Abstract
As the use of screening mammography expands, the proportion of invasive breast cancer ≤1 cm is increasing. The aims of this study were: (1) to identify risk factors for systemic metastases in patients with ≤1 cm invasive breast cancer and (2) to investigate the patient groups at the greatest risk for metastases with such small tumors. Data were collected retrospectively from the breast cancer registry of our institution for patients with invasive breast cancer from October 1994 to December 2004. Of 4,036 patients who received curative breast cancer surgery, we identified 427 patients who had T1a or T1b breast cancer excluding 39 patients who received neoadjuvant chemotherapy. Ipsilateral axillary lymph node involvement was found in 13% (57/427) of patients at the time of surgery. A multivariate analysis was conducted in 370 (T1aN0, T1bN0) patients without lymph node involvement. In a Cox-regression model, HER-2 positive and triple negative (TN) groups were identified as independent risk factors to predict distant relapse-free survival (DRFS) [Hazard ratio (HR) 8.8, P = 0.003 for HER-2 positive group; HR 5.1, P = 0.026 for TN group] in T1bN0 tumors. Statistical significance was not maintained when the analysis was limited to T1aN0 tumors. Even though T1aN0 and T1bN0 tumors have a relatively low risk of systemic failure, anti-HER-2-directed therapy for HER-2 group and new innovative adjuvant systemic treatment for TNBC patients with T1bN0 tumors should be considered. Prospective adjuvant trials are warranted in these subgroups of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the use of screening mammography grows, the proportion of invasive breast cancer with tumor size ≤1 cm is increasing [1–3]. Patients with breast cancers ≤1 cm have a relatively low incidence of loco-regional axillary lymph nodal metastases as well as systemic metastases and represent a subset whose prognosis is so favorable that the use of adjuvant systemic therapy is not routinely recommended, particular in node-negative patients [4–7]. However, 10–30% of the breast cancers with tumor ≤1 cm without lymph node metastases treated with locoregional therapy eventually recur [6–9]. Some of these patients might benefit from systemic adjuvant treatment according to risk factors [10, 11]. According to National Comprehensive Cancer Network (NCCN) guideline for these small and node-negative breast cancers, adjuvant chemotherapies are considered for hormone receptor (HR) negative, Human Epidermal Growth Factor Receptor 2 (HER-2) positive breast cancer with category 3 and HR negative, HER-2 negative breast cancer patients with category 1. Although adjuvant systemic therapy has been recently recommended for some patients who have risk factors for relapse with stage T1bN0M0 breast cancer, there is neither enough evidence, nor unanimous guideline for adjuvant systemic chemotherapy to this group of patients at this time [12–14].
Certain subgroups of patients with stage T1a–bN0M0 breast cancer are likely to be at greater risk of recurrence, including systemic failure, than others. High nuclear and/or histologic tumor grade and lymphovascular invasion (LVI) are reportedly associated with poorer outcomes in some retrospective trials [15, 16]. Gene expression profiling by microarray analysis according to the level of mRNA expression of specific genes revealed that breast cancer is not a single disease. Understanding tumor biology leads to marked advances in specific therapeutic strategies such as a HER-2-directed therapy for HER-2-positive breast cancer [17–19]. However, the prognostic significances of HR and HER-2 status for these small tumors are unclear. Conflicting results for HR status offer far from convincing evidence for its role as a prognostic factor in T1a–bN0M0 breast cancer [8, 20, 21]. HER-2 overexpression, a known risk factor for relapse and poorer clinical outcome, also needs to be validated in this setting; insufficient data are available to support it as a predictive factor in small and node-negative breast cancer [22–24]. In fact, four large prospective adjuvant clinical trials that demonstrated a definite clinical benefit for adding trastuzumab for the treatment of HER-2-overexpressing breast cancer did not include this population of patients [25–28]. Triple-negative breast cancer (TNBC) has been known to be an aggressive subtype that shares molecular and pathologic features with BRCA1-associated breast cancers. Thus, new therapeutic approaches based on biologic background are undergoing clinical trials including platinum compounds [29–31], EGFR targeting agents [32, 33], antiangiogenic agents [34], and poly (ADP-ribose) polymerase-1 (PARP1) inhibitors [35, 36]. However, adjuvant treatment for these small TNBC still needs to be defined.
