Abstract
Purpose
The purpose of this study was to assess differences in breast cancer-specific mortality within tumors of the same size when breast cancer was defined using the three tumor markers estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2).
Methods
We identified 104,499 cases of node-negative primary female invasive breast cancer from the California Cancer Registry. Tumor size was categorized as T1a, T1b, T1c, T2, and T3. Breast cancer was defined using ER, PR, and HER2. Kaplan–Meier Survival analysis was conducted and Cox Regression was used to compute the adjusted risk of mortality for the ER+/PR+/HER2+, ER−/PR−/HER2− (TNBC), and ER−/PR−/HER2+ (HER2-overexpressing) subtypes when compared with the ER+/PR+/HER2−. Separate models were computed for each tumor size.
Results
Unadjusted survival analysis showed that for all tumor sizes, the ER+/PR+ subtypes regardless of HER status have better breast cancer-specific survival than ER−/PR− subtypes. Subtype was not an important factor for risk of mortality for T1a tumors. The ER+/PR+/HER2+ subtype was only a risk for mortality in T1b tumors that were unadjusted for treatment. For all other tumor sizes, the ER+/PR+/HER2+ had the same mortality as the ER+/PR+/HER2− subtype regardless of adjustment for treatment. The HER2-overexpressing subtype had a higher risk of mortality than the ER+/PR+/HER2− subtype except for T1b tumors that were adjusted for treatment. For all tumor sizes, the TNBC had higher hazard ratios than all other subtypes.
Conclusions
T1a tumors have the same risk of mortality regardless of ER/PR/HER2 subtype, and ER and PR negativity plays a stronger role in survival than HER2 positivity for tumors of all size.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of screening mammography has lead to increased detection of node-negative, stage 1 breast cancer [1,2,3]. However, the decision to treat small, node-negative breast cancer remains uncertain since women with T1a and T1b tumors have been noted to have an excellent prognosis without chemotherapy [4,5,6,7,8].
In addition to tumor size, tumor subtype is an important prognostic factor for breast cancer survival, but its importance is dependent in part on how subtype is defined. Many studies describe breast cancer subtypes with reference to hormone receptor status and independently, human epidermal growth factor receptor 2 (HER2) status. There are eight combinations of estrogen receptor (ER), progesterone receptor (PR), and HER2 with significant differences in the demographics, tumor characteristics, and survival but it is not common for subtype to be defined using all three markers [9, 10].
The purpose of this study was to assess differences in breast cancer-specific mortality when breast cancer is defined using all three markers and within tumors of the same size.
Methods
The study utilized the California Cancer Registry (CCR) to identify 104,499 cases of node-negative primary female invasive breast cancer first diagnosed between January 1, 2000 and December 31, 2014 and reported to the CCR as of December 31, 2015 (ICDO-3 sites C50.0–C50.9) [11]. Cases had complete data for tumor size, grade, American Joint Commission on Cancer (AJCC) stage of diagnosis, cause of death, age, socioeconomic status (SES), and race/ethnicity.
Cases were reported to the Cancer Surveillance Section of the California Department of Public Health from hospitals and other facilities providing care or therapy to cancer patients residing in California [12]. Breast cancer-specific mortality was defined as a death due to breast cancer as documented by the codes ranging from C50.01 to C50.91 of the International Statistical Classification of Diseases and Related Health Problems, 10th Revision [13].
Tumor size was categorized as T1a and micro (<1.00–4.99 mm), T1b (5.00–9.99 mm), T1c (10.00–19.99 mm), T2 (20.00–49.99 mm), and T3 (50.00+ mm).
ER and PR status were recorded according to pathologists’ interpretation of the assays. ER and PR were considered negative if immunoperoxidase staining of tumor cell nuclei was less than 5%. ER and PR status may also have been determined by examining cytosol protein. ER was considered negative if there were fewer than 3 fmol/mg of cytosol protein, and PR was considered negative if there were fewer than 5 fmol/mg of cytosol protein [11].
