Abstract
The study of innovative biodegradable implant materials is one of the most interesting research topics at the forefront in the area of biomaterials. Biodegradable implant materials in the human body can be gradually dissolved, absorbed, consumed or excreted, so there is no need for the secondary surgery to remove implants after the surgery regions have healed. However, most of the biodegradable materials, usually polymers, do not have good mechanical properties to be reliable for bearing the load of the body. Magnesium and its alloys due to the excellent biodegradability and biocompatibility as well as the suitable mechanical compatibility with human bone are very promising candidates for the development of temporary, degradable implants in load-bearing applications. However, Mg alloys are corrosion susceptible in a biological environment. Besides, the high corrosion rate and the low bioactivity of magnesium implants are the challenging problems, which need to be resolved before employing them in clinical applications. This paper provides a review of state-of-the-art of magnesium alloy implants for orthopedic and tissue engineering applications and describes recent progress in the design of novel structure design Mg alloys and potential approaches to improve their biodegradation performance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
To allow healing, broken bones must be firmly stabilized to avoid even micro-movements under the influence of considerable forces. Since inflammation may irritate bone repair, the implant must be highly biocompatible. Metallic implants are preferred for load-bearing applications because of their superior mechanical strength and fracture toughness. Currently approved and commonly used metallic biomaterials include stainless steels, titanium and cobalt-chromium-based alloys. They have good corrosion resistance to maintain long-term structural stability in the body. However, if these implants stay in the body for a long time, they may cause permanent physical irritation, a chronic inflammatory response, or they may release toxic elements. All of these interactions impair health (Jacobs et al. 1998; Lhotka et al. 2003; Jacobs et al. 2003). Moreover, the materials exhibit distinctly different mechanical properties as compared to the biological tissues they replace. Specifically, the elastic modulus difference between the traditional implants and the natural bone induces stress shielding of the bone, interfering with bone turnover, leading to bone loss and possibly inducing secondary bone fracture (Bostman et al. 2000; Nagels et al. 2003). Furthermore, the materials listed above are non-degradable. For short-term applications, such as bone fracture fixation or scaffolds that need to support bones during regeneration, the implant has to be removed by secondary surgery after recovery of the tissue function. This second surgery increases pain for the patients, surgery risk and medical costs. Thus, the development of biodegradable implants for treatment of complex bone fractures has become one of the priority areas in biomedical materials research. These implants should degrade at a rate adapted to tissue healing, ideally decreasing their strength and stiffness in a way matching the increase in load bearing capacity of the supported tissue, and maintaining some mechanical integrity until the tissue has healed completely.
Magnesium as degradable implants
Current biodegradable implants are mainly made of resorbable polymers and bioceramics. However, poor mechanical strength of the polymers and brittleness of the ceramics often limit their application as load-bearing devices (Hou et al. 2014). Here, degradable metal implants, made from magnesium (Mg) or iron (Fe) and their alloys, have a great potential as materials for temporary implants. However, biodegradable metals with better mechanical properties, good biocompatibility, no biotoxicity, and suitable degradation properties matching the tissue healing are still lacking and need to be developed.
Recently, Mg and its alloys have been presented as a new class of biodegradable metallic materials and gained more and more attention as a potential matrix material for orthopedic applications (Razavi et al. 2010a; Sharma et al. 2012; Witte 2010; Staiger et al. 2006). For a variety of reasons, they have attracted special interest for temporary implant applications such as bone plates and screws in orthopedics and as stents in cardiovascular implantology:
-
(i)
Most importantly, Mg and its alloys have a natural ability to biodegrade due to their corrosion susceptibility in aqueous solutions, especially if these contain chloride ions (Witte et al. 2006; Kraus et al. 2012). As compared to Fe and its alloys, Mg alloy implants degrade faster in physiological environments.
-
(ii)
Mg exhibits excellent biocompatibility (Li et al. 2004; Maguire and Cowan 2002): Mg ions (Mg2+) that are released during implantation and degradation are used in the regular metabolism and, to date, no critical toxic limits or side effects have been reported for Mg2+ ions.
-
(iii)
The elastic modulus of Mg (40–45 GPa) better matches the stiffness of natural bone (3–20 GPa) as compared to conventional metallic materials such as stainless steel (~ 200 GPa), cobalt-based alloys (~ 230 GPa), and titanium alloys (~ 115 GPa), thus reducing the stress shielding effect (Niinomi et al. 2012; Davies 2003).
-
(iv)
Mg alloys are exceptionally light weight metals with density ranging from 1.74 to 2.0 g/cm3, which is much less than that of, e.g. biomedical titanium alloys (4.4–4.5 g/cm3) and close to that of natural bone (1.8–2.1 g/cm3) (Gu et al. 2010a), thereby leading to lighter implants as compared to other metallic biomaterials.
