consider biologically meaningful latency time windows and minimize the possibility of protopathic bias. Fourth, our exposure definition was time-dependent as a result of the sampling scheme used to select controls. Fifth, because exposure is prospectively entered in the GPRD, the possibility of recall bias is eliminated. Finally, the GPRD database contains information on a number of important confounders, such as BMI, excessive alcohol use, and smoking. Therefore, we were able to adjust for a number of confounders often absent in administrative databases.
This study has some of limitations. First, the GPRD does not collect information on breast cancer prognostic markers, such as tumor size, histological grade, and nodal status. However, while these are likely to be good predictors of recurrence, it is unclear how the presence of these markers would influence the prescribing of CYP2D6 inhibitors concomitantly with tamoxifen. In fact, inclusion of these variables in a recent cohort study had no material effect on the point estimates [15]. Similarly, the GPRD does not collect information on CYP2D6 genotype, which some studies have shown to be an independent predictor of treatment outcome [5]. Since this information was not available to the prescribing physicians, we do not believe that it directly influenced their decision to concurrently prescribe tamoxifen with a CYP2D6 inhibitor [33]. Furthermore, all patients in this study were prescribed tamoxifen, likely with the belief that they would adequately metabolize the drug. Thus, CYP2D6 genotype does not satisfy the definition of a confounder as it was not associated with the exposures of interest. Second, tamoxifen treatment is usually initiated outside the primary care setting. However, in UK, patient follow-up and renewal of prescription are routinely carried out by general practitioners. Finally, drug information in the GPRD represents prescriptions written by general practitioners. As such, it is unknown whether prescriptions were actually filled at the pharmacy and whether patients fully complied with the treatment regimen. However, we have previously shown that tamoxifen compliance, as measured by renewal between prescriptions, was over 80% in this population during the study period [34].
To our knowledge, this is the largest population-based study to have investigated the effects of concurrent use of tamoxifen with CYP2D6 inhibitors on breast cancer recurrence. Using an exhaustive list of known CYP2D6 inhibitors, our results do not indicate an increased risk of recurrence among concurrent users. These results remained unchanged after performing several secondary and sensitivity analyses. While the results of this study do not provide definitive evidence on this question, they add to the existing literature finding null effects of concurrent use of tamoxifen with CYP2D6 inhibitors on breast cancer recurrence.
References
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365:1687–1717
Perez EA (2007) Safety profiles of tamoxifen and the aromatase inhibitors in adjuvant therapy of hormone-responsive early breast cancer. Ann Oncol 18(Suppl 8):viii26–viii35
Jordan VC (2007) New insights into the metabolism of tamoxifen and its role in the treatment and prevention of breast cancer. Steroids 72:829–842
Ingelman-Sundberg M (2005) Genetic polymorphisms of cytochrome P450 2D6 (CYP2D6): clinical consequences, evolutionary aspects and functional diversity. Pharmacogenomics J 5:6–13
Seruga B, Amir E (2010) Cytochrome P450 2D6 and outcomes of adjuvant tamoxifen therapy: results of a meta-analysis. Breast Cancer Res Treat 122:609–617
Lacy C, Armstrong L, Goldman M, Lance L (2007) Cytochrome P450 enzymes: substrates, inhibitors, and inducers. In: Lacy C, Armstrong L, Goldman M, Lance L (eds) Drug information handbook, 15th edn. LexiComp Inc., Hudson, pp 1899–1912
Stearns V, Johnson MD, Rae JM, Morocho A, Novielli A, Bhargava P et al (2003) Active tamoxifen metabolite plasma concentrations after coadministration of tamoxifen and the selective serotonin reuptake inhibitor paroxetine. J Natl Cancer Inst 95:1758–1764
Jin Y, Desta Z, Stearns V, Ward B, Ho H, Lee KH et al (2005) CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 97:30–39
Lehmann D, Nelsen J, Ramanath V, Newman N, Duggan D, Smith A (2004) Lack of attenuation in the antitumor effect of tamoxifen by chronic CYP isoform inhibition. J Clin Pharmacol 44:861–865
Goetz MP, Knox SK, Suman VJ, Rae JM, Safgren SL, Ames MM et al (2007) The impact of cytochrome P450 2D6 metabolism in women receiving adjuvant tamoxifen. Breast Cancer Res Treat 101:113–121
Lash TL, Pedersen L, Cronin-Fenton D, Ahern TP, Rosenberg CL, Lunetta KL et al (2008) Tamoxifen’s protection against breast cancer recurrence is not reduced by concurrent use of the SSRI citalopram. Br J Cancer 99:616–621
