Abstract
BRCA1 and BRCA2 germ-line mutations predispose to breast and ovarian cancer. Large genomic rearrangements of BRCA1 account for 0–36% of all disease causing mutations in various populations, while large genomic rearrangements in BRCA2 are more rare. We examined 642 East Danish breast and/or ovarian cancer patients in whom a deleterious mutation in BRCA1 and BRCA2 was not detected by sequencing using the multiplex ligation-dependent probe amplification (MLPA) assay. We identified 15 patients with 7 different genomic rearrangements, including a BRCA1 exon 5–7 deletion with a novel breakpoint, a BRCA1 exon 13 duplication, a BRCA1 exon 17–19 deletion, a BRCA1 exon 3–16 deletion, and a BRCA2 exon 20 deletion with a novel breakpoint as well as two novel BRCA1 exon 17–18 and BRCA1 exon 19 deletions. The large rearrangements in BRCA1 and BRCA2 accounted for 9.2% (15/163) of all BRCA1 and BRCA2 mutations in East Denmark. Nine patients had the exon 3–16 deletion in BRCA1. By SNP analysis we find that the patients share a 5 Mb fragment of chromosome 17, including BRCA1, indicating that the exon 3–16 deletion represents a Danish founder mutation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Germ-line BRCA1 (MIM# 113705) and BRCA2 (MIM# 600185) mutations confer a lifetime risk of approximately 80% for breast cancer and 20–50% for ovarian cancer in female carriers, and in addition a moderate increased risk of other cancer types [1]. The BRCA1 locus was linked to chromosome 17q21 in 1990 [2] and cloned in 1994 [3]. The gene spans approximately 81 kb and is composed of 23 exons encoding a protein of 1863 amino acids. Sequence conservation between mammalian species is weak, but a Zinc-binding RING domain at the amino terminus, involved in BARD1 binding [4], and an acidic carboxyl terminus containing two BRCA1 C-terminal (BRCT) domains, involved in protein interactions with several proteins including CtIP, BRIP1, and Abraxas [5–7], are highly conserved. The BRCA2 locus was linked to chromosome 13q12-13 in 1994 [8] and cloned 1 year later [9]. The BRCA2 gene spans approximately 84 kb and is composed of 27 exons, which encodes a protein of 3418 amino acids. It contains eight BRC domains, which are involved in protein binding, including binding with Rad51 [10, 11]. BRCA1 and BRCA2 are both involved in the maintenance of genome stability [12, 13] and DNA repair via homologous recombination [14, 15], but they are also suggested to play a role in transcriptional regulation [16], cell cycle control [17], chromatin remodelling [18] and ubiquitinylation [19].
The majority of BRCA1 and BRCA2 mutations are nonsense and small deletions/insertion mutations that lead to premature translation termination and production of truncated BRCA1 and BRCA2 proteins. Large genomic rearrangements were not reported until 1997 [20], but it has subsequently been reported that large genomic rearrangements—in particular in BRCA1—may account for 3–15% of all BRCA1 and BRCA2 mutations.
Using the multiplex ligation-dependent probe amplification (MLPA) assay, we report the identification of 15 breast and/or ovarian cancer patients from East Denmark with seven different large genomic rearrangements of which one is a specific Danish BRCA1 founder mutation, two are novel deletions in BRCA1, and other two contain novel breakpoints.
Materials and methods
Patients
Following referral to oncogenetic counselling patients from Danish families with clustering of breast and/or ovarian cancer have since 1999 been offered BRCA1 and BRCA2 mutation screening according to the guidelines of the Danish Breast Cancer Cooperative Group (DBCG) (www.dbcg.dk). Families were classified as high-risk families based on manually evaluation of pedigrees and by use of tables and typically contained patients with breast cancer before the age of 40 years, with both breast and ovarian cancer, with two first degree relatives with breast cancer before the age of 50 years or ovarian cancer, with three first degree relative over two generation of which one was younger than 50 years, or patients with male breast cancer. Affected individuals or obligate carriers with a family history consistent with autosomal dominant inheritance of breast and/or ovarian cancer were screened for BRCA1 and BRCA2 mutations. Eligible for the current study were patients who received counselling between 1999 and 2007, and in whom a deleterious mutation in BRCA1 and BRCA2 not could be demonstrated by the initial pre-screening with denaturing high performance liquid chromatography (dHPLC) and sequencing. All together 642 probands were analysed for large genomic rearrangements by MLPA analysis. Blood samples were obtained from breast and ovarian cancer patients after informed consent and the original consent encompassed additional screening in case of new methods or targets. The family history was verified using the registry of the DBCG, hospital medical records and pathology reports and genetic counselling was provided for every family member.
