Abstract
Objective
To describe demographic, genetic, and clinical characteristics of patients with neuronopathic Gaucher disease (NGD).
Methods
All patients enrolled in the Neurological Outcomes Subregistry of the International Collaborative Gaucher Group (ICGG) Gaucher Registry as of June 2007 were identified.
Results
The study cohort comprised 131 patients from 17 countries who were enrolled in the Neurological Outcomes Subregistry. The onset of neurological manifestations had occurred before 2 years of age in 47% (61 out of 131 patients), 2 years of age or older in 41% (54 out of 131), and could not be ascertained in the remaining 12% (16 out of 131). The most common manifestations were inability to look to the extreme up or down (45%, 55 out of 123), abnormally slow object tracking (43%, 53 out of 123), convergent squint (36%, 44 out of 121), and ataxia (15 to 20%, 18–27 out of 117). Seizures were reported in 19 out of 122 patients (16%), and myoclonic seizures were reported in 3 out of 121 patients (2%). The most common genotypes were L444P/L444P (76 out of 108, 70%), L444P/D409H (9 out of 108, 8%), D409H/D409H (8 out of 108, 7%), and L444P/rare allele (6 out of 108, 6%); full sequencing was not performed in all patients.
Conclusions
Neurological manifestations of GD often begin to appear before the age of 2 years. The most common neurological signs and manifestations are brainstem abnormalities and fine motor dysfunction. The most common genotype is L444P/L444P.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gaucher disease (GD) is an autosomal recessive lysosomal storage disease that results from a deficiency of acid β-glucosidase (EC 3.2.1.45; glucocerebrosidase), which leads to an accumulation of its substrate, glucocerebroside, in the reticuloendothelial system, particularly the spleen, liver, bone marrow, and lung. Common manifestations include anemia, thrombocytopenia, splenomegaly, hepatomegaly, and skeletal pathology (Charrow et al. 2000; Grabowski 2005; Grabowski et al. 2006).
In a small number of patients the brain may be affected; these patients are classified as having neuronopathic GD (NGD). Neuronopathic forms of GD are rare. It is estimated that approximately 6% of Gaucher patients have NGD; 5% have the chronic neuronopathic form, and 1% have the acute form of the disease (Charrow et al. 2000).
Patients with NGD frequently develop neurological manifestations in infancy or childhood. Acute (type 2) NGD usually presents in the first 6 months of life and frequently leads to death before 2 years of age. In chronic (type 3) NGD, patients typically live into their third decade of life. Typical neurological manifestations consist of oculomotor apraxia, supranuclear ophthalmoplegia, extrapyramidal features, myoclonic or generalized seizures, cerebellar ataxia, and developmental delay. Horizontal supranuclear gaze palsy is often one of the first neurological signs of NGD.
More than 260 mutations are known in the glucocerebrosidase gene (Grabowski et al. 2006). There is some genotype/phenotype correlation, so that the presence of the N370S allele does not absolutely preclude NGD, whereas homozygosity for the L444P mutation predicts a high likelihood of NGD. However, even within each genotype group, there is significant unexplained variability in the phenotypic spectrum (Grabowski et al. 2006).
The rarity of NGD has rendered large-scale, systematic study difficult. For this reason, most reports in the literature are of small numbers of patients from single ethnic or geographic locations. This study provides a worldwide perspective on NGD by taking advantage of the largest database available on patients with NGD, the Neurological Outcomes Subregistry of the International Collaborative Gaucher Group (ICGG) Gaucher Registry. We report the demographic, genetic and clinical characteristics of patients enrolled in the Neurological Outcomes Subregistry to gain an insight into the full phenotypic spectrum of NGD.
Methods
ICGG Gaucher Registry
The ICGG Gaucher Registry was established in 1991 to track the clinical, biochemical and therapeutic characteristics of patients with GD, irrespective of disease severity and treatment status (Charrow et al. 2000). The governance and the scientific direction of the Registry is overseen by an independent international group of physician experts in GD, with logistical support from Genzyme Corporation (Cambridge, MA, USA). To date, over 700 physicians from 60 countries have voluntarily submitted de-identified patient data with Institutional Review Board–Ethics Committee approvals.