Magnesium biodegradation in body environments
Mg corrosion in aqueous solution is an electrochemical phenomenon. The electrochemical degradation mechanism of Mg in aqueous solution occurs according to (Mueller et al. 2010; Chen et al. 2015):
producing magnesium hydroxide (Mg(OH)2) and hydrogen gas. The soluble magnesium hydroxide film forms a slightly effective protective layer on the surface of Mg which prevents further corrosion in water. However, if the corrosive medium contains any chlorides with concentrations above 30 mmol/L (Sha 2003); magnesium hydroxide is converted to magnesium chloride (MgCl2) (Staiger et al. 2006):
In the physiological environment, high chloride concentrations in the range of ~ 150 mmol/L are present, resulting in the production of highly soluble magnesium chloride which does not provide an effective protection from further corrosion. Therefore, corrosion progresses as the bare Mg surface is exposed to the aggressive environment again and again (Witte et al. 2006, 2008). The release of hydroxide ions from magnesium hydroxide upon the reaction with chlorine ions results in a local increase in pH value near the host tissue (Gu et al. 2010b; Wong et al. 2010).
Besides chlorine ions, the body fluid contains calcium and phosphate ions which triggers the production of MgxCay(PO4)z(OH)n compounds, such as calcium phosphate and/or calcium magnesium phosphate, by the interaction between Mg2+, Ca2+ and PO43−. These complex bioactive mineral products form a deposition layer on the Mg surface and inhibit further corrosion and increase in pH value (Jang et al. 2013). Furthermore, in addition to the variety of inorganic components, body fluids contain organic components, such as biomolecules, proteins, cells, or even bacteria, which may adsorb or adhere to the Mg surface and thereby affect the dissolution behavior. The presence of proteins and other organic molecules in blood which create a protective coating around Mg implants slowing down corrosion (Wagener et al. 2015; Yamamoto and Hiromoto 2009). However, the influence of proteins on Mg dissolution rate can change with time such that they may first inhibit and later accelerate degradation. The nature of the degradation products strongly influences the subsequent degradation steps on the Mg surface as well as the biological response of the bone tissue. The formation of corrosion products that serve as protective layers may explain to some extent the lower degradation rates observed in vivo as compared to in vitro tests, and reveal the importance of both proteins and different cell interactions with/nearby the implant on the degradation behavior (Willumeit-Römer et al. 2014). However, all these interactions may disturb the local physiological equilibrium at the implantation site.
As outlined above, there is a variety of interactions with the corroding Mg alloy surface and between the processes taking place at the implantation site, making the corrosion scenario in body environments highly complex as compared to that in a simple salt solution. Moreover, the degradation predictions become difficult as not only does the implant environment vary with the region of implantation from one patient to another and due to individual differences in reaction, but it can also vary with time (Tang et al. 2006). Indeed, time-dependent corrosion studies showed that the degradation process starts with a very high degradation rate and slows down with increasing immersion time. This is related to the nature of the corrosion layer formed on the Mg surface (Witte et al. 2005; Wang and Shi 2011).
In addition to the complex degradation processes, Mg implants experience considerable mechanical loading while exposed to the body fluid due to walking, running and other body movements. For example, a spine can experience maximum loads beyond 3500 N, whereas a cardiovascular stent needs to sustain very high numbers of cyclic loading due to the heart beats (Raman and Choudhary 2013; Choudhary and Raman 2012). The dynamic loading during normal physical activities, along with the corrosive physiological environment does pose the threat of corrosion fatigue (CF, under cyclic loading) and stress corrosion cracking (SCC, under tensile loading), due to the dual effect of corrosion and (tensile) stresses which lead to crack formation and possible fracture of implants. CF and SCC are a serious concern for implants made of Mg alloys, for several reasons: (i) common temporary implants (such as screws, pins and plates) have sharp contours acting as stress raisers; (ii) Mg alloys readily suffer of pitting corrosion in chloride solutions, including body fluids, and pits are the most common crack initiation sites of CF and SCC (Kannan and Raman 2008; Kannan et al. 2011); (iii) hydrogen released from Mg corroding in body fluids plays a dominant role in corrosion-assisted cracking, i.e., in SCC and CF, because crack initiation and propagation are accompanied and supported by hydrogen adsorption and diffusion into the material (Jafari et al. 2015; Gu et al. 2010c).