MLPA analysis
Genomic DNA was purified from whole blood samples using the QIAamp DNA mini kit (Qiagen) according to the manufacturer’s instructions. MLPA analysis was performed according the manufactures instructions (MRC-Holland) using the SALSA P002 BRCA1 and the SALSA P045 BRCA2 MLPA kits. GeneMarker software (SoftGenetics) was used for fragment analysis. When a positive result (30% change) appeared the analysis was repeated (for BRCA1 with MLPA kit P087). Moreover single exon deletions identified by MLPA analysis were sequenced using an ABI 3730 DNA analyzer (Applied Biosystems) using the BigDye terminator v1.1 cycler sequencing kit (Applied Biosystems) to exclude the presence of variants affecting the hybridization of the MLPA probes.
DNA breakpoint analysis
When possible deletions were verified by long range PCR using the Expand long template PCR kit (Roche) as recommended by the manufacturer. For the BRCA1 exon 13 duplication, the genomic DNA was amplified with the following primers 5′-GATTATTTCCCCCCAGGCTA-3′ and 5′-AGATCATTAGCAAGGACCTGTG-3′ as described [21]. The samples were separated by agarose gel electrophoresis and visualized by ethidium bromide staining. For the BRCA1 exon 3–16 deletion, the genomic DNA was amplified with the following primers 5′-GAAAAAGTAAGAGACACCTATAG-3′ and 5′-CTTTATAAGCTGAGAGGTAACTAG-3′, for the BRCA1 exon 5–7 deletion we used the following primers 5′-ACCTAGTCACCCCCTTCACC-3′ and 5′-CCAGCCCCAGAATGATTACTT-3′, for the BRCA1 exon 17–18 deletion we used the primers 5′-GAATGTCCATGGTGGTGTCTGGC-3′ and 5′-GCCTGCATAATTCTTGATGATCC-3′ and finally for the BRCA2 exon 20 deletion the following primers 5′-GCTAACAGTACTCGGCCTGCTCGC-3′ and 5′-GCTTCTTTCCTTTAGAAATTACCCAG-3′ were used.
In all these cases the samples were separated by agarose gel electrophoresis and visualized by ethidium bromide staining. Finally, the bands were purified and sequenced using an ABI3730 DNA analyzer (Applied Biosystems) using the BigDye terminator v1.1 cycler sequencing kit (Applied Biosystems). For genomic breakpoint determination the genomic reference sequences NC_000017 and NC_000013.9, and the coding DNA reference sequences NM_007294 and NM_000059 were used.
SNP chip analysis
Genomic DNA was applied to 250 K StyI (~238.000 SNPs) SNP-microarray chips and processed according to the manufacturer’s instructions (Affymetrix). Briefly, 250 ng of genomic DNA was digested with StyI and ligated to adapters. Adapter ligated DNA was amplified, purified, fragmented and labeled with biotin and hybridized to the arrays for 18 h. The Affymetrix 450 fluidics station and the Affymetrix 3000 G7 gene scanner were used to wash, stain and scan the arrays. The CEL files were analysed using the BRLMM algorithm from Affymetrix Genotyping analysis software (GTYPE). For the 9 individuals with the BRCA1 exon 3–16 deletion we removed all SNPs with missing genotypes or with missing position annotation leaving 222.543 SNPs. Using the HapMap Ceph parents as a reference sample we estimated the co-ancestry between individuals using a moment approach [22]. The co-ancestry coefficient was lower than 5% between all pairs of individuals meaning that none of the individuals are closely related. We estimated the length of the possible shared haplotypes from the genotypes. We defined the possible shared haplotype as a region where all the genotypes are consistent with a single haplotype in the sense that there are no pairs of individuals that are homozygous for different alleles.