Neurological Outcomes Subregistry
The Neurological Outcomes Subregistry of the ICGG Gaucher Registry was initiated in 2004 with the goal of capturing the full worldwide spectrum of NGD. It was designed to focus on the neurological manifestations of NGD, its natural history, and its response to treatment. All patients with a confirmed diagnosis of GD who have neurological manifestations as a result of the disease are eligible. The Neurological Outcomes Subregistry receives scientific direction from an independent international group of experts in NGD and logistical support from Genzyme Corporation. Data for the Neurological Outcomes Subregistry are collected on standard case report forms.
Study population
The dataset for this analysis included all GD patients who were also enrolled in the Neurological Outcomes Subregistry as of 1 June 2007. In every case the diagnosis of GD was based on assay of acid β-glucosidase activity or genotyping of the GBA1 gene that encodes lysosomal glucocerebrosidase. The diagnosis of NGD was made by each patient′s treating physician.
Demographic and clinical characteristics
The following baseline demographic characteristics were recorded for each patient in the study: gender, ethnicity (as indicated by the reporting physician), GBA1 genotype and country of origin. Full GBA1 gene sequencing was not performed in all patients. Clinical characteristics of GD at diagnosis included hemoglobin concentration, platelet count, spleen volume, liver volume, bone pain, bone crisis, and growth parameters. Criteria for diagnosis of bone crises in the Registry include acute onset of bone pain requiring immobilization of the affected area and narcotics for the relief of pain, accompanied by one or more of the following: periosteal elevation, elevated white blood cell count, elevated levels of inflammatory markers, fever or debilitation >3 days (Charrow et al. 2007). Organ volumes were expressed as multiples of the predicted normal for body weight (approximately 2.5% and 0.2% of body weight for liver and spleen, respectively) (Ludwig 1979). For each clinical criterion, the data point recorded closest to the diagnosis date within ±2 years was included in the analysis. Since all clinical features are not always reported at the time of each patient′s GD diagnosis, this time frame was used to account for any time delays in reporting these data.
Neurological characteristics
Neurological phenotype was ascertained by age of onset of neurological manifestations, age at first assessment in the Neurological Outcomes Subregistry, developmental delay and developmental age. All the data elements contained on the Neurological Outcomes Subregistry case report forms were used in this report. These included data on cranial nerve assessments (Table 3), motor assessments (Table 4), and numbers of seizures. The evaluation of the signs and symptoms of NGD was made by the treating physician.
Data analysis
Descriptive statistics were used to analyze data in this study, according to demographic and clinical characteristics of GD, and neurological characteristics. Proportions were calculated for categorical variables (i.e., gender, genotype, ethnicity, neurological characteristics). Summary statistics [mean, standard deviation (SD), percentiles] were calculated for continuous measures (i.e., age). All analyses were conducted in SAS 8.2 (SAS Institute Inc., Cary, NC, USA) in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (STROBE statement 2008) (http://www.strobe-statement.org).
Results
Study population
As of 1 June 2007, 4,760 patients with GD were enrolled in the ICGG Gaucher Registry. Of these, 131 were also enrolled in the Neurological Outcomes Subregistry.
Demographic characteristics
General
The demographic characteristics are shown in Table 1 (n = 131). The median age at GD diagnosis was 1 year. There were approximately equal numbers of male (47%) and female (53%) patients. The largest number of patients was reported from Egypt (31%), followed by the UK (14%) and Poland (13%). Most patients with available genotype data reported the genotype of L444P/L444P (76 out of 108 patients, 70%). Nine patients (8%) had L444P/D409H, eight patients (7%) had D409H/D409H, six (6%) had L444P/rare allele and nine (8%) reported other genotypes.
Characteristics of patients were also analyzed separately by country (supplementary material). No distinct pattern was observed; however, this also might have been due to the small number of patients in each country. Since no differences between countries were observed, all the data were combined.
Neurological
Neurological manifestations were first noted before the age of 2 years in 47% (n = 61) of patients and at 2 years of age or older in 41% of patients (n = 54); data were not available for 12% of patients (n = 16). Developmental delay (as assessed by the treating physician) was reported in 54 (43%) of the 125 patients for whom this information was recorded.
Neurological disease characteristics
Cranial nerves
Cranial nerve characteristics at first reported assessment are shown in Table 2.
The majority (71%) of patients had problems with horizontal gaze (ability to look to the extreme right or left), head movement rather than eye movement (63%), or head thrusting (55%). A high proportion of patients showed problems with abnormal vertical gaze (45%), abnormal slow object tracking (43%), and convergent squint (36%). Other abnormalities included dysarthria (22%), swallowing difficulties (20%), chewing difficulties (11%), and stridor (11%). Stridor was observed among younger patients (median age first noted was 1 year), and dysarthria was observed among older patients (median age first noted was 4 years).