To understand which patients with small (≤1 cm) breast cancer without lymph node metastases are at the greatest risk for a poor outcome, we conducted this retrospective study. The aims of this study were to identify the risk factors for recurrence in patients with ≤1 cm invasive breast cancer, and to determine which patients are at the greatest risk of such failure in this setting based on primary tumor characteristics, HR and HER-2 status.
Patients and methods
Patients
We conducted a retrospective analysis of medical records of the patients with histologically confirmed invasive breast cancer who had received curative surgery at Samsung Medical Center from October 1994 to December 2004. Our institute is university hospital with comprehensive cancer center. Most of the patients of our institute were referred from private clinics or community hospitals. All pathologic specimens were reviewed by two experienced pathologists, who determined primary tumor characteristics represented as histologic and nuclear grade, size, presence of LVI, multiplicity, and the receptor status of the estrogen receptor (ER), progesterone receptor (PgR), HER-2 using immunohistochemical (IHC) staining. ER and PgR positivity was defined as an Allred score from 3 to 8 by IHC using antibodies to the ER (Immunotech, France) and PgR (Novocastra, UK). HER-2 status was evaluated using an antibody (DAKO, USA) and/or fluorescence in situ hybridization (FISH). Grades 0 and 1 for HER-2 by IHC were defined as a negative result, and grade 3 as a positive result. Amplification of the HER-2 was confirmed by FISH if HER-2 was rated as 2+ by IHC. HR positive (+ve) group was defined as ER and/or PgR positive irrespective of HER-2 status. HER-2 group was defined as HR negative (−ve) and HER-2 positive patients. TNBC group was defined as ER, PR, and HER-2 negative. All core biopsies from referral institutes were reviewed by experienced pathologists in our institute including IHC staining prospectively at the time of initial referral. The pathologic reviews with IHC staining for all the surgical specimens were done prospectively and comprehensively by two experienced pathologists in our institute. Our study protocol was approved by the institutional review board of Samsung Medical Center.
Systemic adjuvant treatments after surgery
After definitive surgery with curative aim, most of the patients received adjuvant systemic treatments. Out of 427 patients, 148 (34.7%) were treated with adjuvant chemotherapy. Among 342 HR positive patients, 306 (89.5%) patients received adjuvant hormonal treatment.
Statistical analysis
RFS was from the date of curative surgery to the date when breast cancer recurred irrespective of locoregional or distant metastases including ipsilateral and contralateral breast recurrences. Distant relapse-free survival rate (DRFS) was from the date of curative surgery to the date of documented distant metastases. Deaths that took place prior to cancer recurrence were censored at the time of death. OS was from the date of curative surgery to the date of death. The RFS, DRFS, and OS were estimated by the Kaplan–Meier product limit method. The log-rank test was used to compare survival rates. A P-value <0.05 was considered significant.
The differences in responses between phenotypic subtypes were estimated by the χ2 test or Fisher’s exact test. A binary logistic regression analysis was used for the multivariate analysis of the impact of each potential prognostic variable on lymph node involvement. A Cox proportional hazards regression model was used to assess the effect of each potential prognostic variable on RFS, DRFS, and OS. All potential prognostic variables were included in the model, and variables were then removed from this model one at a time in a backward selection process using the likelihood ratio test and a significance level of 0.05.
REMARK guidelines
This study was a retrospective cohort analysis using medical records between 1994 and 2004 at a single institute. However, in reporting our study, we have adhered to the guidelines in 2005 of an important methodology paper entitled “Reporting recommendations for tumor marker prognostic studies (REMARK guidelines)” [37, 38]. To decrease potential bias arising in review of the medical record, we included “Patient Cohort” that fulfilled the criteria as data (Fig. 1).
