Abstract
Background
Overexpression of human epidermal growth factor receptor 2 (HER2) or amplification of its gene is a prognostic factor in primary breast cancer and a predictor for tamoxifen treatment efficacy in oestrogen receptor (ER) positive disease. In the present study we explored a defined cohort of breast cancer patients included in a randomised trial in order to assess prognostic and tamoxifen treatment information yielded by HER2 status.
Methods
Premenopausal breast cancer patients with stage II tumours (n = 564) were included and allocated to 2 years of adjuvant tamoxifen treatment versus no adjuvant treatment. ER, progesterone receptor (PR) status and HER2 status was determined by immunohistochemistry using a tissue microarray. HER2 amplification was analysed by fluorescent in situ hybridisation and tumours being amplified and/or HER2 3+ were considered HER2+. HER2 status was evaluable in 83% of the patients and 12.6% were HER2+. In untreated patients, HER2 was a negative prognostic factor in ER+ patients, HR 2.95; 95% CI: 1.61–5.38, p < 0.001, but not in ER- patients, HR 0.67; 95% CI: 0.28–1.61, p = 0.4, and a significant interaction between the two markers was found, p < 0.01. HER2 status was not related to tamoxifen treatment efficacy in ER+ patients (term of interaction p = 0.95). When stratifying for PR status, similar results were achieved.
Discussion
HER2+ and ER+ breast cancer constituted a subgroup of tumours with poor prognosis in premenopausal breast cancer, whereas no treatment interaction was found between HER2 status and tamoxifen in ER+ tumours. The poor prognosis in HER2+ and ER+ patients may interfere with the interpretation of HER2 data in non-randomised trials of adjuvant tamoxifen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Overexpression of the human epidermal growth factor receptor 2 (HER2) or amplification of its gene, HER2, is identified in 10–30% of primary human breast cancers and associated with an aggressive tumour type with poor survival [1–6]. Gene expression patterns derived from cDNA microarray studies have elucidated that HER2 amplified tumours constitute a specific group of breast cancers separated from the luminal [oestrogen receptor (ER) expressing] and basal groups (ER- and HER2−) of breast cancer [7]. HER2 is inversely related to hormone receptor content and the fraction of tumours being both hormone receptor positive and HER2+ is limited (<10%). The ER+ luminal group can further be separated into luminal A, B and C, where luminal C has the worst prognosis with a genetic pattern similar to ER- tumours in the HER2+ and basal-like subgroups [7]. The ER+ group with poor prognosis has been related to amplification of HER2 which may activate ER-independent genes responsible for the aggressiveness of this tumour type [8]. Although ER+ tumours are generally related to a more favourable prognosis, the specific ER+ and HER2+ subgroup seems to constitute a clinical entity with poor outcome deserving to be identified in the clinical setting in order to optimise treatment [6–10].
Human epidermal growth factor receptor 2 status is associated with treatment prediction of both endocrine and cytotoxic treatment interfering with interpretation of its prognostic role in retrospective studies of mixed patient populations [4, 11, 12]. HER2+ tumours respond better to anthracycline-based therapies than HER2− tumours do and HER2 positivity tend to be a marker of resistance to tamoxifen by ligand-independent ER activation [12–15]. This negative effect by HER2 in ER+ patients can be overcome by oestrogen lowering therapies like aromatase inhibitors in postmenopausal patients [16]. However, studies of biomarkers in the neo-adjuvant setting suggest that therapeutic resistance to aromatase inhibitors in ER+ and HER+ tumours may develop over time indicating that this cohort of patients has a poor prognosis despite modern endocrine treatment [17]. Today HER2 can be targeted by a monoclonal humanised antibody—trastuzumab—which has shown efficacy in combination with chemotherapy treatment in both metastatic, locally advanced and adjuvant setting and is now tested in combination with endocrine treatment as an option for endocrine responsive tumours overexpressing HER2 [18–20].