Motor system
Motor characteristics at first reported assessment are displayed in Table 3.
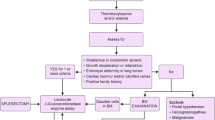
The most frequent motor abnormalities were muscle weakness (25%); extrapyramidal features (18%); spasticity (15%); intention tremor (24%); and tremor at rest (16%). Figure 1 indicates the percentage of patients with motor and cranial nerve symptoms and the median age at which each symptom appeared.
Seizures
Nineteen out of 122 patients (16%) had suffered from seizures when first assessed (Fig. 1). Some patients had experienced more than one type of seizure. The types reported were tonic–clonic seizures (7 out of 122, 6%), clonic seizures (5 out of 122, 4%), tonic seizures (3 out of 120, 3%), myoclonic seizures (3 out of 121, 2%), typical absence seizures (2 out of 119, 2%), and atypical absence seizures (1 out of 119, 1%).
Hematological and visceral disease at the time of diagnosis of Gaucher disease
Hematological, visceral and bone manifestations at the time of diagnosis are shown in Table 4.
Anemia was seen in 39 out of 65 (60%) patients, and moderate (60 to <120 × 1,000 platelets/mm3) or severe (<60 × 1,000 platelets/mm3) thrombocytopenia in 33 out of 63 (52%) of the non-splenectomized patients. Thirty-five out of 35 patients (100%) had splenomegaly, and 94% were >15 multiples of normal (33 out of 35 of patients). More than half (56%, 36 out of 64) of the pediatric patients suffered from growth retardation (defined as below the 5th percentile for height). Bone pain was reported in 6 out of 53 (11%) patients and a history of bone crisis in 1 out of 53 (2%) patients. Visceral disease characteristics were similar in all patients, regardless of the patients’ ages at the onset of neurological manifestations.
Discussion
We performed a cross-sectional analysis of the demographic, genetic and clinical characteristics of 131 patients enrolled in the Neurological Outcomes Subregistry of the ICGG Gaucher Registry, the largest known registry of its kind. This study is important, because in a rare ‘ultra-orphan’ disease, such as NGD, a full appreciation of the worldwide spectrum of the disease is only possible through a large longitudinal international disease registry. This study represents the largest cohort of patients with NGD in the Neurological Outcomes Subregistry (n = 131) presented in the literature to date. Previous reports (Dreborg et al. 1980; Erikson 1986) have focused on smaller numbers of patients (n = 22; Dreborg et al. 1980; Erikson 1986) from individual countries such as Japan (Ida et al. 1999), Poland (Tylki-Szymańska et al. 2006), or China (Choy et al. 2007). In our report the proportions of patients from Egypt (31%) and Sweden (11%) suggest that the prevalence of NGD might be higher in these countries; although, due to the voluntary nature of submitting data to the Registry, this might be a reporting artifact.
The most common GBA1 mutation in this cohort was L444P, accounting for 77% of all disease alleles; 70% of all patients were homozygous for this mutation. Interestingly, this mutation is normally present in the pseudogene sequence, and it is believed to have arisen by gene conversion events (Beutler and Grabowski 1995). The N370S mutation was detected in one patient with a genotype of N370S/L444P. Homozygosity for the L444P mutation in the Japanese patients resulted in severe disease and central nervous system involvement (Ida et al. 1999; Eto and Ida 1999). However, in our cohort, neurological involvement appeared to be less severe. The most commonly observed abnormalities related to the cranial nerves were inability to reach the limits of horizontal and vertical gaze, head thrusting, abnormally slow object tracking and convergent squint. Motor abnormalities included ataxia as well as muscle weakness, extrapyramidal features, spasticity, and tremor (at rest as well as when reaching). Seizures were reported by 16% of patients.
The defining manifestations of NGD often begin to appear before the age of 2 years; our data indicated a high prevalence of neurological symptoms in this age group (Fig. 1). Our data showed that, regardless of the age at the onset of neurological manifestations, both groups of children had severe visceral involvement when Gaucher disease was diagnosed, as evidenced by severe splenomegaly. This degree of visceral involvement is also commonly seen in children with non-neuronopathic Gaucher disease (Kaplan et al. 2006). In our data, bone pain and bone crisis (bone pain 81%; bone crisis 95%) are absent in most patients 2 years of age or older (Table 4). Since the neurological manifestations are complex, it is recommended that neurological signs and manifestations be monitored by clinicians experienced in performing neurological examinations, such as pediatric neurologists.
