Abstract
Mounting evidence suggests that neuronal PAS domain protein 2 (NPAS2) and other circadian genes are involved in tumorigenesis and tumor growth, possibly through their control of cancer-related biologic pathways. A missense polymorphism in NPAS2 (Ala394Thr) has been shown to be associated with risk of human tumors including breast cancer. The current study further examined the prognostic significance of NPAS2 in breast cancer by genotyping the Ala394Thr polymorphism and measuring NPAS2 expression. DNA extracted from 348 breast cancer tissue samples was analyzed for NPAS2 genotype using the TaqMan allelic discrimination assay. Of these, 287 also had total RNA available for use in real-time PCR assays to determine NPAS2 expression. NPAS2 genotypes and expression levels were analyzed for associations with prognostic outcomes, as well as correlations with clinical characteristics. A high level of NPAS2 expression was strongly associated with improved disease free survival (AHR = 0.43, 95% CI: 0.21–0.86, P trend = 0.022) and overall survival (AHR = 0.42, 95% CI: 0.19–0.96, P trend = 0.036). In addition, there was a borderline, but nonsignificant association between the NPAS2 genotype corresponding to Thr394Thr and disease free survival (AHR = 1.82, 95% CI: 0.96–3.46). The Ala/Ala, Ala/Thr, and Thr/Thr genotypes were also differentially distributed by tumor severity, as measured by TNM classification (χ 2 (6df, N = 344) = 14.96, P = 0.020). These findings provide the first evidence suggesting prognostic significance of the circadian gene NPAS2 in breast cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Circadian rhythm is the 24 h oscillation of many biologic and physiologic processes, such as cell division, proliferation, and metabolism [1, 2]. Circadian oscillations are maintained by transcriptional/posttranslational feedback loops among the core circadian genes [3]. Up to now, nine mammalian core circadian genes have been identified, which are expressed in the SCN as well as peripheral tissues [4]. NPAS2 is the largest circadian gene (176.68 kb) and is located on chromosome 2 at 2q11.2 [5]. It is a member of the basic helix-loop-helix (bHLH)-PAS family of transcription factors that is expressed in the mammalian forebrain and several peripheral tissues [5, 6]. NPAS2, an essential component of the feedback loop, dimerizes with ARNTL, another core circadian protein, and binds to DNA sequences to activate gene transcription [7, 8]. NPAS2/ARNTL heterodimer controls the transcription of two other circadian genes PER and CRY, which are required for maintaining biologic rhythms in many organisms [7–10].
Emerging data have demonstrated that NPAS2 has a substantial impact on tumor related biologic pathways, possibly through regulation of cancer-related genes, such as those involved in cell cycle checkpoint and DNA repair. In mice, the NPAS2/ARNTL heterodimer has been shown to bind to the promoter of the oncogene Myc and suppress its transcription [11]. Our functional assays have also demonstrated that NPAS2 affects cell cycle arrest and DNA repair, and an expression assay has further indicated that NPAS2 regulates the expression of critical genes in those processes [12].
NPAS2 is a conserved gene and has only one nonsynonymous polymorphism in its entire coding sequences, according to the NCBI dbSNP database. This SNP, an A to G coding polymorphism (dbSNP ID: rs2305160), results in a substitution at amino acid position 394 from alanine (Ala) to threonine (Thr). The Thr variants (Ala/Thr and Thr/Thr genotypes) have been previously shown to be associated with reduced risk of non-Hodgkin’s Lymphoma, especially B-cell lymphoma [13], while the Ala/Thr genotype has been associated with decreased risk of breast cancer [14], as well as reduced risk of prostate cancer [15].
As a potential tumor suppressor, NPAS2 expression could be deregulated in tumorigenesis. Expression of PER1 and PER2, two NPAS2 target genes, has been shown to be down-regulated in breast cancer compared to normal breast tissue [16, 17]. However, the expression of NPAS2 in cancer has yet to be determined. In addition, little is known about the genetic and expression variations of NPAS2 in relation to clinical characteristics of breast cancer. No association between circadian genes and cancer survival has been reported previously, apart from a very recent report showing that the combination of low CRY1 and low ARNTL expression was a prognostic factor in ovarian cancer, but either CRY1 or ARNTL alone was not associated with ovarian cancer survival [18]. To evaluate whether NPAS2 could be a potential marker to predict breast cancer prognosis, we analyzed NPAS2 genotype and phenotype (mRNA expression) using tissue samples from breast cancer patients in the current study.