Results
Patient cohort (Fig. 1)
We identified 4,036 patients who were diagnosed as breast cancer and received curative surgery for the treatment of breast cancer at Samsung Medical Center from October 1994 to 2004. Of the 4,036 patients who had received definitive surgery, 359 patients with ductal carcinoma in situ (DCIS) or lobular carcinoma in situ (LCIS) and 123 patients with microinvasive cancer were excluded from the analysis. Among the 3,554 invasive breast cancer patients, we identified 466 patients with a primary tumor size of 1 cm or less. After excluding 39 patients who received neoadjuvant chemotherapy, our final cohort was 427 T1a–b patients, which are composed of 57 node-positive (13.0%) and 370 node-negative cases. The median follow-up duration was 61 months (36.0–161.6).
Clinicopathological characteristics according to the status of ipsilateral axillary nodal involvement (Tables 1, 2)
The median age at diagnosis of all 427 T1a–b patients was 47 years (range, 22–81 years) and the median tumor size was 0.8 cm (0.11–1.0 cm). During the median 61 months of follow-up, the relapse rate was 5.2% (22/427), the distant relapse rate was 3.5% (15/427), and the 5-year OS rate was 97.7% (417/427).
Ipsilateral axillary lymph node involvement was found in 13% (57/427) of cases at the time of surgery. Axillary lymph node involvement was more common in patients with high nuclear (36.8% vs. 20.1%, P = 0.005) and histologic grade (35.2% vs. 17.2%, P = 0.002) tumors, presence of LVI (27.5% vs. 10.2%, P = 0.005), multifocal or multicentric tumors (24.6% vs. 7.3%, P < 0.0001), invasive ductal carcinoma (96.5% vs. 85.6%, P = 0.040), ER negativity (41.1% vs. 21.8%, P = 0.002), PR negativity (51.8% vs. 32.3%, P = 0.004), HER-2 positivity (33.9% vs. 12.0%, P < 0.0001), and triple negativity (TNBC) (24.5% vs. 11.0%, P = 0.002) (Table 1). In a logistic-regression multivariate analysis, tumor multiplicity (hazard ratio (HR) 3.87, 95% CI; 1.849–8.087, P < 0.0001), HER-2 group (ER−/PR−/HER-2+) (HR 2.90, 95% CI 1.337–6.280, P = 0.007), and TNBC group (ER−/PR−/HER-2−) (HR 2.34, 95% CI 1.019–5.371, P = 0.045) were identified as risk factors for axillary lymph node involvement (Table 2).
Clinical outcomes of 370 T1a–bN0M0 breast cancer patients
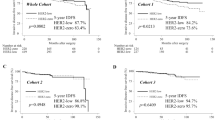
To identify predictive factors for systemic failure in small (≤1 cm) tumors without lymph-node involvement, we analyzed DRFS in 370 T1a–bN0M0 patients. The HER-2 and TNBC group showed poorer DRFS than HR positive group with statistical significance (Fig. 2a). HER-2 and TNBC group were identified as independent risk factors for RFS (HR 7.2, 95% CI 2.024–25.715, P = 0.002 for HER-2 group; HR 5.5, 95% CI 1.542–19.422, P = 0.009 for TNBC group) and DFRS (HR 5.7, 95% CI 1.039–31.510, P = 0.045 for HER-2 group; HR 6.0, 95% CI 1.339–26.847, P = 0.049 for TNBC group). TNBC group was identified as an independent risk factor for OS (HR 15.9, 95% CI 2.561–99.246, P = 0.003), but HER-2 group was not (HR 1.2, 95% CI 0.915–4.234, P = 0.124) (Fig. 2b); (Table 3).