The aim of the present study was to stratify patients with primary breast cancer according to HER2 status using validated methods for HER2 determination [21] and relate it to prognosis and tamoxifen treatment information. The patients were included in a randomised controlled trial of premenopausal patients allocated to adjuvant tamoxifen or no adjuvant treatment with a median follow-up of 13.9 years published in detail previously [22]. The untreated control arm enabled us to evaluate the prognostic role of HER2 status in relation to ER and progesterone receptor (PR) status without interference with adjuvant treatment. Patients with hormone receptor positive tumours and HER2+ tumours constituted a group with extremely poor prognosis supporting the findings obtained by the cDNA classification. In this study, HER2 status was not a predictor of tamoxifen response and it can be speculated that the tamoxifen predictive role associated with HER2 status is merely reflecting its prognostic impact in hormone receptor positive breast cancer.
Materials and methods
Clinical trial
Five hundred and sixty-four premenopausal patients with primary breast cancer were included in multicentre trial between January 1984 and September 1991 and randomised to 2 years of adjuvant tamoxifen treatment or no adjuvant treatment following primary surgical treatment. The trial has been described in detail before, and briefly patients with unifocal, stage II invasive breast cancer were included irrespective of ER status [22]. All patients with node positive disease had loco-regional radiotherapy and less than 2% had additional adjuvant treatment. The median follow-up time was 13.9 years for patients without any event. Patient and tumour characteristics are presented in Table 1. The study was approved by the Ethics Committees at Lund and Linköping Universities.
Tumour tissue microarray
Histopathological blocks were retrieved in 500 of 564 patients and a tumour tissue microarray was constructed. Two biopsies, 0.6 mm in diameter, were obtained from each donor block, corresponding to a previously marked area on a slide of invasive tumour, and mounted in a recipient block using a tissue array machine according to the manufacturer’s instructions (Beecher Instruments, MD, USA).
Immunohistochemistry
Oestrogen and progesterone receptor
The Ventana Benchmark system with prediluted antibodies (Anti-ER Clone 6F11 and Anti-PgR Clone 16) was used. In line with the clinically established cut-off used for hormone receptor assessment, tumours with more than 10% positively stained nuclei were considered positive.
HER2
Expression of HER2 was determined by immunohistochemistry and 428 of 500 tumour blocks were evaluable using the Ventana Benchmark system with a prediluted antibody (Pathway CB-11, 760–2694) and tumours were evaluated semi-quantitatively according to a standard, written protocol (HercepTest). The protocol categorises tumours into four groups; grade 0: lack of staining in all tumour cells or membrane staining in less than 10% of the tumour cells, grade 1+: weak, not circumferential membrane staining in more than 10% of the tumour cells, grade 2+: intermediate, circumferential membrane staining in more than 10% of the tumour cells, grade 3+: intense and circumferential staining in more than 10% of the tumour cells.
HER2 gene amplification
Human epidermal growth factor receptor 2 gene amplification was determined by fluorescent in situ hybridisation (FISH) using an automated staining procedure according to the manufacturer’s recommendations (Ventana Medical Systems Ind., AZ, USA). Briefly, unstained, formalin-fixed, paraffin-embedded tumour sections were deparaffinised, pretreated and denaturated before incubation overnight with the hybridisation probe. The sections were counterstained and evaluated for HER2 gene copy number using a fluorescence microscope at a magnification of 400×. All tumour cells within the biopsies in the TMA were evaluated. Tumours were considered amplified when displaying six or more signals per tumour cell. Due to insufficient tumour material and fixation artefacts, 127 (27%) tumours were not evaluable.
HER2 status
All patients with amplified tumours and all patients with a 3+ where FISH analysis could not be evaluated were considered HER2+.
