Abstract
In order to analyze the clinicopathological features of Chinese triple negative tumors, we performed a retrospective study of 1993 female unilateral breast cancer patients undergoing surgery in Cancer Hospital of Fudan University, Shanghai, China. Survival curves were performed with Kaplan–Meier method and annual recurrence hazard was estimated by hazard function. We observed that the rate of larger tumors in triple negative patients was higher than that in HR+/ERBB2− women, but lower than that in ERBB2+ subgroup (P = 0.0001). In addition, 21.83% of triple negative patients had four or more axillary lymph nodes involved as compared to 27.40% of ERBB2+ women and 22.75% of HR+/ERBB2− subgroup (P = 0.0056). In the survival analysis, we found a statistical significance for recurrence-free survival (RFS) among the three subgroups (P = 0.0037), with the rate of 72.89% for ERBB2+ patients, 78.40% for HR+/ERBB2− ones and 75.76% for triple negative ones at the 11th year respectively. When it came to hazard peaks, discrepancies existed in different subgroups. Similar to HR+/ERBB2− patients, triple negative subgroup showed an early major recurrence surge peaking at approximately year 2.5 as opposed to ERBB2+ counterparts with a tapering sharp at the 1st year. Furthermore, the first peak of triple negative tumors was higher than that of HR+/ERBB2− patients, but lower than that of ERBB2+ ones. Therefore, our findings suggested biological characteristics and prognostic outlook of Chinese triple negative breast cancers might be more favorable and somewhat different from those in Western populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the aging of society and changes of lifestyle, the incidence of breast cancer remains to increase all over the world, especially in developing countries including China [1]. However, the mortality rate has seen a dramatic decline mainly due to the introduction of adjuvant systemic therapy [2]. As an indispensable component of it, targeted treatment has revealed its striking effect on the improvement of breast cancer prognosis [3–6]. Despite the unfailing emergence of targeted agents, a significant subgroup of patients derives little benefit, whose breast cancer features absent expression of estrogen, progesterone and ERBB2 receptors, namely “triple negative”.
Triple negative category accounts for 10–15% of breast cancers [7], which is characterized by aggressive clinical history. An extensive body of literature has reported that this subgroup was associated with shorter survival times [8–15] and even exhibited a trend towards a poorer outcome compared with ERBB2+ phenotype [9, 15]. Furthermore, a higher percentage of visceral metastases, local relapse and cerebral metastases arose in triple negative breast cancers than that in non-triple negative counterparts, while the incidence of bone metastases was just the opposite [12, 16, 17]. On the other hand, the use of trastuzumab and lapatinib has led to considerable reduction in the recurrence or mortality risk of ERBB2+ patients [4], which may render the triple negative women at most risk of early recurrence.
However, few studies have been conducted among non-western populations. Kurebayashi and coworkers reported the survival by each subtype in Japanese breast cancer patients that ERBB2+ and luminal A subgroup remained to live shortest and longest respectively before metastatic disease occurred, whereas the curves for triple negative and luminal B phenotype were mostly intermediate and virtually superimposable for disease-free survival (DFS) as well as for overall survival (OS), with a highly significant difference between subclasses (P < 0.001 for both DFS and OS) [18]. Despite controversies, these conflicting results provide evidence for an increasing recognition that breast cancer is a heterogeneous disease categorized as different subtypes with distinct biological characteristics [9]. Therefore, it is most urgent for further investigation on the prognosis of triple negative breast cancer in Chinese patients due to the unavailability of similar data.
In most studies, prognosis was generally delineated by survival curves rather than hazard function. In the former, the cumulative event-free time distribution is usually illustrated to describe the proportion of patients who remain event-free at a given time after primary therapy, which results in the lack of insight into changes of the event probability over time. However, the hazard function is capable of highlighting such information as the risk of event at any instant among the remaining ‘at risk’ individuals. It depicts not only the timing but also the magnitude of the hazard rate [19].
In recent years, there is an increasing number of investigators who have become intrigued in the hazard function. The applicability of this method has been described in clinical trials, as exemplified by serial reports of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial. These data clearly substantiate the long-term benefit in risk reduction for anastrozole over tamoxifen throughout the entire follow-up period [20, 21]. Therefore, the hazard function is of extraordinary value in prognostic evaluation, contributing to strategy development of both treatment and follow-up. However, the prognostic pattern for triple negative breast cancer has not been well studied by use of the hazard function, which has been a major shortcoming in probing the full complexities of this category. It is noteworthy that, due to the dearth of therapeutic targets and follow-up measures at present, this disease entity is a much-feared diagnosis among the majority of patients with breast cancer [7]. In consequence, the profound understanding of recurrence hazard for triple negative tumors will most likely lead to a shift in how we deal with such patients.