Distant relapse-free survival (DRFS) and Overall survival (OS) Kaplan–Meier curve T1a–bN0M0 and T1bN0M0 breast cancer patients according to HR and HER-2 status. a DRFS of T1a–bN0M0 patients; black line represents DRFS of HR positive group, redline represents of DRFS of HER-2 positive group, and green line represents of DRFS of TN group (P = 0.0108 by log-rank test). b OS of T1a–bN0M0 patients; black line represents OS of HR positive group, red line represents of DRFS of HER-2 positive group, and green line represents of DRFS of TN group (P = 0.0047 by log-rank test). c DRFS of T1bN0M0 patients; black line represents DRFS of HR positive group, red line represents of OS of HER-2 positive group, and green line represents of OS of TN group (P = 0.0002 by log-rank test). d OS of T1bN0M0 patients; black line represents OS of HR positive group, red line represents of OS of HER-2 positive group, and green line represents of OS of TN group (P = 0.0075 by log-rank test). e DRFS of T1a–bN0M0 HER-2+ patients according to ER status (n = 54); green line represents DRFS of HER-2+/ER+ patients, red line represents of DRFS of HER-2+/ER− patients (P = 0.46 by log-rank test)
Clinical outcomes of T1bN0M0 (n = 280) and T1aN0M0 (n = 90) breast cancer patients
In order to differentiate the sub-populations of patients more likely to benefit from systemic adjuvant treatment, we analyzed T1bN0 and T1aN0 patients separately. In T1bN0 patients, the HER-2 and TNBC groups had significantly worse DRFS than the HR positive group (Fig. 2c, d). HER-2 and TNBC groups were identified as independent risk factors for RFS (HR 8.8, 95% CI 2.1–37.2, P = 0.003 for HER-2 group; HR 5.1, 95% CI 1.2–21.3, P = 0.026 for TNBC), DRFS (HR 8.8, 95% CI 1.7–62.9, P = 0.003 for TNBC group; HR 5.1 95% CI 0.9–33.0 for TNBC group, P = 0.026), and OS (HR 5.0, 95% CI 1.8–30.2, P = 0.067 for HER-2 group; HR 11.1, 95% CI 1.5–80.8, P = 0.017 for TNBC group) (Table 3).
When only T1aN0M0 patients were evaluated, HER-2 and TNBC groups were no longer independent predictive factors for systemic failure. Survival curves for T1aN0M0 patients could not be drawn since most of the observations are censored.
Discussion
Currently, two tests with clinical utility, oncotype DXTM [39, 40] and MammaPrint® [41] through the Microarray in Node-Negative Disease May Avoid Chemotherapy (MINDACT) trial [42], are used for individualized therapy for low risk, node negative group to avoid unnecessary excessive treatment. Conversely, the aims of this study were to identify the high risk group for recurrence in node-negative patients with ≤1 cm invasive breast cancer, and to determine which patients are at the greatest risk of such failure in this setting to benefit from adjuvant treatment.
We first investigated predictive factors associated with ipsilateral axillary lymph node metastases in patients with tumor size ≤1 cm. A positive correlation between tumor size and node status has been generally reported [43, 44]. Accordingly, the identified predictive factors for lymph node involvement may help to explain poor clinical outcomes with early systemic failure. High histologic and/or nuclear grade and LVI were associated with higher ipsilateral axillary lymph node involvement in our study and other previous investigations (Table 1) [6, 45, 46]. The degree of lymph node positivity we observed (13.3%) was also similar to other reports [47, 48]. We found hormonal and HER-2 status were closely related with ipsilateral axillary lymph node involvement (Table 1). Furthermore, tumor multiplicity, HER-2 group, and TNBC group were identified as independent risk factors for ipsilateral axillary lymph node involvement (Table 2). Because the current staging system does not reflect complex features of multifocal and multicentric breast cancers [49], we tried to figure out the significance of multiplicity. However, multiplicity did not maintain its statistical significance in our multivariate analysis for survival though that was independent risk factors for lymph node involvement. Pathologic grade, EIC, and LVI were also not maintained their statistical significances related to lymph node involvement in the logistic regression multivariate analysis. We infer from these findings that breast cancer subtypes by gene expression profile may encompass biologic characteristics of primary tumor represented as histologic and/or nuclear grades, EIC, and LVI. Differences in these primary tumor characteristics among subgroups support our supposition. Biologic aggressiveness could be expressed through tumor characteristics. It is difficult to conclude that tumor characteristics have independent significance as predictive markers since the results have been conflicting in the few studies [6, 50].
