Abstract
Background The risk of developing breast cancer is strongly correlated with the overall exposure to oestrogen and most tumours are more or less dependent on oestrogen for their growth. A great majority of breast cancers occur after menopause when the ovaries have ceased to be functional, yet breast tumours in postmenopausal women maintain high intratumoural oestrogen concentrations, primarily through enzymatic conversion of androgenic precursors. Patients with a hormone dependent tumour generally receive the anti-oestrogen tamoxifen that mediate its anti-tumour effect by competing with oestrogen for binding to the oestrogen-receptor (ER). We therefore propose that the levels of oestrogen producing enzymes may affect the prognosis in postmenopausal breast cancer patients treated with tamoxifen. Methods We measured the mRNA and protein levels of aromatase and sulfatase by real-time PCR (n = 161) and immunohistochemistry (n = 131) in postmenopausal women with breast cancer. Results A significant better recurrence-free survival was detected in patients with weak or high protein expression of stromal aromatase (P = 0.0008), as also demonstrated by a decreased relative risk (RR = 0.50, CI = 0.33–0.76, P = 0.003). When we combined patients with weak and high stromal aromatase and selected only ER-positive patients, the improved prognosis was even more evident (P = 0.0000) and was shown to be a significant prognostic factor in a multivariate Cox-model (HR = 0.15, CI = 0.06–0.39, P = 0.000). The mRNA expression of aromatase and sulfatase, as well as the protein expression of sulfatase revealed no prognostic significance. Conclusion Protein expression of stromal aromatase may serve as a significant prognostic marker in ER-positive patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most frequently diagnosed cancer in western women [1–3] and approximately 2/3 of postmenopausal patients have oestrogen-dependent carcinomas [4]. Tamoxifen given for five years is standard endocrine therapy in oestrogen-receptor (ER) positive breast cancers with a reduction of both recurrence and mortality [5–8]. Still, at least one third of ER-positive breast cancers can be defined as de novo or primary resistant and in addition almost 50% of all ER-positive mammary carcinoma fail to respond to tamoxifen even though they initially were sensitive [8, 9]. The mechanisms underlying the resistance to tamoxifen are complex and not fully understood. However, since tamoxifen mediates its anti-tumour effects by competing with oestrogen for binding to the ER [10, 11] one such mechanism of treatment failure could be the concentration of oestrogens in the tumour. The circulating levels of oestrogens are low in postmenopausal women, but the mammary gland produce concentrations that are higher than in serum [12]. In breast cancers of postmenopausal women local oestrogen levels have shown to be up to 20 times higher than in plasma, which may depend on the tumours ability to produce factors stimulating the local production of oestrogens from circulating precursors [13].
Two major pathways are considered to be involved in the local synthesis of oestrogens. One is aromatisation of androstenedione to oestrone or testosterone to oestradiol by the enzyme aromatase. The other is conversion of oestrone-sulfate to oestrone by the enzyme sulfatase. The latter seems to have greater impact on the local level of oestrogens, since oestrone-sulfate is the major circulating form of plasma oestrogen [14–19]. Moreover, the level of sulfatase expression and activity in human breast tumours has been shown to be higher than that of aromatase [12, 20–24].
In the current study it was hypothesised that the local levels of enzymes participating in the biosynthesis of oestrogens may influence the outcome of breast cancer patients treated with tamoxifen. Both mRNA and protein expression levels of aromatase and sulfatase were screened for and correlated with clinicopathologic factors to elucidate their prognostic role.
Materials and methods
Patients
The present study included 161 postmenopausal patients with a breast cancer in stage II or III, diagnosed between 1985 and 1994 in the South East Health Care Region of Sweden. The daily dose of tamoxifen was 40 mg. Oestrogen-receptor (ER) and progesterone-receptor (PgR) content was measured in clinical routine practice by isoelectric focusing before 1988, and later on with enzyme immunoassay (EIA). Samples with concentrations of ≥0.1 fmol/μg (or ≥0.3 fmol/μg with EIA) were classified as positive. The mean follow-up time was 9.5 years (range: 0.08–16.9 years, median: 11 years). The local ethical committee in Linköping, Sweden approved the study.
