Abstract
Ovarian cancer is the leading cause of death from gynecological cancer. The anti-apoptotic protein Bcl-xL is frequently overexpressed in ovarian carcinoma which correlates with chemotherapy resistance. It has been demonstrated that Bcl-xL cooperates with another anti-apoptotic protein, Mcl-1, to protect ovarian cancer cells against apoptosis, and that their concomitant inhibition induces massive cell death. Here, we examined the interest of ABT-737, a potent BH3-mimetic molecule targeting Bcl-xL, both alone and in combination with Mcl-1 modulators, in ovarian cancer cell lines. As a single agent, ABT-737 was ineffective at promoting cell death in the four cell lines we tested in vitro. However, the specific inhibition of Mcl-1 by siRNA dramatically increased the sensitivity of chemoresistant cells to ABT-737. Platinum compounds also sensitize to ABT-737 by dose-dependently decreasing Mcl-1 expression or by increasing the expression of pro-apoptotic BH3-only proteins Noxa and, to a lower extent, Bim. Furthermore, we demonstrated that Noxa accumulation was involved in apoptosis occurring in response to the combination of ABT-737 and platinum compounds, since cells were protected from apoptosis by its silencing. Moreover, the combination was also highly cytotoxic ex vivo in sliced SKOV3 tumor nodes. However we observed in these slices a strong basal expression of Noxa and apoptotic cell death in response to ABT-737 alone. Therefore, we have revealed that the modulation of the Mcl-1/Noxa axis by platinum compounds results in a strong sensitization of chemoresistant ovarian carcinoma cells to ABT-737, which could constitute a promising therapeutic in these cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian carcinoma represents the leading cause of death from gynecologic cancer which is due to both late diagnosis and chemoresistance. Standard treatment includes debulking surgery and subsequent platinum-based chemotherapy. Despite good initial response rates, frequent recurrence and subsequent acquired chemoresistance are responsible for therapeutic failure, and lead to an overall survival rate of about 30 % [1].
Although the process of chemoresistance appears to be multifactorial, progression towards drug resistance can be achieved through the inactivation of apoptosis, generally considered as a hallmark of cancer [2]. Therefore, the knowledge of these drug resistance mechanisms allows the identification of ways to reactivate the apoptotic response [3].
The Bcl-2 protein family plays a major role in the control of chemotherapy-induced apoptosis through the control of the mitochondrial apoptotic pathway. These proteins share four homology domains with Bcl-2 (BH1-4). Anti-apoptotic proteins (Bcl-2, Bcl-xL…) contain the BH1 to BH4 domains, whereas pro-apoptotic proteins contain either the BH1 to BH3 domains (multi-domain members such as Bax and Bak) or the BH3 domain only (BH3-only group such as Bad, Bid, Noxa, Puma and Hrk). Under cellular stress, BH3-only proteins initiate apoptosis by either blocking the activity of anti-apoptotic members or directly activating pro-apoptotic members, which is mediated via interaction of the BH3 domain of one protein with the hydrophobic pocket of another [4].
Expression of Bcl-2 family members is frequently deregulated during carcinogenesis [4], which is often associated with resistance to anti-cancer treatment, especially in ovarian carcinoma [5]. In fact, Bcl-xL is frequently overexpressed in ovarian carcinoma in a chemoresistance-associated manner [5, 6] and we previously showed that its down-regulation in response to cisplatin was strictly associated with massive apoptotic cell death and absence of recurrence in vitro [7]. Moreover, Mcl-1 is also highly expressed and associated with poor prognosis in these cancers [8]. Although the down-regulation of either Bcl-xL or Mcl-1 remains ineffective the concomitant inhibition of these proteins with siRNA was sufficient to induce massive cell death, highlighting the pivotal role these anti-apoptotic proteins play in chemoresistant ovarian carcinoma and mesothelioma [9, 10]. A combination of tools that simultaneously inhibit these two targets is particularly efficient to induce apoptosis in ovarian cancer cells refractory to conventional chemotherapy.
In this context, BH3-mimetic molecules represent a promising therapeutic strategy for the treatment of resistant ovarian carcinoma. These molecules bind to the BH3-binding groove in anti-apoptotic proteins of the Bcl-2 family and promote cell death either as single agents [11, 12] or in combination with other drugs, such as doxorubicin or cisplatin, in various cancer cells [13].
ABT-737 is a small chemical molecule that mimics the direct binding of Bad to Bcl-2, Bcl-xL and Bcl-w, with a high-affinity (Ki < 1nM). However, it does not bind to other anti-apoptotic proteins, such as Mcl-1 and Bfl-1 [14]. ABT-737 has exhibited preclinical activity as a single agent in a wide variety of cancer cells, such as hematopoietic cell lines [15–17] and, to a lower extent, solid tumor cell lines [18–20]. However, it is unable to induce cell death as a single agent in other tumor models, such as prostate cancer [21]. This relative resistance has previously been linked to a persistence of Mcl-1 expression [22–24]. Therefore, the use of Mcl-1 targeting agents in combination with ABT-737 could constitute an interesting therapeutic strategy [9, 10, 25]. Similarly, we previously demonstrated that Mcl-1 knockdown was an essential determinant of the response to Bcl-xL inhibition by another BH3-mimetic molecule, HA14-1 [26].
Here, we report that strategies involving either the direct or indirect inactivation of Mcl-1, such as RNA interference or platinum compounds, result in a sensitization of SKOV3 and IGROV1-R10 chemoresistant ovarian cancer cells to ABT-737-induced apoptosis, both in vitro and ex vivo. Moreover, the imbalance of the Mcl-1/Noxa axis is involved in the strong apoptosis induced by a combination of ABT-737 with platinum compounds.
Materials and methods
Cell culture
IGROV1, OAW42, A2780 and SKOV3 cell lines were established from human ovarian adenocarcinomas. Resistant IGROV1-R10 cells were obtained by reiterating treatments with increasing concentrations of cisplatin [27]. These cell lines were grown as described previously [7]. Briefly, all the cell lines except OAW42, were grown in RPMI-1640 medium supplemented with 2 mM Glutamax™, 25 mM HEPES, 10 % fetal calf serum, and 33 mM sodium bicarbonate (Fisher Scientific Bioblock, Illkirch, France). OAW42 cells were grown in DMEM medium supplemented with 4,500 mg/l glucose, 2 mM Glutamax™, 1 mM sodium pyruvate, 10 % fetal calf serum, 33 mM sodium bicarbonate (Gibco BRL, Lyon, France), and 20 UI/l recombinant human insulin (Lilly, Suresnes, France). Cells were maintained in a 5 % CO2 humidified atmosphere at 37 °C.
Reagents
ABT-737 and its inactive enantiomer were provided by Abbott laboratories (Abbott Park, IL, USA) and cycloheximide (CHX) was purchased from Sigma–Aldrich. These compounds were commonly stored as stock solutions in DMSO at −20 °C. Cisplatin and carboplatin were provided by Merck (Lyon, France).