We successively narrowed our analyses to T1a–bN0M0 and T1bN0M0 patients. HER-2 group and TNBC group were identified as independent risk factors for DRFS in T1a–bN0M0 patients (Fig. 2a, b; Table 3). Because node-positive patients already represent a high-risk group for relapse and adjuvant treatment is routinely recommended even in patients with small primary tumors, T1a–bN0 patients constitute our primary group of interest. Excluding node-positive patients, HER-2 group and TNBC were identified as independent risk factors for RFS and DRFS in T1a–bN0M0 patients (Fig. 2a; Table 3). When the analysis was limited to T1bN0 patients, the statistical power of the both risk factors were much stronger in terms of RFS, DRFS, and OS, particular in TNBC group (Fig. 2c, d; Table 3). This statistical significance was not maintained limiting to T1aN0 patients.
A nationwide population-based study showed that HER-2 positivity is superior to ER as a risk factor for DRFS [5]. Additionally, HER-2 positivity has been reported as a risk factor even in node-negative patients [22]. Interestingly, when HER-2+/ER+ tumors were included in this analysis with HER-2+/ER− tumors, the role of HER-2 as a independent predictor for worse outcome was diminished, even though the population was limited to T1bN0 in our study (data not shown). It is not clear how co-expression of HR and HER-2 affects the clinical outcome in HER-2-overexpressing breast cancer, but it may mitigate the aggressiveness of HER-2 in small node-negative invasive breast cancer. In addition, DRFS of HER-2 positive patients in our study were different according to ER status though statistical significance did not reach (Fig. 2e). According to a few recent reports, ER expression may affect the tumor behavior of HER-2+ breast cancer including hormone responsiveness [51–54]. Conversely, HER-2+/ER+ population may occupy some parts of luminal B cluster by gene-expression microarray [55]. Further investigation on the interaction between HER-2 and ER should be evaluated even in small tumors.
The HERA trial recently found that adjuvant trastuzumab therapy reduces the risk of relapse in ER−/PR− patients, even in node-negative patients [56]. Importantly, Kaplan–Meier survival curve of HER-2 group showed markedly improved OS like as HR+ group than DRFS, which was not found in TNBC (Fig. 2b, d). This survival benefit cannot be explained completely due to very small number of the patients. However, it is possible to have some benefit from the addition of trastuzumab after relapse, because the two relapsed patients are surviving since having been treated with trastuzumab plus taxane chemotherapies. It also can imply that HER-2-directed therapy should be considered from the adjuvant setting to prevent relapse, even in small tumor. Although the efficacy of trastuzumab remains to be fully demonstrated, the anti-HER-2 antibody may provide a therapeutic option to prevent poorer clinical outcomes. Because of the heterogeneity of HER-2-overexpressing breast cancers, the benefit from HER-2-directed therapy could be different in small (0.5–1 cm), node-negative tumors as well. A randomized, phase III trial of adjuvant treatment (chemotherapy with or without anti-HER-2 therapy or anti-HER-2 therapy alone) is needed in this subpopulation of HER-2-overexpressing breast cancer patients.
It has already been established that tumor size does not correlate with nodal status in TNBC, especially for BRCA1-associated tumors [57–59]. There is no definitive evidence, however, that “triple negativity” as well as HER-2 functions as an independent risk factor for survival in small node-negative invasive breast cancer. We found that TNBC patients may have worse outcomes than any other subtype in T1bN0 patients, a finding supported by the OS rate analysis (HR 11.1, P = 0.017 by Cox-regression analysis, Table 3). New innovative adjuvant treatment strategies including targeted therapy based on biology are urgently needed for this specific group of patients.
Taken together, the biologic aggressiveness of HER-2 positivity and TNBC may override the extent of objective disease encapsulated by the TNM staging system.