Materials and methods
Breast cancer sample collection
Three hundred and forty eight patients who underwent surgery for primary breast cancer in the Department of Gynecologic Oncology at University of Turin between January 1998 and July 1999 were recruited into a clinical study of breast cancer. The study was approved by the university’s ethical review committee. Fresh tumor samples were collected from the patients during surgery. The tissue specimens were snap-frozen in liquid nitrogen immediately after resection and then stored at −80°C until analysis. Clinical and pathological information collected for the study includes age at surgery, tumor grade, tumor size, number of lymph nodes that tested positive for cancer, histologic type, postoperative treatment, and treatment response. Tumors were staged according to the TNM (Tumor classification, lymph Node status, and Metastases) classification system [19]. Patients were followed from surgery through Feb 2007. Follow-up was scheduled every 4 months for the first 2 years, every 6 months from year 3 to year 5, and once a year thereafter. The median follow-up time among the patients was 86.2 months, ranging from 8 to 108 months. During the follow-up, information on relapse and death was collected; 81 patients experienced relapse, and 60 died during the course of follow-up. The average age at surgery was 57 years, and the range was 23–83 years. REMARK (REporting recommendations for tumor MARKer prognostic studies) is a set of guidelines which establishes standards for reporting relevant details of tumor marker studies, including prespecified hypotheses, patient and specimen characteristics, assay methods, study design, data analysis, data presentation, and interpretation of the study findings [20]. The research design and data presentation of this study is adherent to REMARK guidelines.
Genotyping
Frozen tumor samples were pulverized manually in liquid nitrogen. Genomic DNA was extracted from approximately 100 mg of tissue powder following a standard phenol–chloroform protocol. The TaqMan assay was used to determine NPAS2 genotypes (C_15976652_10 for SNP rs2305160, Applied Biosystems, Inc., Foster City, CA). The assay was performed using PCR conditions of 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 60 s. Plates were then read by the ABI7500 instrument and data were analyzed by the allelic discrimination function of the Fast 7500 software (Applied Biosystems, Inc.). Determination of genotypes was performed independently by observers blinded to clinical data.
Real-time PCR
Pulverized tissue powders were also used for total RNA extraction following a standard phenol–chloroform protocol. The RNA samples were treated with DNase to remove genomic DNA contamination and were concentrated using the RNeasy MinElute Cleanup kit (Qiagen Inc., Valencia, CA). One microgram of total RNA from each sample was processed for conversion to cDNA using the Cloned AMV First-Strand cDNA Synthesis kit (Invitrogen, Carlsbad, CA).
cDNA samples from 287 patients were available to be used in the real-time PCR assay. Primers for NPAS2 (forward: TCTGGATCACAGAGCACCTC, reverse: CAGGAGCTCCAGGTCATCA) and hypoxanthine-guanine phosphoribosyltransferase (HPRT1) (forward: GGATATAAGCCAGACTTTGTTGG, reverse: CAAACATGATTCAAATCCCTGA), were designed in-house and chemically synthesized by Integrated DNA Technologies (IDT, Coralville, IA). Real-time PCR was performed in duplicate using the Power SYBR green master mix (Applied Biosystems, Inc.) on an ABI7500 Fast real-time PCR instrument (Applied Biosystems, Inc.). The PCR conditions included incubation at 95°C for 10 min to activate Taq polymerase, and 40 cycles of 94°C for 15 s, 57°C for 30 s, and 72°C for 30 s. In each sample, the expression of NPAS2 was normalized to the expression of the housekeeping gene HPRT1, and NPAS2 expression was quantified as 1,000 × 2−ΔCt. Calculation of NPAS2 expression levels from the real-time PCR data was independently performed by observers blinded to clinical data.