Platinum compounds exposure and ABT-737 treatment
Schedule for cisplatin treatment
Exponentially growing cells were exposed to 20 μg/ml cisplatin in serum-free medium for 2 h and then incubated in complete growth medium either supplemented with ABT-737 or not for 46 h.
Schedule for carboplatin treatment
Exponentially growing cells were exposed to 20 μg/ml carboplatin with ABT-737 or DMSO in complete medium for 48 h.
For each condition, cell viability was assessed by the trypan blue exclusion test.
Apoptosis assay
Morphological characterization of apoptotic cells by nuclear staining with DAPI
After treatment, both detached and adherent cells were pooled after trypsinization, applied to a polylysine-coated glass slide by cytocentrifugation and fixed with a solution of ethanol/chloroform/acetic acid (6:3:1). The preparations were then incubated for 15 min at room temperature with 1 μg/ml DAPI solution (Boehringer Mannheim-Roche, Mannheim, Germany), washed in distillated water, mounted under a coverslip in Mowiol (Calbiochem) and analyzed under a fluorescence microscope (BX51, Olympus, Rungis, France).
Cell cycle analysis by flow cytometry
Adherent and floating cells were pooled, washed with 1× PBS and fixed with ethanol. Before flow cytometry analysis, cells were centrifuged at 2,000 rpm for 5 min and incubated for 30 min at 37 °C in PBS to allow the release of low-molecular weight DNA (characteristic of apoptotic cells). Cell pellets were stained with propidium iodide (PI) using the DNA Prep Coulter Reagent Kit (Beckman-Coulter, Villepinte France). Samples were thereafter analyzed using a Gallios flow cytometer (Beckman Coulter) and cell cycle distribution was determined using Kaluza acquisition software (Beckman Coulter).
Western-immunoblotting
Cells were rinsed with ice-cold PBS and lyzed in a lysis buffer [50 mM Tris–HCl (pH 8.1), 150 mM NaCl, 1 % Nonidet P-40, 5 mM EDTA, 10 mM NaF, 4 mM phenylmethylsulfonyl fluoride, 2 mM aprotinin, 10 mM NaPPi, 1 mM Na3VO4 and a complete mixture of protease inhibitors (Roche Applied Science, Meylan, France)] and incubated on ice for 30 min. Lysates were collected. After centrifugation (13,200×g, 10 min, 4 °C), protein concentrations were determined using the Bradford assay (Bio-Rad, Hercules, CA). Equal amount of proteins (20 μg) were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis on a 4–12 % gradient polyacrylamide precast gel (Invitrogen, Cergy-Pontoise, France) and transferred to Immobilon polyvinylidene difluoride membranes (Millipore, Saint-Quentin-en-Yvelines, France). After blocking non-specific binding sites for 1 h at RT by 5 % (wt/vol) non-fat dry milk in tris-buffered saline with 0.5 % (vol/vol) Tween 20 (T-TBS), the membranes were incubated either overnight at 4 °C or 2 h at RT with the following primary antibodies: anti-Mcl-1 (1:750, S-19, Santa Cruz Biotechnology, Le Perray-en-Yvelines, France), anti-Noxa (1:250, Calbiochem, VWR, Fontenay-sous-Bois, France) and anti-actin (1/10,000, Millipore, Saint-Quentin-en-Yvelines, France). Bcl-xL (1:1,000, #2,764, 54H6 clone), PARP (1:1,000, #9,542), Bim (1:500, #2,819) and caspase-3 (1:500, #9,662) antibodies were purchased from Cell Signaling Technology (Ozyme, Sain-Quentin-en-Yvelines, France). Membranes were then washed with T-TBS and incubated with the appropriate horseradish peroxidase-conjugated anti-rabbit or anti-mouse secondary antibodies (1:5,000 or 1:2,000, respectively; GE Healthcare, Orsay, France). Revelation was carried out using ECL Prime Western Blot detection reagent (GE Healthcare, Orsay, France).
siRNA transfection
PAGE-purified siRNAs were synthesized and annealed by the Eurogentec Company (Liège, Belgium). Specific double-stranded 21 nt RNA oligonucleotides forming a 19 bp duplex core with 2 nt 3′ overhangs were used to silence Mcl-1 expression. siRNA guide sequences targeting indicated genes were as follows: Control (5′-acuugccguuuacgtuctt-3′, siControl), Mcl-1 (5′-uguuuagccacaaaggcac-3′, siMCL1), Noxa (5′-gcuauuuuaccaucuggua-3′, siNoxa) and Bim (5′-uaacagucguaagauaacc-3′, siBim).
siRNA duplexes were transfected using the INTERFERin™ transfection reagent according to the manufacturer’s instructions (Polyplus-Transfection, Strasbourg, France). Briefly, cells were seeded in 25 cm2 flasks the day before to reach 30–50 % confluency at the time of transfection. The transfection reagent and siRNAs were mixed and complex formation was allowed to proceed for 15 min at room temperature (RT) before adding to cells. The day after transfection, cells were changed to regular cell media. After the indicated time, cells were trypsinized and washed with ice-cold phosphate-buffered saline (PBS) before analysis.
Real-time cellular cytotoxicity assay (xCELLigence)
Compound-mediated cytotoxicity was monitored with the real-time cell analyzer multi-plate (RTCA MP) Instrument, using the xCELLigence system (Roche Applied Science, Mannheim, Germany). This system monitors cellular events in real time by measuring electrical impedance across interdigitated micro-electrodes integrated on the bottom of tissue culture E-plates view (Roche). The increase in the number and size of cells attached to the electrode sensors leads to increased impedance, from which the cell index (CI) values are derived and displayed in the plot. Therefore, this index reflects changes in cell viability as described by Ke et al. [28]. Briefly, 96-well E-plates view were seeded with 3 × 103 cells/well and placed onto the RTCA MP located inside a tissue culture incubator, where cells were left to grow for 24 h before treatment and impedance was continuously measured until the end of the treatment. Standard deviations of well replicates were analyzed with the RTCA Software.
RNA isolation and quantitative reverse transcripase-PCR (RT-PCR)
Total RNA were isolated from ovarian carcinoma cell lines using Trizol (Invitrogen). RNA quantity and quality were assessed using the NanoDrop™ 2000 spectrophotometer (Thermo Scientific, Palaiseau, France). The first strand cDNA was synthesized using Omniscript reverse transcriptase kit (Qiagen, Courtaboeuf, France) with random hexamers. cDNA (25 ng) were combined with 10 μmol/l of each forward and reverse primers, 50 μmol/l of the TaqMan® probe and 2× TaqMan® Fast Universal PCR Master Mix (Applied Biosystems) in a 20 μl final reaction volume. Corresponding custom inventoried (ID: Hs00172036_m1 for Mcl-1 and Hs99999905_m1 for GAPDH) TaqMan® Gene Expression Assays were used (Applied Biosystems). All PCR amplification reactions were carried out in triplicate and detection was done on an Applied ABI Prism 7500 Fast PCR system (Applied Biosystems). GAPDH was used as a housekeeping reference gene for normalization.