HER2 was assessed through immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH). IHC is scored on a qualitative scale from 0 to 3+, based on interpretation of staining intensity, with 0 through 1+ classified as negative, 2+ as borderline, and 3+ as positive [14] FISH was scored on a quantitative scale with less than 2 copies of the HER2 gene classified as negative and two or more copies as positive [15].
Using ER, PR, and HER2, eight breast cancer subtypes were defined: ER+/PR+/HER2−, ER+/PR+/HER2, ER+/PR−/HER2−, ER+/PR−/HER2, ER−/PR+/HER2−, ER−/PR+/HER2+, ER−/PR−/HER2− (triple-negative or TNBC), and ER−/PR−/HER2+ (HER2-overexpressing).
SES was derived using data from the 2000 US census for cases diagnosed from 2000–2005 and the American Community Survey was used for cases diagnosed from 2006–2014 [16]. This SES variable is an index that utilizes education, employment characteristics, median household income, proportion of the population living 200% below the Federal Poverty Level, median rent and median housing value of census tract of residence for case and denominator population. A principal component analysis was used to identify quintiles of SES ranging from 1 (the lowest) to 5 (the highest) [17]. This area based SES measure has been used in many studies utilizing cancer registry data [18,19,20,21,22,23,24,25,26].
Race/ethnicity was classified based on information obtained from the medical record which was derived from patient self-identification, assumptions based on personal appearance, or inferences based on the race of the parents, birthplace, surname, or maiden name. The four mutually exclusive categories of race/ethnicity used in this study were white, African American or black, Hispanic, and Asian/Pacific Islander (API).
Statistical analysis
Contingency tables were used to evaluate the distribution of age, subtype, tumor grade, race/ethnicity, treatment, and SES for each tumor size. Differences in mean age between the tumor sizes were compared using analysis of variance and post hoc tests.
Kaplan–Meier survival analysis and the Log-Rank test were used to compare unadjusted survival rates among the subtypes for each tumor size. Five-year and 10-year survival and 95% confidence intervals were reported. Cox Proportional Hazards modeling was used to compute the risk of mortality for the ER+/PR+/HER2+, TNBC, and HER2-overexpressing subtypes when compared with the ER+/PR+/HER2−. These four subtypes were chosen to facilitate comparison of ER+/PR+ tumors with ER−/PR− tumors and to evaluate the effect of HER2-positivity.
Separate models were computed for each tumor size so that all hazard ratios (HR) and 95% confidence intervals (CI) assessed differences between tumor subtypes of the same size. One set of models was adjusted for age, tumor grade, race/ethnicity, and SES. The second set of models included all of these variables and in addition, surgery (lumpectomy, mastectomy), chemotherapy, hormone therapy, and radiation therapy. Stage was excluded from analyses because of its strong correlation with tumor size. Variables were considered statistically significant and HRs were interpreted only when the Wald χ 2 was p < 0.05.
All analyses were performed using IBM SPSS 21.0 [27]. This research study involved analysis of existing data from the CCR without subject identifiers or intervention. Therefore, the study was categorized as exempt from institutional review board oversight.
Results
Median follow-up time was 5.2 years (range, 0–14.9 years). Table 1 shows the distribution of demographic and clinicopathologic features by increasing tumor size. The highest percent of cases (41.8%) were T1c. Women with T3 tumors were younger than women with smaller sized tumors (F 4, 104,494 = 196,692, p < 0.001).
The ER+/PR+/HER2−, ER+/PR+/HER2+, ER−/PR−/HER2−, and ER−/PR−/HER2+ subtypes comprised 87.3% of all cases. TNBC and the ER−/PR−/HER2+ subtypes had a higher percent of T2 and T3 tumors when compared with the other subtypes. Black women had the highest percent of T2 and T3 tumors. The two lowest SES categories had the highest percent of the largest tumors. Table 2 shows that for all tumor sizes, the ER+/PR+/HER2− had the best and the TNBC had the worst 5 and 10 year survival. Based on overlapping confidence intervals, the ER+/PR+/HER2+ subtype had the same 5 and 10 year unadjusted survival as the ER+/PR+/HER2− subtype except for the 5-year survival of T1c.