Results
To determine the frequency of large genomic rearrangements (LGRs) in BRCA1 and BRCA2 in East Denmark, we examined 642 breast and/or ovarian cancer patients previously screened negative for small disease causing mutations in BRCA1 and BRCA2 by MLPA analysis as recently described [23]. The MLPA analysis revealed 15 LGRs in BRCA1 and BRCA2, including a BRCA1 exon 3–16 deletion in nine patients with breast and/or ovarian cancer or family members with breast and/or ovarian cancer, a BRCA1 exon 5–7 deletion in a patient with breast and ovarian cancer, a BRCA1 exon 13 duplication in a patient with breast cancer, a BRCA1 exon 17–18 deletion in a breast cancer patient with Iranian ancestors, a BRCA1 exon 17–19 deletion in a patient with breast cancer, a BRCA1 exon 19 deletion in a patient with breast and ovarian cancer, and a BRCA2 exon 20 deletion in a male with pancreatic and breast cancer (Fig. 1a–g and Table 1). All BRCA1 changes were verified in a new DNA sample using the P087 BRCA1 MLPA control kit. Moreover, all single exon deletions were sequenced to exclude the presence of a nucleotide variant within the probe-binding site.
Multiplex ligation-dependent probe amplification (MLPA) analysis of BRCA1 and BRCA2 large genomic rearrangements. MLPA analysis of the BRCA1 exon 3–16 deletion (a), the BRCA1 exon 5–7 deletion (b), the BRCA1 exon 13 amplification (c), the BRCA1 exon 17–18 deletion (d), the BRCA1 exon 17–19 deletion (e), the BRCA1 exon 19 (f), and the BRCA2 exon 20 deletion (b) are shown. The green squares are BRCA1 and BRCA2 probes, the blue squares are control probes, while the deleted or duplicated exons are indicated by red squares
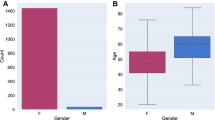
Since we previously identified deleterious mutations in BRCA1 and BRCA2 in 148 families, LGRs account for 9.2% (15/163) of all disease causing mutations identified in East Denmark. Of the 15 LGRs identified, 14 were in BRCA1, while only 1 was identified in BRCA2, showing that BRCA1 LGRs account for 12.5% (14/112), while BRCA2 accounts for 2% (1/51) out of all BRCA1 and BRCA2 disease causing mutations identified. The average age on onset for all female probands was approximately 36 years (excluding one woman without cancer and one with unknown age of breast cancer onset), while the average age on onset for the eight female patients with the BRCA1 exon 3–16 deletion was approximately 35 years (Table 1). Most families also had family member with breast cancer and in 7 out of 14 families with BRCA1 LGRs we find the occurrence of both breast and ovarian cancer (Table 1).
To determine the breakpoints for the deletions long-range PCR was performed. The size of the PCR products from the nine patients with the BRCA1 exon 3–16 deletion was examined by agarose gel electrophoresis, and found to be identical (Fig. 2a). Sequencing showed that the genomic breakpoint was located at g.8655_55240del46586 (c.81-1018_4986+716del46586) (Fig. 2a). The BRCA1 exon 5–7 deletion breakpoint was determined to be g.18296_23289del4994 (c.136-623_441+1959del4994) (Fig. 2b), while the BRCA1 exon 13 duplication was examined by PCR and yielded a band of approximately 1 kb showing the breakpoint to be identical to the recently published [21] (Fig. 2c). Moreover, the breakpoints for the BRCA1 exon 17–18 deletion was determined to be located at g.55023_61749del6727 (c.4986+498_5152+171del6727) (Fig. 2d), whereas the breakpoints for the BRCA1 17–19 deletion and exon 19 was undetermined due to insufficient amounts of DNA. Finally, the breakpoint for the BRCA2 exon 20 deletion was determined to be located at g.55520_56675del1156 (c.8531_8632+1054) (Fig. 2e).