On the basis of the above points, we carried out a retrospective analysis on the clinicopathological features of triple negative breast cancer patients undergoing surgery in Cancer Hospital of Fudan University, Shanghai, China. Considering the heterogeneity of breast cancer, we sought to gather relevant information so as to get a clear picture of the prognosis for Chinese patients with triple negative phenotype and its discrepancies from other populations, accordingly, offering the implications for the underlying distinction in tumor biology between different subgroups and various races.
Materials and methods
Patients
This study was conducted retrospectively from a large database of patients undergoing surgery from January 1, 1991 to December 31, 2003 in Cancer Hospital of Fudan University, Shanghai, China. Before surgery all patients were evaluated through complete physical examination, chest radioscopy, bilateral mammography, ECG, ultrasonography of breasts, axillary fossa, cervical parts, abdomen, and pelvis, complete blood count, and routine biochemical tests. After exact staging, each patient was treated with lumpectomy or mastectomy followed by adjuvant therapy according to the standards used at the time of surgery. Follow-up information regarding tumor recurrences and survival status was accomplished through the retrieve of follow-up medical records kept in the outpatient department, personal contact with the patient as well as the assistance of Shanghai Center for Disease Control and Prevention (CDC). Thereinto, personal contact with the patient referred to routine correspondence or telephone visits, which were carried out in Cancer Hospital of Fudan University every 3 months during the first two years, every 6 months during the next two years and once a year thereafter. Recurrence or its absence was diagnosed by query to the patient, by biopsy, or by scan of bone, chest, abdomen, pelvis or skull. Whenever the tumor recurred, additional information, including sites of recurrence and therapy, was requested. All data were entered into a computerized database and verified to minimize errors in data entry.
Similar to other relevant reports [22, 23], 1993 patients were included in our study if they met all of the following criteria: female gender, an initial diagnosis of unilateral primary breast cancer without distant metastases, at least 3 months of follow-up information for disease recurrence and death, and available information on age, tumor size, number of involved axillary lymph nodes (ALN), status of estrogen receptor (ER), progesterone receptor (PR) as well as ERBB2. The mean age at diagnosis was 52 years old (range 16–90). Median follow-up was 2.81 years, ranging from 3 months to 11 years. Among them, 1696 (85.10%) were administered adjuvant chemotherapy of different regimens for 4–6 cycles. Out of 1391 patients with positive ER and/or PR (ER/PR), 696 (50.04%) received adjuvant endocrine therapy, among whom 681 took tamoxifen and 15 aromatase inhibitors. None of the patients received trastuzumab.
Immunohistochemistry and scoring
For each patient in our database, ER, PR, ERBB2, TP53 and Cathepsin-D status were determined by immunohistochemical staining, which was carried out as a standard operating procedure in the pathology department of Cancer Hospital, Fudan University. All primary monoclonal antibodies were from Dako. For TP53 worthy of note, the antibody labels both wild- and mutant-type of the p53 protein. The percentage and the intensity of tumor cells stained were assessed by at least two pathologists, and were denoted respectively as a proportion score and an intensity score. The former was interpreted as follows: a score of 0 required no staining seen, 1 required ≤25% of cells positive, 2 required 25–50% of cells stained, 3 required 50–75% of positive cells and 4 required >75% of staining cells. As to the intensity score, a negative result was defined as a score of 0, weakly positive as 1, moderately positive as 2, and strongly positive as 3. The final score was calculated as the product of the proportion score and the intensity score. Thereby, staining results ranged from score 0 to 12. This semiquantitative scoring system for nuclear ER, PR, TP53 and plasma Cathepsin-D were defined as negative for score 0 and as positive for scores of 1–12 with staining of carcinoma cells, whereas ERBB2 status was defined as negative for scores of 0–8 (namely, 0, 1+ and 2+ in the DAKO scoring system) and as positive for strong membranous staining with scores of 9–12 (namely DAKO score 3+).