Statistical methods
The statistical calculations were performed using SPSS Version 13.0 (SPSS, Chicago, IL, USA) and Stata Version 9.2 (StataCorp, College Station, TX, USA). Recurrence-free survival (RFS) was chosen as endpoint in the present study. RFS included breast cancer-specific death, distant, regional and local recurrences as primary event and all analyses were performed with the intention to treat rule. Kaplan–Meier plots were used to illustrate the survival in specified cohorts and the log-rank test to test for equality of survival curves. Hazard ratios were estimated using Cox regression for 10-year RFS. Proportional hazards assumptions were checked using Schoenfeld’s test. The null hypothesis of prognostic effects by HER2 status in hormone receptor positive and negative patients were evaluated using a Cox model with a term for the interaction between hormone receptor status and HER2 status. Comparisons of tumour characteristics were made by Chi-square test for categorised variables and by Mann–Whitney for continuous variables. All p-values corresponded to two-sided tests and values less than 0.05 were considered significant.
Results
Descriptive results
Human epidermal growth factor receptor 2 status was determined in 470 of 564 patients (83%) from FISH data available in 373 patients and IHC data in 428 patients. There was a strong correlation between HER2 3+ and HER2 gene amplification by FISH (r = 0.84, p < 0.001) with a kappa-value of 0.84. Of the analysed patients, 12.6% were defined as HER2+ by the combination of gene amplification and/or HER2 3+ and a detailed description of the data according to treatment arm is given in Table 1. HER2 positivity was significantly associated with Nottingham histological grade 3 (p < 0.001), ER negativity (p < 0.001), PR negativity (p < 0.001) and of borderline significance to T2 (p = 0.08), but not to lymph node metastases (p = 0.2) or age <45 versus ≥45 years (p = 0.1).
To further explore the association between HER2 status and hormone receptor status, the relation of HER2 status to PR status was explored in ER+ tumours and stratified according to median age (<45 and ≥45 years, respectively). HER2 status was not related to PR in patients younger than 45 years in contrast to patients older than 45 years (Table 2).
Clinical outcome: prognosis
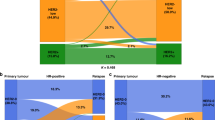
We first evaluated the association of HER2 status with RFS by log-rank tests in the untreated cohort not receiving any adjuvant treatment. There was no significant prognostic information yielded by HER2 status (log-rank, p = 0.2) after maximum follow-up time including all untreated patients. When stratifying the cohort according to ER status, there was a strong negative effect by HER2 positivity in the ER+ group (log-rank, p = 0.0005), whereas there was no effect by HER2 status in the ER- group (log-rank, p = 0.4) (Fig. 1a, b).
Ten-year RFS data are presented in Table 3 showing that node positivity and Nottingham histological grade were significant predictors of outcome in untreated patients whereas age, tumour size, HER2 status, ER and PR status were not. However, when the cohort was stratified for ER status we found a 10-year RFS in ER+ and HER2− patients of 55.5%, whereas ER+ and HER2+ patients had a 10-year RFS of 18.8% with a significant effect by HER2 status in ER+ patients (HR 2.95; 95% CI 1.61–5.38, p < 0.001) (Table 4). There was no prognostic effect by HER2 status in the ER- cohort (HR 0.67; 0.28–1.61, p = 0.4). When stratifying the untreated cohort for PR status, similar results were achieved and are provided in Table 4.
The prognostic interaction between ER and PR status and HER2 status was evaluated in a Cox multivariate analysis including ER status or PR status (-/+), HER2 status (-/+) and an interaction variable for hormone receptor status and HER2 status (-/+). We found a significant interaction between ER status and HER2 status (p = 0.008) as well as between PR status and HER2 status (p = 0.014) in terms of 10-year RFS. The term of interaction was significant also when adjusting for age, tumour size, node status, Nottingham histological grade and PR status in a Cox multivariate analysis (p = 0.042) as given in Table 3. The term of interaction between HER2 status and PR status was of borderline significance (p = 0.066) in a corresponding multivariate analysis.