Breakpoint analysis of BRCA1 and BRCA2 large genomic rearrangements. (a) Long-range PCR analysis and gel electrophoresis was performed on the 9 patients harbouring the BRCA1 exon 3–16 deletion. The resulting PCR fragments are shown to the left. The breakpoint was determined by sequencing (on the right) and designated g.8655_55240del46586 (c.81-1018_4986+716del46586) (b) The breakpoint for the BRCA1 exon 5–7 deletion was determined by long-range PCR and sequencing to be g.18296_23289del4994 (c.136-623_441+1959del4994). (c) The BRCA1 exon 13 duplication was examined by PCR analysis and gel electrophoresis and yielded a band of approximately 1 kb showing that the breakpoint is identical to the recently published [21]. The size marker is shown in lane 1, control DNA in lane 2 and 3, and patient DNA in lane 4 and 5. (d) The breakpoint for the BRCA1 exon 17–18 deletion was determined by long-range PCR and sequencing to be g.55023_61749del6727 (c.4986+498_5152+171del6727). (e) Finally, the breakpoint for the BRCA2 exon 20 deletion was determined by long-range PCR and sequencing to be g.55520_56675del1156 (c.8531_8632+1054). The site of crossover is indicated in all cases
To determine if the BRCA1 exon 3–16 deletion represented a Danish founder mutation, we compared the SNP profiles of the affected families by analysis on a 500 K SNP-array. If the mutation was a founder mutation, the affected individuals are expected to share a single haplotype around the mutation. Figure 3 shows the lengths of possible shared haplotypes on chromosome 17. We note a 5 Mb long shared haplotype around the BRCA1 consisting of 300 SNPs. This is by far the largest possible shared haplotype in the genome when removing possible shared haplotypes with less than 100 SNPs (see supplementary Fig. 1). Based on the possible shared haplotypes the nine individuals positive for the BRCA1 mutation are more closely related in the BRCA1 region, than any other region on the genome. We therefore infer that the mutation in the BRCA1 region happened once and segregated in the population to these nine individuals. This can be seen even though none of the individuals showed any close relatedness, when considering the whole genome variation.
Discussion
The human genome contains about one Alu repeat every 5 kb and these may cause large genomic rearrangements and homologous recombination events. The BRCA1 gene spans ~81 kb DNA and almost 42% of the genomic sequence is composed of Alu sequences. BRCA2 is slightly larger but contains fewer Alu repeats and it is presumed, that this is the reason why LGRs are less frequently observed in BRCA2. In our consecutive series of Danish high risk breast and ovarian cancer families, LGRs overall accounts for 9.2% of all disease-causing mutations in BRCA1 and BRCA2 taken as a group and for 12.5% of all BRCA1 disease causing mutations. This is higher than previously reported from West Denmark, where LGRs were identified in 2.3% of all disease causing BRCA1 and BRCA2 mutations, and 3.8% of BRCA1 disease-causing mutations [24], and from Finland [25] and the French part of Canada [26] where no LGRs were found. In contrast the data are more in agreement with results from France (9.5%) [27], Spain (8.2%) [28], Germany (8%) [29] and Czech Republic (6%) [30], but lower than observed in the Netherlands (27–36%) [23, 31] and Italy (19%) [32]. Only one family with a LGR in BRCA2 was identified, in accordance with studies from other populations, which found no families with BRCA2 LGRs [25, 33, 34]. The mutation was identified in a male patient, in agreement with the finding that LGRs in BRCA2 are more frequent in families with male breast cancer [35, 36]. The clinical feature of the families exhibiting LGRs was not different from those exhibiting other types of mutations. As previously reported many of the families with mutation in BRCA1 contain both breast and ovarian cancer and a young age at diagnosis [37]. We find the occurrence of both breast and ovarian cancer in 7 out of 14 families with BRCA1 LGRs and that the average age of cancer onset for female probands was approximately 36 years.