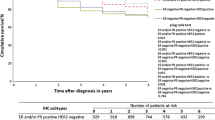
For T1a (Fig. 1a), T2 (Fig. 1d), and T3 (Fig. 1e) tumors, there were no statistically significant differences in unadjusted breast cancer-specific survival between the ER+/PR+/HER2− and ER+/PR+/HER2+ subtypes. The ER+/PR+/HER2− had better survival than the ER+/PR+/HER2+ subtype for T1b (χ 2 = 9.24, p = 0.002) (Fig. 1b) and T1c tumors (χ 2 = 6.15, p = 0.013) (Fig. 1c). For all tumor sizes, the TNBC and HER2-overexpressing subtypes had statistically significant worse survival than the ER+/PR+/HER2− subtype.
Results of the Cox Regression Analysis (Table 3) indicated that for T1a tumors, the Wald χ 2 was not statistically significant with or without adjustment for treatment. The ER+/PR+/HER2+ subtype was only a risk for mortality in T1b tumors that were unadjusted for treatment. For all other tumor sizes, the ER+/PR+/HER2+ had the same mortality as the ER+/PR+/HER2− subtype regardless of adjustment for treatment. Table 3 also showed that TNBC tumors had an increased risk of mortality for T1b and larger tumors regardless of adjustment for treatment. The HER2-overexpressing subtype had a higher risk of mortality than the ER+/PR+/HER2− subtype except for T1b tumors that were adjusted for treatment. For all tumor sizes, the TNBC had higher hazard ratios than the HER2-overexpressing subtype.
Discussion
The results of the present study found that for T1a tumors, there is no increased risk of mortality regardless of subtype. However, the treatment-adjusted risk of mortality for the TNBC and HER2-overexpressing subtypes varies by tumor size. For T1a tumors there is no increased risk of mortality for the TNBC but the risk of mortality is increased for all larger sized TNBC tumors with or without adjustment for treatment. In general, this is also true for the HER2-overexpressing subtype.
There is evidence for and against treatment of small, node-negative tumors. Chemotherapy has been shown to have no effect on the risk of mortality in T1a and T1b luminal B tumors after adjustment for age, grade, and lymph node status [8]. The present study is in agreement and provides additional insight on the role of tumor subtype for various sized tumors. We found no increased risk of treatment-adjusted mortality for the node-negative ER+/PR+/HER2+ subtype of any size when compared with the ER+/PR+/HER2− subtype. In addition, 5 and 10 year unadjusted survival of the ER+/PR+/HER2+ subtype is very similar to the ER+/PR+/HER2− subtype.
The unofficial mantra in medical oncology is that HER2 positivity always imparts a dire prognosis. However, the present study suggests that when taking ER and PR into consideration, HER positivity is not always detrimental. In fact, it appears that ER and PR negativity may be more important, supporting previous research [9, 28]. The risk of mortality for the ER+/PR+/HER2+ subtype is very similar to the ER+/PR+/HER2− subtype and the hazard ratios for the TNBC are higher than the HER2-overexpressing subtype for all tumor sizes. Conversely, other investigators have found that HER2-positive T1a and T1b tumors have a significant risk of relapse when compared with HER2-negative tumors and suggests treatment is warranted even for small, HER2-positive tumors regardless of ER and PR status [4, 5].
This retrospective, population-based study using registry data has limitations and cannot provide definitive answers for or against treatment of small tumors of any subtype. These limitations have been amply described [20, 29, 30]. Histologic grading of tumors as well as tests for ER, PR, and HER2 were performed by a wide variety of laboratories without central review. Treatment information from the CCR is quite generic and lacks specific information regarding drug type, dose, and use of anti-HER2 directed therapy. Despite these limitations, the strength of this study is the use of a large number of node-negative breast cancer cases which allowed for stratified analysis of tumor size. Findings obtained from several thousand cases provide real world insight.
Conclusions
This study shows that T1a tumors have the same risk of mortality regardless of ER/PR/HER2 subtype and that ER and PR negativity plays a stronger role in survival than HER2 positivity for tumors of all size.