Clinical outcome: tamoxifen treatment prediction
In order to explore the tamoxifen treatment effect in hormone receptor positive patients, we first selected the 324 ER+ patients. There was a significant tamoxifen effect in the ER+ group (log-rank, p = 0.005), but no effect was noted in the ER- group (log-rank, p = 0.8). Two years of adjuvant tamoxifen was significantly beneficial in the ER+ and HER2− cohort (n = 275), (HR 0.64; 95% CI 0.44–0.93, p = 0.02), whereas no significant effect by tamoxifen was seen in the ER+ and HER2+ cohort (n = 24), (HR 0.71; 95% CI 0.23–2.20, p = 0.6). However, when the treatment effect was explored using a multivariate interaction model including HER2 status and treatment, there was no statistically difference in tamoxifen treatment efficacy according to HER2 status (term of interaction, p = 0.95).
When analysing ER+ patients in the two age cohorts in relation to HER2 and tamoxifen treatment interaction, similar results were achieved (patients <45 years, term of interaction, p = 0.15, patients ≥45 years, term of interaction p = 0.23). Finally, we analysed ER+ and PR+ (n = 291) and ER+ and PR- (n = 15) separately (term of interaction in ER+ and PR+ patients, p = 0.89). The group with ER+ and PR- patients included 15 patients with only three events and did not allow any meaningful analysis.
Discussion
In the present study, we analysed hormone receptor and HER2 status by validated methods in a cohort of premenopausal breast cancer patients allocated to no adjuvant treatment or 2 years of adjuvant tamoxifen. In the untreated cohort, we defined a group of patients with hormone receptor positive and HER2+ tumours (amplified and/or HER2 3+) with poor prognosis (less than 20% 10-year RFS). This finding has been indicated in previous studies based on cDNA arrays as well as immunohistochemical studies, although careful data about adjuvant treatment has not been provided before [7–10]. HER2 status did not add any prognostic information in the hormone receptor negative group in the present study and there was a statistically significant interaction between the two biomarkers in terms of prognosis. The biological explanation to the prognostic interaction has to be further elucidated, but one proposed explanation is that the classified subgroup with ER+ and HER2+ tumours express genes which are not ER dependent and may contribute to a more aggressive breast cancer with poor prognosis, not typically associated with the ER+ subgroup of breast cancer [8]. The prognostic interaction was significant also when adjusting for conventional prognostic markers supporting the robustness of the finding.
Human epidermal growth factor receptor 2 status is considered both a prognostic and treatment predictive marker and in this cohort, we were able to explore its relation to adjuvant tamoxifen treatment efficacy in premenopausal patients. We found that tamoxifen treatment efficacy in hormone receptor positive patients was not statistically related to HER2 status. Contradictory results have been published in pre- and postmenopausal patients, using both randomised and non-randomised trials [11–15, 23–25]. In a randomised trial including only premenopausal patients there was no correlation between HER2 status and tamoxifen treatment effect [24]. However, the active trial arm was allocated to both oophorectomy and adjuvant tamoxifen so no definitive conclusion could be drawn regarding tamoxifen treatment effect related to HER2 status [24]. The data presented in Love’s study has led to a more careful examination of hormone receptor status and HER2 status in relation to age as a possible alternative explanation to the findings in Love’s study of premenopausal women [26]. In line with previous publications, we found that PR status is inversely related to HER2 status in ER+ breast tumours in patients 45 years and older, but not in younger patients. Since PR negativity is convincingly presented as a surrogate marker to HER2 positivity and a non-functional ER [12, 15], we analysed data from patients <45 years as well as ≥45 years and subgroups of ER+ patients with and without PR positivity in relation to tamoxifen treatment. However, we were not able to find any difference in tamoxifen treatment effect according to HER2 status in any of the defined subgroups.
Human epidermal growth factor receptor 2 status is a negative prognostic factor in hormone receptor positive and tamoxifen treated patients suggesting that HER2 positivity is associated with tamoxifen treatment failure [4, 11, 12]. On the other hand, HER2 status is a prognostic factor in hormone receptor positive breast cancer not treated with tamoxifen and the proposed tamoxifen predictive information achieved by HER2 in non-randomised trials can therefore reflect HER2’s prognostic role in hormone receptor positive breast cancer, rather than treatment resistance. Although there are quite a few randomised trials in which HER2 status has been explored in relation to tamoxifen treatment, the retrospective nature of the studies comparing small subgroups of included patients confers to a low statistical power and the uncertainty of HER2 in relation to endocrine treatment effect will probably never be fully elucidated using the retrospective approach [15, 23, 24].