Of the seven different LGRs found in East Denmark, five have previously been described. In particular the BRCA1 3–16 deletion has previously been reported in two patients from West Denmark [24] and in a ovarian cancer patient from Britain/USA [38]. The 9 probands exhibited the same breakpoint (g.8655_55240del46586/c.81-1018_4986+716del46586), that is identical to that reported by others [24]. The nine families share a 5 Mb fragment containing the mutation, which suggests that it represents a founder mutation and not a mutation hot-spot. LGR founder mutations have also been reported in other populations, including BRCA1 exon 13 and exon 22 deletions in the Netherlands [31]. The BRCA1 exon 5–7 deletion was found in a patient with British ancestors. This deletion has previously been identified in both a German [39], and an Italian [32] family with breast and ovarian cancer. The deletion introduces a frameshift, which is predicted to result in a truncation at codon 163 in BRCA1. The breakpoint in our patient was identified to be g.18296_23289del4994 (c.136-623_441+1959del4994), which is different to those previously identified [39], indicating that the involved intronic regions are inclined to rearrangements. The BRCA1 exon 13 duplication has previously been identified in Britain, Sweden, Germany and Asia [21, 39–41]. It is known to include a 6-kb fragment containing two exon 13 fragments [21], introducing a frameshift. We were able to verify the exon 13 duplication by PCR as described [21], implying that the breakpoint is identical to the previously reported duplication. The BRCA1 exon 17–19 deletion has previously been described in an American/European breast and ovarian cancer family [42], but no breakpoint was identified. This deletion does not create a frameshift, but deletes amino acids 1663–1731 which contains one of the BRCT domains involved in protein interactions with BRIP1, CtIP, and Abraxas [5–7]. Interestingly, this region has also been reported to be triplicated [23]. Finally, we identified a single LGR in BRCA2. This was a BRCA2 exon 20 deletion in a male with pancreas and breast cancer. Three female family members moreover had late onset breast cancer. Long-range PCR analysis revealed that the patient had a 1.156 bp genomic deletion. A BRCA2 exon 20 deletion has previously been observed in Italy in a family with breast cancer, including male breast cancer [43]. In that study the breakpoint was defined as a 4.953 bp deletion (g.56447_61399del4953), which is different to the 1156 bp deletion identified in our study (g.55520_56675del1156/c.8531_8632+1054). Finally the BRCA1 exon 17–18 and the BRCA1 exon 19 deletions have not been described before. The breakpoint in the BRCA1 exon 17–18 deletion occurred at g.55023_61749del6727 (c.4986+498_5152+171del6727). Both deletions introduce a frameshift and introduce stop codons at codon 1719 and at codon 1732 in BRCA1, respectively.
In conclusion, we show that LGRs in BRCA1 and BRCA2 are common in East Denmark and account for 9.2% of the disease causing mutations. We also report two novel deletions and show that the BRCA1 exon 3–16 deletion is a founder mutation. Finally our study suggests that, even though the number of LGRs in BRCA2 in East Denmark is low, MLPA analysis of BRCA2 should be included in the screening of high-risk breast and/or ovarian cancer families.