Statistical analysis
Recurrence-free survival (RFS) was defined as the time from surgery to the earliest occurrence of relapse (locoregional or distant) or death from any cause. Those without any evidence of relapse were censored at the last date they were known to be alive. Clinicopathologic parameters were compared between different subgroups using one-way analysis of variance (ANOVA) test for continuous variables, chi-square test for unordered categorical variables and nonparametric Kruskal–Wallis rank test for ordinal categorical variables. Post hoc multiple comparison tests were conducted with the Bonferroni method.
Survival distributions were estimated by the Kaplan–Meier product-limit method and were compared using the log-rank test. Cox proportional hazards regression and time dependent Cox non-proportional hazards regression were applied to modeling the relationship between subgroup and RFS, adjusted for known prognostic variables, including tumor size (≤2 cm, >2 cm), ALN status (0, 1–3, ≥4), TP53 (negative and positive) and Cathepsin-D (negative and positive) expression as well as use of adjuvant chemotherapy (yes, no) and endocrine therapy (yes, no). The proportional hazards assumption was tested by global test [24, 25]. For graphical display of RFS, annual hazard rates were estimated using a Kernel method of smoothing. All statistical tests were two sided and P < 0.05 was considered significant. All statistical analyses were performed with Stata statistical software package (release 9.0; Stata Corporation, College Station, Texas, USA). Relative risks (RRs) were presented with their 95% confidence intervals (CIs).
Considerable evidence revealed that many covariate effects on recurrence risk were time-varying, that is, they were not proportional throughout the entire follow-up interval [26–31]. Accordingly, several estimates such as RRs were further compared within different time frames (i.e. 0–2 years from surgery and from 2 years to the end of the follow-up period).
Results
General characteristics
According to different combinations of hormone receptor (HR) and ERBB2 status, 1993 patients were categorized into the three subgroups as follows: ERBB2+ (32.41%), HR+/ERBB2− (48.97%, HR+ referred to ER+ or PR+) and triple negative (18.62%). ERBB2+ patients tended to be younger at diagnosis than HR+/ERBB2− and triple negative counterparts, although there was no statistical significance (51.4, 52.8 and 52.4 respectively, P > 0.05; Table 1). The rate of larger tumors (greater than 2 cm in diameter) in triple negative patients was moderately higher than that in HR+/ERBB2− women, but much lower than that in ERBB2+ subgroup (70.35%, 66.19% and 76.32% respectively, P = 0.0001; Table 1). In addition, 21.83% of patients whose tumors were triple negative had four or more nodes involved in the axilla as compared to 27.40% of patients with ERBB2+ tumors and 22.75% of those with HR+/ERBB2− tumors (P = 0.0056; Table 1). We made further analysis with post hoc multiple comparison (Bonferroni) tests, which demonstrated that statistical difference was discerned between ERBB2+ and triple negative tumors rather than between HR+/ERBB2− and triple negative breast cancers (data not shown) in terms of ALN status. Such was also the distribution of TP53 expression and Cathepsin-D status (Table 1; part of data not shown). When it came to histologic grade, triple negative and ERBB2+ patients were more likely to have grade III tumors than HR+/ERBB2− subgroup (33.54% and 34.36% vs. 20.35%, P = 0.0001; Table 1).
Initial symptoms varied from one subgroup to another. In comparison with HR+/ERBB2− and triple negative patients, nipple-related symptoms such as nipple discharge, nipple indrawn or changed accounted for a higher proportion in ERBB2+ women, whereas intramammary symptoms including a breast lump and breast pain were just the opposite (P = 0.029; Table 1).
Subgroups also influenced the proportion and timing of recurrence. When compared with triple negative tumors, more recurrence events were observed in ERBB2+ patients but less in HR+/ERBB2− ones (P = 0.002; Table 1). Besides, 71.91% recurrence occurred in ERBB2+ subgroup within two years of follow-up, while the corresponding rates for HR+/ERBB2− and triple negative subgroups were 57.32% and 47.37% respectively (P = 0.019).
Survival analysis
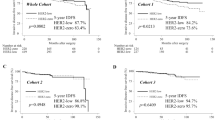
In the univariate analysis, we found significantly different recurrence-free survivals (RFS) among the three subgroups throughout the entire follow-up period (P = 0.0037; Table 2), with the rate of 72.89% for ERBB2+ tumors, 78.40% for HR+/ERBB2− tumors and 75.76% for triple-negative tumors at the 11th year respectively (Fig. 1). A similar effect remained to be validated till 2 years from surgery (P < 0.0001; Table 3), yet failed to be sustained for the interval from 2 years after surgery to the end of follow-up (P = 0.4539; Table 3).