There is always the possibility of patient selection bias in retrospective single center studies like this one, but this study also had a sizeable patient cohort. The median age of 47 years seems to be younger than average. However, in a difference from Western countries, the age distribution of breast cancer peaked in the late forties in Korea [60]. The median age of the Korean breast cancer patients from the published data were reported as from 46 to 49 [24, 61, 62], 47-years is within the range. Thus, our population did not show any selection bias in terms of age distribution. Our results offer instructive information for this specific population of patients, which would need a long period to progress in a prospective trial.
In conclusion, HER-2 and TNBC group were identified as independent predictive factors for worse outcome in T1bN0 invasive breast cancer patients, who are at greater risk of systemic failure. Prospective randomized clinical trials of anti-HER-2 directed therapy for HER-2 group and new innovative adjuvant systemic treatment for TNBC group with T1bN0 tumors are warranted.
References
Miller BA, Feuer EJ, Hankey BF (1993) Recent incidence trends for breast cancer in women and the relevance of early detection: an update. CA Cancer J Clin 43:27–41
Jemal A, Clegg LX, Ward E et al (2004) Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer 101:3–27
Schootman M, Jeffe D, Reschke A et al (2004) The full potential of breast cancer screening use to reduce mortality has not yet been realized in the United States. Breast Cancer Res Treat 85:219–222
Rosen PP, Groshen S, Kinne DW et al (1993) Factors influencing prognosis in node-negative breast carcinoma: analysis of 767 T1N0M0/T2N0M0 patients with long-term follow-up. J Clin Oncol 11:2090–2100
Joensuu H, Pylkkänen L, Toikkanen S (1999) Late mortality from pT1N0M0 breast carcinoma. Cancer 85:2183–2189
Chen YY, Schnitt SJ (1998) Prognostic factors for patients with breast cancers 1 cm and smaller. Breast Cancer Res Treat 51:209–225
Leitner SP, Swern AS, Weinberger D et al (1995) Predictors of recurrence of patients with small (one centimeter or less) localized breast cancer (T1a, bN0M0). Cancer 76:2266–2274
Quiet CA, Ferguson DJ, Weichselbaum RR et al (1995) Natural history of node-negative breast cancer: a study of 826 patients with long-term follow-up. J Clin Oncol 13:1144–1151
Chia SK, Speers CH, Bryce CJ et al (2004) Ten-year outcomes in a population-based cohort of node-negative, lymphatic, and vascular invasion-negative early breast cancers without adjuvant systemic therapies. J Clin Oncol 22:1630–1637
Martin M, Pienkowski T, Mackey J et al (2005) Adjuvant docetaxel for node-positive breast cancer. N Engl J Med 352:2302–2313
Henderson IC, Berry DA, Demetri GD et al (2003) Improved outcomes from adding sequential paclitaxel but not from escalating doxorubicin dose in an adjuvant chemotherapy regimen for patients with node-positive primary breast cancer. J Clin Oncol 21:976–983
Eifel P, Axelson JA, Costa J et al (2001) National Institutes of Health Consensus Development Conference Statement: adjuvant therapy for breast cancer. J Natl Cancer Inst 93:978–989
National Comprehensive Cancer Network: Clinical Practice Guidelines in Oncology, Version 1.2009, Breast Cancer. http://www.nccn.org/professinals/physician_gls/PDF/breast.pdf
Goldhirsch A, Wood WC, Gelber RD et al (2007) 10th St. Gallen conference: progress, promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol 18(7):1133–1144
Lee AK, Loda M, Mackarem G et al (1997) Lymph node negative invasive breast carcinoma 1 centimeter or less in size (T1a, bN0M0): clinicopathologic features and outcome. Cancer 79:761–771
Mann GB, Port ER, Rizza C et al (1999) Six-year follow-up of patients with microinvasive, T1a, and T1b breast carcinoma. Ann Surg Oncol 6:591–598
Slamon DJ, Godolphin W, Jones LA et al (1989) Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244:707–712