References
Thompson D, Easton D (2004) The genetic epidemiology of breast cancer genes. J Mammary Gland Biol Neoplasia 9:221–236. doi:10.1023/B:JOMG.0000048770.90334.3b
Hall JM, Lee MK, Newman B, Morrow JE, Anderson LA, Huey B et al (1990) Linkage of early-onset familial breast cancer to chromosome 17q21. Science 250:1684–1689. doi:10.1126/science.2270482
Miki Y, Swensen J, Shattuck-Eidens D, Futreal PA, Harshman K, Tavtigian S et al (1994) A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science 266:66–71. doi:10.1126/science.7545954
Wu LC, Wang ZW, Tsan JT, Spillman MA, Phung A, Xu XL et al (1996) Identification of a RING protein that can interact in vivo with the BRCA1 gene product. Nat Genet 14:430–440. doi:10.1038/ng1296-430
Cantor SB, Bell DW, Ganesan S, Kass EM, Drapkin R, Grossman S et al (2001) BACH1, a novel helicase-like protein, interacts directly with BRCA1 and contributes to its DNA repair function. Cell 105:149–160. doi:10.1016/S0092-8674(01)00304-X
Wang B, Matsuoka S, Ballif BA, Zhang D, Smogorzewska A, Gygi SP et al (2007) Abraxas and RAP80 form a BRCA1 protein complex required for the DNA damage response. Science 316:1194–1198. doi:10.1126/science.1139476
Yu X, Wu LC, Bowcock AM, Aronheim A, Baer R (1998) The C-terminal (BRCT) domains of BRCA1 interact in vivo with CtIP, a protein implicated in the CtBP pathway of transcriptional repression. J Biol Chem 273:25388–25392. doi:10.1074/jbc.273.39.25388
Wooster R, Neuhausen SL, Mangion J, Quirk Y, Ford D, Collins N et al (1994) Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q12-13. Science 265:2088–2090. doi:10.1126/science.8091231
Wooster R, Bignell G, Lancaster J, Swift S, Seal S, Mangion J et al (1995) Identification of the breast cancer susceptibility gene BRCA2. Nature 378:789–792. doi:10.1038/378789a0
Sharan SK, Morimatsu M, Albrecht U, Lim DS, Regel E, Dinh C et al (1997) Embryonic lethality and radiation hypersensitivity mediated by Rad51 in mice lacking BRCA2. Nature 386:804–810. doi:10.1038/386804a0
Wong AK, Pero R, Ormonde PA, Tavtigian SV, Bartel PL (1997) RAD51 interacts with the evolutionarily conserved BRC motifs in the human breast cancer susceptibility gene BRCA2. J Biol Chem 272:31941–31944. doi:10.1074/jbc.272.51.31941
Xu X, Weaver Z, Linke SP, Li C, Gotay J, Wang XW et al (1999) Centrosome amplification and a defective G2-M cell cycle checkpoint induce genetic instability in BRCA1 exon 11 isoform-deficient cells. Mol Cell 3:389–395. doi:10.1016/S1097-2765(00)80466-9
Yu VP, Koehler M, Steinlein C, Schmid M, Hanakahi LA, van Gool AJ et al (2000) Gross chromosomal rearrangements and genetic exchange between nonhomologous chromosomes following BRCA2 inactivation. Genes Dev 14:1400–1406
Davies AA, Masson JY, McIlwraith MJ, Stasiak AZ, Stasiak A, Venkitaraman AR et al (2001) Role of BRCA2 in control of the RAD51 recombination and DNA repair protein. Mol Cell 7:273–282. doi:10.1016/S1097-2765(01)00175-7
Moynahan ME, Pierce AJ, Jasin M (2001) BRCA2 is required for homology-directed repair of chromosomal breaks. Mol Cell 7:263–272. doi:10.1016/S1097-2765(01)00174-5
Shin S, Verma IM (2001) BRCA2 cooperates with histone acetyltransferases in androgen receptor-mediated transcription. Proc Natl Acad Sci USA 2003 100(12):7201–7206
Marmorstein LY, Kinev AV, Chan GK, Bochar DA, Beniya H, Epstein JA et al (2001) A human BRCA2 complex containing a structural DNA binding component influences cell cycle progression. Cell 104:247–257. doi:10.1016/S0092-8674(01)00209-4