Chubak J, Buist DS, Boudreau DM, Rossing MA, Lumley T, Weiss NS (2008) Breast cancer recurrence risk in relation to antidepressant use after diagnosis. Breast Cancer Res Treat 112:123–132
Ahern TP, Pedersen L, Cronin-Fenton DP, Sorensen HT, Lash TL (2009) No increase in breast cancer recurrence with concurrent use of tamoxifen and some CYP2D6-inhibiting medications. Cancer Epidemiol Biomarkers Prev 18:2562–2564
Lash TL, Cronin-Fenton D, Ahern TP, Rosenberg CL, Lunetta KL, Silliman RA et al (2010) Breast cancer recurrence risk related to concurrent use of SSRI antidepressants and tamoxifen. Acta Oncol 49:305–312
Dezentje VO, van Blijderveen NJ, Gelderblom H, Putter H, Van Herk-Sukel MP, Casparie MK et al (2010) Effect of concomitant CYP2D6 inhibitor use and tamoxifen adherence on breast cancer recurrence in early-stage breast cancer. J Clin Oncol 28:2423–2429
Siegelmann-Daniel N, Kurnik D, Lomnicky Y, Vesterman-Landes J, Katzir I, Bialik M et al. (2010) Potent CYP2D6 inhibiting drugs do not increase relapse rate in early breast cancer patients treated with adjuvant tamoxifen. Breast Cancer Res Treat. doi: 10.1007/s10549-010-1008-7
Holzman D (2009) Tamoxifen, antidepressants, and CYP2D6: the conundrum continues. J Natl Cancer Inst 101:1370–1371
Walley T, Mantgani A (1997) The UK General Practice Research Database. Lancet 350:1097–1099
Garcia Rodriguez LA, Perez GS (1998) Use of the UK General Practice Research Database for pharmacoepidemiology. Br J Clin Pharmacol 45:419–425
Jick H, Jick SS, Derby LE (1991) Validation of information recorded on general practitioner based computerised data resource in the United Kingdom. BMJ 302:766–768
Lawrenson R, Williams T, Farmer R (1999) Clinical information for research; the use of general practice databases. J Public Health Med 21:299–304
Lawrenson R, Todd JC, Leydon GM, Williams TJ, Farmer RD (2000) Validation of the diagnosis of venous thromboembolism in general practice database studies. Br J Clin Pharmacol 49:591–596
Jick SS, Kaye JA, Vasilakis-Scaramozza C, Garcia Rodriguez LA, Ruigomez A, Meier CR et al (2003) Validity of the general practice research database. Pharmacotherapy 23:686–689
Suissa S (2005) Novel approaches to pharmacoepidemiology study design and statistical analysis. In: Strom B (ed) pharmacoepidemiology, 4th edn. John Wiley & Sons, Chichester England, pp 811–829
Essebag V, Platt RW, Abrahamowicz M, Pilote L (2005) Comparison of nested case-control and survival analysis methodologies for analysis of time-dependent exposure. BMC Med Res Methodol 5:5
Essebag V, Genest J Jr, Suissa S, Pilote L (2003) The nested case-control study in cardiology. Am Heart J 146:581–590
de Vos D, Slee PH, Stevenson D, Briggs RJ (1992) Serum elimination half-life of tamoxifen and its metabolites in patients with advanced breast cancer. Cancer Chemother Pharmacol 31:76–78
Brewster DH, Thomson CS, Hole DJ, Black RJ, Stroner PL, Gillis CR (2001) Relation between socioeconomic status and tumour stage in patients with breast, colorectal, ovarian, and lung cancer: results from four national, population based studies. BMJ 322:830–831
Carroll DG, Kelley KW (2009) Use of antidepressants for management of hot flashes. Pharmacotherapy 29:1357–1374
Kelly CM, Juurlink DN, Gomes T, Duong-Hua M, Pritchard KI, Austin PC et al (2010) Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population based cohort study. BMJ 340:c693
Decensi A, Robertson C, Viale G, Pigatto F, Johansson H, Kisanga ER et al (2003) A randomized trial of low-dose tamoxifen on breast cancer proliferation and blood estrogenic biomarkers. J Natl Cancer Inst 95:779–790
Kisanga ER, Gjerde J, Guerrieri-Gonzaga A, Pigatto F, Pesci-Feltri A, Robertson C et al (2004) Tamoxifen and metabolite concentrations in serum and breast cancer tissue during three dose regimens in a randomized preoperative trial. Clin Cancer Res 10:2336–2343
Lash TL, Lien EA, Sorensen HT, Hamilton-Dutoit S (2009) Genotype-guided tamoxifen therapy: time to pause for reflection? Lancet Oncol 10:825–833
Huiart L, Dell’Aniello S, Suissa S (2009) Patterns of use of tamoxifen and aromatase inhibitors: a population-based observational study. J Clin Oncol 27:556
Acknowledgments
Dr. Laurent Azoulay is the recipient of a ‘Chercheur-Boursier’ Award from the Fonds de la recherche en santé du Québec. Dr. Samy Suissa is the recipient of a Distinguished Investigator Award from the Canadian Institutes of Health Research. This study was supported by the Canadian Institutes of Health Research and Canada Foundation for Innovation.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Azoulay, L., Dell’Aniello, S., Huiart, L. et al. Concurrent use of tamoxifen with CYP2D6 inhibitors and the risk of breast cancer recurrence. Breast Cancer Res Treat 126, 695–703 (2011). https://doi.org/10.1007/s10549-010-1162-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1162-y