Abstract
Breast cancer is the most common cancer in women worldwide, accounting for just over 1 million new cases annually. Population-based statistics show that globally, when compared to whites, women of African ancestry (AA) tend to have more aggressive breast cancers that present more frequently as estrogen receptor negative (ERneg) tumors. ERneg tumors fail to respond to current established targeted therapies, whether for treatment or prevention. Subsets of the ERneg phenotype include those that are also negative for the progesterone receptor (PR) and HER2; these are called “triple negative” (TN) breast cancers. TN tumors frequently have pathological characteristics resembling “basal-like” breast cancers. Hence, the latter two terms are often used interchangeably; yet, despite extensive overlap, they are not synonymous. The ERneg, TN, and basal-like phenotypic categories are important because they carry worse prognoses than ER-positive (ERpos) tumors, in addition to lacking obvious molecular targets, such as HER2 and the ER, for known therapies. Furthermore, among premenopausal women the three subsets occur more frequently in women of African descent compared to white women with breast cancer. The contribution of these three subtypes of poor-prognosis tumors to the higher breast cancer mortality in black women is the focus of this review. We will attempt to clarify some of the issues, including risk factors, in terms of their contribution to that component of health disparities that involves biological differences in breast cancer between women of AA and white women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most common cancer in women worldwide. Although less frequent in black women, breast cancer mortality is higher than in whites. Black women, particularly those who are premenopausal, more commonly present with estrogen receptor negative (ERneg) tumors and ERneg subtypes, including “triple negative” (TN) breast cancers, which are also negative for the progesterone receptor (PR) and HER2. Because TN tumors frequently resemble “basal-like” breast cancers pathologically, the two terms are often used interchangeably; despite extensive overlap, however, they are not synonymous. The ERneg, TN, and basal-like categories are more aggressive and carry worse prognoses than ER-positive (ERpos) tumors and lack obvious molecular targets, including HER2 and ER, for known therapies such as trastuzumab, tamoxifen, and aromatase inhibitors. These ERneg, poor-prognosis tumors, combined with adverse socioeconomic factors, contribute to the higher breast cancer mortality in women of African descent [1].
Epidemiology of breast cancer health disparities in women of African ancestry
Although breast cancer incidence is lower among women of African ancestry (AA, black women) than whites at ages >40 years, a crossover in age-adjusted incidence is evident in the higher rates in black women <40 years [2]. From 1992 to 2004 breast cancer incidence among US women <40 years was 16.8 versus 15.1 per 100,000 women-years for black versus white women, with even higher rates for AA women younger than 30 years [3]. Stage-for-stage breast cancer morbidity and mortality are higher for black than white women, with black women being far more likely to be diagnosed with aggressive breast cancer at a later-stage, less likely to receive stage-appropriate treatment, and more likely to have lower stage-for-stage survival rates [4, 5]. These observations suggest a composite of socioeconomic and biological disparities as potential causes for the worse outcomes. Socioeconomic status (SES) contributes to breast cancer disparities [6], seen in lower levels of mammographic screening together with higher overall mortality and 5-year case-specific probability of death among AA compared to white women [7]. SES is also reflected in residential segregation, with black women who are living in segregated areas being less likely to receive adequate breast cancer care, in turn contributing to disparity in treatment, although not mortality [8].
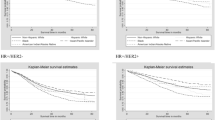
Yet, endogenous biological differences also contribute to breast cancer disparities. In two large adjuvant trials, AA and white women with comparable treatment-related variables differed in progression-free and overall survival [9], suggesting a biological role in the differential outcomes. In fact, tumors in the AA women had higher mitotic indices, more cyclin D1 over-expression, and higher grades [10–12]. Poor-prognosis breast cancers among premenopausal black women have high proliferation rates, poor differentiation, frequent P53 mutations, greater lymph node involvement, and larger tumor size [13–15]. In young AA women, ER/PR-negative tumors showed a significantly higher frequency of hypermethylation in four of five designated genes; cyclin D2 methylation was significantly associated with shorter survival [16].
Importantly, ERneg breast cancer and its pathological subtypes (see below) occur more frequently in AA women, particularly premenopausal AAs [9, 15]. These clinically aggressive ERneg subtypes are also more common in women of AA living in Africa, Great Britain, and the Caribbean [17–19].
Biology of ERneg subtypes of breast cancer
Breast cancer is a heterogeneous disease for which progressive clarification of subtypes has been based on evolving technology. Immunohistochemistry (IHC), a mainstay of classification, distinguishes ERpos from ERneg breast cancers, the latter being associated with greater aggressiveness and poorer prognosis. Subsets of ERneg cancers based on staining characteristics for three key breast cancer cell antigens, ER, PR, and HER2, include the much-discussed TN [20, 21]. IHC staining of cytokeratins (CKs) further sub-classifies tumors into clinically meaningful pathological subtypes [22–24]. “Basal-like” refers to the 8–20% of breast tumors that stain positively for high molecular weight CKs (CK5/6, CK14, and CK17) since these CKs are expressed in the basal/myoepithelial cells of normal breast ducts [21, 22, 25]. These are high-grade cancers with short overall and disease-free survival [24, 26–30] and are usually, but not always, TN [20, 28, 31]. Basal-like cancers often express HER1/EGFR [24, 28]. Variable expression of known basal-like markers makes their classification according to IHC staining characteristics somewhat inconsistent [24, 25, 30, 32–34]. Sporadic basal-like tumors share key features with BRCA1-mutation-associated hereditary breast cancers, including morphology, a frequent TN status, and expression of basal CKs, p53, P-cadherin, and HER1/EGFR. Conversely, breast cancers in women carrying BRCA1 mutations are frequently basal-like as well as TN [35–37].