RNA isolation
Fresh frozen breast cancer tissues (∼30 mg) were homogenised using a micro-dismembrator (B Braun, Melsungen, Germany) and total RNA was isolated utilising SV Total RNA Isolation System (Promega, Madison, WI, USA). Briefly, weighed tissues were placed into liquid nitrogen for about 10 min followed by 35 s of disruption and homogenisation at 2900 rpm. The disrupted tissue was immediately transferred to 225 μl of SV RNA Lysis Buffer, and then 350 μl of RNA Dilution Buffer was added to the lysate before heating at 70°C for 3 min. After centrifugation, 175 μl of the clear lysate was taken for further procedures according to the manufacturer’s instruction. The purified RNA was eluted in nuclease-free water and stored at −70°C until use.
cDNA synthesis
Total RNA was reversed transcribed into cDNA in a final volume of 20 μl using. SuperScript™II Reverse Transcriptase (Invitrogen™, Life Technologies, Stockholm, Sweden). For aromatase and sulfatase each cDNA synthesis mixture contained: 1–5 μg of total RNA, 4 μl of 5× first strand buffer (Invitrogen™ Life Technologies, Stockholm, Sweden), 1 μl of 10 mM dNTP Mix (Invitrogen™ Life Technologies, Stockholm, Sweden), 13 units of RNAguard RNase Inhibitor (Amersham Biosciences, Uppsala, Sweden), 200 units of reverse transcriptase, 0.25 μg random primers (Invitrogen™ Life Technologies, Stockholm, Sweden), water up to 20 μl. The following thermal conditions were recommended; 42°C for 50 min followed by an inactivation at 70°C for 15 min.
Real-time PCR
A relative quantification method was applied for measuring the mRNA levels of aromatase and sulfatase using a standard curve, which was constructed with four-fold serial dilutions of cDNA from human Breast Cancer Total RNA (Ambion®. Standard curves were produced for the two target genes and for an endogenous control (i.e. β-actin) in each run. The target message in unknown samples was quantified to determine a relative measure of the starting quantities. A relative quantity was calculated by dividing the mean Ct-value of the gene of interest with the mean Ct-value of the endogenous control. The data output was then expressed as a fold-difference of expression levels. PCR assays were constructed in 23 μl in duplicates for each sample and standard curve dilution using a 96-well reaction plate in ABI PRISM™ 7700 Sequence Detector (PE Applied Biosystems, Stockholm, Sweden). The PCR reaction mixture for each double assay (50 μl) of aromatase mRNA and sulfatase mRNA was composed of 25 μl of qPCR MasterMix Plus (Eurogentec SA LIEGE Science Park, Ougrée, Belgium), 2.5 μl of primers (stock: 18 μM) and probe (stock: 5 μM) mixture for aromatase, sulfatase, and β-actin respectively (Assays-on-Demand™ Gene Expression Products, Applied Biosystems, Stockholm, Sweden), 9 μl of cDNA, and water up to 50 μl. Primers and probe mixture for β-actin gene detection was Pre-Developed TaqMan® Assay Reagents, Human B-actin (20×) (Applied Biosystems, Stockholm, Sweden). Settings for the PCR thermal profile were: 50°C for 2 min and 95°C for 10 min followed by 40 cycles of 95°C for 15 s and 60°C for 60 s. The Sequence Detection System version 1.7a made all desired calculations.