Challenges of magnesium biodegradable implants
The excellent biodegradability and biocompatibility as well as the suitable mechanical compatibility with human bone make Mg and its alloys very promising candidates for the development of temporary, degradable implants in load-bearing applications (Radha and Sreekanth 2017; Živić et al. 2014). However, there are a number of issues currently impeding the development. The main obstacle to the clinical use of Mg alloys is their too high corrosion rate in the complex physiological environment, containing water, dissolved oxygen, proteins, minerals, chloride and hydrogen ions, besides others (Li et al. 2008; Lopez et al. 2010). This fast corrosion under physiological conditions (that is, at pH values of 7.4–7.6 and high chloride concentration) is due to the rapid conversion of Mg hydroxide into highly soluble Mg chloride (Song and Atrens 1999). This leads to several problems:
-
(i)
The mechanical integrity of the Mg alloy implant deteriorates too fast, and, hence, the implant reaches inadequate mechanical properties before the host tissue has been sufficiently healed. The combination of the chloride containing environment and the Mg ions from anodic dissolution species further accelerates pitting corrosion, inducing localized high stresses which then may lead to the formation of cracks (González 2013; Choudhary and Raman 2013).
-
(ii)
The rapid corrosion of Mg is associated with the release of hydrogen (H2) gas (Liu and Schlesinger 2009). In the human body, the evolved hydrogen bubbles can accumulate in gas pockets in the vicinity of the implant. This may delay healing and may lead to necrosis of the tissues, because the gas pockets can cause separation of tissues and tissue layers (Seal et al. 2009; Witte et al. 2005).
-
(iii)
The severe Mg dissolution induces an alkalization (pH increase) near the Mg implant surface (Ng et al. 2010; Song and Song 2007). Although the human body automatically strives to adjust the pH value of the body fluid and the blood, local alkalization will be inevitable around a rapidly corroding Mg implant. This can unfavorably affect the pH dependent physiological reaction balances in the vicinity of the implant and may even lead to an alkaline poisoning effect if the regional in vivo pH value exceeds 7.8.
To resolve these drawbacks and develop clinically viable, degradable implant solutions, it is critical to slow down and control the biodegradation of Mg alloys. Thus, biocompatible Mg-based implants are needed that maintain their mechanical integrity longer, for the whole reparative phase of 4–16 weeks, depending on fracture configuration and location, status of the adjacent soft tissues, and patient characteristics (species, age, health status, concurrent injuries/diseases) (Frost 1989), to ensure sufficient healing of the fractured bone. Afterwards the implants should degrade entirely within a short period of time.
Novel structure design for Mg-based biodegradable metals
Based on research of literatures, many kinds of Mg-based metals with novel structure have been specially developed for the biomedical applications. Advances have been made on the design of porous structure, phase structure, grains, and amorphous structure to adjust the implant performance.
Porous structure
Porous implants, so-called scaffolds, with an interconnected pore structure are of particular interest for orthopedic implants as they allow tissue ingrowth, thereby improving implant fixation (Li et al. 2002; Wang et al. 2016, 2017; Jasmawati et al. 2015; Zardiackas et al. 2001; Clemow et al. 1981; Zou et al. 2004). The interconnected pore networks also support ingrowth and survival of the vascular system required for continuing bone development (Murray and Semple 1981; Li et al. 2005), as they facilitate the delivery of oxygen and nutrients to the cells and the removal of waste products stemming from cell metabolism and from degradation of the scaffold (Pamula et al. 2008, 2009). In addition, by adjusting the porosity, the modulus of materials can be controlled which offers the opportunity to design materials with a modulus close to that of natural bone (Lefebvre et al. 2008). These unique features make porous Mg with-bone mimicking characteristics an ideal scaffold for bone tissue regeneration. Mg scaffolds with an adjusted degree of porosity can provide appropriate mechanical support, can serve as templates for bone regeneration, and they offer excellent biocompatibility and biodegradability. Therefore, porous Mg scaffolds cannot only provide sufficient initial mechanical stability but they can also foster good bone ingrowth, which is necessary for biological fixation (Zhuang et al. 2008; Zreiqat et al. 2002; Persaud-Sharma and McGoron 2012). However, the already high corrosion rate may be increased by porosity, due to the increase in surface area accessible to the body fluids, together with a better transport of body fluids, both of which accelerate the rate of the bio-chemical reactions (Zreiqat et al. 2002).
Fine grained structure
A fine grain structure with increased grain boundary area reduces the structural discontinuity between the oxide layer and Mg and compensates the mismatch, thus decreases the degree of oxide cracking (Birbilis et al. 2010; Orlov et al. 2011; Ralston and Birbilis 2010). It might therefore be expected that a fine grain structure is more corrosion resistant in Mg alloys. A significant number of research showed that grain refinement after alloying and further treatment such as rolling and extrusion could affect the morphology and distribution of the primary or secondary phase, and the second phase could influence the anodic and cathodic polarization behaviors in electrochemical test (Witte 2010; Rosalbino et al. 2013; Pu et al. 2011). Subsequently, the yield strength (YS), ultimate tensile strength (UTS), elongation and corrosion properties of materials could be affected grain refinement.