Ex vivo study
Six-week old nude mice were xenografted subcutaneously with 10.106 SKOV3 or IGROV1-R10 cells. After sufficient tumor development (diameter 5 mm), mice were autopsied under sterile conditions to obtain tumors for ex vivo experiments. Next, vibratome-sliced samples (400 μm) were immediately fixed with 3 % PFA, or frozen at −80 °C for immunoblotting (T0), or transferred into sterile pre-warmed complete RPMI 1640 culture medium supplemented with 1 % antibiotic and treated with either vehicle (DMSO) or ABT-737, with or without platinum compounds for 48 h. Then, slices were also fixed and frozen as described above. The histology samples were confirmed with microscopic assessment by a cytopathologist. Tumor tissue sections were subjected to immunohistochemistry for cleaved caspase 3 (#9661S Cell Signaling Technology, Ozyme, Sain-Quentin-en-Yvelines, France).
In order to measure caspase 3 and PARP cleavages as well as expression of Bcl-2 family proteins by western-blot, proteins were extracted as described below. Slices were placed in 2 ml frozen microcentrifuge tubes containing two tungsten carbide beads (3 mm diameter—Qiagen) and an appropriate volume of lysis buffer. Tubes were then placed in the Tissue Lyzer adapter set 2 × 24 for 4 min at 20–30 Hz (Qiagen). Supernatants were then incubated on ice for 30 min before centrifugation (10,000 rpm for 10 min). The amount of protein was quantified by the Bradford assay technique before immunoblotting.
Results
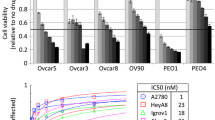
ABT-737 is ineffective as a single agent in ovarian cancer cells in vitro
Four human ovarian carcinoma cell lines (two cisplatin-resistant cell lines: IGROV1-R10 and SKOV3 and two cisplatin-sensitive: A2780 and OAW42) were exposed to an increasing range of ABT-737 concentrations for 24 h. We did not observe any substantial effect of ABT-737 on cell proliferation or cell death (quantified by cell cycle analysis), regardless of cell line sensitivity to cisplatin, even for the highest concentration (10 μM) presented in Fig. 1.
Response of four ovarian carcinoma cell lines to 10 μM ABT-737. Two cisplatin-resistant (IGROV1-R10, SKOV3) and two cisplatin-sensitive (A2780, OAW42) cell lines were either treated with 10 μM ABT-737 or not (DMSO) for 24 h. Response was measured by morphological features and DNA content. Histograms of cell cycle analysis represent the mean ± SEM of sub-G1 peaks from three independent experiments
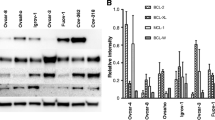
Mcl-1 down-regulation sensitizes ovarian cells to ABT-737
To critically test the functional significance of Mcl-1 in the resistance of ovarian cells to ABT-737, we examined the effect of Mcl-1 knockdown by means of a previously validated and specific siRNA. As single agents, neither ABT-737 nor siMCL1 were effective, however their combination led to massive cell death in SKOV3 cells (Fig. 2a left panel). The apoptotic nature of cell death was highlighted by strong cell detachment and sub-G1 peak on a DNA content histogram (Fig. 2a right panel), as well as PARP and caspase 3 cleavages appearing at a concentration as low as 0.1 μM (Fig. 2b). Neither the combination of ABT-737 with control siRNA, nor the combination of enantiomer with siMCL1 induced cell death (supp data 1). Real-time cellular activity measurements (xCELLigence technology) also confirmed the cytotoxic effect of the siMCL1/ABT-737 combination (Fig. 2c). This graph showed that a dramatic drop in CI occurred for those cells transfected with siMCL1 and treated with 1 and 10 μM ABT-737. Conversely, we did not observe any effect on CI with either ABT-737 or siMCL1 used as single agents.
Silencing Mcl-1 sensitizes SKOV3 cells to ABT-737. SKOV3 cells were transfected with either an ineffective siRNA (siControl) or siMCL1 for 24 h. After transfection, cells were exposed to increasing doses of ABT-737 for another 24 h. a In each case morphological features and DNA content were studied. Histograms of cell cycle analysis represent the mean ± SEM of sub-G1 peaks from three independent experiments, b expression levels of Mcl-1, Noxa and PARP and caspase 3 cleavages were studied by western-blot, c real time analysis of cellular cytotoxicity of the ABT-737/siMCL1 combination. The histogram was obtained using the xCELLigence System as described in “Materials and methods” section. Cells were grown for 24 h, then transfected with either siControl or siMCL1 (arrow). Cells were treated with increasing doses of ABT-737 24 h after transfection (dotted arrow). CI was recorded every 2 h. The results are the means of three replicates, with displayed standard error bars, d cells were pre-treated with either DMSO or 10 μM ABT-737 for 16 h, then treated with 2 μg/ml cycloheximide (CHX) for 20, 40 and 60 min. Mcl-1 and Noxa expression were analyzed by western blot and quantified by Image J software. The relative intensity of each lane was calculated with respect to the sample at 0 min (lower panels)
It is interesting to note that as a single agent, ABT-737 caused a significant dose-dependent induction of both Mcl-1 and Noxa in our models (Fig. 2b). In order to characterize the nature of this induction, SKOV3 cells were pre-treated with either ABT-737 or its vehicle DMSO for 16 h, then treated with the translation inhibitor, CHX, for the indicated times. We revealed by immunoblot that the degradation of Mcl-1 and Noxa was delayed in the presence of ABT-737, with respective half-life values increasing from 36 to 60 min (Mcl-1) (Fig. 2d upper panel) and from 72 to 460 min (Noxa) (Fig. 2d lower panels). This suggests that the induction of Mcl-1 and Noxa by ABT-737 involves post-translational events. Similar results were also obtained in IGROV1-R10 cells (Fig. 3).
Silencing Mcl-1 sensitizes IGROV1-R10 cells to ABT-737. IGROV1-R10 cells were transfected with either an ineffective siRNA (siControl) or with siMCL1 for 24 h. After transfection, cells were exposed to increasing doses of ABT-737 for another 24 h. a Morphological features and DNA content were studied for these conditions. Histograms of cell cycle analysis represent the mean ± SEM of sub-G1 peaks from three independent experiments, b Expression levels of Mcl-1, Noxa and PARP and caspase 3 cleavages were studied by western-blot, c real time analysis of cellular cytotoxicity of ABT-737/siMCL1 combination. The histogram was obtained using the xCELLigence system as described in “Materials and methods” section. Cells were grown for 24 h, then transfected with either siControl or siMCL1 (arrow). Cells were treated with increasing doses of ABT-737 24 h after transfection (dotted arrow). Cell Index was recorded every 2 h. The results are the means of three replicates, with displayed standard error bars, d cells were pre-treated with either DMSO or 10 μM ABT-737 for 16 h, then treated with 2 μg/ml cycloheximide for 20, 40 and 60 min. Mcl-1 and Noxa expression were analyzed by western blot and quantified by Image J software. The relative intensity of each lane was calculated with respect to the sample at 0 min (lower panels)
Cisplatin and carboplatin both sensitize ovarian cells to ABT-737 and vice versa
We combined cisplatin and ABT-737 in SKOV3 cells and observed that cisplatin alone induced only an S phase elongation and a G2-M blockade, whereas it synergized with ABT-737 to induce massive cell death (Fig. 4a). This combination led to a strong cell detachment and the appearance of a sub-G1 peak (37.2 % for CDPP/ABT-737 combination vs. 8.06 % for ABT-737 alone) (Fig. 4c upper panel) associated with cell death occurring from the G2-M phases, evident by the shifts on the FS/FL3 histograms (cell size/DNA content) (Fig. 4b). Cell viability confirmed that ABT-737 as a single agent remained almost ineffective and cisplatin was only cytostatic, whereas their combination was highly cytotoxic (Fig. 4c lower panel). This strong synergistic effect was also supported by complete PARP and caspase 3 cleavages (Fig. 4d). Similar findings were also obtained in IGROV1-R10 cells (data not shown).