References
Tabar L, Duffy SW, Vitak B, Chen HH, Prevost TC (1999) The natural history of breast carcinoma: what have we learned from screening? Cancer 86(3):449–462
Berry DA, Cronin KA, Plevritis SK, Fryback DG, Clarke L, Zelen M, Mandelblatt JS, Yakovlev AY, Habbema JD, Feuer EJ (2005) Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med 353(17):1784–1792
Mandelblatt JS, Stout NK, Schechter CB, van den Broek JJ, Miglioretti DL, Krapcho M, Trentham-Dietz A, Munoz D, Lee SJ, Berry DA, van Ravesteyn NT, Alagoz O, Kerlikowske K, Tosteson AN, Near AM, Hoeffken A, Chang Y, Heijnsdijk EA, Chisholm G, Huang X, Huang H, Ergun MA, Gangnon R, Sprague BL, Plevritis S, Feuer E, de Koning HJ, Cronin KA (2016) Collaborative modeling of the benefits and harms associated with different U.S. breast cancer screening strategies. Ann Intern Med 164(4):215–225. doi:10.7326/M15-1536
Curigliano G, Viale G, Bagnardi V, Fumagalli L, Locatelli M, Rotmensz N, Ghisini R, Colleoni M, Munzone E, Veronesi P, Zurrida S, Nole F, Goldhirsch A (2009) Clinical relevance of HER2 overexpression/amplification in patients with small tumor size and node-negative breast cancer. J Clin Oncol 27(34):5693–5699. doi:10.1200/JCO.2009.22.0962
Gonzalez-Angulo AM, Litton JK, Broglio KR, Meric-Bernstam F, Rakkhit R, Cardoso F, Peintinger F, Hanrahan EO, Sahin A, Guray M, Larsimont D, Feoli F, Stranzl H, Buchholz TA, Valero V, Theriault R, Piccart-Gebhart M, Ravdin PM, Berry DA, Hortobagyi GN (2009) High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. J Clin Oncol 27(34):5700–5706. doi:10.1200/JCO.2009.23.2025
Cancello G, Maisonneuve P, Rotmensz N, Viale G, Mastropasqua MG, Pruneri G, Montagna E, Dellapasqua S, Iorfida M, Cardillo A, Veronesi P, Luini A, Intra M, Gentilini O, Scarano E, Goldhirsch A, Colleoni M (2011) Prognosis in women with small (T1mic, T1a, T1b) node-negative operable breast cancer by immunohistochemically selected subtypes. Breast Cancer Res Treat 127(3):713–720. doi:10.1007/s10549-011-1465-7
Vaz-Luis I, Ottesen RA, Hughes ME, Mamet R, Burstein HJ, Edge SB, Gonzalez-Angulo AM, Moy B, Rugo HS, Theriault RL, Weeks JC, Winer EP, Lin NU (2014) Outcomes by tumor subtype and treatment pattern in women with small, node-negative breast cancer: a multi-institutional study. J Clin Oncol 32(20):2142–2150. doi:10.1200/JCO.2013.53.1608
Ignatov T, Eggemann H, Burger E, Costa SD, Ignatov A (2017) Management of small T1a/b breast cancer by tumor subtype. Breast Cancer Res Treat. doi:10.1007/s10549-017-4168-x
Parise CA, Bauer KR, Brown MM, Caggiano V (2009) Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999–2004. Breast Journal 15(6):593–602. doi:10.1111/j.1524-4741.2009.00822.x
Parise CA, Caggiano V (2014) Breast cancer survival defined by the ER/PR/HER2 subtypes and a surrogate classification according to tumor grade and immunohistochemical biomarkers. J Cancer Epidemiol 2014:469251. doi:10.1155/2014/469251
Fritz AG (2000) International classification of diseases for oncology: ICD-O, 3rd edn. World Health Organization, Geneva
Cancer reporting in California: abstracting and coding procedures for hospitals. California cancer reporting system standards, vol. I (2008). California Department of Public, Cancer Surveillance and Research Branch, Sacramento
ICD10Data.com. http://www.icd10data.com/. Accessed Jan 2016
DAKO (2003) HERCEPTest® Information Web site. Summary of Procedure. http://www.herceptin.com/herceptin/professional/testing/faqs.jsp. Accessed June 2006
PathVysion® (2002) HER-2 DNA Probe Kit Package Insert, vol. February. Vysis, Inc.