Tissue microarray and immunohistochemistry
Formalin-fixed and paraffin-embedded tumour material was available for 131 of the 161 patients included in the study. Morphologically representative areas were selected and assembled in a tissue microarray. In brief, three 0.8 mm cylindrical cores from each breast cancer specimen were placed in a recipient paraffin block with a maximal of 243 cores, including liver as control. The tissue microarray blocks were then cut with a microtome into 4 μm thick sections and mounted onto glass slides. The slides were deparaffinised with xylene, rehydrated in decreasing series of ethanol and finally rinsed in distilled water. Antigen retrieval was accomplished by placing the slides in 10 mM citrate buffer (pH 6.0), incubate in high pressure cooker, followed by cooling and washing in phosphate buffer saline (PBS)/0.2% BSA at pH 7.4. After quenching endogenous peroxidase activity with 3% H2O2 in methanol, the slides were incubated with serum-free protein blocking solution (DakoCytomation, Glostrup, Denmark) for 10 min in order to block non-specific immunostaining. Separate slides were incubated with primary antibodies at 4°C over night; mouse polyclonal antibody against a partial recombinant sulfatase (1:300 dilution, Abnova Corporation, Taipei, Taiwan) and mouse monoclonal antibody against human aromatase (1:5 dilution, Acris Antibodies, Hiddenhausen, Germany). After washing with PBS/0.2% BSA, the slides were incubated with respective secondary anti-body (EnVision HRP anti-rabbit or anti-mouse DAKO) for 30 min. Bound antibodies were stained with diaminobenzidine and counterstained with haematoxillin. The slides were finally dehydrated in series of ethanol and mounted.
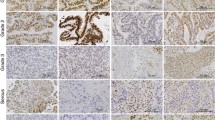
Immunohistochemical scoring
Two observers (PW and SW) first evaluated the slides independently and then an additional scoring was performed simultaneously. The distribution of immunoreactivity was estimated as proportion of staining. If more than 1/3 of the sections were stained the sample was defined as positive (1). Staining intensity of the immunoreactions was recorded as 0, negative; 1, weak; 2, strong. The proportion and intensity scores were then put together to obtain a total score (proportion of staining + the staining intensity), which ranged from 0 to 4. The final categorisation revealed three groups: negative (total score 0), weak (total score 1–2), and strong (total score 3–4). Patients were excluded when tissues were non-representative or missing. All immunohistochemical evaluations were performed without knowledge of tumour characteristics and clinical outcome. Aromatase protein expression was found in the cytoplasm of carcinoma cells and/or in the stroma surrounding the tumour cells. Sulfatase was detected in the cytoplasm of breast cancer cells whereas the stroma was negative.
Statistical analyses
Statistical Package for Social Sciences (SPSS) Advanced Models™ 12.0 software was used for the statistical analyses. To examine the relationship between the mRNA/protein expression and tumour characteristics and to calculate the mRNA/protein expression levels and the relative risk of recurrence we used Pearson’s χ 2 and correlation (R) tests. In the χ 2 tests weak and strong staining for protein expression of aromatase were grouped together and defined as positive expression. The survival curves of recurrences were estimated using the Kaplan–Meier method and the differences between survival rates for patients with different expression levels was assessed by Log-Rank test. Further, we performed a multivariate Cox-model in order to adjust for the tumour characteristics between the different expression profiles. Differences between groups were judged significant at confidence levels greater than 95% (P < 0.05).
Results
Real-time PCR and immunohistochemistry
Messenger RNA expression of sulfatase and aromatase was detected in all of the 161 tumours and to discriminate between the expression levels patients were divided according to the median. Protein expression of sulfatase was detected in cancer epithelial cells in 123 cases and no patient was without immunoreactivity. The staining was therefore divided into two categories: 1, weak staining (76 cases); and 2, strong staining (47 cases). Aromatase protein expression was found in the cytoplasm of carcinoma cells (122 cases) and in the stroma (124 cases). 70 patients showed expression of aromatase in both cell structures. The immunoreactivity for aromatase was divided into three categories; 0, negative staining; 1, weak staining; and 2, strong staining. No correlation could be seen between mRNA and protein expression levels (data not shown).