Effect of cisplatin/ABT-737 treatment in SKOV3 cells. a SKOV3 cells were either exposed to cisplatin 20 μg/ml or not for 2 h, then treated with either 10 μM ABT-737 or vehicle for 46 h. Morphological/nuclear features were then studied, b FS/FL3 histograms (cell size/DNA content) were used to characterize the nature of cell death, c upper panel: histograms of cell cycle analysis represent the mean ± SEM of sub-G1 peaks from three independent experiments, lower panel: cell viability was quantified by Trypan blue coloration. Data represent the mean ± SEM of three independent experiments, d expression levels of Mcl-1, Noxa, and Bim, as well as PARP and caspase 3 cleavages were then studied by western blot. Data are representative of three independent experiments
It should be noted that in SKOV3 cells, cisplatin alone induced both Noxa and Bim, which was reinforced by the presence of ABT-737 (Fig. 4d). Interestingly, the cisplatin/ABT-737 combination completely abolished ABT-737-induced Mcl-1. This result suggests that massive apoptosis only occurs once there is an optimal increase of BH3-only proteins Noxa and Bim and down-regulation of Mcl-1. As carboplatin is more frequently used in clinical practice than cisplatin, due to its lower toxicity, we tested its combination with ABT-737. Three exposure protocols were performed: (i) 24 h-carboplatin/ABT-737 cotreatment followed by 24 h without drug; (ii) 48 h-carboplatin/ABT-737 cotreatment; (iii) 24 h-carboplatin exposure followed by 24 h ABT-737 exposure (Fig. 5a). We observed that concomitant 24 h-exposure to carboplatin and ABT-737 was completely ineffective in inducing apoptosis (Protocol 1 data not shown). However, both 48 h exposure protocols (protocols 2 and 3) led to massive cell death, revealing how important the presence of ABT-737 is during the last 24 h following carboplatin exposure. The comparison between protocols 2 and 3 revealed that optimal results were obtained with a concomitant 48 h exposure to carboplatin and ABT-737 (Protocol 2, Fig. 5b). Even though carboplatin was able to decrease Mcl-1 expression, it had no impact on ABT-737-induced Mcl-1 up-regulation, as was the case for cisplatin (Fig. 5c). However, carboplatin reinforced the ABT-737-increased level of Noxa, and to a lower extent, Bim. Therefore, as previously observed with cisplatin, greater cell death occurs in those conditions which optimize the inactivation of Mcl-1.
Schedules of carboplatin and ABT-737. a SKOV3 cells were treated following three protocols of exposure to carboplatin and ABT-737, b morphological features and DNA content were then studied for protocols 2 and 3, c expression levels of Mcl-1, Noxa and Bim, as well as PARP cleavage, were studied by western blot for protocols 2 and 3. Data are representative of three independent experiments
Noxa is required for platinum-induced sensitization to ABT-737
We next investigated the impact of targeting Noxa by siRNA on the apoptosis of SKOV3 cells induced by the combinations of AB7-737/cisplatin, and ABT-737/carboplatin. Noxa silencing reduced apoptotic cell death induced by both combinations, as shown by morphological and nuclear features (Fig. 6a vs. 6b, c left panels), as well as the inhibition of PARP and caspase 3 cleavages quantified by densitometry (Fig. 6b, c right panels and inserts). Cell cycle analysis revealed that siNOXA led to the protection of SKOV3 cells (with a drop of sub-G1 peak around 37 % for the condition siNOXA/CA + ABT-737 compared to its control siCONTROL/CA + ABT-737 and 25 % for the CDDP/ABT-737 combination Fig. 4d). On the contrary, Bim did not appear to have a major role since its knockdown by siRNA did not protect cells from carboplatin/ABT-737-induced apoptosis (supp data 2). These results indicate that up-regulation of Noxa is required for the sensitization to ABT-737 induced by platinum compounds.
Silencing Noxa attenuates ABT-737/platinum compounds-induced apoptosis. SKOV3 cells were transfected for 24 h with either nonspecific siRNA (siControl) or siNoxa, as described in “Materials and methods” section. a Transfected cells were then treated for 48 h with DMSO or 10 μM ABT-737 alone, b 20 μg/ml cisplatin ± 10 μM ABT-737, c 20 μg/ml carboplatin ± 10 μM ABT-737 as described in “Materials and methods” section. After treatment, cells were harvested and morphological and nuclear features were analyzed. Noxa expression, PARP and caspase 3 cleavages were studied by western blot. Caspase 3 cleavage was also quantified by Image J software (inserts). The relative intensity of each lane was calculated with respect to the sample where cell death was the strongest (b CDDP/ABT-737 and c CA + ABT-737). Data are representative of three independent experiments, d histograms of cell cycle analysis represent the mean ± SEM of sub-G1 peaks relative to the control conditions
Ex vivo experiments
We next studied the impact of three-dimensional tissue organization and microenvironment on response to treatment. We worked ex vivo using tissue sections (400 μm) from SKOV3 tumor nodes initially subcutaneously xenografted into nude mice. Immunohistodetection of cleaved caspase 3 showed that neither DMSO nor carboplatin alone induced cell death, whereas ABT-737 as a single agent induced apoptosis in a large fraction of the tumor cell population. Moreover, this effect was reinforced by its combination with carboplatin (Fig. 7a). Indeed, for this combination, the tumor tissue appeared disorganized, tumor cells presented numerous structural alterations, most of the cell nuclei appeared condensed or fragmented, and we observed strong immunostaining with a cleaved caspase 3 antibody.
Ex vivo effect of carboplatin/ABT-737 combination. Six-week old nude mice were xenografted subcutaneously with SKOV3 cells. Nodes were cut into 400 μm-slices and treated for 48 h with DMSO, 10 μM ABT-737, 20 μg/ml carboplatin or 20 μg/ml carboplatin + 10 μM ABT-737. a Immunohistology was performed on paraffin sections: cleaved caspase 3 staining was realized to evaluate cell death, b expression levels of Mcl-1, Bim, Noxa and Bcl-xL as well as caspase 3 cleavage were studied by western blot. Data are representative of three independent experiments
These observations were confirmed by western blot, as the combination of ABT-737/carboplatin resulted in a marked appearance of active caspase 3 protein, whereas DMSO or carboplatin alone had no effect (Fig. 7b). Interestingly, we also noted in experiments performed ex vivo, that both Noxa and Bim were strongly expressed at the basal level (T0).