Statistical analysis
All statistical analyses were performed using the SAS statistical software, version 9.1 (SAS Institute Inc., Cary, NC). Associations of NPAS2 genotypes and expression with clinical characteristics, including age at surgery, histologic subtype, tumor size, lymph node involvement, tumor grade, and estrogen and progesterone receptor status were examined using the χ 2 test (for genotype) or analysis of variance (ANOVA, for expression). Hazard ratios (HR) with 95% confidence intervals (CI) were calculated using Cox proportional hazards regression analysis to examine the association of NPAS2 genotypes and expression levels with patient survival. An adjusted hazard ratio (AHR) with 95% CI was calculated from a Cox proportional hazards model that included age at diagnosis (continuous), TNM stage (4 categories), grade (3 categories), histologic subtype (2 categories), estrogen receptor (continuous) and progesterone receptor status (continuous). No variables used in the modeling violated the proportional hazards assumption, and no notable interactions were detected. P values <0.05 were considered statistically significant. Kaplan–Meier survival analysis was used to plot the proportion of the population that were alive (overall survival) or cancer-free (cancer-free survival) by the length of follow-up, in months.
Results
NPAS2 genotypes and expression were associated with clinical characteristics
There was no significant difference in NPAS2 expression by genotype at Ala394Thr (P = 0.704), and therefore NPAS2 expression was considered independent from its genotype at this particular locus. Distributions of the NPAS2 genotypes and mRNA expression by various clinical and pathological variables are shown in Table 1. A significant association was noted with tumor severity, as measured by TNM classification, with genotypes unequally distributed across the four TNM stages (χ 2 (6df, N = 344) = 14.96, P = 0.020). The vast majority of the patients were in PT1c and PT2 TNM stages (93%). The Ala/Thr and homozygous Thr/Thr genotypes were differentially distributed by tumor severity, as measured by TNM Classification of Malignant Tumors stage. The expression of NPAS2 was higher in lobular than ductal carcinomas. It was also higher in low grade tumors compared to high grade tumors (P = 0.021), and slightly higher in lymph node negative cases compared to lymph node positive cases (P = 0.079).
NPAS2 genotype Thr/Thr was associated with poor survival
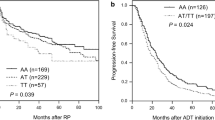
The adjusted survival analysis showed that there was a borderline, but not statistically significant association between the homozygous Thr/Thr genotype and poor disease-free survival compared to the Ala/Ala and Ala/Thr genotypes (AHR = 1.82, 95% CI: 0.96–3.46) (Table 2). The Thr/Thr genotype also appeared to be associated with poor overall survival compared to the Ala/Ala and Ala/Thr genotypes, although again, this association did not reach statistical significance (AHR = 1.78, 95% CI: 0.81–3.91). We further stratified the analysis by adjuvant treatments including adjuvant chemotherapy, adjuvant hormonal therapy, and both. However, no significant results were detected (data not shown). Kaplan–Meier survival analysis was also performed in order to generate survival curves (Fig. 1). There were no significant associations detected between NPAS2 genotypes and overall survival (P = 0.854) or disease-free survival (P = 0.679).
Kaplan–Meier survival analysis; a overall survival and b disease-free survival, by NPAS2 genotypes. The figure demonstrates the effect of the NPAS2 genotypes on survival (months) among breast cancer patients. The genotypes are Ala/Ala (homozygous wild type, n = 169); Ala/Thr (heterozygous, n = 134); and Thr/Thr (homozygous variant, n = 43). There were no significant associations detected between NPAS2 genotypes and overall survival (P = 0.854) or disease-free survival (P = 0.679)
High NPAS2 expression was associated with improved survival
Cox proportional hazards regression analysis was also performed for NPAS2 expression while adjusting for patient age at surgery, disease stage, tumor grade, histologic subtype, lymph node involvement, estrogen status, and progesterone status in the analysis. NPAS2 expression levels were grouped into three categories: low, medium, and high, based on the tertile distribution of NPAS2 expression among the control subjects. As shown in Table 2, high levels of NPAS2 expression were associated with better disease-free survival in both unadjusted and adjusted survival analyses (HR = 0.38, 95% CI: 0.19–0.75, P trend <0.001; and AHR = 0.43, 95% CI: 0.21–0.86, P trend = 0.022). A similar significant association between high NPAS2 expression and better overall survival was also observed (HR = 0.38, 95% CI: 0.17–0.86, P trend = 0.017; and AHR = 0.42, 95% CI: 0.19–0.96, P trend = 0.036). No significant results were detected (data not shown) if analyses were performed by stratifying the sample according to adjuvant treatments including adjuvant chemotherapy, adjuvant hormonal therapy, and both. Kaplan–Meier survival analysis was also performed, and survival curves are presented in Fig. 2. We found a borderline, but not statistically significant association between the level of NPAS2 expression and overall survival (P = 0.060), and a significant association with disease-free survival (P = 0.017).