Human epidermal growth factor receptor 2 status by validated methods using HercepTest and FISH at centralised laboratories is today included in routine analysis of breast cancer and used as a prognostic marker [21]. The classification of hormone receptor positive and HER2+ tumours are limited to 7–8% of primary breast cancer due to the inverse relationship between hormone receptor status and HER2 status. For patients in this subgroup with a primary tumour at an early stage, i.e. T1N0, endocrine treatment is often the only recommended adjuvant treatment postoperatively. In postmenopausal patients aromatase inhibitors are advocated in favour of tamoxifen in HER2+ patients based on biomarker studies in the neo-adjuvant setting. Further supporting this treatment option is the ATAC trial where patients with ER+ and PR- tumours—interpreted as surrogate marker for HER2+ tumours—tended to have a more favourable outcome in the anastrozole arm compared to the tamoxifen arm [16]. There is today indications that therapeutic resistance to the oestrogen-lowering approach with an aromatase inhibitor develops over time in ER+ HER2+ tumours by oestrogen-independent proliferation and the role of endocrine monotherapy is therefore questioned in this group of patients [17]. The specific humanised monoclonal antibody directed towards HER2 is efficient in both hormone receptor positive and negative breast cancer and offers today a treatment option to all HER2+ breast cancer patients with metastatic, locally advanced or early disease [18–20]. The finding in this study that hormone receptor positive HER2+ breast cancer has an extreme poor prognosis supports the choice to advocate more efficient adjuvant treatment options than endocrine treatment of any modality seems to offer.
References
Slamon DJ, Godolphin W, Jones LA et al (1989) Studies of the HER−2/neu proto-oncogene in human breast and ovarian cancer. Science 244(4905):707–712
Borg A, Tandon AK, Sigurdsson H et al (1990) HER−2/neu amplification predicts poor survival in node-positive breast cancer. Cancer Res 50:4332–4337
Press MF, Bernstein L, Thomas PA et al (1997) HER−2/neu gene amplification characterized by fluorescence in situ hybridization: poor prognosis in node-negative breast carcinomas. J Clin Oncol 15(8):2894–2904
Sjogren S, Inganas M, Lindgren A et al (1998) Prognostic and predictive value of c-erbB−2 overexpression in primary breast cancer, alone and in combination with other prognostic markers. J Clin Oncol 16:462–469
Schmidt M, Lewark B, Kohlschmidt N et al (2005) Long-term prognostic significance of HER−2/neu in untreated node-negative breast cancer depends on the method of testing. Breast Cancer Res 7(2):R256–266
Joensuu H, Isola J, Lundin M et al (2003) Amplification of erbB2 and erbB2 expression are superior to estrogen receptor status as risk factors for distant recurrence in pT1N0M0 breast cancer: a nationwide population-based study. Clin Cancer Res 9(3):923–930
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98(19):10869–10874
Kun Y, How LC, Hoon TP et al (2003) Classifying the estrogen receptor status of breast cancers by expression profiles reveals a poor prognosis subpopulation exhibiting high expression of the ERBB2 receptor. Hum Mol Genet 12(24):3245–3258
Witton CJ, Reeves JR, Going JJ et al (2003) Expression of the HER1–4 family of receptor tyrosine kinases in breast cancer. J Pathol 200(3):290–297
Kim MJ, Ro JY, Ahn SH et al (2006) Clinicopathologic significance of the basal-like subtype of breast cancer: a comparison with hormone receptor and Her2/neu-overexpressing phenotypes. Hum Pathol 37(9):1217–1226
Borg A, Baldetorp B, Ferno M et al (1994) ERBB2 amplification is associated with tamoxifen resistance in steroid-receptor positive breast cancer. Cancer Lett 81:137–144