Unlike children with type 1 GD (Kaplan et al. 2006), the majority of patients in the Neurological Outcomes Subregistry do not present with bone pain and bone crisis (Table 4). The types of bone diseases commonly reported (Tylki-Szymańska and Czartoryska 1999) in patients with NGD are typically chest deformities and kyphoscoliosis. Kyphosis in NGD is thought to be highly prevalent and raises the possibility that it might have a neurological basis. At the present time, the Neurological Outcomes Subregistry does not systematically collect data on kyphosis; however, we hope to expand data collection in the future.
The Neurological Outcomes Subregistry represents the largest cohort of patients with neurological manifestations of Gaucher disease, enabling descriptive epidemiological analyses to be carried out for this rare disorder. However, we accept that it has limitations. Since participation is voluntary, physicians determine both the specific assessments that are carried out and the actual frequency of these assessments according to the individual patient’s needs. Therefore, the amount and frequency of data collection may vary by site and by geographic region. Patients in the Neurological Outcomes Subregistry were classified as having NGD by their treating physician. The accuracy with which neurological signs are assessed and recorded depends on each physician′s experience. In addition, early signs of neurological involvement may be subtle and therefore missed. For these reasons, it is possible that the data could represent an underestimate of the true prevalence of each manifestation, and the age at onset of the neurological manifestations might truly be earlier than reported to the Subregistry. Standard training materials are provided by the Neurological Outcomes Subregistry to all participating physicians; however, this does not ensure uniformity of criteria for defining each manifestation. If possible, it is recommended that neurological signs and manifestations be monitored by trained observers who are experienced in performing neurological examinations. Alternatives include the use of a recently developed severity scoring tool to aid in the assessment and follow-up of patients with NGD (Davies et al. 2007) or the confining of detailed data collection and analyses to a few centers with the necessary experience.
Genotype data may be inaccurate, as full sequencing is not determined worldwide. The most common genotypes reported in the Neurological Outcomes Subregistry were L444P/L444P, L444P/D409H, D409H/D409H, and L444P/rare allele. Some Albanian and Greek patients with L444P and D409H alleles have a second mutation that makes this mutation more severe (Grabowski et al. 2006). In order to identify such mutations, as well as others not yet reported, it is hoped that, in the future, physicians will add complete DNA sequencing information to the Neurological Outcomes Subregistry database so that additional gene mutations may be identified.
Future analyses to characterize the natural history of NGD and to examine effects of enzyme therapy and progression of neurological manifestations over the course of the disease will depend on additional accumulation of follow-up data. The further collection of data from around the world will also enable us to confirm whether the phenotype expressed differs between Neurological Outcomes Subregistry patient populations in various countries (Ida et al. 1999; Eto and Ida 1999; Khalifa et al. 1999; El-Beshlawy et al. 2006; Grabowski et al. 2006; Tylki-Szymańska et al. 2006; Choy et al. 2007). We hypothesize that there will be phenotypic differences among geographic regions and among people of different ethnic groups, as suggested in the literature (Erikson 1986; Erikson et al. 1997; Ida et al. 1999; Khalifa et al. 1999; Tylki-Szymańska et al. 2006, although our current data may be limited to detect these differences.
In summary, Neurological Outcomes Subregistry patients commonly present with neurological symptoms such as brainstem abnormalities and fine motor dysfunction which appear before 2 years of age. These children often have the genotype L444P/L444P and severe visceral disease.