Kaplan–Meier survival analysis; a overall survival and b disease-free survival, by levels of NPAS2 expression. The figure demonstrates the effect of the levels of NPAS2 expression on survival (months) among breast cancer patients. NPAS2 expression was grouped into three categories: low (n = 94), medium (n = 97), and high (n = 96), based on the tertile distribution of NPAS2 expression among the control subjects. The level of NPAS2 expression showed a borderline, but nonsignificant association with overall survival (P = 0.06), and was significantly associated with disease-free survival (P = 0.017)
Discussion
The genetic variant in NPAS2 (Ala394Thr) studied here, has previously been shown to be a susceptibility biomarker for human cancers in our earlier case–control studies [13–15]. The distribution of NPAS2 genotypes detected in the current group of breast cancer samples is similar to those previously reported [14]. Our previous findings suggest that the variant Thr allele might have a protective role in cancer development. However, the current results show that the homozygous Thr394Thr genotype is marginally associated with poorer disease-free survival in breast cancer patients. These findings, suggesting a protective role in tumor development, but a deleterious effect in terms of survival, could be due to the potential tumor suppressor role of the NPAS2 gene in cell cycle checkpoint and DNA damage response [7]. A pathway-based expression analysis of genes important for DNA damage signaling demonstrated that knockdown of NPAS2 significantly represses the expression of several cell cycle and DNA repair genes [12]. The Ala394Thr polymorphism is located in the PAS domain of NPAS2, which is a signal sensor domain and may affect protein sensory capacity or impede NPAS2/ARNTL heterodimerization [14]. Since the Thr allele is associated with protection from tumor initiation, this variant may enhance the tumor suppressor capacity of NPAS2 and facilitate DNA repair capacity. After tumor formation, however, tumor cells with high DNA repair capability are hard to destroy in tumor treatments and may cause poor survivorship. Our observations are also congruent with previous findings that genetic polymorphisms associated with increased cancer risk tend to be related to disease-free survival of cancer patients [21].
In addition to NPAS2 genotypes, our results demonstrated that high levels of NPAS2 expression are significantly associated with tumor grade, overall survival, and disease-free survival in breast cancer patients. These results, especially those relating high NPAS2 expression to small size, low grade, and lymph node negative tumors, suggest that high NPAS2 expression may have a protective role in breast cancer progression. Tumors with small size, low tumor grade, and negative lymph node involvement usually predict better survival, which could explain the observed correlation between high NPAS2 expression and better survival. Subgroup analyses were also done to explore the effects of adjuvant treatment on the relationship between NPAS2 and breast cancer survival and no significant associations were detected in any of the treatment subgroups. Since the sample size was quite small, subgroup analyses may not have sufficient power to detect any significant associations.
Although the molecular mechanisms for the role of NPAS2 in tumor progression are not clear, as a transcriptional regulator, NPAS2 may influence the expression of other cancer-relevant genes. NPAS2 binds to E-Box motifs of its target genes and may directly or indirectly affect circadian regulation and other cancer related pathways [22]. For example, the heterodimer of transactivators CLOCK or NPAS2 with ARNTL regulate the transcription of PER1, PER2, CRY1, and CRY2 [7]. Two of these circadian regulators, PER1 and PER2, have been linked to cell cycle and DNA damage response pathways [11]. Overexpression of either PER1 or PER2 in cancer cells inhibits their neoplastic growth and increases their rate of apoptosis. Loss or dysregulation of PER1 and PER2 expression has been found in many types of human cancer, and their expression levels are decreased in breast tumors relative to normal breast tissue [17]. Recently, it has also been shown that PER1, PER2, CRY2, CLOCK, and CSNK1E were all significantly down-regulated in ovarian cancer [18]. Decreased expression of circadian genes may result in disturbance of cell cycle regulation, and is correlated with tumor size [23]. On the other hand, overexpression of PER1 and PER2 may decrease cancer cell growth both in vitro and in vivo [24, 25], and induces apoptosis [26]. Given that NPAS2 positively controls PER1 and PER2 expression, high levels of NPAS2 expression may increase PER1 and PER2 expression and consequently decrease the growth of cancer cells. This could be one molecular explanation for the observed association between high levels of NPAS2 expression and better survival among breast cancer patients.