Similar results were obtained with cisplatin, although in this case, a greater toxicity was observed using this drug as single agent and nodes exposed to a combination of ABT-737/cisplatin were completely desegregated (data not shown). The same experiments were carried out using IGROV1-R10 cell lines which led to similar results (data not shown).
Discussion
Chemoresistance is one of the leading causes of therapeutic failure in ovarian carcinoma. We previously demonstrated that chemoresistance results from Bcl-xL and Mcl-1 cooperation and that their concomitant inhibition leads to massive apoptosis. The aim of this study was to demonstrate that such a concomitant inhibition could be achieved by combining the Bcl-xL-targeting BH3-mimetic molecule, ABT-737, with platinum derivatives which indirectly act on Mcl-1 expression or activity.
Our results revealed that ABT-737 as a single agent is not able to induce massive cell death in ovarian cancer cells, even with doses as strong as 10 μM in vitro. This has also been observed in most solid tumors such as lung [29], breast [30], colon [31], or prostate cancers [21]. In contrast, this compound demonstrated an anti-tumor effect as a single agent in hematological malignancies [15, 16, 32], which could correlate to the strong expression of Bcl-2 in these cells. However, we did not observe any differences in sensitivity to ABT-737 between the Bcl-2 expressing ovarian cancers cells (SKOV3, OAW42) and the non-expressing cell line (IGROV1-R10). In addition, we previously showed that the expression of Bcl-2 is not associated with the response to another BH3-mimetic, HA14-1 [26].
It could be hypothesized that there is less ABT-737 available to act on its targets in ovarian carcinoma due to its higher inactivation, degradation or elimination in these cells. However, the massive apoptosis observed in Mcl-1 silenced-cells after exposure to concentrations of ABT-737 as low as 0.1 μM proves that this agent is able to efficiently inhibit its targets. Therefore, resistance to ABT-737 is most likely to be linked to the protective signal constituted by the presence of Mcl-1, rather than the lessened ability of ABT-737 to target Bcl-xL. This is in agreement with our previous work demonstrating that ovarian cancer cell death requires both Bcl-xL and Mcl-1 inactivation [9, 10]. It is also consistent with the involvement of Mcl-1 in resistance to ABT-737 as previously shown in hematological malignancies [23, 33] as well as solid tumors [18] and with other BH3-mimetic such as HA14-1 [26]. We have been able to highlight the importance of this concept since in our cells, Mcl-1 appeared to be dose-dependently up-regulated upon ABT-737 treatment and such a result has also been observed in other cancer types [24, 34, 35]. Unlike Yecies et al. [35], ABT-737 did not induce Mcl-1 transcription in our models (supp data 3 panel A). Therefore it could be hypothesized that ABT-737 modulates Mcl-1 degradation. Two pathways of degradation are involved in Mcl-1 turn-over. The first one was attributed to the proteasome by Nijhawan et al. [36] in Hela cells. The lysine residues are targeted for ubiquitination by Mcl-1 Ubiquitin Ligase E3 (MULE) and addressed to the proteasome. Mcl-1 can also be phosphorylated by GSK3 beta and ubiquitinilated by a second E3-ligase, namely beta transducin-containing protein (beta-TrCP) and degradated by proteasome [37]. Secondly, Mcl-1 is known to be additionally subject to non-proteasomal degradation and cleaved by caspase 3 at two sites within the N-terminus [38, 39]. In our experiment, CHX (a well-established protein synthesis inhibitor) induced a rapid decrease in Mcl-1 expression (less than 1 h) that was substantially blocked in the presence of ABT-737. The quickness of this down-regulation as well as the fact that CHX treatment does not induce apoptosis and caspase 3 activation (no caspase 3 cleavage, Supp. Data 3, panel B) lead us to think that this degradation is mediated by proteasome and that Mcl-1 up-regulation results from a delayed degradation in ABT-737-treated cells. The same experiment was carried on by Hikita et al. [40] and led to the same conclusions.
Although the mechanisms involved are not clear at present, it is known that Mcl-1 stabilization can result from USP9X-mediated deubiquitination [41], AKT-induced GSK3β inhibition [42], binding to BH3-only Bim or Puma [43] or ERK-induced phosphorylation [44]. The two latter mechanisms were recently highlighted in leukemia cell models [45]. In fact, the authors demonstrated that cells which have developed an acquired resistance to ABT-737 exhibit increased expression of Mcl-1 in addition to post-translational modifications (i.e. ERK-induced Ser-64 and Thr-163 phosphorylation) that facilitate both Mcl-1 stabilization and its interaction with the BH3-only protein Bim.
Targeting Mcl-1 is therefore a rational strategy to improve the efficacy of ABT-737. Knockdown of Mcl-1 expression strongly sensitizes ovarian carcinoma cells to this BH3-mimetic, adding ovarian cancer to the list of cell types in which the expression levels of Mcl-1 determine the susceptibility to ABT-737-induced apoptosis [14, 33, 34, 46].
It is important to note that in our study Mcl-1 silencing was accompanied by a reduction in Noxa expression. This result was also observed by others in melanoma cell lines [47], although further studies are required to understand this mechanism.
Strikingly, we also observed a dose-dependent increase in Noxa expression upon ABT-737 treatment. ABT-737 has already been proven to induce transcriptional induction of Noxa in small cell lung cancer [29]. However, a recent study showed that within a panel of BH3-mimetics, ABT-737 was the only molecule unable to induce Noxa mRNA [48]. Overall, our findings reveal that Noxa is stabilized by ABT-737 and to our knowledge this is the first time that ABT-737 has been demonstrated to stabilize this protein.
Platinum derivatives have been described to reduce expression of Mcl-1 either through post-translational degradation [49], or the increased expression of BH3-only proteins [13, 19]. In our model of ovarian carcinoma, Bim and Noxa appeared to be dose-dependently increased by cisplatin, whereas Mcl-1 expression was decreased. In fact, we demonstrated that this decrease was dose and time dependent, with optimal values of 20 μg/ml CDDP and 48 h in SKOV3 cells (Supp data 4A). The analysis of Mcl-1 mRNA allowed us to rule out transcriptional events in our models (Supp data 4B left and right panels). It is noteworthy that even if Mcl-1 is overexpressed in response to ABT-737, cisplatin is able to overcome this induction.