In Cox proportional hazards regression analysis, we found that tumor size (P = 0.013; RR = 1.863, 95% CI 1.138–3.048), ALN status (P < 0.0001; RR = 2.508, 95% CI 2.007–3.133), use of adjuvant chemotherapy (P = 0.001; RR = 0.422, 95% CI 0.251–0.708) and endocrine therapy (P = 0.002; RR = 0.546, 95% CI 0.370–0.807)were independent prognostic factors for RFS excluding subgroup (P = 0.099; RR = 0.867, 95% CI 0.731–1.060; Table 2) during the period from the beginning to the end of follow-up. To further evaluate whether prognostic effect of subgroup remained unabated over time, the test for lack of proportionality was performed [24, 25]. However, it was statistically significant (global test, P = 0.0084), which clarified a violation of proportional hazards for subgroup and hinted at a demand for the employment of Cox non-proportional hazards regression rather than Cox proportional hazards regression in this analysis. In time dependent Cox model, subgroup (P = 0.026; RR = 0.758, 95% CI 0.593–0.968) as well as tumor size (P = 0.014; RR = 1.860, 95% CI 1.136–3.043), ALN status (P < 0.0001; RR = 2.502, 95% CI 2.002–3.126), use of adjuvant chemotherapy (P = 0.001; RR = 0.425, 95% CI 0.253–0.714) and endocrine therapy (P = 0.003; RR = 0.551, 95% CI 0.373–0.814; Table 2) were included when subgroup was taken as an time-varying covariate. To identify the optimal cutoff point for time-varying pattern of subgroup, we examined all the time points in the unit of follow-up year. As expected, women with triple negative breast cancers had a significantly increased likelihood of recurrence within 2 years after surgery (P = 0.004; RR = 0.716, 95% CI 0.571–0.897) rather than thereafter (P = 0.446; RR = 1.111, 95% CI 0.847–1.457; Table 3).
Recurrence hazard analysis
As to hazard peaks, discrepancies existed in different subgroups. Triple negative patients showed an early major recurrence surge peaking at the 2.5th year after surgery, followed by a gradual decline until year 6.5 and then a modest increase. As to HR+/ERBB2− patients, the hazard plot exhibited a wide initial plateau-like wave covering at least 4 years and a subsequent rise from approximately the 8th year. The hazard rate for ERBB2+ patients displayed a tapering sharp at the 1st year, accompanied with a second ridge at year 5.5 as well as a quite similar pattern to triple negative counterparts thereafter. Furthermore, the first peak of triple negative tumors was higher than that of HR+/ERBB2− patients, but lower than that of ERBB2+ ones (Fig. 2).
Discussion
Our study is, to the best of our knowledge, the largest retrospective analysis on clinicopathological features of the triple negative tumors in Chinese breast cancer patients. According to Carey et al., the triple negative subtype occurred with a higher incidence in pre-menopausal African American women (39%) when compared to post-menopausal African American women (14%) and non-African American women of any age (16%) in the Carolina Breast Cancer Study, a population-based, case–control study [13]. Additionally, 87 out of 149 (59%) patients were identified as triple negative in a random cohort of Nigerians [32]. By contrast, there was a rather lower frequency of triple negative tumors (8–14%) in Japanese patients [18, 33]. In this analysis, triple negative tumors accounted for 18.62% among all types of Chinese breast cancer, which was much similar to Japanese series. Therefore, the prevalence of triple negative breast cancers seemed to differ by race as had been suggested by other studies [13, 34]. Whether this racial preference is attributed to genetic or environmental factors, or to a combination of both still remains unclear and open to investigation [7].
Both tumor size and ALN status have been accepted as sufficiently established to guide risk allocation [35, 36]. In addition, TP53 together with Cathepsin-D is somewhat indicative of prognosis despite inadequate evidence for routine use in clinical practice [37]. We detected a moderate rate of larger tumors as well as a low percentage of positive ALN status, TP53 and Cathepsin-D staining in triple negative category, contributing to its better survival compared with ERBB2+ phenotype. However, these findings were discordant with western reports, which demonstrated relatively large tumors, slightly more nodes involved [10] and high p53 protein expression [38] in triple negative cancers, accordingly, well elucidating the corresponding aggressive biological behavior and poor clinical outcomes [8, 10, 11, 14]. This absolute disagreement mirrored the fact that breast cancer is a disease of heterogeneity, and therefore, race, as an important, even pivotal factor, should be taken into account when talking of clinicopathological features for triple negative tumors.