More refined taxonomic categories of breast cancer are based on distinctions in gene expression at the messenger RNA (mRNA) level as assayed on gene-dense microarray chips. An early study used hierarchical clustering analysis to group breast tumor samples based on common expression of specific, “intrinsic” genes. Co-expressed genes often belonged to one of eight cellular pathways previously implicated in carcinogenesis [38]. Key IHC-based biomarkers, including ER-α and HER2, were represented on the mRNA array. In fact, clustering of breast cancer samples based on common expression profiles has revealed the most important discriminator of subtypes to be the ER status of the tumor [28]. Categorization of each sample in terms of its profile of eight gene expression clusters pointed to the correlation of a given expression profile with an established pathological type of breast cancer, as based on IHC staining [32, 38]: ERpos/luminal-like (subsequently divided into luminal A, B, and C [39]); basal-like (ERneg, CKs5/6, and 17-positive); HER2/Erb-B2-positive; and normal breast. ERneg samples comprise at least two subtypes, basal-like and HER2-positive.
Despite the detailed information embedded in microarray analysis, this technology is not yet suited to large population studies or routine clinical application, in part due to the expense of arrays and the difficulty of utilizing clinically available formalin-fixed, paraffin-embedded tissues for this purpose [29]. Furthermore, the equivalence of array-based and clinical pathologic criteria in distinguishing breast cancer subtypes has not been rigorously validated [30, 40–42], in part due to inherent heterogeneity of sub-types such as basal-like. The resulting inconsistencies are compounded by the interchangeable use of the terms “basal-like” and TN [21, 43, 44]. Although they frequently share histopathological, clinical, and demographic features [21, 29], including absence of expression of ER, PR, and HER2, the two terms are not synonymous. Like basal-like tumors, the 10–17% of breast cancers that are TN are high-grade invasive ductal of no special type, metaplastic carcinomas, or medullary cancers. Both types express HER1/EGFR in up to 66% of cases [21], both behave aggressively, often presenting as interval cancers, both types are ERneg and HER2-negative and hence, lack tailored therapies, and both are more prevalent in AA and young (<50 years) women. However, differences between the two types are evident in the 15–54% of basal-like cancers that express at least one of the markers, ER or HER2 (“double negative”) [21, 29, 45]; conversely, only 85% of tumors that are ERneg and Her2-negative are basal-like by expression arrays. In addition, the “basal” CKs and HER1/EGFR, key to defining a tumor as basal-like by IHC, are expressed in only 46–90% of TN tumors [21, 44, 46, 47].
Connecting ERneg breast cancer biology to racial disparities
The evidence for a higher incidence of ERneg [48], particularly TN, breast cancer, among AA women dovetails nicely with the potential of expression arrays to delineate breast cancer subtypes in an increasingly precise manner. To surmount the technical challenges to reliable application of microarray analysis to large-scale studies, the complex mRNA expression clusters have been distilled into equivalent, or “surrogate”, IHC markers [28, 30, 44, 49]. A panel of four antibodies specific for ER, HER1, HER2, and CK5/6, has yielded a useful set of IHC subtype definitions (IHC surrogates for microarray-based definitions): basal-like (ERneg, PR-negative, HER2-negative, CK5/6-positive, and/or HER1-positive); HER2-positive/ERneg (HER2-positive, ERneg, PR-negative); luminal A (ERpos and/or PR-positive, HER2-negative); and luminal B (ERpos and/or PR-positive, HER2-positive). A surrogate IHC antibody panel accurately identified 21 tumors determined as basal-like based on their gene expression profiles and was successfully applied in large-scale fashion to tumors from 930 patients to show association between low survival and basal-like CK expression [28]. In the Carolina Breast Cancer Study (CBCS) population [13, 50], the antibody panel revealed that patients with the basal-like tumor subtype were more likely to be AA. These data are consistent with the previously discussed evidence for excess ERneg breast cancers among AA women [48]. Although the overall study population had a 20% prevalence of basal-like tumors, the AA patients had a 26% prevalence compared to 16% in non-AAs. The excess of basal-like tumors in AAs was restricted to premenopausal women (basal-like comprising 27.2% of AA premenopausal versus 16% of AA postmenopausal breast cancers) [50].
In women of AA, reproductive factors, including multiparity, younger age at menarche and early age at first pregnancy have been shown to protect against ER/PR-positive breast cancer but may be positively associated with ER/PR-negative tumors [50–52]. A meta-analysis of epidemiologic studies reported decreased risk of both receptor subtypes in association with breastfeeding and late age at menarche, the latter association being more significant for ER/PR-positive breast cancer [53]. Breastfeeding ≥6 months versus never breastfeeding were also protective for TN disease [54]. In their application of IHC surrogate markers for breast cancer subtypes to the CBCS, Millikan et al. [50] showed that breastfeeding was protective for basal-like breast cancer, with significant trends for lifetime duration of lactation, number of children breastfed, and average number of months’ breastfeeding per child. Both basal-like breast cancer and risk factors for this subtype were more prevalent among premenopausal AA than white women [50]. The authors estimated that encouraging breastfeeding and reducing abdominal adiposity could prevent approximately 68% of basal-like breast cancers.
Low SES was associated with basal-like cancers, late-stage at diagnosis and poor survival in a number of studies. Lower income correlated with increased risk of late-stage breast cancer, whereas higher educational attainment tracked with higher rates of breast cancer [55]. Regarding ERneg tumors, a few studies revealed that low SES and experiencing social deprivation placed women at increased risk for ERneg breast cancer risk [56, 57]. TN breast cancer was associated not only with race/ethnicity of African descent but also with having a lower SES [58]. For example, data from the California Cancer Registry showed that women with TN tumors were significantly more likely to be of African and Hispanic descent as well as to live in socioeconomically deprived areas [45, 58, 59].