Composite structure
The development of composite structure may represent an alternative method to achieve the desired improvements of Mg-based biomaterials. Mg matrix composites exhibit adjustable mechanical and corrosion properties as determined by the selection of the reinforcement material. The content, distribution, and size of the reinforcements are of major importance for mechanical and degradation properties of Mg composites. High flexibility in component design and reinforcement material in composites also can rectify the biocompatibility of Mg (Daoud et al. 2007; Mabuchi et al. 1995; Feng and Han 2011). In consideration of biocompatibility, reinforcements in Mg composites are usually HA (Gu et al. 2010d; Khanra et al. 2010; Witte et al. 2007), FA (Razavi et al. 2010b), calcium polyphosphate (Feng and Han 2010) and calcium (Razavi et al. 2010b).
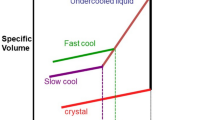
Glassy structure
Investigations were also carried out recently for Mg-based metallic glasses due to their single-phase, chemically homogeneous alloy system and the absence of second-phase, which could impair the mechanical properties and corrosion resistance. However, one of the unsolved problems for the manufacturability and the applications of bulk metallic glasses is that their glass-forming ability is very sensitive to the preparation techniques and impurity of components since oxygen in the environment would markedly deteriorate the glass-forming ability. Moreover, intrinsic brittleness and/or embrittlement due to structural relaxation are a primary negative concern for the future clinical application of Mg-based metallic glasses.
Approaches to improve magnesium biodegradation
Efforts to control the corrosion rate of Mg have comprised various strategies such as purification, alloying, and surface modification. Purification of Mg reduces the corrosion rate considerably; however, due to the low yield strength of pure Mg, its application in orthopedics and other load bearing applications is limited (Song 2007). In contrast, certain alloying elements can be added to improve the corrosion resistance of pure Mg. Using suitable alloying elements mechanical strength and corrosion resistance of Mg-alloys can be enhanced but cytotoxicity and long term inflammatory consequences of these elements are the major concern. Hence, alloying elements need to be selected carefully to maintain biocompatibility, because they will also be dissolved in the body fluid during degradation (Zhang et al. 2013). Furthermore, most Mg alloys are susceptible to localized degradation due to their inhomogeneous microstructure which may impair the mechanical integrity during service (Kannan 2010). In addition, the high electronegative potential of Mg (− 2.4 V) makes it difficult to achieve a significantly lower degradation rate just by alloying.
Surface modification is one of the most effective ways not only to reduce and control the degradation behavior but also to improve the surface biocompatibility of Mg. Compared to changing the bulk structure and composition, surface modification is simpler and more conveniently implemented on Mg alloys to tailor the surface corrosion resistance while preserving the favorable bulk attributes. Surface modification has recently been shown to provide excellent improvements in the corrosion performance of Mg alloy implants, through a treatment process that provides a resistive barrier against the body environment (Wan et al. 2016; Liu et al. 2014; Razavi et al. 2013; Jai Poinern et al. 2012). In comparison with alloy design, it is less costly, flexible to construct multi-functional surfaces and the addition of potentially toxic alloying elements is eliminated. In the case of biodegradable Mg-based implants, the aim of the surface modification is just to control their degradation rate and to improve their surface biocompatibility, but not to permanently change the surface properties, which might involve loss of degradability or toxicity to surrounding tissues. Hence, a biodegradable dynamic interface is the goal, in order to endow the implants with desirable corrosion resistance and surface biocompatibility as well as maintain the mechanical strength of the substrate during service (Wu et al. 2013). Various surface modification strategies have been proposed such as conversion coatings (Mao et al. 2013; Zomorodian et al. 2012), sol–gel coatings (Rojaee et al. 2013), chemical deposition (Hiromoto et al. 2013; Wang et al. 2010), plasma electrolytic oxidation (PEO) (Lin et al. 2013, 2014; Pan et al. 2013), hydroxyapatite coatings (Tomozawa and Hiromoto 2011; Wang et al. 2011) and organic coatings (Zomorodian et al. 2013). The details of various surface modification methods and their importance for biomedical applications of Mg alloys are addressed in recent reviews (Yang et al. 2011; Hornberger et al. 2012; Wang et al. 2012).
Conclusion
Mg is a promising biomaterial for bone substitution due to its excellent set of properties, comprising a relatively low Young’s modulus comparable with that of natural bone, sufficient strength, excellent biocompatibility and biodegradability. These unique features make Mg with-bone mimicking characteristics an ideal scaffold for bone tissue regeneration. However, the use of Mg under physiological conditions remains problematic. Therefore, a strategically designed Mg scaffold that retains its mechanical strength over a sufficient time span and corrodes at a controlled rate is necessary.