The triple negative breast cancers in this study were more prone to presenting with intramammary symptoms than nipple-related ones at diagnosis. It has been reported that the type of initial symptom was related to delay in seeking for medical care. Breast lump or breast pain were more likely to be recognized by women as a symptom provoking their eventual attendance to a doctor [39–41]. Besides, several researches substantiated that a longer time period before visiting the doctor was linked to a shorter survival from breast cancer [42, 43]. By this token, patients’ interpretation of initial symptom might also exert an indirect impact on prognosis, which was quite congruent with our observations.
At present, much enthusiasm has been aroused for triple negative breast cancers due not only to tricky treatments but also to poor prognosis. In terms of survival, the previous studies were almost confined to western populations [8, 10–12, 14, 15]. Besides racial disparities, subgroup taxonomy should not be ignored either when comparing survival data between different series. In the majority of studies, subgroup as an explanatory variable was dichotomized as triple negative or the other breast cancers [10–12, 14, 44], which featured clarity and uniformity but obscured diversity and complexity. By contrast, it was capable of uncovering much fuller prognostic profiles in a multichotomized way. Herein existed slight differences of note. Some researchers divided subgroup mainly into HR+, ERBB2+/HR− and triple negative phenotypes [13, 15, 18]. This classification was more or less concordant with intrinsic molecular subtypes defined by microarray; nevertheless, it was not a perfect way. ERBB2 amplification, as a powerful prognostic marker [45], has been identified to confer a strong negative effect on survival in untreated ER+ patients [46]. And further, no significant difference in disease-free survival (DFS) was observed between patients with and without tamoxifen treatment for those co-expressing HR and ERBB2 [46, 47], which validated the in vitro findings that ERBB2 overexpression compromised the antitumor effect of tamoxifen [48–51]. Taken together, all of these data inferred that ERBB2 status added prognostic information in HR+ breast cancer patients regardless of ET, corroborating that HR+/ERBB2+ tumors constituted a clinical entity with poor outcome separated from HR+/ERBB2− counterparts [46, 52, 53]. Based on the superiority of the ERBB2 status to HR as a prognostic factor in breast cancer [54], subgroup was classified into ERBB2+, HR+/ERBB2− and triple negative in this study just as other few publications [8]. Our results indicated that RFS for triple negative category was obviously superior to that for ERBB2+ patients but relatively inferior to that for HR+/ERBB2− subgroup, which was totally coherent with Nielson’s report [8] and partly consistent with others studies [13, 15, 18, 34].
There is growing attention toward violations of proportional hazards. Failure to recognize the patterns of time-variation might miss the effects of clinically important or biologically interesting factors [24]. Valid conclusions for early prognostic effects can be yielded with short follow-up, whereas those for late effects fail to be verified without longer follow-up, as represented by HR status [24]. Our analysis indicated that the recurrence risk for triple negative subgroup was not proportional across the time, which was consistent with previous reports [10]. Alertly detecting and explicitly modeling time-dependence, which may be a more common phenomenon than is appreciated in the medical literature, could conduce to novel biological insights and clinical use of various factors [24].
Up to now, there is no universally agreed-upon pattern of recurrence risk for triple negative patients owing to little information [10]. Moreover, such pattern had not yet been reported in Chinese populations. Dent and colleagues [10] found a single peak reaching the maximum at about 1 year after diagnosis for patients with triple negative breast cancers, as distinguished from a steady risk of recurrence spanning 17 years after diagnosis for those with other cancers [10]. It was slightly discrepant from their report that we demonstrated double-peaked time distribution of recurrence risk irrespective of subgroup and intermediate recurrence pattern for triple negative tumors between that for ERBB2+ and HR+/ERBB2− counterparts, since the first peak for triple negative subgroup lied between those for ERBB2+ and HR+/ERBB2− ones with regard to both timing and height. On this premise, prognosis for Chinese triple negative patients seemed somewhat better than that for Western counterparts. Despite contradictory results, there is no denying the fact that the risk of recurrence or death persists for a long duration, even for years or decades after surgery, which has been supported by manifold data [22, 27, 55–57].