SES may actually operate through lifestyle risk factors in influencing ERneg breast cancer. Dietary and physical activity behaviors (Tables 1, 2), although associated with breast cancer susceptibility, have not been extensively studied in relation to ER status. Healthy diets [60–62], high phytoestrogen intake [63–65] high folate intake [66, 67], fiber intake [68, 69], and possible calcium intake [70] may protect against ERneg tumors. The protective effect of folate occurs specifically in women consuming alcohol [71]. Also, postmenopausal women consuming ≥1,272 dietary folate equivalents of total folate over 10 years appear to derive a greater benefit for ERneg than ERpos breast cancers [67]. Although vitamin D had a protective effect on ERneg breast cancers in some studies, this is not always significant; in other studies the benefit existed only for ERpos cancers [72, 73]. However, a small case study of 91 women with breast cancer found that low serum vitamin D level and vitamin D deficiency were associated with increased risk for TN tumors [74]. Strenuous to moderate levels of physical activity may lower ERneg breast cancer risk [75, 76], with exercising during adolescence and within the last 10 years being associated with decreased risk of ER/PR-negative breast cancer in both premenopausal and postmenopausal women [77]. However, Bardia et al. [78] did not find a significant association between physical activity and ERneg breast cancer risk; rather, this study showed an association with ERpos breast cancer risk. In one study abdominal adiposity was associated with increased risk of basal-like breast cancer [50], while others showed that obese women with ERneg disease had reduced disease-free survival and increased mortality [79, 80]. Although prevalent among pre- and postmenopausal AA women, obesity has not been implicated as a risk factor for ERneg tumors in this population.
Therapeutic interventions in ERneg breast cancer
A need exists for therapies targeted to the ERneg subtypes, especially in women of African descent who are at elevated risk of developing these aggressive cancers. Animal models that mimic attributes of ERneg breast cancer have been used to identify agents or regimens to treat and prevent these cancers. In the MMTV-Neu (mouse HER2) mouse model for ERneg, PRneg, Neu-positive breast cancer, RXR agonists and EGFR1/2 inhibitors showed preventive activity [83, 84]. Human basal-like/TN signatures are approximated in tumors in (1) SV40-T-antigen-expressing and (2) BRCA1-knockout mouse models [85]. The latter association is expected, given the prevalence of basal-like/TN features among human BRCA1-mutation-associated breast cancers [35–37], although only 40% of mouse BRCA1-knockout tumors resemble human TN tumors by microarray analysis. Preventive protocols in this ERneg model have shown that: (1) early ovariectomy inhibits later tumor formation; (2) tamoxifen is ineffective; (3) early treatment with a HER1/EGFR inhibitor decreases tumor formation; and (4) a high affinity poly(adenosine diphosphate [ADP]-ribose) polymerase (PARP) inhibitor is effective and specific in preventing BRCA1-associated lesions [86–88]. T-antigen mouse model tumors resemble human basal-like breast cancers, with alterations in P53 and RB [89]. The ornithine decarboxylase inhibitor difluoromethyl ornithine (DFMO) and certain RXR agonists (Targretin) prevent T-antigen-driven tumor development [90, 91]. Also, certain cytotoxic chemotherapy recapitulates activity in human basal-like/TN tumors, where two-thirds respond, with 40% giving a long-term response (>10 years) (Perou, personal communication). This application of animal models to the search for therapy targeting ERneg breast cancer subtypes provides important leads to drug interventions in clinical trials in humans.
The juncture where ERneg breast cancer biology meets health disparities presents a major public health challenge. Given the disproportionate burden of ERneg and basal-like/TN tumors among AA women, the lack of directed interventions against ERneg breast cancers is especially problematic. Basal-like/TN breast cancers lack established targets like ER or HER2 that can serve as a focus for treatment; therefore, the main goal in developing treatment is to move away from empirical chemotherapy toward drugs with highly specific activity against these aggressive ERneg subtypes. Traditionally, anthracycline-based and/or cisplatin-based regimens have been selected for first-line therapy, although with mixed results. Gene expression studies are refining our understanding of molecular pathways that are clinically important in subsets of breast cancers without established targets [39, 92]. Such biomolecular characterization of ERneg tumors provides the basis for clinical trials designed to characterize drug effects on specific targets and correlate such effects with clinical and tumor biomarker responses. These trials offer an invaluable resource for improving ERneg breast cancer treatment and prevention. The inclusion of minority women in ERneg target identification trials is critical.
Querying ClinicalTrials.gov with two search terms, “breast cancer” and “ERneg”, identifies about 20 trials that are studying a handful of promising molecular targets for ERneg breast cancer. These targets (Table 3) include EGFR (erlotinib, cetuximab), defective DNA repair (platinum), c-Kit (dasatinib), VEGF (bevacizumab, sunitinib), Chk1 (gemcitabine), and PARP (BSI-201, AZD2281). PARP inhibitors are likely to be useful, particularly in BRCA-mutation carriers [93]. However, a theoretical rationale suggests that PARP inhibitors should work more broadly in ERneg breast cancer even in women who are not mutation carriers [94]. Specifically with regard to breast cancer prevention in women at high risk for ERneg breast cancer, several trials are currently investigating agents such as green tea, lapatinib, PARP inhibitors, polyphenon E, targretin, 9cUAB30, and atorvastatin.
Discussion and future directions
The intertwined mix of factors that contribute to cancer health disparities seen in complex diseases such as cancer has been the subject of much discussion [95]. An especially controversial component of this discussion relates to the relative contribution of endogenous/biological variables that characterize a given group, as opposed to exogenous factors, including SES, cultural and behavioral characteristics. Among endogenous contributors, genetic/genomic modifications, such as specific rare mutations in established cancer-associated genes as well as the clustering of common genomic polymorphisms in selected populations, are being investigated for their role in cancer risk in these groups [96–99].