Arpino G, Weiss H, Lee AV et al (2005) Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst 97(17):1254–1261
Stål O, Borg A, Ferno M et al (2000) ErbB2 status and the benefit from two or five years of adjuvant tamoxifen in postmenopausal early stage breast cancer. Ann Oncol 11:1545–1550
De Placido S, De Laurentiis M, Carlomagno C et al (2003) Twenty-year results of the Naples GUN randomized trial: predictive factors of adjuvant tamoxifen efficacy in early breast cancer. Clin Cancer Res 9(3):1039–1046
Dowsett M, Houghton J, Iden C et al (2006) Benefit from adjuvant tamoxifen therapy in primary breast cancer patients according oestrogen receptor, progesterone receptor, EGF receptor and HER2 status. Ann Oncol 17(5):818–826
Dowsett M, Cuzick J, Wale C et al (2005) Retrospective analysis of time to recurrence in the ATAC trial according to hormone receptor status: an hypothesis-generating study. J Clin Oncol 23(30):7512–7517
Ellis MJ, Tao Y, Young O et al (2006) Estrogen-independent proliferation is present in estrogen-receptor HER2−positive primary breast cancer after neoadjuvant letrozole. J Clin Oncol 24(19):3019–3025
Slamon DJ, Leyland-Jones B, Shak S et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344(11):783–792
Pegram MD, Pienkowski T, Northfelt DW et al (2004) Results of two open-label, multicenter phase II studies of docetaxel, platinum salts, and trastuzumab in HER2−positive advanced breast cancer. J Natl Cancer Inst 96(10):759–769
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2−positive breast cancer. N Engl J Med 353(16):1659–1672
Press MF, Sauter G, Bernstein L et al (2005) Diagnostic evaluation of HER−2 as a molecular target: an assessment of accuracy and reproducibility of laboratory testing in large, prospective, randomized clinical trials. Clin Cancer Res 11(18):6598–6607
Ryden L, Jonsson PE, Chebil G et al (2005) Two years of adjuvant tamoxifen in premenopausal patients with breast cancer: a randomised, controlled trial with long-term follow-up. Eur J Cancer 41(2):256–264
Knoop AS, Bentzen SM, Nielsen MM et al (2001) Value of epidermal growth factor receptor, HER2, p53, and steroid receptors in predicting the efficacy of tamoxifen in high-risk postmenopausal breast cancer patients. J Clin Oncol 19(14):3376–3384
Love RR, Duc NB, Havighurst TC et al (2003) Her-2/neu overexpression and response to oophorectomy plus tamoxifen adjuvant therapy in estrogen receptor-positive premenopausal women with operable breast cancer. J Clin Oncol 21(3):453–457
Ryden L, Jirstrom K, Bendahl PO et al (2005) Tumor-specific expression of vascular endothelial growth factor receptor 2 but not vascular endothelial growth factor or human epidermal growth factor receptor 2 is associated with impaired response to adjuvant tamoxifen in premenopausal breast cancer. J Clin Oncol 23(21):4695–4704
Huang HJ, Neven P, Drijkoningen M et al (2005) Association between HER-2/neu and the progesterone receptor in oestrogen-dependent breast cancer is age-related. Breast Cancer Res Treat 91(1):81–87
Acknowledgement
The study was supported by funds from the Swedish Cancer Society, Swedish Research Council, Gunnar Nilsson Cancer Foundation, Mrs Berta Kamprad Foundation, Skane county council’s research and development Foundation and Minna Breining Cancer Foundation at the Department of Oncology, Lund.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rydén, L., Landberg, G., Stål, O. et al. HER2 status in hormone receptor positive premenopausal primary breast cancer adds prognostic, but not tamoxifen treatment predictive, information. Breast Cancer Res Treat 109, 351–357 (2008). https://doi.org/10.1007/s10549-007-9660-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9660-2