This study has some potential and inevitable limitations on account of its retrospective nature. Recurrences are probably somewhat underreported or misinformed for a substantial portion of the patients in this database; nonetheless, underreporting or misinformation of recurrences would have not varied by clinicopathological parameters [51]. Besides, we did not evaluate the effect of treatment on survival in the present study, but all the RRs were adjusted for treatment administered [10].
In conclusion, biological behavior and clinical outcome for triple negative tumors in Chinese breast cancer patients may be more favorable and somewhat different from those in Western populations. However, this does not mean the unnecessity of aggressive treatment for these patients as the sustained existence of recurrence risk should also be taken seriously. Although there is to date no specific systemic regimen for recommendation due to little data on which to base treatment selection [7], this treatment bottle-neck have prompted a better knowledge of triple negative category to shed more light on efficacious ways of post-operative management, including both treatment and follow-up [58].
References
Jemal A, Siegel R, Ward E et al (2007) Cancer statistics, 2007. CA Cancer J Clin 57:43–66
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365:1687–1717. doi:10.1016/S0140-6736(05)66544-0
Joensuu H, Kellokumpu-Lehtinen PL, Bono P et al (2006) Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med 354:809–820. doi:10.1056/NEJMoa053028
Romand EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684. doi:10.1056/NEJMoa052122
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672. doi:10.1056/NEJMoa052306
Slamon D, Eiermann W, Robert N et al (2005) Phase III randomized trial comparing doxorubicin and cyclophosphamide followed by docetaxel (AC→T) with doxorubicin and cyclophosphamide followed by docetaxel and trastuzumab (AC→TH) with docetaxel, carboplatin and trastuzumab (TCH) in HER2 positive early breast cancer patients: BCIRG 006 study. Paper presented at the 28th San Antonio Breast Cancer Symposium, Henry B. Gonzalez Convention Center, San Antonio, Texas, USA, 8–11 December 2005
Cleator S, Heller W, Coombes RC (2007) Triple-negative breast cancer: therapeutic options. Lancet Oncol 8:235–244. doi:10.1016/S1470-2045(07)70074-8
Nielsen TO, Hsu FD, Jensen K et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5374. doi:10.1158/1078-0432.CCR-04-0220
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874. doi:10.1073/pnas.191367098
Dent R, Trudeau M, Pritchard KI et al (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13:4429–4434. doi:10.1158/1078-0432.CCR-06-3045
Bauer KR, Brown M, Cress RD et al (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer 109:1721–1728. doi:10.1002/cncr.22618
Rodriguez-Pinilla SM, Sarrio D, Honrado E et al (2006) Prognostic significance of basal-like phenotype and fascin expression in node-negative invasive breast carcinomas. Clin Cancer Res 12:1533–1539. doi:10.1158/1078-0432.CCR-05-2281
Carey LA, Perou CM, Livasy CA et al (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502. doi:10.1001/jama.295.21.2492
Banerjee S, Reis-Filho JS, Ashley S et al (2006) Basal-like breast carcinomas: clinical outcome and response to chemotherapy. J Clin Pathol 59:729–735. doi:10.1136/jcp. 2005.033043
Carey LA, Dees EC, Sawyer L et al (2004) The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 15:2329–2334
Haffty BG, Yang Q, Reiss M et al (2006) Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol 24:5652–5657. doi:10.1200/JCO.2006.06.5664
Chang BW, Decker RH, Haffy BG et al (2007) Incidence of brain metastases in early-stage triple negative breast cancer patients. Paper presented at the 49th American Society for Therapeutic Radiology and Oncology (ASTRO) Annual Meeting, Los Angeles, California, USA, 28 October–1 November 2007
Kurebayashi J, Moriyab T, Ishidad T et al (2007) The prevalence of intrinsic subtypes and prognosis in breast cancer patients of different races. Breast 16:S72–S77. doi:10.1016/j.breast.2007.07.017