In addition to genetic predisposition to cancer, biologic factors include somatic features of cancer, such as subsets of common cancers that are disproportionately represented in specific racial groups. Our review addresses one such example, ERneg breast cancers and their TN/basal-like subsets, both distinguished by definitive gene expression profiles. These occur with higher frequency in women of AA who have breast cancer, particularly those who are premenopausal. Because of the worse prognosis of these subtypes, they undoubtedly contribute to the worse outcomes observed in this population. The question remains, however, whether and to what extent the increased propensity toward these aggressive cancers is biologically innate, i.e., genetically determined, and to what extent these cancers are byproducts of exogenous factors, including components of SES, culture, and behavior. The argument has been made that the excessive concentration of aggressive cancer subtypes in particular populations, such as the ERneg breast cancers in AA women, can be explained by epigenetic, as opposed to genetic, factors [95]. Epigenetic factors include molecular mechanisms that regulate gene expression, offering a venue through which the effect of the environment is mediated. Thus, the malleability of epigenetic changes as they interact with factors such as diet [100, 101] and physical activity [102] might explain differential cancer presentations and outcomes in specific racial groups. Yet, epigenetic modifications cannot be completely extricated from genetic influences. Apart from the specialized case of the <1% of genes that are imprinted, recent evidence points to the heritability of more generalized epigenetic modifications, both DNA methylation and histone modifications [103]. Therefore, future research must address the interplay between SES, health behaviors and both genetic and epigenetic factors, as they jointly contribute to the worse cancer presentations and outcomes in individual racial groups.
More in-depth research into the SES and health behavioral components of this interplay will be necessary in order to disentangle socioeconomic disparities from race/ethnicity and from genetic factors with regard to their contributions to breast tumor characteristics. This effort requires prospective cohort studies involving large numbers of racially/ethnically diverse women from whom carefully annotated data regarding tumor subtypes are collected. The heterogeneity of breast cancer, especially as regards racially diverse populations, will feed into cancer prevention strategies. Similarly, deeper understanding of gene-environment interactions as they relate to breast cancer risk and prognosis will allow clinicians to address the worse outcomes evident in patients from specific populations.
The National Healthcare Disparities Report by the Agency for Healthcare Research and Quality (AHRQ) detailed progress that has been made in eliminating health disparities and identified gaps in quality and access to care [104]. This detailed portrait of cancer health disparities indicates that the cause is multifactorial, especially in women of AA. Experts have debated what factor(s) should be targeted to achieve the greatest impact in eliminating disparities: should the target be socioeconomic, race, biology, access, substandard care, lack of insurance, higher stage of disease at diagnosis, or other not so well defined factors? A panel of experts convened by the American Society of Clinical Oncology’s (ASCO) Health Disparities Advisory Group debated these issues [105], and ASCO issued a policy statement pointing to low income, lack of insurance, and access to care as playing a major role in health disparities [106]. Importantly, the Institute of Medicine Report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare, concluded that racial and ethnic disparities continue to persist even after controlling for income and insurance status [107]. Clinical studies have shown that even in equal access systems or where identical care is given, minorities continue to have worse outcomes in organ specific cancers that are hormonally influenced, e.g., breast, prostate, and ovarian cancers [9, 108, 109]. Why these hormonally sensitive cancers, and not others, add another component to the worse outcomes is not obvious and presents an area of health disparities that is ripe for investigation.
The ERneg breast cancers and their TN/basal-like subsets constitute a concrete biological class that is overrepresented in AA women. Therefore, a major part of the agenda to address health disparities as they relate to breast cancer in AA women must include studies of this aggressive subset of breast cancers. In addition to the epidemiologic investigations just discussed, confirmation of targeted drug activity in the treatment setting via appropriately designed clinical trials will spawn a new generation of prevention trials where the putative targets of drug action can be confirmed and monitored. The knowledge from this effort should not only increase the opportunity to intervene against ERneg breast cancer for prevention and treatment, but also provide the personalized approach that will be beneficial in addressing the deficit in breast cancer health care outcomes that are experienced by women of AA and other minority groups.
In summary, more than one factor needs to be considered in the effort to eliminate breast cancer health disparities. Additional research to address interactions among known factors as well as interactions with other undiscovered factors that influence cancer disparities, both intrinsic/endogenous and extrinsic/exogenous, is necessary.