References
Birbilis N, Ralston KD, Virtanen S, Fraser HL, Davies CHJ (2010) Grain character influences on corrosion of ECAPed pure magnesium. Corros Eng, Sci Technol 45(3):224–230
Bostman O, Viljanen J, Salminen S, Pihlajamaki H (2000) Response of articular cartilage and subchondral bone to internal fixation devices made of poly-L-lactide: a histomorphometric and microradiographic study on rabbits. Biomaterials 21:2553–2560
Chen K, Dai J, Zhang X (2015) Improvement of corrosion resistance of magnesium alloys for biomedical applications. Corros Rev 33:101–117
Choudhary L, Raman RK (2012) Magnesium alloys as body implants: fracture mechanism under dynamic and static loadings in a physiological environment. Acta Biomater 8:916–923
Choudhary L, Raman RKS (2013) Microstructure mechanical property and in vitro biocorrosion behavior of single-phase biodegradable Mg-1.5 Zn-0.6 Zr alloy. Eng Fract Mech 103:94–102
Clemow JT, Weinstein AM, Klawitter JJ, Koeneman J, Anderson J (1981) Interface mechanics of porous titanium implants. J Biomed Mater Res 15:73–82
Daoud A, El-khair MTA, Abdel-Aziz M, Rohatgi P (2007) Fabrication, microstructure and compressive behavior of ZC63 Mg–microballoon foam composites. Compos Sci Technol 67:1842–1853
Davies JR (2003) Metallic materials in handbook of materials for medical devices. ASM International, Materials Park, pp 21–50
Feng A, Han Y (2010) The microstructure, mechanical and corrosion properties of calcium polyphosphate reinforced ZK60A magnesium alloy composites. J Alloys Compds 504:585–593
Feng A, Han Y (2011) Mechanical and in vitro degradation behavior of ultrafine calcium polyphosphate reinforced magnesium-alloy composites. Mater Des 32:2813–2820
Frost HM (1989) The biology of fracture healing. An overview for clinicians. Part I. Clin Orthop Relat Res 248:283–293
González S et al. (2013) Biodegradation and mechanical integrity of magnesium and magnesium alloys suitable for implants, Chapter 12
Gu XN, Zheng YF (2010) A review on magnesium alloys as biodegradable materials. Front Mater Sci China 4:111–115
Gu XN, Zhou W, Zheng Y, Cheng Y, Wei S, Zhong S, Xi TF, Chen LJ (2010a) Corrosion fatigue behaviors of two biomedical Mg alloys—AZ91D and WE43—in simulated body fluid. Acta Biomater 6:4605–4613
Gu X, Zhou W, Zheng Y, Liu Y, Li Y (2010b) Degradation and cytotoxicity of lotus-type porous pure magnesium as potential tissue engineering scaffold material. Mater Lett 64:1871–1874
Gu XN, Zhou WR, Zheng YF, Dong LM, Xi YL, Chai DL (2010c) Microstructure, mechanical property, bio-corrosion and cytotoxicity evaluations of Mg/HA composites. Mater Sci Eng, C 30:827–832
Hiromoto S, Tomozawa M, Maruyama N (2013) Fatigue property of a bioabsorbabale magnesium alloy with a hydroxyapatite coating formed by a chemical solution deposition. J Mech Behav Biomed Mater 25:1–10
Hornberger H, Virtanen S, Boccaccini AR (2012) Biomedical coatings on magnesium alloys—a review. Acta Biomater 8:2442–2455
Hou LD, Li Z, Pan Y, Du L, Li XL, Zheng YF, Li L (2014) In vitro and in vivo studies on biodegradable magnesium alloy. Prog Nat Sci 24:466–471
Jacobs JJ, Gilbert JL, Urban RM (1998) Corrosion of metal orthopaedic implants. J Bone Joint Surg 80:268–282
Jacobs JJ, Hallab NJ, Skipor AK, Urban RM (2003) Metal degradation products: a cause for concern in metal-metal bearings? Clin Orthop Relat Res 417:139–147
Jafari S, Singh Raman RK, Davies CHJ (2015) Corrosion fatigue of a magnesium alloy in modified simulated body fluid. Eng Fract Mech 137:2–11
Jai Poinern GE, Brundavanam S, Fawcett D (2012) Biomedical magnesium alloys: a review of material properties, surface modifications and potential as a biodegradable orthopaedic implant. Am J Biomed Eng 2(6):218–240
Jang Y, Collins B, Sankar J, Yun Y (2013) Effect of biologically relevant ions on the corrosion products formed on alloy AZ31B: an improved understanding of magnesium corrosion. Acta Biomaterial 9:8761–8770
Jasmawati N, Djuansjah JRP, Kadir MRA, Sukmana I (2015) Porous magnesium scaffolds for bone implant applications: a review. Adv Mater Res 1125:437–440
Kannan MB (2010) Influence of microstructure on the in vitro degradation behaviour of magnesium alloy. Mater Lett 64:739–742