Simes RJ, Zelen M (1985) Exploratory data analysis and the use of the hazard function for interpreting survival data: an investigator’s primer. J Clin Oncol 3:1418–1431
Howell A on behalf of the ATAC Trialists’ Group (2005) Author’s reply. Lancet 365:1225–1226
The Arimidex T Alone or in Combination (ATAC) Trialists’ Group (2008) Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 100-month analysis of the ATAC trial. Lancet Oncol 9:45–53. doi:10.1016/S1470-2045(07)70385-6
Jatoi I, Tsimelzon A, Weiss H et al (2005) Hazard rates of recurrence following diagnosis of primary breast cancer. Breast Cancer Res Treat 89:173–178. doi:10.1007/s10549-004-1722-0
McShane LM, Altman DG, Sauerbrei W et al (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100:229–235. doi:10.1007/s10549-006-9242-8
Hilsenbeck SG, Ravdin PM, de Moor CA et al (1998) Time-dependence of hazard ratios for prognostic factors in primary breast cancer. Breast Cancer Res Treat 52:227–237. doi:10.1023/A:1006133418245
Grambsch PM, Therneau TM (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81:515–526. doi:10.1093/biomet/81.3.515
Hupperets PS, Volovics L, Schouten LJ et al (1997) The prognostic significance of steroid receptor activity in tumor tissues of patients with primary breast cancer. Am J Clin Oncol 20:546–551. doi:10.1097/00000421-199712000-00002
Saphner T, Tormey DC, Gray R (1996) Annual hazard rates of recurrence for breast cancer after primary therapy. J Clin Oncol 14:2738–2746
Schmitt M, Thomssen C, Ulm K et al (1997) Time-varying prognostic impact of tumour biological factors urokinase (uPA), PAI-1 and steroid hormone receptor status in primary breast cancer. Br J Cancer 76:306–311
Hahnel R, Spilsbury K (2004) Oestrogen receptors revisited: long-term follow up of over five thousand breast cancer patients. ANZ J Surg 74:957–960. doi:10.1111/j.1445-1433.2004.03215.x
Zahl PH, Tretli S (1997) Long-term survival of breast cancer in Norway by age and clinical stage. Stat Med 16:1435–1449. doi :10.1002/(SICI)1097-0258(19970715)16:13<1435::AID-SIM570>3.0.CO;2-8
Zahl P-H (2003) Regression analysis with multiplicative and time-varying additive regression coefficients with examples from breast and colon cancer. Stat Med 22:1113–1127. doi:10.1002/sim.971
Olopade OI, Ikpatt FO, Dignam JJ et al (2004) “Intrinsic Gene Expression” subtypes correlated with grade and morphometric parameters reveal a high proportion of aggressive basal-like tumors among black women of African ancestry. Paper presented at American Society of Clinical Oncology Annual Meeting, New Orleans, Louisiana, USA, 5–8 June 2004
Nishimura R, Arima N (2008) Is triple negative a prognostic factor in breast cancer? Breast Cancer (in press). doi:10.1007/s12282-008-0042-3
Lund MJ, Trivers KF, Porter PL et al (2008) Race and triple negative threats to breast cancer survival: a population-based study in Atlanta, GA. Breast Cancer Res Treat (in press). doi:10.1007/s10549-008-9926-3
Goldhirsch A, Glick JH, Gelber RD et al (2005) Meeting highlights: international expert consensus on the primary therapy of early breast cancer 2005. Ann Oncol 16:1569–1583. doi:10.1093/annonc/mdi326
Goldhirsch A, Wood WC, Gelber RD et al (2007) Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol 18:1133–1144. doi:10.1093/annonc/mdm271
Harris L, Fritsche H, Mennel R et al (2007) American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 25:5287–5312. doi:10.1200/JCO.2007.14.2364
Abd El-Rehim DM, Ball G, Pinder SE et al (2005) High-throughput protein expression analysis using tissue microarray technology of a large well-characterised series identifies biologically distinct classes of breast cancer confirming recent cDNA expression analyses. Int J Cancer 116:340–350. doi:10.1002/ijc.21004
Burgess C, Hunter MS, Ramirez AJ (2001) A qualitative study of delay among women reporting symptoms of breast cancer. Br J Gen Pract 51:967–971
Meechan G, Collins J, Petrie KJ (2003) The relationship of symptoms and psychological factors to delay in seeking medical care for breast symptoms. Prev Med 36:374–378. doi:10.1016/S0091-7435(02)00053-1
Burgess CC, Ramirez AJ, Richards MA et al (1998) Who and what influences delayed presentation in breast cancer? Br J Cancer 77:1343–1348