References
Browne D (2008) Public Health Democracy: U.S. and Global Health Disparities in Breast Cancer. Woodrow Wilson International Center for Scholars, Global Health Initiative, Washington, DC www.wilsoncenter.org/globalhealth
Anderson WF, Rosenberg PS, Menashe I, Mitani A, Pfeiffer RM (2008) Age-related crossover in breast cancer incidence rates between black and white ethnic groups. J Natl Cancer Inst 100:1804–1814. doi:10.1093/jnci/djn411
Brinton LA, Sherman ME, Carreon JD, Anderson WF (2008) Recent trends in breast cancer among younger women in the United States. J Natl Cancer Inst 100:1643–1648. doi:10.1093/jnci/djn344
Morris GJ, Mitchell EP (2008) Higher incidence of aggressive breast cancers in African–American women: a review. J Natl Med Assoc 100:698–702
McBride R, Hershman D, Tsai WY, Jacobson JS, Grann V, Neugut AI (2007) Within-stage racial differences in tumor size and number of positive lymph nodes in women with breast cancer. Cancer 110:1201–1208. doi:10.1002/cncr.22884
ACS (2009) Cancer facts & figures 2009. American Cancer Society, Atlanta, GA. [http://www.cancer.org/downloads/STT/cffaa_2009-2010.pdf]
Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman MC (2009) Trends in area-socioeconomic and race-ethnic disparities in breast cancer incidence, stage at diagnosis, screening, mortality, and survival among women ages 50 years and over (1987–2005). Cancer Epidemiol Biomarkers Prev 18:121–131. doi:10.1158/1055-9965.EPI-08-0679
Haas JS, Earle CC, Orav JE, Brawarsky P, Keohane M, Neville BA, Williams DR (2008) Racial segregation and disparities in breast cancer care and mortality. Cancer 113:2166–2172. doi:10.1002/cncr.23828
Hershman DL, Unger JM, Barlow WE, Hutchins LF et al (2009) Treatment quality and outcomes of African American versus white breast cancer patients: retrospective analysis of Southwest oncology studies S8814/S8897. J Clin Oncol 27:2157–2162. doi:10.1200/JCO.2008.19.1163
Porter PL, Garcia R, Moe R, Corwin DJ, Gown AM (1991) C-erbB-2 oncogene protein in in situ and invasive lobular breast neoplasia. Cancer 68:331–334
Porter PL, Lund MJ, Lin MG, Yuan X et al (2004) Racial differences in the expression of cell cycle-regulatory proteins in breast carcinoma. Cancer 100:2533–2542. doi:10.1002/cncr.20279
Amend K, Hicks D, Ambrosone CB (2006) Breast cancer in African–American women: differences in tumor biology from European–American women. Cancer Res 66:8327–8330. doi:10.1158/0008-5472.CAN-06-1927
Carey LA, Perou CM, Livasy CA, Dressler LG et al (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502. doi:10.1001/jama.295.21.2492
Ihemelandu CU, Leffall LD Jr, Dewitty RL, Naab TJ et al (2007) Molecular breast cancer subtypes in premenopausal African–American women, tumor biologic factors and clinical outcome. Ann Surg Oncol 14:2994–3003. doi:10.1245/s10434-007-9477-6
Ihemelandu CU, Naab TJ, Mezghebe HM, Makambi KH et al (2008) Basal cell-like (triple-negative) breast cancer, a predictor of distant metastasis in African American women. Am J Surg 195:153–158. doi:10.1016/j.amjsurg.2007.09.033
Mehrotra J, Ganpat MM, Kanaan Y, Fackler MJ et al (2004) Estrogen receptor/progesterone receptor-negative breast cancers of young African–American women have a higher frequency of methylation of multiple genes than those of Caucasian women. Clin Cancer Res 10:2052–2057
Nalwoga H, Arnes JB, Wabinga H, Akslen LA (2007) Frequency of the basal-like phenotype in African breast cancer. APMIS 115:1391–1399. doi:10.1111/j.1600-0463.2007.00862.x
Bowen RL, Duffy SW, Ryan DA, Hart IR, Jones JL (2008) Early onset of breast cancer in a group of British black women. Br J Cancer 98:277–281. doi:10.1038/sj.bjc.6604174
Hennis AJ, Hambleton IR, Wu SY, Leske MC, Nemesure B (2009) Breast cancer incidence and mortality in a Caribbean population: comparisons with African–Americans. Int J Cancer 124:429–433. doi:10.1002/ijc.23889
Schneider BP, Winer EP, Foulkes WD, Garber J et al (2008) Triple-negative breast cancer: risk factors to potential targets. Clin Cancer Res 14:8010–8018. doi:10.1158/1078-0432.CCR-08-1208
Reis-Filho JS, Tutt AN (2008) Triple negative tumours: a critical review. Histopathology 52:108–118. doi:10.1111/j.1365-2559.2007.02889.x
Nagle RB, Bocker W, Davis JR, Heid HW, Kaufmann M, Lucas DO, Jarasch ED (1986) Characterization of breast carcinomas by two monoclonal antibodies distinguishing myoepithelial from luminal epithelial cells. J Histochem Cytochem 34:869–881
Dairkee S, Heid HW (1993) Cytokeratin profile of immunomagnetically separated epithelial subsets of the human mammary gland. In Vitro Cell Dev Biol Anim 29A:427–432
Gusterson BA, Ross DT, Heath VJ, Stein T (2005) Basal cytokeratins and their relationship to the cellular origin and functional classification of breast cancer. Breast Cancer Res 7:143–148. doi:10.1186/bcr1041
Fulford LG, Easton DF, Reis-Filho JS, Sofronis A, Gillett CE, Lakhani SR, Hanby A (2006) Specific morphological features predictive for the basal phenotype in grade 3 invasive ductal carcinoma of breast. Histopathology 49:22–34. doi:10.1111/j.1365-2559.2006.02453.x
Moll R (1998) Cytokeratins as markers of differentiation in the diagnosis of epithelial tumors. Subcell Biochem 31:205–262
van de Rijn M, Perou CM, Tibshirani R, Haas P et al (2002) Expression of cytokeratins 17 and 5 identifies a group of breast carcinomas with poor clinical outcome. Am J Pathol 161:1991–1996