Although carboplatin may be considered as an analogue of cisplatin, its pharmacokinetic properties, side effects, and intrinsic activity are significantly different from those of cisplatin [50]. The steric hindrance may explain the slow reactivity of carboplatin with DNA [51]. Indeed, a preclinical study showed that carboplatin produces lower levels of DNA platination and DNA fragmentation compared to cisplatin. The authors concluded that these results suggest that the processes leading to drug-induced cell death may differ for different platinum drugs [52]. Therefore it could be suggested that this difference of DNA platination could be at least in part responsible for different activations of down-stream pathways and for subsequently different modulations of Mcl-1 expression. However, in patients with advanced ovarian cancer, a chemotherapy regimen consisting of carboplatin plus paclitaxel results in less toxicity, is easier to administer and is not inferior when compared with cisplatin plus paclitaxel [53]. This led carboplatin to progressively become the standard platinum compound used for ovarian cancers therapeutic care.
We demonstrated by different drug schedules that carboplatin exposure had to precede ABT-737 treatment to trigger strong apoptosis. Indeed, the concomitant exposure to ABT-737 and carboplatin during 24 h did not produce any effect, whereas a 24 h carboplatin exposure followed by a 24 h ABT-737 exposure induced massive cell death, as did a 48 h simultaneous treatment. Therefore, when combined with ABT-737, carboplatin constitutes an interesting sensitizing agent, as suggested by a mathematical model [54].
Taken together, these observations indicate that a minimum of 24 h is required for the indirect inactivation of Mcl-1 (for instance through the induction of Noxa) and it is imperative that ABT-737 is present following this 24 h period, which has also been suggested by Witham et al. [55]. This latter point also suggests that in the absence of ABT-737, the inactivation of its targets is reversible, therefore its presence is essential for inactivating neo-synthesized Bcl-xL and its other targets. Such observations could have an important impact on subsequent therapeutic applications.
We also observed that the carboplatin/ABT-737 combination led to a strong induction of Noxa. However, it was surprising to note that Mcl-1 is not necessarily degraded upon this type of treatment in ovarian cancer cell lines and similar results were also observed in renal cell carcinoma [56]. The induction of Noxa without subsequent Mcl-1 degradation is not in agreement with the notion that Noxa mediates Mcl-1 degradation. However, other studies describing similar results concluded that changes in Noxa expression do not always correlate with changes in Mcl-1 [29].
In our models, neither ABT-737 alone nor carboplatin alone allowed a sufficient Noxa induction to lead to cell death. In contrast, their combination led to a stronger induction of Noxa, that could overcome the threshold needed to counteract Mcl-1 up-regulation. This result leads to the conclusion that in cases where carboplatin does not overcome the ABT-737-induced increase in Mcl-1 expression, the induction of BH3-only proteins appears to be crucial for both Mcl-1 inactivation and ABT-737 efficacy.
Requirement of Noxa induction for carboplatin-mediated sensitization to ABT-737 was demonstrated by the observation that siNoxa protects cells against apoptosis. Moreover, the role of Noxa was confirmed since siNOXA also counteracts ABT-737/cisplatin-mediated apoptosis, a condition in which Mcl-1 is itself partially decreased. Thus, in all cases, both Mcl-1 down regulation and/or Noxa induction are essential for optimal induction of cell death. Similar observations were also described in head and neck carcinoma [46]. Our findings strongly support the notion that the Mcl-1/Noxa axis has to be modulated in order to sensitize cells to ABT-737 [47, 57].
As chemotherapy and ABT-737 led to a significant induction of Bim, we also tested its involvement in this combination-mediated apoptosis. Our results ruled out the implication of Bim in carboplatin/ABT-737-induced apoptosis since targeting this BH3-only protein did not protect cells from death, unlike Noxa.
To better understand the complexity and impact of the micro-environment and tissue organization, we evaluated treatment in ex vivo conditions. Xenografted SKOV3 and IGROV1-R10 tumor nodes slices were concomitantly exposed to platinum compounds and ABT-737 ex vivo. The tissues remained healthy as assessed by their histological appearance even after 48 h, excluding difficulties due to this technique. However, in this particular case (tri-dimensional preserved architecture and ex vivo culture during 48 h), ABT-737 alone was able to induce tumor cell death, whereas this was not the case in vitro. This effect could be explained by the high expression of Noxa and Bim at the basal level (i.e. immediately after tumor excision), which could be a consequence of intra-tumoral pressure and hypoxia frequently observed in tumor nodes in vivo [58–60]. Mcl-1 has also recently been demonstrated to be down-regulated in hypoxic tumor areas, thus conditioning the preferential response to ABT-737 [61]. The modulation of the Mcl-1/BH3-only balance could thus explain the sensitization of our cells to ABT-737 ex vivo. Indeed, High et al. [62] demonstrated that the expression of the pro-apoptotic protein Bim significantly correlated with in vivo sensitivity of acute lymphoblastic leukemia xenografts to ABT-737. Hence, the in vivo environment may provide signals to induce Mcl-1 antagonists or directly decrease Mcl-1 expression, explaining why ABT-737 displayed single-agent efficacy. Additional studies are however required to understand the molecular mechanisms involved.
Our results are also in agreement with a study performed on sliced human prostate tumor samples exposed ex vivo to a ABT-737/cisplatin combination [21]. In this study, ABT-737 alone induced apoptosis in some cases, although to a lower extent when compared to the cisplatin/ABT-737 combination. Moreover, the authors also showed that ABT-737 as a single agent was able to induce the regression of prostate tumor allografts, whereas it was ineffective in vitro.
In conclusion, our study confirmed that a therapeutic strategy based on inhibiting Bcl-xL strictly requires Mcl-1 inhibition to induce cell death in chemoresistant ovarian carcinoma cells. Platinum compounds could therefore constitute efficient ABT-737-sensitizing agents, through their ability to either down-regulate Mcl-1 or induce expression of BH3-only proteins. Furthermore, Noxa was demonstrated to be crucial for platinum compounds-induced sensitization to ABT-737. We showed that ABT-737 is able to induce apoptosis on its own ex vivo, which could be associated with strong basal expression of Noxa and Bim. However, apoptosis induction was strongly reinforced when ABT-737 was combined with carboplatin.
In conclusion, this strategy of combining ABT-737 with platinum compounds appears to be an attractive option for reversing resistance to platinum derivatives, which are the most active drugs in ovarian cancer. Conversely, this study has revealed platinum derivatives as pertinent sensitizers to ABT-737 through their direct or indirect inhibition of Mcl-1, which opens up new avenues for this promising BH3-mimetic molecule in the clinic.