One potential limitation of this study is that a single sample, taken at one time point, was used to represent NPAS2 expression. The expression of circadian genes, including NPAS2, usually undergoes a daily oscillation. This raises a concern that this may not be representative of the NPAS2 expression levels, which are present at different stages of the circadian phase. However, cancer tissues are composed of heterogeneous populations of tumor cells that are not circadian synchronized. Recently, Tokunaga et al. showed that there was no relationship between tumor removal time and the expression level of circadian genes in ovarian tumor [18]. Furthermore, it has been determined that circulating breast tumor cells have no circadian rhythm [27]. As such, adjacent individual tumor cells may be in various stages of the circadian phase, and it is therefore appropriate to compare expression levels between patients, as any sample of tumor cells should represent the average expression for a given individual over all stages.
In summary, the findings from the current study indicate that the expression of NPAS2 may serve as a strong prognostic biomarker, and the genotype of NPAS2 may be a marginal prognostic biomarker, in addition to its association with breast cancer risk. This is one of the first reports relating expression levels of a circadian gene and cancer survival, and further examination of NPAS2 and other circadian genes as prognostic biomarkers in additional cancer types is warranted.
References
Vansteensel MJ, Michel S, Meijer JH (2008) Organization of cell and tissue circadian pacemakers: a comparison among species. Brain Res Rev 58:18–47
Kohsaka A, Bass J (2007) A sense of time: how molecular clocks organize metabolism. Trends Endocrinol Metab 18:4–11
Ko CH, Takahashi JS (2006) Molecular components of the mammalian circadian clock. Hum Mol Genet 15(Spec No 2):R271–R277
Kaeffer B, Pardini L (2005) Clock genes of mammalian cells: practical implications in tissue culture. In Vitro Cell Dev Biol Anim 41:311–320
Zhou YD, Barnard M, Tian H, Li X, Ring HZ, Francke U, Shelton J, Richardson J, Russell DW, McKnight SL (1997) Molecular characterization of two mammalian bHLH-PAS domain proteins selectively expressed in the central nervous system. Proc Natl Acad Sci U S A 94:713–718
Gilles-Gonzalez MA, Gonzalez G (2004) Signal transduction by heme-containing PAS-domain proteins. J Appl Physiol 96:774–783
Chen-Goodspeed M, Lee CC (2007) Tumor suppression and circadian function. J Biol Rhythms 22:291–298
Reick M, Garcia JA, Dudley C, McKnight SL (2001) NPAS2: an analog of clock operative in the mammalian forebrain. Science 293:506–509
Vitaterna MH, King DP, Chang AM, Kornhauser JM, Lowrey PL, McDonald JD, Dove WF, Pinto LH, Turek FW, Takahashi JS (1994) Mutagenesis and mapping of a mouse gene, clock, essential for circadian behavior. Science 264:719–725
Bunger MK, Wilsbacher LD, Moran SM, Clendenin C, Radcliffe LA, Hogenesch JB, Simon MC, Takahashi JS, Bradfield CA (2000) Mop3 is an essential component of the master circadian pacemaker in mammals. Cell 103:1009–1017
Fu L, Pelicano H, Liu J, Huang P, Lee C (2002) The circadian gene Period2 plays an important role in tumor suppression and DNA damage response in vivo. Cell 111:41–50
Hoffman AE, Zheng T, Ba Y, Zhu Y (2008) The circadian gene NPAS2, a putative tumor suppressor, is involved in DNA damage response. Mol Cancer Res 6:1461–1468