Nielsen TO, Hsu FD, Jensen K, Cheang M et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5374. doi:10.1158/1078-0432.CCR-04-0220
Rakha EA, Reis-Filho JS, Ellis IO (2008) Basal-like breast cancer: a critical review. J Clin Oncol 26:2568–2581. doi:10.1200/JCO.2007.13.1748
Livasy CA, Karaca G, Nanda R, Tretiakova MS, Olopade OI, Moore DT, Perou CM (2006) Phenotypic evaluation of the basal-like subtype of invasive breast carcinoma. Mod Pathol 19:264–271. doi:10.1038/modpathol.3800528
Cleator S, Heller W, Coombes RC (2007) Triple-negative breast cancer: therapeutic options. Lancet Oncol 8:235–244. doi:10.1016/S1470-2045(07)70074-8
Sotiriou C, Pusztai L (2009) Gene-expression signatures in breast cancer. N Engl J Med 360:790–800. doi:10.1056/NEJMra0801289
Prat A, Perou CM (2009) Mammary development meets cancer genomics. Nat Med 15:842–844. doi:10.1038/nm0809-842
Lim E, Vaillant F, Wu D, Forrest NC et al (2009) Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nat Med 15:907–913. doi:10.1038/nm.2000
Foulkes WD, Stefansson IM, Chappuis PO, Begin LR et al (2003) Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst 95:1482–1485
Lakhani SR, Reis-Filho JS, Fulford L, Penault-Llorca F et al (2005) Prediction of BRCA1 status in patients with breast cancer using estrogen receptor and basal phenotype. Clin Cancer Res 11:5175–5180. doi:10.1158/1078-0432.CCR-04-2424
Atchley DP, Albarracin CT, Lopez A, Valero V et al (2008) Clinical and pathologic characteristics of patients with BRCA-positive and BRCA-negative breast cancer. J Clin Oncol 26:4282–4288. doi:10.1200/JCO.2008.16.6231
Perou CM, Sorlie T, Eisen MB, van de Rijn M et al (2000) Molecular portraits of human breast tumours. Nature 406:747–752. doi:10.1038/35021093
Sorlie T, Perou CM, Tibshirani R, Aas T et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874. doi:10.1073/pnas.191367098
Foekens JA, Atkins D, Zhang Y, Sweep FC et al (2006) Multicenter validation of a gene expression-based prognostic signature in lymph node-negative primary breast cancer. J Clin Oncol 24:1665–1671. doi:10.1200/JCO.2005.03.9115
Tavtigian SV, Pierotti MA, Borresen-Dale AL (2006) International Agency for Research on Cancer workshop on ‘Expression array analyses in breast cancer taxonomy’. Breast Cancer Res 8:303. doi:10.1186/bcr1609
Parker JS, Mullins M, Cheang MC, Leung S et al (2009) Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol 27:1160–1167. doi:10.1200/JCO.2008.18.1370
Bidard FC, Conforti R, Boulet T, Michiels S, Delaloge S, Andre F (2007) Does triple-negative phenotype accurately identify basal-like tumour? An immunohistochemical analysis based on 143 ‘triple-negative’ breast cancers. Ann Oncol 18:1285–1286. doi:10.1093/annonc/mdm360
Cheang MC, Voduc D, Bajdik C, Leung S et al (2008) Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res 14:1368–1376. doi:10.1158/1078-0432.CCR-07-1658
Brown M, Tsodikov A, Bauer KR, Parise CA, Caggiano V (2008) The role of human epidermal growth factor receptor 2 in the survival of women with estrogen and progesterone receptor-negative, invasive breast cancer: the California Cancer Registry, 1999–2004. Cancer 112:737–747. doi:10.1002/cncr.23243
Ross JS, Hatzis C, Symmans WF, Pusztai L, Hortobagyi GN (2008) Commercialized multigene predictors of clinical outcome for breast cancer. Oncologist 13:477–493. doi:10.1634/theoncologist.2007-0248
Yamamoto Y, Ibusuki M, Nakano M, Kawasoe T, Hiki R, Iwase H (2009) Clinical significance of basal-like subtype in triple-negative breast cancer. Breast Cancer 16:260–267. doi:10.1007/s12282-009-0150-8
Chlebowski RT, Chen Z, Anderson GL, Rohan T et al (2005) Ethnicity and breast cancer: factors influencing differences in incidence and outcome. J Natl Cancer Inst 97:439–448. doi:10.1093/jnci/dji064
Jumppanen M, Gruvberger-Saal S, Kauraniemi P, Tanner M et al (2007) Basal-like phenotype is not associated with patient survival in estrogen-receptor-negative breast cancers. Breast Cancer Res 9:R16. doi:10.1186/bcr1649
Millikan RC, Newman B, Tse CK, Moorman PG et al (2008) Epidemiology of basal-like breast cancer. Breast Cancer Res Treat 109:123–139. doi:10.1007/s10549-007-9632-6
Ursin G, Bernstein L, Lord SJ, Karim R et al (2005) Reproductive factors and subtypes of breast cancer defined by hormone receptor and histology. Br J Cancer 93:364–371. doi:10.1038/sj.bjc.6602712
Yang XR, Sherman ME, Rimm DL, Lissowska J et al (2007) Differences in risk factors for breast cancer molecular subtypes in a population-based study. Cancer Epidemiol Biomarkers Prev 16:439–443. doi:10.1158/1055-9965.EPI-06-0806
Ma H, Bernstein L, Pike MC, Ursin G (2006) Reproductive factors and breast cancer risk according to joint estrogen and progesterone receptor status: a meta-analysis of epidemiological studies. Breast Cancer Res 8:R43. doi:10.1186/bcr1525
Phipps AI, Malone KE, Porter PL, Daling JR, Li CI (2008) Reproductive and hormonal risk factors for postmenopausal luminal, HER-2-overexpressing, and triple-negative breast cancer. Cancer 113:1521–1526. doi:10.1002/cncr.23786
Clegg LX, Reichman ME, Miller BA, Hankey BF et al (2009) Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 20:417–435. doi:10.1007/s10552-008-9256-0
Gordon NH (1995) Association of education and income with estrogen receptor status in primary breast cancer. Am J Epidemiol 142:796–803
Taylor A, Cheng KK (2003) Social deprivation and breast cancer. J Public Health Med 25:228–233