Abbreviations
- CA:
-
Carboplatin
- CDDP:
-
Cisplatin (cis-diammino-dichloro-platinum(II))
- CHX:
-
Cycloheximide
- DAPI:
-
4′,6-diamidino-2-phenylindole
- PARP:
-
Poly (ADP-ribosyl) polymerase
- PI:
-
Propidium iodide
- HA14-1:
-
Ethyl [2-amino-6-bromo-4-(1-cyano-2-ethoxy-2-oxoethyl)]-4H-chromene-3-carboxylate
- HES:
-
Hematoxylin eosin safran
References
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144:646–674
Fesik SW (2005) Promoting apoptosis as a strategy for cancer drug discovery. Nat Rev Cancer 5:876–885
Adams JM, Cory S (2007) The Bcl-2 apoptotic switch in cancer development and therapy. Oncogene 26:1324–1337
Williams J, Lucas PC, Griffith KA et al (2005) Expression of Bcl-xL in ovarian carcinoma is associated with chemoresistance and recurrent disease. Gynecol Oncol 96:287–295
Dodier P, Piche A (2006) Bcl-X(L) is functionally non-equivalent for the regulation of growth and survival in human ovarian cancer cells. Gynecol Oncol 100:254–263
Villedieu M, Louis MH, Dutoit S et al (2007) Absence of Bcl-xL down-regulation in response to cisplatin is associated with chemoresistance in ovarian carcinoma cells. Gynecol Oncol 105:31–44
Shigemasa K, Katoh O, Shiroyama Y et al (2002) Increased MCL-1 expression is associated with poor prognosis in ovarian carcinomas. Jpn J Cancer Res 93:542–550
Brotin E, Meryet-Figuiere M, Simonin K et al (2010) Bcl-XL and MCL-1 constitute pertinent targets in ovarian carcinoma and their concomitant inhibition is sufficient to induce apoptosis. Int J Cancer 126:885–895
Varin E, Denoyelle C, Brotin E et al (2010) Downregulation of Bcl-xL and Mcl-1 is sufficient to induce cell death in mesothelioma cells highly refractory to conventional chemotherapy. Carcinogenesis 31:984–993
Trudel S, Li ZH, Rauw J, Tiedemann RE, Wen XY, Stewart AK (2007) Preclinical studies of the pan-Bcl inhibitor obatoclax (GX015-070) in multiple myeloma. Blood 109:5430–5438
Oliver L, Mahe B, Gree R, Vallette FM, Juin P (2007) HA14-1, a small molecule inhibitor of Bcl-2, bypasses chemoresistance in leukaemia cells. Leuk Res 31:859–863
Arisan ED, Kutuk O, Tezil T, Bodur C, Telci D, Basaga H (2010) Small inhibitor of Bcl-2, HA14-1, selectively enhanced the apoptotic effect of cisplatin by modulating Bcl-2 family members in MDA-MB-231 breast cancer cells. Breast Cancer Res Treat 119:271–281
Oltersdorf T, Elmore SW, Shoemaker AR et al (2005) An inhibitor of Bcl-2 family proteins induces regression of solid tumours. Nature 435:677–681
Chauhan D, Velankar M, Brahmandam M et al (2007) A novel Bcl-2/Bcl-X(L)/Bcl-w inhibitor ABT-737 as therapy in multiple myeloma. Oncogene 26:2374–2380
Del GMV, Brown JR, Certo M, Love TM, Novina CD, Letai A (2007) Chronic lymphocytic leukemia requires BCL2 to sequester prodeath BIM, explaining sensitivity to BCL2 antagonist ABT-737. J Clin Investig 117:112–121
Kuroda J, Kimura S, Andreeff M et al (2008) ABT-737 is a useful component of combinatory chemotherapies for chronic myeloid leukaemias with diverse drug-resistance mechanisms. Br J Haematol 140:181–190
Wesarg E, Hoffarth S, Wiewrodt R et al (2007) Targeting BCL-2 family proteins to overcome drug resistance in non-small cell lung cancer. Int J Cancer 121:2387–2394
Tahir SK, Yang X, Anderson MG et al (2007) Influence of Bcl-2 family members on the cellular response of small-cell lung cancer cell lines to ABT-737. Cancer Res 67:1176–1183
Tagscherer KE, Fassl A, Campos B et al (2008) Apoptosis-based treatment of glioblastomas with ABT-737, a novel small molecule inhibitor of Bcl-2 family proteins. Oncogene 27:6646–6656
Bray K, Chen HY, Karp CM et al (2009) Bcl-2 modulation to activate apoptosis in prostate cancer. Mol Cancer Res 7:1487–1496
Chen S, Dai Y, Harada H, Dent P, Grant S (2007) Mcl-1 down-regulation potentiates ABT-737 lethality by cooperatively inducing Bak activation and Bax translocation. Cancer Res 67:782–791
Konopleva M, Contractor R, Tsao T et al (2006) Mechanisms of apoptosis sensitivity and resistance to the BH3-mimetic ABT-737 in acute myeloid leukemia. Cancer Cell 10:375–388
Kang MH, Wan Z, Kang YH, Sposto R, Reynolds CP (2008) Mechanism of synergy of N-(4-hydroxyphenyl)retinamide and ABT-737 in acute lymphoblastic leukemia cell lines: Mcl-1 inactivation. J Natl Cancer Inst 100:580–595
Willis SN, Chen L, Dewson G et al (2005) Proapoptotic Bak is sequestered by Mcl-1 and Bcl-xL, but not Bcl-2, until displaced by BH3-only proteins. Genes Dev 19:1294–1305
Simonin K, Brotin E, Dufort S et al (2009) Mcl-1 is an important determinant of the apoptotic response to the BH3-mimetic molecule HA14-1 in cisplatin-resistant ovarian carcinoma cells. Mol Cancer Ther 8:3162–3170
Poulain L, Lincet H, Duigou F et al (1998) Acquisition of chemoresistance in a human ovarian carcinoma cell is linked to a defect in cell cycle control. Int.J. Cancer 78:454–463
Ke N, Wang X, Xu X, Abassi YA (2011) The xCELLigence system for real-time and label-free monitoring of cell viability. Methods Mol Biol 740:33–43
Hauck P, Chao BH, Litz J, Krystal GW (2009) Alterations in the Noxa/Mcl-1 axis determine sensitivity of small cell lung cancer to the BH3-mimetic ABT-737. Mol Cancer Ther 8:883–892
Kutuk O, Letai A (2008) Alteration of the mitochondrial apoptotic pathway is key to acquired paclitaxel resistance and can be reversed by ABT-737. Cancer Res 68:7985–7994
Cragg MS, Jansen ES, Cook M, Harris C, Strasser A, Scott CL (2008) Treatment of B-RAF mutant human tumor cells with a MEK inhibitor requires Bim and is enhanced by a BH3-mimetic. J Clin Investig 118:3651–3659
Kline MP, Rajkumar SV, Timm MM et al (2007) ABT-737, an inhibitor of Bcl-2 family proteins, is a potent inducer of apoptosis in multiple myeloma cells. Leukemia 21:1549–1560
van Delft MF, Wei AH, Mason KD et al (2006) The BH3-mimetic ABT-737 targets selective Bcl-2 proteins and efficiently induces apoptosis via Bak/Bax if Mcl-1 is neutralized. Cancer Cell 10:389–399
Yin S, Dong Y, Li J et al (2012) Methylseleninic acid potentiates multiple types of cancer cells to ABT-737-induced apoptosis by targeting Mcl-1 and Bad. Apoptosis 17:388–399
Yecies D, Carlson NE, Deng J, Letai A (2010) Acquired resistance to ABT-737 in lymphoma cells that up-regulate MCL-1 and BFL-1. Blood 115:3304–3313