Bochar DA, Wang L, Beniya H, Kinev A, Xue Y, Lane WS et al (2000) BRCA1 is associated with a human SWI/SNF-related complex linking chromatin remodeling to breast cancer. Cell 102:257–265. doi:10.1016/S0092-8674(00)00030-1
Morris JR, Solomon E (2004) BRCA1: BARD1 induces the formation of conjugated ubiquitin structures, dependent on K6 of ubiquitin, in cells during DNA replication and repair. Hum Mol Genet 13:807–817. doi:10.1093/hmg/ddh095
Puget N, Torchard D, Serova-Sinilnikova OM, Lynch HT, Feunteun J, Lenoir GM et al (1997) A 1-kb Alu-mediated germ-line deletion removing BRCA1 exon 17. Cancer Res 57:828–831
Puget N, Sinilnikova OM, Stoppa-Lyonnet D, Audoynaud C, Pages S, Lynch HT et al (1999) An Alu-mediated 6-kb duplication in the BRCA1 gene: a new founder mutation? Am J Hum Genet 64:300–302. doi:10.1086/302211
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D et al (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81:559–575. doi:10.1086/519795
Hogervorst FB, Nederlof PM, Gille JJ, McElgunn CJ, Grippeling M, Pruntel R et al (2003) Large genomic deletions and duplications in the BRCA1 gene identified by a novel quantitative method. Cancer Res 63:1449–1453
Thomassen M, Gerdes AM, Cruger D, Jensen PK, Kruse TA (2006) Low frequency of large genomic rearrangements of BRCA1 and BRCA2 in western Denmark. Cancer Genet Cytogenet 168:168–171. doi:10.1016/j.cancergencyto.2005.12.016
Lahti-Domenici J, Rapakko K, Paakkonen K, Allinen M, Nevanlinna H, Kujala M et al (2001) Exclusion of large deletions and other rearrangements in BRCA1 and BRCA2 in Finnish breast and ovarian cancer families. Cancer Genet Cytogenet 129:120–123. doi:10.1016/S0165-4608(01)00437-X
Moisan AM, Fortin J, Dumont M, Samson C, Bessette P, Chiquette J et al (2006) No evidence of BRCA1/2 genomic rearrangements in high-risk French-Canadian breast/ovarian cancer families. Genet Test 10:104–115. doi:10.1089/gte.2006.10.104
Gad S, Caux-Moncoutier V, Pages-Berhouet S, Gauthier-Villars M, Coupier I, Pujol P et al (2002) Significant contribution of large BRCA1 gene rearrangements in 120 French breast and ovarian cancer families. Oncogene 21:6841–6847. doi:10.1038/sj.onc.1205685
de la Hoya M, Gutierrez-Enriquez S, Velasco E, Osorio A, Sanchez de Abajo A, Vega A et al (2006) Genomic rearrangements at the BRCA1 locus in Spanish families with breast/ovarian cancer. Clin Chem 52:1480–1485. doi:10.1373/clinchem.2006.070110
Hartmann C, John AL, Klaes R, Hofmann W, Bielen R, Koehler R et al (2004) Large BRCA1 gene deletions are found in 3% of German high-risk breast cancer families. Hum Mutat 24:534. doi:10.1002/humu.9291
Vasickova P, Machackova E, Lukesova M, Damborsky J, Horky O, Pavlu H et al (2007) High occurrence of BRCA1 intragenic rearrangements in hereditary breast and ovarian cancer syndrome in the Czech Republic. BMC Med Genet 8:32. doi:10.1186/1471-2350-8-32
Petrij-Bosch A, Peelen T, van Vliet M, van Eijk R, Olmer R, Drusedau M et al (1997) BRCA1 genomic deletions are major founder mutations in Dutch breast cancer patients. Nat Genet 17:341–345. doi:10.1038/ng1197-341
Agata S, Viel A, Della Puppa L, Cortesi L, Fersini G, Callegaro M et al (2006) Prevalence of BRCA1 genomic rearrangements in a large cohort of Italian breast and breast/ovarian cancer families without detectable BRCA1 and BRCA2 point mutations. Genes Chromosomes Cancer 45:791–797. doi:10.1002/gcc.20342
Gad S, Klinger M, Caux-Moncoutier V, Pages-Berhouet S, Gauthier-Villars M, Coupier I et al (2002) Bar code screening on combed DNA for large rearrangements of the BRCA1 and BRCA2 genes in French breast cancer families. J Med Genet 39:817–821. doi:10.1136/jmg.39.11.817