Slamon DJ, Clark GM, Wong SG et al (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235:177–182
Slamon DJ, Leyland-Jones B, Shak S et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpress HER2. N Engl J Med 344:783–792
Colleoni M, Rotmensz N, Peruzzotti G et al (2004) Minimal and small size invasive breast cancer with no axillary lymph node involvement: the need for tailored adjuvant therapies. Ann Oncol 15:1633–1639
Mirza AN, Mirza NQ, Vlastos G et al (2002) Prognostic factors in node-negative breast cancer: a review of studies with sample size more than 200 and follow-up more than 5 years. Ann Surg 235:10–26
Chia S, Norris B, Speers C et al (2008) Human epidermal growth factor receptor 2 overexpression as a prognostic factor in a large tissue microarray series of node-negative breast cancers. J Clin Oncol 26:5697–5704
Joensuu H, Isola J, Lundin M et al (2003) Amplification of erbB2 and erbB2 expression are superior to estrogen receptor status as risk factors for distant recurrence in pT1N0M0 breast cancer: a nationwide population-based study. Clin Cancer Res 9:923–930
Choi YH, Ahn JH, Kim SB et al (2009) Tissue microarray-based study of patients with lymph node-negative breast cancer shows that HER2/neu overexpression is an important predictive marker of poor prognosis. Ann Oncol 20:1337–1343
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672
Joensuu H, Kellokumpu-Lehtinen PL, Bono P et al (2006) Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med 354:809–820
Romond EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Slamon D, Eiermann W, Robert N et al (2005) Phase III randomized trial comparing doxorubicin and cyclophosphamide followed by docetaxel (AC → T) with doxorubicin and cyclophosphamide followed by docetaxel and trastuzumab (AC → TH) with docetaxel, carboplatin and trastuzumab (TCH) in HER2 positive early breast cancer patients: BCIRG 006 study. Breast Cancer Res Treat 94(suppl 1):S5
Uhm JE, Park YH, Yi SY et al (2009) Treatment outcomes and clnicopathologic characteristics of triple-negative breast cancer patients who received platinum-containing chemotherapy. Int J Cancer 124:1457–1462
Chia JW, Ang P, See H et al (2007) Triple-negative metastatic/recurrent breast cancer: treatment with paclitaxel/carboplatin combination chetmotherapy (abstract 1086). J Clin Oncol 26(suppl 15):43s
Garber JE, Richardson A, Harris LN et al (2006) Neo-adjuvant cisplatin in triple-negative breast cancer (abstract 3074). Breast Cancer Res Treat 100:S149
Nielsen TO, Hsu FD, Jensen K et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5374
Hoadley KA, Weigman VJ, Fan C et al (2007) EGFR associated expression profiles vary with breast cancer subtype. BMC Genomics 8:258
Miller K, Wang M, Gralow J et al (2007) Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med 357:2666–2676
O’Shaughnessy J, Osborne C, Yoffe M et al (2009) Efficacy of BSI-201, a poly (ADP-ribose) polymerase-1 (PARP1) inhibitor, in combination with gemcitabine/carboplatin (G/C) in patients with metastatic triple-negative breast cancer (TNBC): results of a randomized phase II trial. J Clin Oncol 27(suppl 2):793s36
Gronwald J, Byrski T, Huzarski T et al (2009) Neoadjuvant therapy with cisplatin in BRCA-positive breast cancer patients. J Clin Oncol 27(suppl 1):7s
McShane LM (2005) Reporting recommendations for tumor marker prognostic studies. J Clin Oncol 23:9067–9072
McShane LM, Altman DG, Sauerbrei W et al (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235
Paik S, Shak S, Tang G et al (2004) A multigene assay to predict recurrence of tamoxifen treted, node-negative breast cancer. N Engl J Med 351:2817–2826
Paik S (2007) Development and clnical utility of a 21-gene recurrence score prognostic assay in patients with early breast cancer treated wtih tamoxifen. Oncologist 12:615–631
van de Vijver MJ, He YD, van’t Veer LJ et al (2002) A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 347:1999–2009