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer registry. Cancer 109:1721–1728. doi:10.1002/cncr.22618
Parise CA, Bauer KR, Brown MM, Caggiano V (2009) Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999–2004. Breast J 15:593–602. doi:10.1111/j.1524-4741.2009.00822.x
Fung TT, Hu FB, Holmes MD, Rosner BA, Hunter DJ, Colditz GA, Willett WC (2005) Dietary patterns and the risk of postmenopausal breast cancer. Int J Cancer 116:116–121. doi:10.1002/ijc.20999
Fung TT, Hu FB, McCullough ML, Newby PK, Willett WC, Holmes MD (2006) Diet quality is associated with the risk of estrogen receptor-negative breast cancer in postmenopausal women. J Nutr 136:466–472
Agurs-Collins T, Rosenberg L, Makambi K, Palmer JR, Adams-Campbell L (2009) Dietary patterns and breast cancer risk in women participating in the Black Women’s Health Study. Am J Clin Nutr 90:621–628. doi:10.3945/ajcn.2009.27666
Touillaud MS, Pillow PC, Jakovljevic J, Bondy ML, Singletary SE, Li D, Chang S (2005) Effect of dietary intake of phytoestrogens on estrogen receptor status in premenopausal women with breast cancer. Nutr Cancer 51:162–169. doi:10.1207/s15327914nc5102_6
McCann SE, Kulkarni S, Trevisan M, Vito D et al (2006) Dietary lignan intakes and risk of breast cancer by tumor estrogen receptor status. Breast Cancer Res Treat 99:309–311. doi:10.1007/s10549-006-9196-x
Zhang M, Yang H, Holman CD (2009) Dietary intake of isoflavones and breast cancer risk by estrogen and progesterone receptor status. Breast Cancer Res Treat 118:553–563
Zhang SM, Hankinson SE, Hunter DJ, Giovannucci EL, Colditz GA, Willett WC (2005) Folate intake and risk of breast cancer characterized by hormone receptor status. Cancer Epidemiol Biomarkers Prev 14:2004–2008. doi:10.1158/1055-9965.EPI-05-0083
Maruti SS, Ulrich CM, White E (2009) Folate and one-carbon metabolism nutrients from supplements and diet in relation to breast cancer risk. Am J Clin Nutr 89:624–633. doi:10.3945/ajcn.2008.26568
Giles GG, Simpson JA, English DR, Hodge AM, Gertig DM, Macinnis RJ, Hopper JL (2006) Dietary carbohydrate, fibre, glycaemic index, glycaemic load and the risk of postmenopausal breast cancer. Int J Cancer 118:1843–1847. doi:10.1002/ijc.21548
Park Y, Brinton LA, Subar AF, Hollenbeck A, Schatzkin A (2009) Dietary fiber intake and risk of breast cancer in postmenopausal women: the National Institutes of Health-AARP Diet and Health Study. Am J Clin Nutr 90:664–671. doi:10.3945/ajcn.2009.27758
Larsson SC, Bergkvist L, Wolk A (2009) Long-term dietary calcium intake and breast cancer risk in a prospective cohort of women. Am J Clin Nutr 89:277–282. doi:10.3945/ajcn.2008.26704
Sellers TA, Vierkant RA, Cerhan JR, Gapstur SM et al (2002) Interaction of dietary folate intake, alcohol, and risk of hormone receptor-defined breast cancer in a prospective study of postmenopausal women. Cancer Epidemiol Biomarkers Prev 11:1104–1107
Robien K, Cutler GJ, Lazovich D (2007) Vitamin D intake and breast cancer risk in postmenopausal women: the Iowa Women’s Health Study. Cancer Causes Control 18:775–782. doi:10.1007/s10552-007-9020-x
Blackmore KM, Lesosky M, Barnett H, Raboud JM, Vieth R, Knight JA (2008) Vitamin D from dietary intake and sunlight exposure and the risk of hormone-receptor-defined breast cancer. Am J Epidemiol 168:915–924. doi:10.1093/aje/kwn198
Rainville C, Khan Y, Tisman G (2009) Triple negative breast cancer patients presenting with low serum vitamin D levels: a case series. Cases J 2:8390. doi:10.4076/1757-1626-2-8390
Dallal CM, Sullivan-Halley J, Ross RK, Wang Y et al (2007) Long-term recreational physical activity and risk of invasive and in situ breast cancer: the California teachers study. Arch Intern Med 167:408–415. doi:10.1001/archinte.167.4.408
Peters TM, Schatzkin A, Gierach GL, Moore SC et al (2009) Physical activity and postmenopausal breast cancer risk in the NIH-AARP diet and health study. Cancer Epidemiol Biomarkers Prev 18:289–296. doi:10.1158/1055-9965.EPI-08-0768
Adams SA, Matthews CE, Hebert JR, Moore CG et al (2006) Association of physical activity with hormone receptor status: the Shanghai Breast Cancer Study. Cancer Epidemiol Biomarkers Prev 15:1170–1178. doi:10.1158/1055-9965.EPI-05-0993
Bardia A, Hartmann LC, Vachon CM, Vierkant RA et al (2006) Recreational physical activity and risk of postmenopausal breast cancer based on hormone receptor status. Arch Intern Med 166:2478–2483. doi:10.1001/archinte.166.22.2478
Berclaz G, Li S, Price KN, Coates AS et al (2004) Body mass index as a prognostic feature in operable breast cancer: the International Breast Cancer Study Group experience. Ann Oncol 15:875–884
Dignam JJ, Wieand K, Johnson KA, Raich P, Anderson SJ, Somkin C, Wickerham DL (2006) Effects of obesity and race on prognosis in lymph node-negative, estrogen receptor-negative breast cancer. Breast Cancer Res Treat 97:245–254. doi:10.1007/s10549-005-9118-3
Olsen A, Tjonneland A, Thomsen BL, Loft S et al (2003) Fruits and vegetables intake differentially affects estrogen receptor negative and positive breast cancer incidence rates. J Nutr 133:2342–2347
Enger SM, Ross RK, Paganini-Hill A, Carpenter CL, Bernstein L (2000) Body size, physical activity, and breast cancer hormone receptor status: results from two case-control studies. Cancer Epidemiol Biomarkers Prev 9:681–687
Lu C, Speers C, Zhang Y, Xu X et al (2003) Effect of epidermal growth factor receptor inhibitor on development of estrogen receptor-negative mammary tumors. J Natl Cancer Inst 95:1825–1833