Peelen T, van Vliet M, Bosch A, Bignell G, Vasen HF, Klijn JG et al (2000) Screening for BRCA2 mutations in 81 Dutch breast-ovarian cancer families. Br J Cancer 82:151–156. doi:10.1054/bjoc.1999.0892
Tournier I, Paillerets BB, Sobol H, Stoppa-Lyonnet D, Lidereau R, Barrois M et al (2004) Significant contribution of germline BRCA2 rearrangements in male breast cancer families. Cancer Res 64:8143–8147. doi:10.1158/0008-5472.CAN-04-2467
Woodward AM, Davis TA, Silva AG, Kirk JA, Leary JA (2005) Large genomic rearrangements of both BRCA2 and BRCA1 are a feature of the inherited breast/ovarian cancer phenotype in selected families. J Med Genet 42:e31. doi:10.1136/jmg.2004.027961
Couch FJ, DeShano ML, Blackwood MA, Calzone K, Stopfer J, Campeau L et al (1997) BRCA1 mutations in women attending clinics that evaluate the risk of breast cancer. N Engl J Med 336:1409–1415. doi:10.1056/NEJM199705153362002
Ramus SJ, Harrington PA, Pye C, DiCioccio RA, Cox MJ, Garlinghouse-Jones K et al (2007) Contribution of BRCA1 and BRCA2 mutations to inherited ovarian cancer. Hum Mutat 28:1207–1215. doi:10.1002/humu.20599
Preisler-Adams S, Schonbuchner I, Fiebig B, Welling B, Dworniczak B, Weber BH (2006) Gross rearrangements in BRCA1 but not BRCA2 play a notable role in predisposition to breast and ovarian cancer in high-risk families of German origin. Cancer Genet Cytogenet 168:44–49. doi:10.1016/j.cancergencyto.2005.07.005
Kremeyer B, Soller M, Lagerstedt K, Maguire P, Mazoyer S, Nordling M et al (2005) The BRCA1 exon 13 duplication in the Swedish population. Fam Cancer 4:191–194. doi:10.1007/s10689-004-7023-2
Lim YK, Lau PT, Ali AB, Lee SC, Wong JE, Putti TC et al (2007) Identification of novel BRCA large genomic rearrangements in Singapore Asian breast and ovarian patients with cancer. Clin Genet 71:331–342. doi:10.1111/j.1399-0004.2007.00773.x
Unger MA, Nathanson KL, Calzone K, Antin-Ozerkis D, Shih HA, Martin AM et al (2000) Screening for genomic rearrangements in families with breast and ovarian cancer identifies BRCA1 mutations previously missed by conformation-sensitive gel electrophoresis or sequencing. Am J Hum Genet 67:841–850. doi:10.1086/303076
Agata S, Dalla Palma M, Callegaro M, Scaini MC, Menin C, Ghiotto C et al (2005) Large genomic deletions inactivate the BRCA2 gene in breast cancer families. J Med Genet 42:e64. doi:10.1136/jmg.2005.032789
Acknowledgements
Lis Krüger and Lis Nielsen are acknowledged for excellent technical assistance. This study was supported by the Neye Foundation.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2008_88_MOESM1_ESM.pdf
Supplementary Fig. 1. SNP array analsis of genomic DNA from patients with BRCA1 exon 3-16 deletion. For each chromosome the length of the possible shared haplotypes are shown as lines above the SNP density of the same chromsome. The SNP density is not completely uniform across the genome and some regions, like centromeric regions, have little of no SNPs on the chip. The largest possible shared haplotype at postion 34,179,358-39,461,220 on chromosome 17 around the BRCA1 region that consists of 301 SNPs. The possible shared haplotype with the second largest number of SNP is on chromosome 12 at position 86,691,951 to 88,423,908 and contains 68 SNPs and is 1.26 Mb long. (PDF 448 kb)
Rights and permissions
About this article
Cite this article
Hansen, T.v.O., Jønson, L., Albrechtsen, A. et al. Large BRCA1 and BRCA2 genomic rearrangements in Danish high risk breast-ovarian cancer families. Breast Cancer Res Treat 115, 315–323 (2009). https://doi.org/10.1007/s10549-008-0088-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0088-0