Richards MA, Westcombe AM, Love SB et al (1999) Influence of delay on survival in patients with breast cancer: a systematic review. Lancet 353:1119–1126. doi:10.1016/S0140-6736(99)02143-1
Facione NC (1993) Delay versus help seeking for breast cancer symptoms: a critical review of the literature on patient and provider delay. Soc Sci Med 36:1521–1534. doi:10.1016/0277-9536(93)90340-A
Kang SP, Martel M, Harris LN (2008) Triple negative breast cancer: current understanding of biology and treatment options. Curr Opin Obstet Gynecol 20:40–46
Ross JS, Fletcher JA, Linette GP et al (2003) The Her-2/neu gene and protein in breast cancer 2003: biomarker and target of therapy. Oncologist 8:307–325. doi:10.1634/theoncologist.8-4-307
Rydén L, Landberg G, Stål O et al (2008) HER2 status in hormone receptor positive premenopausal primary breast cancer adds prognostic, but not tamoxifen treatment predictive, information. Breast Cancer Res Treat 109:351–357. doi:10.1007/s10549-007-9660-2
Horiguchi J, Koibuchi Y, Iijima K et al (2005) Co-expressed type of ER and HER2 protein as a predictive factor in determining resistance to antiestrogen therapy in patients with ER-positive and HER2-positive breast cancer. Oncol Rep 14:1109–1116
Dowsett M, Harper-Wynne C, Boeddinghaus I et al (2001) HER-2 amplification impedes the antiproliferative effects of hormone therapy in estrogen receptor-positive primary breast cancer. Cancer Res 61:8452–8458
Osborne CK, Bardou V, Hopp TA et al (2003) Role of the estrogen receptor coactivator AIB1 (SRC-3) and HER-2/neu in tamoxifen resistance in breast cancer. J Natl Cancer Inst 95:353–361
Schmid P, Wischnewsky MB, Sezer O et al (2002) Prediction of response to hormonal treatment in metastatic breast cancer. Oncology 63:309–316. doi:10.1159/000066224
Arpino G, Weiss H, Lee AV et al (2005) Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst 97:1254–1261
Kun Y, How LC, Hoon TP et al (2003) Classifying the estrogen receptor status of breast cancers by expression profiles reveals a poor prognosis subpopulation exhibiting high expression of the ERBB2 receptor. Hum Mol Genet 12:3245–3258. doi:10.1093/hmg/ddg347
Witton CJ, Reeves JR, Going JJ et al (2003) Expression of the HER1–4 family of receptor tyrosine kinases in breast cancer. J Pathol 200:290–297. doi:10.1002/path.1370
Joensuu H, Isola J, Lundin M et al (2003) Amplification of erbB2 and erbB2 expression are superior to estrogen receptor status as risk factors for distant recurrence in pT1N0M0 breast cancer: a nationwide population-based study. Clin Cancer Res 9:923–930
Karrison TG, Ferguson DJ, Meier P (1999) Dormancy of mammary carcinoma after mastectomy. J Natl Cancer Inst 91:80–85. doi:10.1093/jnci/91.1.80
Demicheli R, Abbattista A, Miceli R et al (1996) Time distribution of the recurrence risk for breast cancer patients undergoing mastectomy: further support about the concept of tumor dormancy. Breast Cancer Res Treat 41:177–185. doi:10.1007/BF01807163
Demicheli R, Valagussa P, Bonadonna G (2002) Double-peaked time distribution of mortality for breast cancer patients undergoing mastectomy. Breast Cancer Res Treat 75:127–134. doi:10.1023/A:1019659925311
Kilburn LS on behalf of the TNT Trial Management Group (2007) ‘Triple Negative’ Breast Cancer: a new area for Phase III breast cancer clinical trials. Clin Oncol (R Coll Radio) 20:35–39. doi:10.1016/j.clon.2007.09.010
Acknowledgements
The authors thank the family members for their willingness to cooperate with our study. This research was supported in part by the grants from the National Basic Research Program of China (2006CB910501), National Natural Science Foundation of China (30371580, 30572109); Shanghai Science and Technology Committee (03J14019, 06DJ14004, 06DZ19504).
Author information
Authors and Affiliations
Corresponding author
Additional information
W.-J. Yin, J.-S. Lu and G.-H. Di have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yin, WJ., Lu, JS., Di, GH. et al. Clinicopathological features of the triple-negative tumors in Chinese breast cancer patients. Breast Cancer Res Treat 115, 325–333 (2009). https://doi.org/10.1007/s10549-008-0096-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0096-0