Tumour characteristics
The association between mRNA/protein expression and tumour characteristics including tumour size, lymph node status, oestrogen (ER) and progesterone receptors (PgR), and S-phase fraction is shown in Tables 1 and 2. Patients with high expression of sulfatase mRNA had more often a tumour with S-phase fraction less than 10 % (P = 0.03) (Table 1). No significant relationship between aromatase mRNA expression and any of the clinicopathological factors could be seen, even though there was a trend for an association between high mRNA expression of aromatase and ER-positivity (P = 0.09).
The protein expression of cancer epithelial aromatase showed a significantly positive correlation to lymph-node status and S-phase fraction (P = 0.04 and P = 0.02, respectively) (Table 2). There was also a negative correlation between epithelial aromatase and tumour size (P = 0.02). Stromal aromatase expression showed borderline significance for an association with PgR-status and S-phase fraction. Those with positive expression of stromal aromatase were more often PgR-positive (P = 0.06) and had tumours with low S-phase fraction (P = 0.06).
Recurrence-free survival and relative risk of recurrence
Recurrence-free survival (RFS) was defined as the time from initial surgery to the clinically documented date of local or distant recurrences, or breast cancer related death. The relative risks of having a relapse among ER-positive and ER-negative postmenopausal breast cancer patients in relation to sulfatase and aromatase mRNA or protein expression are shown in Table 3. Patients with a positive expression of stromal aromatase showed a significantly decreased risk of recurrence or breast cancer related death (RR = 0.50, CI = 0.33–0.76, P = 0.003). In the Kaplan–Meier estimates of the total population (both ER-positive and ER-negative cases) patients with a weak or high protein expression of aromatase in the stroma had a significantly better prognosis than those without expression (P = 0.0008) (Fig. 1). For epithelial aromatase we could see a tendency for a dose response series, with a better prognosis in patients in the higher range of expression (Fig. 2). When we combined patients with weak and high stromal aromatase and selected only ER-positive patients the improved prognosis was even more evident (P = 0.0000) (Fig. 3). We also calculated the prognostic value of aromatase in ER-positive patients with a tumour positive or negative for PgR. Patient’s positive for both ER and PgR showed a significantly better RFS compared to those lacking PgR, if the tumour was positive for stromal aromatase (P = 0.05). In a multivariate Cox-model (adjusted for tumour size, nodal status, and S-phase fraction) high stromal aromatase was demonstrated to be a significant prognostic factor (All patients: HR = 0.35, CI = 0.16–0.76, P = 0.008, ER-positive patients: HR = 0.15, CI = 0.06–0.38, P = 0.000).
No significant difference could be seen among the other expression parameters, even if patients with high sulfatase protein expression tended to have a better RFS (P = 0.09).
Discussion
Today, there is substantial evidence that breast cancer tissues contain enzymes necessary for the local biosynthesis of oestrogen from circulating precursors, which is believed to play an important role in the development and progression of hormone dependent breast cancer, especially in the postmenopausal patient [12, 17, 25–30]. In the current investigation, we measured the mRNA and protein levels of enzymes involved in local oestrogen synthesis (i.e., aromatase and sulfatase) in postmenopausal women with breast cancer. We found that expression of aromatase in the surrounding stroma was a significant prognostic factor in ER-positive patients, with an improved relapse free survival in cases with positive expression. In support to our findings several researchers have described that breast cancer patients who had tumours expressing aromatase showed a prolonged RFS in comparison to those lacking or having a low expression [31–33]. In the present study, as well as in a report by Yamamoto et al. [31], there was also a trend for a better RFS in patients with high expression of cancer epithelial sulfatase although not statistically significant (P = 0.09). Others have however reported opposite results both in relation to clinical and pathological factors as well as RFS [20, 30, 34, 35]. One of the suggestions due to the varying results is the use of different commercial antibodies with variable sensibility [36, 37], but it may also be a consequence of the use of diverse treatment strategies in different patient cohorts. The results of aromatase and sulfatase protein expression in the current patient cohort were in contrary to our initial hypothesis where those with a high expression of aromatase and sulfatase were expected to relapse earlier as they retain the capacity of oestrogen synthesis given the tumour a growth advantage. However, since all patients received tamoxifen our results of aromatase and sulfatase may reflect an oestrogen dependency and the improved prognosis might therefore be the consequence of tamoxifen response. This hypothesis is partly supported by our observation that ER-positive patients with tumours co-expressing PgR had prolonged RFS compared to those lacking PgR, because PgR is induced by oestrogens at the transcriptional level and is recognised to be associated with a better prognosis and treatment response.