Kannan MB, Raman RKS (2008) Stress corrosion cracking of magnesium alloys. Scripta Mater 59:175–178
Kannan M, Raman R, Witte F, Blawert C, Dietzel W (2011) Influence of circumferential notch and fatigue crack on the mechanical integrity of biodegradable magnesium-based alloy in simulated body fluid. J Biomed Mater Res, Part B 96:303–309
Khanra AK, Jung HC, Hong KS, Shin KS (2010) Comparative property study on extruded Mg-HAP and ZM61-HAP composites. Mater Sci Eng, A 527:6283–6288
Kraus T, Fischerauer S, Hänzi A, Uggowitzer P, Löffler J, Weinberg AM (2012) Magnesium alloys for temporary implants in osteosynthesis: in vivo studies of their degradation and interaction with bone. Acta Biomateriala 8:1230–1238
Lefebvre LP, Banhart J, Dunand D (2008) Porous metals and metallic foams: current status and recent developments. Adv Eng Mater 10:775–787
Lhotka C, Szekeres T, Steffan I, Zhuber K, Zweymuller K (2003) Four-year study of cobalt and chromium blood levels in patients managed with two different metal-on-metal total hip replacements. J Orthop Res 21:189–195
Li JP, Li SH, de Groot K, Layrolle P (2002) Macroporous biphasic calcium phosphate scaffold with high permeability/porosity ratio. Key Eng Mater 218:51–54
Li LC, Gao JC, Wang Y (2004) Evaluation of cyto-toxicity and corrosion behavior of alkali-heat-treated magnesium in simulated body fluid. Surf Coat Technol 185:92–98
Li JP, Li SH, van Blitterswijk CA, Groot K (2005) A novel porous Ti6A14 V: characterization and cell attachment. J Biomed Mater Res 73A:223–233
Li Z, Gu X, Lou S, Zheng Y (2008) The development of binary Mg-Ca alloys for use as biodegradable materials within bone. Biomaterials 29:1329–1344
Lin X, Tan L, Wang Q, Zhang G, Zhang B, Yang K (2013) In vivo degradation and tissue compatibility of ZK60 magnesium alloy with micro-arc oxidation coating in a transcortical model. Mater Sci Eng C33:3881–3888
Lin X, Yang X, Tan L, Li M, Wang X, Zhang Y, Yang K, Hu Z, Qiu J (2014) In vitro degradationand biocompatibility of a strontium-containing micro-arc oxidation coating on the biodegradable ZK60 magnesium alloy. Appl Surf Sci 288:718–726
Liu LJ, Schlesinger M (2009) Corrosion of magnesium and its alloys. Corros Sci 51:1733–1737
Liu C, Zhao Y, Chen Y, Liu P, Cai K (2014) Surface modification of magnesium alloy via cathodic plasma electrolysis and its influence on corrosion resistance and cytocompatibility. Mater Lett 132:15–18
Lopez M, Pereda M, Valle J, Lorenzo M, Alonso M, Escudero M (2010) Corrosion behavior of AZ31 magnesium alloy with different grain sizes in simulated biological fluids. Acta Biomater 6:1763–1771
Mabuchi M, Kubota K, Higashi K (1995) High strength and high strain rate super plasticity in a Mg-Mg2Si composite. Scr Metall Mater 33:331–335
Maguire M, Cowan J (2002) Magnesium chemistry and biochemistry. Biometals 15:203–210
Mao L, Yuana G, Niu J, Zong Y, Ding W (2013) In vitro degradation behavior and biocompatibility of Mg–Nd–Zn–Zr alloy byhydrofluoric acid treatment. Mater Sci Eng C33:242–250
Mueller WD, Nascimento ML, de Mele MFL (2010) Critical discussion of the results from different corrosion studies of Mg and Mg alloys for biomaterial applications. Acta Biomater 6:1749–1755
Murray GA, Semple JC (1981) Transfer of tensile loads from a prosthesis to bone using porous titanium. J Bone Joint Surg 63B:138–141
Nagels J, Stokdijk M, Rozing PM (2003) Stress shielding and bone resorption in shoulder arthroplasty. J Shoulder Elbow Surg 12:35–39
Ng WF, Chiu KY, Cheng FT (2010) Effect of ph on the in vitro corrosion rate of magnesium degradable implant material. Mater Sci Eng, C 30:898–903
Niinomi M, Nakai M, Hieda J (2012) Developement of new metallic alloys for biomedical applications. Acta Biomater 8:3888–3903
Orlov D, Ralston KD, Birbilis N, Estrin Y (2011) Enhanced corrosion resistance of Mg alloy ZK60 after processing by integrated extrusion and equal channel angular pressing. Acta Mater 59(15):6176–6186
Pamula E, Bacakova L et al (2008) The influence of pore size on colonization of poly(L-lactide-glycolide) scaffolds with human osteoblast-like MG 63 cells in vitro. J Mater Sci 19:425–435