American Community Survey (2016) U.S. Department of Commerce, United States Census Bureau https://www.census.gov/programs-surveys/acs/. Accessed Jan 2016
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12(8):703–711
Clarke CA, Glaser SL, Keegan TH, Stroup A (2005) Neighborhood socioeconomic status and Hodgkin’s lymphoma incidence in California. Cancer Epidemiol Biomarkers Prev 14(6):1441–1447
Parikh-Patel A, Bates JH, Campleman S (2006) Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988–2000. Cancer 107(5 Suppl):1189–1195
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California Cancer Registry. Cancer 109(9):1721–1728
Zell JA, Rhee JM, Ziogas A, Lipkin SM, Anton-Culver H (2007) Race, socioeconomic status, treatment, and survival time among pancreatic cancer cases in California. Cancer Epidemiol Biomarkers Prev 16(3):546–552
Brown M, Tsodikov A, Bauer KR, Parise CA, Caggiano V (2008) The role of human epidermal growth factor receptor 2 in the survival of women with estrogen and progesterone receptor-negative, invasive breast cancer: the California Cancer Registry, 1999–2004. Cancer 112(4):737–747
Ou SH, Zell JA, Ziogas A, Anton-Culver H (2008) Low socioeconomic status is a poor prognostic factor for survival in stage I nonsmall cell lung cancer and is independent of surgical treatment, race, and marital status. Cancer 112(9):2011–2020
Yin D, Morris C, Allen M, Cress R, Bates J, Liu L (2010) Does socioeconomic disparity in cancer incidence vary across racial/ethnic groups? Cancer Causes Control 21(10):1721–1730
Telli ML, Chang ET, Kurian AW, Keegan TH, McClure LA, Lichtensztajn D, Ford JM, Gomez SL (2011) Asian ethnicity and breast cancer subtypes: a study from the California Cancer Registry. Breast Cancer Res Treat 127(2):471–478. doi:10.1007/s10549-010-1173-8
Parise CA, Bauer KR, Caggiano V (2012) Disparities in receipt of adjuvant radiation therapy after breast-conserving surgery among the cancer-reporting regions of California. Cancer 118(9):2516–2524
(2012) IBM SPSS Statistics for Windows, vol. 21.0. IBM Corp, Armonk
Subramaniam S, Bhoo-Pathy N, Taib NA, Tan GH, See MH, Jamaris S, Ho GF, Looi LM, Yip CH (2015) Breast cancer outcomes as defined by the estrogen receptor, progesterone receptor, and human growth factor receptor-2 in a multi-ethnic Asian country. World J Surg 39(10):2450–2458. doi:10.1007/s00268-015-3133-2
Izquierdo JN, Schoenbach VJ (2000) The potential and limitations of data from population-based state cancer registries. Am J Public Health 90(5):695–698
Parise CA, Caggiano V (2013) Disparities in race/ethnicity and socioeconomic status: risk of mortality of breast cancer patients in the California Cancer Registry, 2000–2010. BMC Cancer 13:449. doi:10.1186/1471-2407-13-449
Acknowledgements
We wish to thank Melissa Taylor and the staff at the Sutter Resource Library for their valuable assistance.
Disclaimer
The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract N01-PC-35136 awarded to the Northern California Cancer Center, contract N01-PC-35139 awarded to the University of Southern California, and contract N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement 1U58DP00807-01 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the authors and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Funding
This study was funded by Grant 947110-1107555 from the Sutter Medical Center Sacramento Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This research study involved analysis of existing data from the CCR without subject identifiers or intervention. Therefore, the study was categorized as exempt from institutional review board oversight.
Rights and permissions
About this article
Cite this article
Parise, C.A., Caggiano, V. Risk of mortality of node-negative, ER/PR/HER2 breast cancer subtypes in T1, T2, and T3 tumors. Breast Cancer Res Treat 165, 743–750 (2017). https://doi.org/10.1007/s10549-017-4383-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4383-5