Zhu Y, Leaderer D, Guss C, Brown HN, Zhang Y, Boyle P, Stevens RG, Hoffman A, Qin Q, Han X, Zheng T (2007) Ala394Thr polymorphism in the clock gene NPAS2: a circadian modifier for the risk of non-Hodgkin’s lymphoma. Int J Cancer 120:432–435
Zhu Y, Stevens RG, Leaderer D, Hoffman A, Holford T, Zhang Y, Brown HN, Zheng T (2008) Non-synonymous polymorphisms in the circadian gene NPAS2 and breast cancer risk. Breast Cancer Res Treat 107:421–425
Chu LW, Zhu Y, Yu K, Zheng T, Yu H, Zhang Y, Sesterhenn I, Chokkalingam AP, Danforth KN, Shen MC, Stanczyk FZ, Gao YT, Hsing AW (2008) Variants in circadian genes and prostate cancer risk: a population-based study in China. Prostate Cancer Prostatic Dis 11:342–348
Chen ST, Choo KB, Hou MF, Yeh KT, Kuo SJ, Chang JG (2005) Deregulated expression of the PER1, PER2 and PER3 genes in breast cancers. Carcinogenesis 26:1241–1246
Winter SL, Bosnoyan-Collins L, Pinnaduwage D, Andrulis IL (2007) Expression of the circadian clock genes Per1 and Per2 in sporadic and familial breast tumors. Neoplasia 9:797–800
Tokunaga H, Takebayashi Y, Utsunomiya H, Akahira JI, Higashimoto M, Mashiko M, Ito K, Niikura H, Takenoshita SI, Yaegashi N (2008) Clinicopathological significance of circadian rhythm-related gene expression levels in patients with epithelial ovarian cancer. Acta Obstet Gynecol Scand:1–11
Sobin LH, Fleming ID (1997) TNM Classification of Malignant Tumors, fifth edition. Union Internationale Contre le Cancer and the American Joint Committee on Cancer. Cancer, 80:1803-1804
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235
Choi JY, Lee KM, Park SK, Noh DY, Ahn SH, Chung HW, Han W, Kim JS, Shin SG, Jang IJ, Yoo KY, Hirvonen A, Kang D (2005) Genetic polymorphisms of SULT1A1 and SULT1E1 and the risk and survival of breast cancer. Cancer Epidemiol Biomarkers Prev 14:1090–1095
Mukaiyama Y, Uchida T, Sato E, Sasaki A, Sato Y, Igarashi J, Kurokawa H, Sagami I, Kitagawa T, Shimizu T (2006) Spectroscopic and DNA-binding characterization of the isolated heme-bound basic helix-loop-helix-PAS-A domain of neuronal PAS protein 2 (NPAS2), a transcription activator protein associated with circadian rhythms. FEBS J 273:2528–2539
Lin YM, Chang JH, Yeh KT, Yang MY, Liu TC, Lin SF, Su WW, Chang JG (2008) Disturbance of circadian gene expression in hepatocellular carcinoma. Mol Carcinog 47:925–933
Lee CC (2006) Tumor suppression by the mammalian Period genes. Cancer Causes Control 17:525–530
Hua H, Wang Y, Wan C, Liu Y, Zhu B, Wang X, Wang Z, Ding JM (2007) Inhibition of tumorigenesis by intratumoral delivery of the circadian gene mPer2 in C57BL/6 mice. Cancer Gene Ther 14:815–818
Hua H, Wang Y, Wan C, Liu Y, Zhu B, Yang C, Wang X, Wang Z, Cornelissen-Guillaume G, Halberg F (2006) Circadian gene mPer2 overexpression induces cancer cell apoptosis. Cancer Sci 97:589–596
Garcia-Saenz JA, Martin M, Maestro M, Vidaurreta M, Veganzones S, Villalobos L, Rodriguez-Lajusticia L, Rafael S, Sanz-Casla MT, Casado A, Sastre J, Arroyo M, Diaz-Rubio E (2006) Circulating tumoral cells lack circadian-rhythm in hospitalized metastasic breast cancer patients. Clin Transl Oncol 8:826–829
Acknowledgments
This work was supported by the US National Institutes of Health (grant CA122676 and CA110937).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yi, C., Mu, L., de la Longrais, I.A.R. et al. The circadian gene NPAS2 is a novel prognostic biomarker for breast cancer. Breast Cancer Res Treat 120, 663–669 (2010). https://doi.org/10.1007/s10549-009-0484-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-009-0484-0