Bogaerts J, Cardoso F, Buyse M et al (2006) TRANSBIG Consortium. Gene signature evaluation as a prognostic tool: challenges in the design of the MINDACT trial. Nat Clin Pract Oncol 3:540–551
Carter CL, Allen C, Henson DE (1989) Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 63:181–187
Olivotto IA, Jackson JS, Mates D et al (1998) Prediction of axillary lymph node involvement of women with invasive breast carcinoma: a multivariate analysis. Cancer 83:948–955
Malbenco DC, Welss LK, Pawllsh KS et al (1999) Axillary lymph node metastases associated with small invasive breast carcinomas. Cancer 85:1530–1536
Rivadeneira DE, Simmons RM, Christos PJ et al (2000) Predictive factors associated with lymph node metastases in T1a and T1b breast carcinomas: analysis in more than 900 patients. J Am Coll Surg 191:1–6
Laura S, Coombs NJ, Ung O et al (2006) Tumour size as a predictor of axillary node metastases in patients with breast cancer. ANZ J Surg 76:1002–1006
Coburn NG, Clarke-Pearson E, Chung MA et al (2006) A novel approach to T classification in tumor-node-metastasis staging of breast cancer. Am J Surg 192:434–438
Coombs NJ, Boyages J (2005) Multifocal and multicentric breast cancer: does each focus matter? J Clin Oncol 23:7497–7502
Rakha EA, El-Sayed ME, Lee AHS et al (2008) Prognostic significance of Nottingham histologic grade in invasive breast carcinoma. J Clin Oncol 26:3153–3158
Van Calster B, Vanden Bempt I, Drijkoningen M et al (2009) Axillary lymph node status of operable breast cancers by combined steroid receptor and HER-2 status: triple positive tumours are more likely lymph node positive. Breast Cancer Res Treat 113:181–187
Marchiò C, Natrajan R, Shiu KK et al (2008) The genomic profile of HER2-amplified breast cancers: the influence of ER status. J Pathol 216:399–407
Prat A, Baselga J (2008) The role of hormonal therapy in the management of hormonal-receptor-positive breast cancer with co-expression of HER2. Nat Clin Pract Oncol 5:531–542
Kun Y, How LC, Hoon TP et al (2003) Classifying the estrogen receptor status of breast cancers by expression profiles reveals a poor prognosis subpopulation exhibiting high expression of the ERBB2 receptor. Hum Mol Genet 12:3245–3258
Cheang MC, Chia SK, Voduc D et al (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750
Untch M, Gelber RD, Jackisch C et al (2008) Estimating the magnitude of trastuzumab effects within patient subgroups in the HERA trial. Ann Oncol 19:1090–1096
Dent R, Trudeau M, Pritchard KI et al (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13:4429–4434
Foulkes WD, Bruder JS, Stefansson JM et al (2004) The prognostic implication of the basal-like (cycle E high/p27low/p53+/glomeruloid-microvascular proliferation+) phenotype of BRCA1-related breast cancer. Cancer Res 64:830–835
Foulkes WD, Metcalfe K, Hanna W et al (2003) Disruption of the expected positive correlation between breast tumor size and lymph node status in BRCA-1 related breast carcinoma. Cancer 98:1569–1577
Jung YS, Ko SS, Youn HJ et al (2008) Chronological changing patterns of clinical characteristics of Korean breast cancer patients during 10 years (1996–2006) using nationwide breast cancer registration on-line program: biannual update. J Surg Oncol 98:318–323
Yoo KY, Kang D, Park SK et al (2002) Epidemiology of breast cancer in Korea: occurrence, high-risk groups, and prevention. J Korean Med Sci 17:1–6
Chang H, Rha SY, Jeung HC et al (2009) Association of the ABCB1 gene polymorphisms 2677G>T/A and 3435C>T with clinical outcomes of paclitaxel monotherapy in metastatic breast cancer patients. Ann Oncol 20:272–277
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, Y.H., Kim, S.T., Cho, E.Y. et al. A risk stratification by hormonal receptors (ER, PgR) and HER-2 status in small (≤1 cm) invasive breast cancer: who might be possible candidates for adjuvant treatment?. Breast Cancer Res Treat 119, 653–661 (2010). https://doi.org/10.1007/s10549-009-0665-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0665-x