When using immunohistochemistry on tumour specimen’s aromatase expression was found both in the stroma and in tumour epithelial cells, which is in agreement with what others have seen [29, 38–42]. Interestingly, we found that protein expression of stromal but not cancer epithelial aromatase was related to breast cancer prognosis. This observation is supported by activity studies showing a higher enzyme activity of aromatase in the stroma compared to normal epithelium and cancer epithelial cells [23, 43]. Several investigations of aromatase protein expression and its correlation to patient outcome have been carried out without discriminating between stromal and epithelial localisation [32, 33, 44], which generate difficulties in comparing results between studies.
We also measured the mRNA levels of sulfatase and aromatase and did not find any significant correlation between mRNA and protein levels. Furthermore, the mRNA levels showed no significant influence on the RFS in the postmenopausal breast cancer patients examined. Nevertheless, we did find a trend for a relationship between high aromatase mRNA levels and ER-positivity, which is in accordance with reports by Brodie et al. [40] and Salhab et al. [35]. However, despite a substantial amount of data there is no consensus concerning the relationship between the expression of sulfatase or aromatase and risk of disease recurrence, or clinicopathological parameters [18, 31–35, 42, 45].
When we compared the protein expression of aromatase and sulfatase with clinicopathological parameters we found that high aromatase in cancer epithelial cells correlated significantly with lymph-node positivity and low expression with low S-phase. This is to some extent logical, since high aromatase would generate more oestrogen and promote tumour growth and the tumour might in turn be more prone to metastasise. The correlation between expression of stromal aromatase and the presence of PgRs seems reasonable since it is in accordance with the concept of PgR being an indicator of oestrogen activity and signifies that ER in the tumour is biologically active.
In conclusion, emerging data implies that breast cancer is regulated by the interaction with stromal cells surrounding the tumour and it is also well known that this tumour-stromal cross-talk regulates aromatase gene expression by the production of various factors such as PGE2, COX2, TNFα, IL-6 and IL-11 [46–50]. It is therefore of importance to elucidate the signalling mechanisms underlying the communication between stromal- and epithelial cell compartments in breast cancer for further knowledge of breast cancer and anti-oestrogen response. In support with the present results we suggest that stroma aromatase may have a significant role in this complex context.