Nijhawan D, Fang M, Traer E et al (2003) Elimination of Mcl-1 is required for the initiation of apoptosis following ultraviolet irradiation. Genes Dev 17:1475–1486
Ding Q, He X, Hsu JM et al (2007) Degradation of Mcl-1 by beta-TrCP mediates glycogen synthase kinase 3-induced tumor suppression and chemosensitization. Mol Cell Biol 27:4006–4017
Weng C, Li Y, Xu D, Shi Y, Tang H (2005) Specific cleavage of Mcl-1 by caspase-3 in tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-induced apoptosis in Jurkat leukemia T cells. J Biol Chem 280:10491–10500
Clohessy JG, Zhuang J, Brady HJ (2004) Characterisation of Mcl-1 cleavage during apoptosis of haematopoietic cells. Br J Haematol 125:655–665
Hikita H, Takehara T, Shimizu S et al (2010) The Bcl-xL inhibitor, ABT-737, efficiently induces apoptosis and suppresses growth of hepatoma cells in combination with sorafenib. Hepatology 52:1310–1321
Schwickart M, Huang X, Lill JR et al (2010) Deubiquitinase USP9X stabilizes MCL1 and promotes tumour cell survival. Nature 463:103–107
Cross DA, Alessi DR, Cohen P, Andjelkovich M, Hemmings BA (1995) Inhibition of glycogen synthase kinase-3 by insulin mediated by protein kinase B. Nature 378:785–789
Warr MR, Acoca S, Liu Z et al (2005) BH3-ligand regulates access of MCL-1 to its E3 ligase. FEBS Lett 579:5603–5608
Ding Q, Huo L, Yang JY et al (2008) Down-regulation of myeloid cell leukemia-1 through inhibiting Erk/Pin 1 pathway by sorafenib facilitates chemosensitization in breast cancer. Cancer Res 68:6109–6117
Mazumder S, Choudhary GS, Al-Harbi S, Almasan A (2012) Mcl-1 phosphorylation defines ABT-737 resistance that can be overcome by increased Noxa expression in leukemic B cells. Cancer Res 72:3069–3079
Li R, Zang Y, Li C, Patel NS, Grandis JR, Johnson DE (2009) ABT-737 synergizes with chemotherapy to kill head and neck squamous cell carcinoma cells via a Noxa-mediated pathway. Mol Pharmacol 75:1231–1239
Lucas KM, Mohana-Kumaran N, Lau D et al (2012) Modulation of Noxa and MCL-1 as a strategy for sensitizing melanoma cells to the BH3-mimetic ABT-737. Clin Cancer Res 18:783–795
Albershardt TC, Salerni BL, Soderquist RS et al (2011) Multiple BH3-mimetics antagonize antiapoptotic MCL1 protein by inducing the endoplasmic reticulum stress response and up-regulating BH3-only protein Noxa. J Biol Chem 286:24882–24895
Yang C, Kaushal V, Shah SV, Kaushal GP (2007) Mcl-1 is downregulated in cisplatin-induced apoptosis, and proteasome inhibitors restore Mcl-1 and promote survival in renal tubular epithelial cells. Am J Physiol Renal Physiol 292:F1710–F1717
Chatelut E (2011) Pharmacology of platinum compounds: differences between the three molecules and factors of interpatient variability. Bull Cancer 98:1253–1261
Braddock PD, Connors TA, Jones M, Khokhar AR, Melzack DH, Tobe ML (1975) Structure and activity relationships of platinum complexes with anti-tumour activity. Chem Biol Interact 11:145–161
Goodisman J, Hagrman D, Tacka KA, Souid AK (2006) Analysis of cytotoxicities of platinum compounds. Cancer Chemother Pharmacol 57:257–267
Ozols RF, Bundy BN, Greer BE et al (2003) Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: a Gynecologic Oncology Group study. J Clin Oncol 21:3194–3200
Jain HV, Meyer-Hermann M (2011) The molecular basis of synergism between carboplatin and ABT-737 therapy targeting ovarian carcinomas. Cancer Res 71:705–715
Witham J, Valenti MR, De-Haven-Brandon AK et al (2007) The Bcl-2/Bcl-XL family inhibitor ABT-737 sensitizes ovarian cancer cells to carboplatin. Clin Cancer Res 13:7191–7198
Zall H, Weber A, Besch R, Zantl N, Hacker G (2010) Chemotherapeutic drugs sensitize human renal cell carcinoma cells to ABT-737 by a mechanism involving the Noxa-dependent inactivation of Mcl-1 or A1. Mol Cancer 9:164
Tromp JM, Geest CR, Breij EC et al (2012) Tipping the Noxa/Mcl-1 balance overcomes ABT-737 resistance in chronic lymphocytic leukemia. Clin Cancer Res 18:487–498
Kim JY, Ahn HJ, Ryu JH, Suk K, Park JH (2004) BH3-only protein Noxa is a mediator of hypoxic cell death induced by hypoxia-inducible factor 1 alpha. J Exp Med 199:113–124
Hetschko H, Voss V, Senft C, Seifert V, Prehn JH, Kogel D (2008) BH3-mimetics reactivate autophagic cell death in anoxia-resistant malignant glioma cells. Neoplasia 10:873–885
Mammen A, Kubin J, Greeley WJ et al (2011) Effect of hypoxia on expression of selected proteins involved in regulation of apoptotic activity in striatum of newborn piglets. Neurochem Res 36:746–753
Harrison LR, Micha D, Brandenburg M et al (2011) Hypoxic human cancer cells are sensitized to BH3-mimetic-induced apoptosis via downregulation of the Bcl-2 protein Mcl-1. J Clin Investig 121:1075–1087
High LM, Szymanska B, Wilczynska-Kalak U et al (2010) The Bcl-2 homology domain 3 mimetic ABT-737 targets the apoptotic machinery in acute lymphoblastic leukemia resulting in synergistic in vitro and in vivo interactions with established drugs. Mol Pharmacol 77:483–494
Acknowledgments
We acknowledge Edwige Lemoisson, Marie-Hélène Louis (BioTICLA Unit) and Maryline Duval (Flow cytometry accommodation, SF 4206 ICORE, University of Caen) for their helpful technical support and ABBOTT Laboratories for providing us with ABT-737. We also acknowledge AngloScribe society for English language editing. This work was supported by the “Ligue Contre le Cancer” (Calvados and Manche’s committee), the “Conseil Régional de Basse–Normandie” and the French State. KS was the recipient of a doctoral fellowship from the “Ligue Contre le Cancer” (Calvados’s Committee). Acquisition of the xCELLigence real-time activity measurement system has been supported by European Community (FEDER) and Comprehensive Cancer Center F. Baclesse.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Karin Simonin and Monique N’Diaye contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Simonin, K., N’Diaye, M., Lheureux, S. et al. Platinum compounds sensitize ovarian carcinoma cells to ABT-737 by modulation of the Mcl-1/Noxa axis. Apoptosis 18, 492–508 (2013). https://doi.org/10.1007/s10495-012-0799-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-012-0799-x