Pamula E, Filová E, Bacáková L, Lisá V, Adamczyk D (2009) Resorbable polymeric scaffolds for bone tissue engineering: the influence of their microstructure on the growth of human osteoblast-like MG 63 cells. J Biomed Mater Res A89:432–443
Pan YK, Chen CZ, Wang DG, Zhao TG (2013) Effects of phosphates on microstructure and bioactivity of micro-arc oxidized calcium phosphate coating on Mg-Zn-Zr magnesium alloy. Colloids Surf B 109:1–9
Persaud-Sharma D, McGoron A (2012) Biodegradable magnesium alloys: a review of material development and applications. J Biomater Tissue Eng 12:25–39
Pu Z, Outeiro JC, Batista AC et al (2011) Surface integrity in dry and cryogenic machining of AZ31b Mg alloy with varying cutting edge radius tools. Procedia Eng 19:282–287
Radha R, Sreekanth D (2017) Insight of magnesium alloys and composites for orthopedic implant applications—a review. J Magnes Alloys 5:286–312
Ralston KD, Birbilis N (2010) Effect of grain size on corrosion: a review. Corros Sci 66(7):075005
Raman RKS, Choudhary L (2013) Cracking of magnesium-based biodegradable implant alloys under the combined action of stress and corrosive body fluid: a review. Emerg Mater Res 2:219–228
Razavi M, Fathi MH, Meratian M (2010a) Fabrication and characterization of magnesium-fluorapatite nanocomposite for biomedical applications. Mater Charact 61:1363–1370
Razavi M, Fathi MH, Meratian M (2010b) Microstructure, mechanical properties and bio-corrosion evaluation of biodegradable AZ91-FA nanocomposites for biomedical applications. Mater Sci Eng, A 527:6938–6944
Razavi M, Fathi M, Savabi O, Razavi S, Hashemi B, Vashaee D, Tayebi L (2013) Surface modification of magnesium alloy implants by nanostructured bredigite coating. Mater Lett 113:174–178
Rojaee R, Fathi M, Raeissi K (2013) Controlling the degradation rate of AZ91 magnesium alloy via sol-gel thin films as derived nanostructured hydroxyapatite coating. Mater Sci Eng C33:3817–3825
Rosalbino F, De Negri S, Scavino G et al (2013) Microstructure and in vitro degradation performance of Mg-Zn-Mn alloys for biomedical application. J Biomed Mater Res A101:704–711
Seal CK, Vince K, Hodgson MA (2009) Biodegradable surgical implants based on magnesium alloys—a review of current research. Mater Sci Eng 4:1–5
Sha BA (2003) Corrosion resistance of magnesium alloys. ASM Handbook 13A, OH, USA
Sharma DP, McGoron A, Biomim J (2012) Biodegradable magnesium alloys: a review of material development and applications. Biomater Tissue Eng 12:25–39
Song G (2007) Control of biodegradation of biocompatible magnesium alloys. Corros Sci 49(4):1696–1701
Song GL, Atrens A (1999) Corrosion mechanisms of magnesium alloys. Adv Eng Mater 1:11–33
Song G, Song S (2007) A possible biodegradable magnesium implant material. Adv Eng Mater 9:298–302
Staiger MP, Pietaka AM, Huadmai J, Diasb G (2006) Magnesium and its alloys as orthopedic biomaterials: a review. Biomaterials 27:1728–1734
Tang YC, Katsuma S, Fujimoto S, Hiromoto S (2006) Electrochemical study of Type 304 and 316L stainless steels in simulated body fluids and cell cultures. Acta Biomater 2:709–715
Tomozawa M, Hiromoto S (2011) Growth mechanism of hydroxyapatite coatings formed on pure magnesium and corrosion behavior of the coated magnesium. Appl Surf Sci 257(19):8253–8257
Wagener V, Faltz AS, Killian MS, Schmuki P, Virtanen S (2015) Protein interactions with corroding metal surfaces: comparison of Mg and Fe. Faraday Discuss 180:347–360
Wan P, Tan L, Yang K (2016) Biodegradable materials for bone repairs: a review. J Mater Sci Technol 32:827–834
Wang H, Shi Z (2011) In vitro biodegradation behavior of magnesium and magnesium alloy. J Biomed Mater Res, Part B 98:203–209
Wang HX, Guan SK, Wang X, Ren CX, Wang LG (2010) In vitro degradation and mechanical integrity of Mg-Zn-Ca alloy coated with Ca-deficient hydroxyapatite by the pulse electrodeposition process. Acta Biomater 6:1743–1748
Wang H, Guan S, Wang Y, Liu H, Wang L, Ren C, Zhu S, Chen K (2011) In vivo degradation behavior of Ca-deficient hydroxyapatite coated Mg-Zn-Ca alloy for bone implant application. Colloids Surf B 88:254–259