References
Parkin DM (1998) Epidemiology of cancer: global patterns and trends. Toxicol Lett 102–103:227–234
Parkin DM (2004) International variation. Oncogene 23:6329–6340
Lutz JM, Francisci S, Mugno E, Usel M, Pompe-Kirn V, Coeberg JW, Bieslka-Lasota M, EUROPREVAL Working Group (2003) Cancer prevalence in Central Europe: the EUROPREVAL Study. Ann Oncol 14:313–322
Pertschuk LP, Kim DS, Nayer K, Feldman JG, Eisenberg KB, Carter AC, Rong ZT, Thelmo WL, Fleisher J, Greene GL (1990) Immunocytochemical estrogen and progestin receptor assays in breast cancer with monoclonal antibodies. Histopathologic, demographic, and biochemical correlations and relationship to endocrine response and survival. Cancer 66:1663–1670
Early Breast Cancer Trialist’s Collaborative Group (EBCTCG) (1998) Tamoxifen for early breast cancer: an overview of the randomized trials. Lancet 352:1451–1467
Macgregor JI, Jordan VC (1998) Basic guide to the mechanisms of antiestrogen action. Pharmacol Rev 50:151–196
Howell A, Howell SJ, Evans DG (2003) New approaches to the endocrine prevention and treatment of breast cancer. Cancer Chemother Pharmacol 52:S39–S44
Schiff R, Massarweh S, Shou J, Osborne CK (2003) Breast cancer endocrine resistance: how growth factor signaling and estrogen receptor coregulators modulate response. Clin Cancer Res 9:447s–454s
Berstein LM, Wang J-P, Zheng H, Yue W, Conaway M, Santen RJ (2004) Long-term exposure to tamoxifen induces hypersensitivity to estradiol. Clin Cancer Res 10:1530–1534
Dhingra K (1999) Antiestrogens-tamoxifen, SERMs and beyond. Invest New Drugs 17:285–311
Clemons M, Damson S, Howell A (2002) Tamoxifen (‘Nolvadex’): a review. Cancer Treat Rev 28:165–180
Pasqualini JR, Chetrite G, Blacker C, Feinstein MC, Delalonde L, Talbi M, Maloche C (1996) Concentrations of estrone, estradiol, and estrone sulfate and evaluation of sulfatse and aromatase activities in pre- and postmenopausal breast cancer patients. J Clin Endocrinol Metab 81:1460–1464
Simpson ER, Davis SR (2001) Minireview: Aromatase and the regulation of estrogen biosynthesis-some new perspectives. Endocrinology 142:4589–4594
Dao TL, Hayes C, Libby PR (1974) Steroid sulfatase activities in human breast tumors. Proc Soc Exp Biol Med 146:381–384
Miller WR, Hawkins RA, Forrest AM (1982) Significance of aromatase activity in human breast cancer. Cancer Res 42:3365s–3368s
Pasqualini JR, Gelly C, Lecerf F (1986) Estrogen sulfates: biological and ultrastructural responses and metabolism in MCF-7 human breast cancer cells. Breast Cancer Res Treat 8:233–240
Sasano H, Harada N (1998a) Intratumoral aromatase in human breast, endometrial, and ovarian malignancies. Endocrine Rev 19:593–607
Utsumi T, Yoshimura N, Takeuchi S, Ando J, Maruta M, Maeda K, Harada N (1999) Steroid sulfatase expression is an independent predictor of recurrence in human breast cancer. Cancer Res 59:377–381
Nakata T, Takashima S, Shiotsu Y, Murakata C, Ishida H, Akinaga S, Li PK, Sasano H, Suzuki T, Saeki T (2003) Role of steroid sulfatase in local formation of estrogen in post-menopausal breast cancer patients. J Steroid Biochem Mol Biol 86:455–460
Evans TR, Rowlands MG, Luqmani YA, Chander SK, Coombes RC (1993) Detection of breast cancer-associated estrone sulfatase in breast cancer biopsies and cell lines using polymerase chain reaction. J Steroid Biochem Mol Biol 46:195–201
Evans TR, Rowlands MG, Law M, Coombes RC (1994) Intratumoral oestrone sulphatase activity as a prognostic marker in human breast carcinoma. Br J Cancer 69:555–561