Wu K, Zhang Y, Xu XC, Hill J et al (2002) The retinoid X receptor-selective retinoid, LGD1069, prevents the development of estrogen receptor-negative mammary tumors in transgenic mice. Cancer Res 62:6376–6380
Herschkowitz JI, Simin K, Weigman VJ, Mikaelian I et al (2007) Identification of conserved gene expression features between murine mammary carcinoma models and human breast tumors. Genome Biol 8:R76. doi:10.1186/gb-2007-8-5-r76
Bachelier R, Xu X, Li C, Qiao W, Furth PA, Lubet RA, Deng CX (2005) Effect of bilateral oophorectomy on mammary tumor formation in BRCA1 mutant mice. Oncol Rep 14:1117–1120
Jones LP, Li M, Halama ED, Ma Y et al (2005) Promotion of mammary cancer development by tamoxifen in a mouse model of Brca1-mutation-related breast cancer. Oncogene 24:3554–3562. doi:10.1038/sj.onc.1208426
Farmer H, McCabe N, Lord CJ, Tutt AN et al (2005) Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434:917–921. doi:10.1038/nature03445
Herschkowitz JI, He X, Fan C, Perou CM (2008) The functional loss of the retinoblastoma tumour suppressor is a common event in basal-like and luminal B breast carcinomas. Breast Cancer Res 10:R75. doi:10.1186/bcr2142
Green JE, Shibata MA, Shibata E, Moon RC, Anver MR, Kelloff G, Lubet R (2001) 2-Difluoromethylornithine and dehydroepiandrosterone inhibit mammary tumor progression but not mammary or prostate tumor initiation in C3(1)/SV40 T/t-antigen transgenic mice. Cancer Res 61:7449–7455
Wu K, Kim HT, Rodriquez JL, Hilsenbeck SG et al (2002) Suppression of mammary tumorigenesis in transgenic mice by the RXR-selective retinoid, LGD1069. Cancer Epidemiol Biomarkers Prev 11:467–474
Carey LA, Dees EC, Sawyer L, Gatti L et al (2007) The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 13:2329–2334. doi:10.1158/1078-0432.CCR-06-1109
Fong PC, Boss DS, Yap TA, Tutt A et al (2009) Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med 361:123–134. doi:10.1056/NEJMoa0900212
Natrajan R, Weigelt B, Mackay A, Geyer FC et al (2009) An integrative genomic and transcriptomic analysis reveals molecular pathways and networks regulated by copy number aberrations in basal-like, HER2 and luminal cancers. Breast Cancer Res Treat. doi: 10.1007/s10549-009-0501-3
Kagawa-Singer M, Dadia AV, Yu MC, Surbone A (2010) Cancer, culture, and health disparities: time to chart a new course? CA Cancer J Clin 60:12–39. doi:10.3322/caac.20051
Olopade OI, Fackenthal JD, Dunston G, Tainsky MA, Collins F, Whitfield-Broome C (2003) Breast cancer genetics in African Americans. Cancer 97:236–245. doi:10.1002/cncr.11019
Nanda R, Schumm LP, Cummings S, Fackenthal JD et al (2005) Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA 294:1925–1933. doi:10.1001/jama.294.15.1925
Caulfield T, Fullerton SM, Ali-Khan SE, Arbour L et al (2009) Race and ancestry in biomedical research: exploring the challenges. Genome Med 1:8. doi:10.1186/gm8
Giri VN, Egleston B, Ruth K, Uzzo RG et al (2009) Race, genetic West African ancestry, and prostate cancer prediction by prostate-specific antigen in prospectively screened high-risk men. Cancer Prev Res (Phila Pa) 2:244–250. doi:10.1158/1940-6207.CAPR-08-0150
Ross SA (2003) Diet and DNA methylation interactions in cancer prevention. Ann NY Acad Sci 983:197–207
Ross SA, Dwyer J, Umar A, Kagan J, Verma M, Van Bemmel DM, Dunn BK (2008) Introduction: diet, epigenetic events and cancer prevention. Nutr Rev 66(Suppl 1):S1–S6. doi:10.1111/j.1753-4887.2008.00055.x
Levin BE (2008) Epigenetic influences on food intake and physical activity level: review of animal studies. Obesity (Silver Spring) 16(Suppl 3):S51–S54. doi:10.1038/oby.2008.518
Lee MP, Dunn BK (2008) Influence of genetic inheritance on global epigenetic states and cancer risk prediction with DNA methylation signature: challenges in technology and data analysis. Nutr Rev 66(Suppl 1):S69–S72. doi:10.1111/j.1753-4887.2008.00072.x
AHRQ (2008) 2007 National Healthcare Disparities Reports 2007. Rockville, MD: US Department of Health and Human Services, Agency for Healthcare Research and Quality. Report No.: AHRQ Pub. No. 08-0041
Anonymous (2009) The right target: how survival is affected by race/ethnicity, socioeconomic status. HemOnc Today 10:1
Goss E, Lopez AM, Brown CL, Wollins DS, Brawley OW, Raghavan D (2009) American society of clinical oncology policy statement: disparities in cancer care. J Clin Oncol 27:2881–2885. doi:10.1200/JCO.2008.21.1680
IOM (2003) Unequal treatment: confronting racial and ethnic disparities in healthcare. In: Smedley BD, Stith AY, Nelson AR (eds) Institute of Medicine, Washington, DC
Dawood S, Broglio K, Kau SW, Green MC et al (2009) Triple receptor-negative breast cancer: the effect of race on response to primary systemic treatment and survival outcomes. J Clin Oncol 27:220–226. doi:10.1200/JCO.2008.17.9952
Albain KS, Unger JM, Crowley JJ, Coltman CA Jr, Hershman DL (2009) Racial disparities in cancer survival among randomized clinical trials patients of the Southwest Oncology Group. J Natl Cancer Inst 101:984–992. doi:10.1093/jnci/djp175
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dunn, B.K., Agurs-Collins, T., Browne, D. et al. Health disparities in breast cancer: biology meets socioeconomic status. Breast Cancer Res Treat 121, 281–292 (2010). https://doi.org/10.1007/s10549-010-0827-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-0827-x