Abbreviations
- GD:
-
Gaucher disease
- ICGG:
-
International Collaborative Gaucher Group
- NGD:
-
neuronopathic Gaucher disease
References
Beutler E, Grabowski GA (1995) Gaucher disease. In: Scriver CH, Beaudet AL, Sly WS, Valle D (eds), The metabolic and molecular bases of inherited disease. McGraw Hill, New York
Charrow J, Andersson HC, Kaplan P, et al (2000) The Gaucher Registry: demographics and disease characteristics of 1698 patients with Gaucher disease. Arch Intern Med 160:2835–2843
Charrow J, Dulisse B, Grabowski GA, Weinreb NJ (2007) The effect of enzyme replacement therapy on bone crisis and bone pain in patients with type 1 Gaucher disease. Clin Genet 71:205–211
Choy FYM, Zhang W, Shi H-P et al (2007) Gaucher disease among Chinese patients: review on genotype/phenotype correlation from 29 patients and identification of novel and rare alleles. Blood Cells Mol Dis 38:287–293
Davies EH, Surtees R, DeVile C, Schoon I, Vellodi A (2007) A severity scoring tool to assess the neurological features of neuronopathic Gaucher disease. J Inherit Metab Dis 30:768–782
Dreborg S, Erikson A, Hagberg B (1980) Gaucher disease—Norrbottnian type. 1. General clinical description. Eur J Pediatr 133:107–118
El-Beshlawy A, Ragab L, Youssry I et al (2006) Enzyme replacement therapy and bony changes in Egyptian paediatric Gaucher disease patients. J Inherit Metab Dis 29:92–98
Erikson A (1986) Gaucher disease—Norrbottnian type (III). Neuropaediatric and neurobiological aspects of clinical patterns and treatment. Acta Paediatr Scand Suppl 326:1–42
Erikson A, Bembi B, Schiffmann R (1997) Neuronopathic forms of Gaucher′s disease. Baillieres Clin Haematol 10:711–723
Eto Y, Ida H (1999) Clinical and molecular characteristics of Japanese Gaucher disease. Neurochem Res 24:207–211
Grabowski GA (2005) Recent clinical progress in Gaucher disease. Curr Opin Pediatr 17:519–524
Grabowski G, Kolodny E, Weinreb N et al (2006) Gaucher disease: phenotypic and genetic variation. Chapter 146.1. The Online Metabolic & Molecular Bases of Inherited Disease. New York: McGraw-Hill Online: http://genetics.accessmedicine.com/serverjava/Arknoid/amed/mmbid/co_chapters/ch146.1/ch146.1_p01.html
Ida H, Rennert OM, Iwasawa I, Kobayashi M Eto Y (1999) Clinical and genetic studies of Japanese homozygotes for the Gaucher disease L444P mutation. Hum Genet 105:120–126
Kaplan P, Andersson HC, Kacena KA, Yee J (2006) The clinical and demographic characteristics of non-neuronopathic Gaucher disease in 887 children at diagnosis. Arch Pediatr Adolesc Med 160:604–609
Khalifa AS, Fateen E, Tantawy AAG et al (1999) Phenotype-genotype expression of Gaucher disease in Egyptian infants and children. Egyptian J Pediatr 16:631–653
Ludwig J (1979) Current methods of autopsy practice. Saunders, Philadelphia, PA
STROBE statement. Strengthening the reporting of observational studies in epidemiology. Available at: http://www.strobe-statement.org. Accessed 1 November 2008
Tylki-Szymańska A, Czartoryska B (1999) Enzyme replacement therapy in type III Gaucher disease. J Inherit Metab Dis 22:203–204
Tylki-Szymańska A, Keddache M, Grabowski GA (2006) Characterization of neuronopathic Gaucher disease among ethnic Poles. Genet Med 8:8–15
Acknowledgements
We would like to thank the patients with neuronopathic Gaucher disease and their physicians and health care personnel who submit data to the Neurological Outcomes Subregistry, the Gaucher Registry support team at Genzyme Corporation, Andrea Gwosdow, Ph.D., for assistance in preparing the manuscript, Robert Brown (Genzyme Corporation) for graphic design of the figure, Michael Yeh, M.D. (Genzyme Corporation), for critical review of the manuscript and Pramod Mistry, M.D., Ph.D., for providing GBA1 gene sequencing for the Egyptian type 3 patients.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Ed Wraith
Competing interests: J. Alexander Cole was employed by Genzyme Corporation when the work was conducted. A. Tylki-Szymańska receives speaking fees from Genzyme Corporation. A. Vellodi receives research grants and speaking fees from Genzyme Corporation. E. Kolodny receives a research grant from Genzyme Corporation. A. El-Beshlawy has no conflict of interest. The article was prepared by a professional medical writer (A. Gwosdow) who was supported by Genzyme Corporation.
Rights and permissions
About this article
Cite this article
Tylki-Szymańska, A., Vellodi, A., El-Beshlawy, A. et al. Neuronopathic Gaucher disease: demographic and clinical features of 131 patients enrolled in the International Collaborative Gaucher Group Neurological Outcomes Subregistry. J Inherit Metab Dis 33, 339–346 (2010). https://doi.org/10.1007/s10545-009-9009-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-009-9009-6