Santner SJ, Feil PD, Santen RJ (1984) In situ estrogen production via the estrone sulfatase pathway in breast tumors: relative importance versus the aromatase pathway. J Clin Endocrinol Metab 59:29–33
Santner SJ, Pauley RJ, Tait L, Kaseta J, Santen RJ (1997) Aromatase activity and expression in breast cancer and benign breast tissue stromal cells. J Clin Endocrinol Metab 82:200–208
Pasqualini JR, Maloche C, Maroni M, Chetrite G (1994) Effect of the progestagen promegestone (R-5020) on mRNA of the oestrone sulphatase in the MCF-7 human mammary cancer cells. Anticancer Res 14:1589–1593
Miller WR, O’Neill JS (1987) The importance of local synthesis of oestrogen within the breast. Steroids 50:537–547
Chetrite GS, Cortes-Prieto J, Philippe JC, Wright F, Pasqualini JR (2000) Comparison of oestrogen concentrations, oestrone sulfatase and aromatase activities in normal, and in cancerous, human breast tissues. J Steroid Biochem Mol Biol 72:23–27
Utsumi T, Yoshimura N, Takeuchi S, Maruta M, Maeda K, Harada N (2000) Elevated steroid sulfatase expression in breast cancer. J Steroid Biochem Mol Biol 73:141–145
Miyoshi Y, Ando A, Shiba E, Taguchi T, Tamaki Y, Noguchi S (2001) Involvement of up-regulation of 17-β-hydroxysteroid dehydrogenase type I in maintenance of high intratumoural high estradiol levels in postmenopausal breast cancers. Int J Cancer 94:685–689
Esteban JM, Warsi Z, Haniu M, Hall P, Shively JE, Chen S (1992) Detection of intratumoral aromatase in breast carcinoma. An immunohistochemical study with clinicopathologic correlation. Am J Pathol 140:337–343
Suzuki T, Nakata T, Miki Y, Kaneko C, Moriya T, Ishida T, Akinaga S, Hirakawa H, Kimura M, Sasano H (2003) Estrogen sulfotransferase and steroid sulfatase in human breast carcinoma. Cancer Res 63:2762–2770
Yamamoto Y, Yamashita J, Toi M, Muta M, Nagai S, Hanai N, Furuya A, Osawa Y, Saji S, Ogawa M (2003) Immunohistochemical analysis of estrone sulfatase and aromatase in human breast cancer tissues. Oncol Rep 10:791–796
Zhang Z, Yamashita H, Toyama T, Omoto Y, Suguira H, Hara Y, Wu X, Kobayashi S, Iwase H (2003) Quantitative determination, by real-time reverse transcription polymerase chain reaction, of aromatase mRNA in invasive ductal carcinoma of the breast. Breast Cancer Res 5:R250–256
Yoshimura N, Harada N, Bukholm I, Kåresen R, Borresen-Dale AL, Kristensen VN (2004) Intratumoral mRNA expression of genes from the oestradiol metabolic pathway and clinical and histopatological parameters of breast cancer. Breast Cancer Res 6:R46–R55
Girault I, Lerebours F, Tozlu S, Spyratos F, Tubiana-Hulin M, Lidereau R, Bièche I (2002) Real-time reverse transcription PCR assay of CYP19 expression: application to a well-defined series of post-menopausal breast carcinomas. J Steroid Biochem Mol Biol 82:323–332
Salhab M, Reed MJ, Al Sarakbi W, Jiang WG, Mokbel K (2006) The role of aromatase and 17-ß-hydroxysteroid dehydrogenase type 1 mRNA expression in predicting the clinical outcome of human breast cancer. Breast Cancer Res Treat 99:155–162
Sasano H, Murakami H (1998b) Immunolocalization of aromatase in human breast disorders using different antibodies. Breast Cancer Res Treat 49:S79–S84
Sasano H, Anderson TJ, Silverberg SG, Santen RJ, Conway M, Edwards DP, Krause A, Bhatnagar AS, Evans DB, Miller WR (2005) The validation of new aromatase monoclonal antibodies for immunohistochemistry–a correlation with biochemical activities in 46 cases of breast cancer. J Steroid Biochem Mol Biol 96:35–39