Wang J, Tang J, Zhang P, Li Y, Wang J, Lai Y (2012) Acceleration effect of basic fibroblast growth factor on the regeneration of peripheral nerve through a 15-mm gap. J Biomed Mater Res B100:1691–1701
Wang X, Xu S, Zhou S, Xu W, Leary M, Choong P, Qian M, Brandt M, Xie Y (2016) Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: a review. Biomaterials 83:127–141
Wang G, Fu H, Zhao Y, Zhou K, Zhu S (2017) Aging microstructural characteristics of ZA-27 alloy and SiCdZA-27 composite. Trans Nonferrous Met Soc China 27:2007–2014
Willumeit-Römer R, Wendel HP, Mihailova B, Agha NA, Feyerabend F (2014) Magnesium degradation influenced by buffering salts in concentrations typical of in vitro and in vivo models. Eur Cells Mater 28:29
Witte F (2010) The history of biodegradable magnesium implants: a review. Acta Biomater 6:1680–1692
Witte F, Kaese V, Haferkamp H, Switzer E, Wirth C, Windhagen H (2005) In vivo corrosion of four magnesium alloys and the associated bone response. Biomaterials 26:3557–3563
Witte F, Fischer J, Nellesen J, Crostack H, Kaese V, Pisch A, Windhagen H (2006) In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials 27:1013–1018
Witte F, Feyerabend F, Maier P, Fischer J, Stormer M, Blawert C, Dietzel W, Hort N (2007) Biodegradable magnesium-hydroxyapatite metal matrix composites. Biomaterials 28:2163–2174
Witte F, Hort N, Vogt C, Kainer K, Willumeit R, Feyeraben F (2008) Degradable biomaterials based on magnesium corrosion. Curr Opin Solid State Mater Sci 12:63–72
Wong HM, Yeung KW, Lam KO, Tam V, Chu PK, Luk KD, Cheung K (2010) A biodegradable polymer-based coating to control the performance of magnesium alloy orthopaedic implants. Biomaterials 31:2084–2096
Wu G, Ibrahim JM, Chu PK (2013) Corrosion behavior of Nd ion implanted Mg-Gd-Zn-Zr alloy in simulated body fluid. Surf Coat Technol 233:2–12
Yamamoto A, Hiromoto S (2009) Effect of inorganic salts, amino acids and proteins on the degradation of pure magnesium in vitro. Mater Sci and Eng C 29:1559–1568
Yang J, Cui F, Lee IS (2011) Surface modifications of magnesium alloys for biomedical applications. Ann Biomed Eng 39:1857–1871
Zardiackas LD, Dillon LD, Mitchell DW, Nunnery LA, Poggie R (2001) Structure, metallurgy and mechanical properties of porous tantalum foam. J Biomed Mater Res 58:180–187
Zhang LN, Hou ZT, Ye X, Xu ZB, Bai XL, Shang P (2013) Aligned single-crystalline perovskite microwave arrays for high-performance flexible image sensors with long-term stability. Front Mater Sci 7(3):227–236
Zhuang H, Han Y, Feng A (2008) Preparation, mechanical properties and in vitro biodegradation of porous magnesium scaffolds. Mater Sci Eng C28:1462–1466
Živić F, Grujović N, Manivasagam G, Richard C, Landoulsi J, Petrović V (2014) The potential of magnesium alloys as bioabsorbable/biodegradable implants for biomedical applications. Tribol Ind 36:67–73
Zomorodian A, Brusciotti F et al (2012) Corrosion resistance of a composite polymeric coating applied on biodegradable AZ31 magnesium alloy. Surf Coat Technol 206:4368–4375
Zomorodian A, Garcia M, Fernandes J, Fernandes M, Montemor M (2013) Corrosion resistance of a composite polymeric coating applied on biodegradableAZ31 magnesium alloy. Acta Biomater 9:8660–8670
Zou X, Li H, Bünger M, Egund N, Lind M, Bünger C (2004) Bone ingrowth characteristics of porous tantalum and carbon fiber interbody devices: an experimental study in pigs. Spine J 4:99–105
Zreiqat H, Howlett C, Zannettion A, Evans P, Knabe C, Shakibaei M (2002) Mechanisms of magnesium-stimulated adhesion of osteoblastic cells to commonly used orthopaedic implants. Biomed Mater Res 62:175–184
Acknowledgements
The authors would like to thank Department of Materials Engineering, Institute of Technology Berlin for the extremely helpful guidance in carrying out the review paper and providing them with the appropriate data required.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kamrani, S., Fleck, C. Biodegradable magnesium alloys as temporary orthopaedic implants: a review. Biometals 32, 185–193 (2019). https://doi.org/10.1007/s10534-019-00170-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10534-019-00170-y