Sasano H, Nagura H, Harada N, Goukon Y, Kimura M (1994) Immunolocalization of aromatase and other steroidogenic enzymes in human breast disorders. Hum Pathol 25:530–535
Lu Q, Nakmura J, Savinov A, Yue W, Weisz J, Dabbs DJ, Wolz G, Brodie A (1996) Expression of aromatase protein and messenger ribonucleic acid in tumor epithelial cells and evidence of functional significance of locally produced estrogen in human breast cancers. Endocrinology 137:3061–3068
Brodie A, Lu Q, Nakamura J (1997) Aromatase in the normal breast and breast cancer. J Steroid Biochem Mol Biol 61:281–284
Singer CF, Fink-Retter A, Gschwantler-Kaulich D, Thalhammer T, Hudelist G, Mueller R, Czerwenka K, Kubista E (2006) Selective spatial upregulation of intratumoral stromal aromatase in breast cancer patients: evidence for imbalance of local estrogen metabolism. Endocr Relat Cancer 13:1101–1107
Miki Y, Suzuki T, Tazawa C, Yamaguchi Y, Kitada K, Honma S, Moriya T, Hirakawa H, Evans DB, Hayashi S, Ohychi N, Sasano H (2007) Aromatase localization in human breast cancer tissues: Possible interactions between intratumoral stroma and parenchymal cells. Cancer Res 67:3945–3954
Santen RJ, Martel J, Hoagland M, Naftolin F, Roa L, Harada N, Hafer L, Zaino R, Pauley R, Santner S (1998) Demonstration of aromatase activity and its regulation in breast tumor and benign breast fibroblasts. Breast Cancer Res Treat 49:S93–S99
Lu J, Li H, Cao D, Di G, Wu J, Sheng K, Han Q, Shen Z, Shao Z (2007) Clinical significance of aromatase protein expression in axillary node negative breast cancer. J Cancer Res Clin Oncol 133:401–409
Miyoshi Y, Ando A, Hasegawa S, Ishitobi M, Taguchi T, Tamaki Y, Noguchi S (2003) High expression of steroid sulfatase mRNA predicts poor prognosis in patients with estrogen receptor-positive breast cancer. Clin Cancer Res 9:2288–2293
Crichton MB, Nichols JE, Zhao Y, Bulun SE, Simpson ER (1996) Expression of transcripts of interleukin-6 and related cytokines by human breast tumors, breast cancer cells, and adipose stromal cells. Mol Cell Endocrinol 118:215–220
Zhao Y, Nichols JE, Valdez R, Mendelson CR, Simpson ER (1996) Tumor necrosis factor-alpha stimulates aromatase gene expression in human adipose stromal cells through use of an activating protein-1 binding site upstream of promoter 1.4. Mol Enocrinol 10:1350–1357
Zhao Y, Agarwal VR, Mendelson CR, Simpson ER (1997) Transcriptional regulation of CYP19 gene (aromatase) expression in adipose stromal cells in primary culture. J Steroid Biochem Mol Biol 61:203–210
Richards JA, Petrel TA, Brueggemeier RW (2002) Signaling pathways regulating aromatase and cyclooxygenases in normal and malignant breast cells. J Steroid Mol Biol 80:203–212
Karuppu D, Kalus A, Simpson ER, Clyne C (2002) Aromatase and prostaglandin inter-relationships in breast adipose tissue: significance for breast cancer development. Breast Cancer Res Treat 76:103–109
Acknowledgements
This study was supported by grants from the Swedish Cancer and Allergy Society, the Swedish Cancer Society, Gunnar Nilsson Cancer Foundation, the Regional Cancer Society of Östergötland Sweden, and the Foundation of Carl and Axel Molin Motala Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Licznerska, B.E., Wegman, P.P., Nordenskjöld, B. et al. In situ levels of oestrogen producing enzymes and its prognostic significance in postmenopausal breast cancer patients. Breast Cancer Res Treat 112, 15–23 (2008). https://doi.org/10.1007/s10549-007-9819-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-007-9819-x