Abstract
Length-of-stay (LOS) for inpatient mental health care is a major driver of variation in resource use internationally. We explore determinants of LOS in England, focusing on the impact of emergency readmission rates which can serve as a measure of the quality of care. Data for 2009/2010 and 2010/2011 are analysed using hierarchical and non-hierarchical models. Unexplained residual variation among providers is quantified using Empirical Bayes techniques. Diagnostic, treatment and patient-level demographic variables are key drivers of LOS. Higher emergency readmission rates are associated with shorter LOS. Ranking providers by residual variation reveals significant differences, suggesting some providers can improve performance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Activity-based funding mechanisms are being used increasingly internationally in mental health services (Mason and Goddard 2009). These funding approaches create incentives for providers to increase efficiency but can also have incentives for providers to reduce quality (Jacobs 2014). In England, an activity-based funding approach—the National Tariff Payment System [formerly known as payment by results (PbR)]—has been extended to mental health to support these aims (Department of Health Payment by Results Team 2012). The unit of activity (or currency) for this payment system is a set of 21 care clusters based on need rather than diagnosis. The intention is that providers will be paid a fixed tariff based on the national average cost which implies that providers incurring costs above (or below) the national average in a particular care cluster will potentially lose (or gain). This payment system should encourage providers to reduce length-of-stay (LOS), as they will have an incentive to control their unit (or cluster) costs (Jacobs 2014). However, relative performance and resource use of mental health providers in England is comparatively under-researched, and patterns of resource use need to be examined if the potential impact of the National Tariff Payment System on mental health providers is to be understood. Using LOS as a proxy for cost and resource use (Martin and Smith 1996) we can explore variation in LOS across providers and the extent to which patient and provider characteristics explain this variation. LOS is a key driver of hospital costs, especially when care is staff-intensive as is the case in mental health (Mason et al. 2011). Differences in LOS can reflect differences in patient needs, but can also be indicative of differences in treatment philosophies and practice patterns (Horgan and Jencks 1987). One of the risks of the National Tariff Payment System is that the incentives to generate efficiencies through reducing unit costs and LOS may have unintended consequences such as skimping on quality (Jacobs 2014) which could have a detrimental effect on patient outcomes. A major challenge in monitoring the quality of mental health care lies in utilising hospital-based data to make inferences about both hospital and community care (Lakhani et al. 2005). Hospital emergency readmission rates are increasingly used as a performance measure and as a basis for hospital reimbursement (Laudicella et al. 2013) and can act as a good proxy measure for inferences about both hospital and community mental health care.
The aim of this paper is to examine variation in LOS among mental health providers in England, in particular the relationship between LOS and quality as reflected by provider emergency readmission rates. The study makes a unique contribution to research in two ways. First, the analysis uses three levels at which factors influence LOS, by considering admission-, patient- and provider-level variables. Second, the paper uses hierarchical and non-hierarchical models to explore variation in LOS and quantify the residual variation using Empirical Bayes estimates with comparative standard errors to compare residual variation across providers, providing quantitative estimates of unexplained differences in LOS between providers after controlling for patient and provider characteristics.
Findings from previous studies
Determinants of LOS for psychiatric inpatient care can be classified in terms of admission, patient or provider characteristics. Table 1 in the online supplementary material gives an overview of the main characteristics considered in previous studies and their relationship with LOS. At an admission-level, diagnostic (primary and secondary diagnoses), treatment (prior service use, involuntary admission) and socio-economic (social support, deprivation) variables are reported as being significantly associated with LOS. In terms of diagnostic variables, the presence of physical co-morbidities as well as a diagnosis of psychosis has been found to be associated with longer LOS while a co-morbid diagnosis of substance misuse disorder is generally reported as reducing LOS. There is less consensus regarding the effect of treatment and socio-economic characteristics. A longer LOS may arise from an involuntary admission if such admissions are indicative of greater severity of illness. Previous studies report that being married is associated with shorter LOS (Tulloch et al. 2011) and that prior service use may be associated with a shorter LOS as patients who are familiar with the mental health system can be treated and discharged more quickly (Rothbard and Schinnar 1996). However, prior service use may also be indicative of greater severity of illness thus resulting in a longer LOS (Huntley et al. 1998). Findings regarding socioeconomic deprivation are mixed. One study (Abas et al. 2008) reports that greater levels of socioeconomic deprivation in the inpatient’s neighbourhood of residence was associated with extended hospitalization after adjustment for demographic factors and primary diagnosis but not after adjustment for comorbid diagnosis, chronicity, function, and severity. Another study (Dekker et al. 1997) reports negative correlations between LOS and deprivation which may have been a consequence of deprived areas having a larger number of patients who are frequently readmitted for a short time. A non-linear relationship between LOS and age has been reported (McCrone and Lorusso 1999). A longer LOS for older people may be related to the availability of social support as well as the availability of and access to continuing health and social care (Bryan 2010; Pertile et al. 2011). Moreover, presentations by elderly patients may be medically complex due to a higher risk of medical co-morbidities and adverse reactions to medications (Pertile et al. 2011).
At a patient-level, Black ethnicity is associated with a longer LOS compared to White or Asian ethnicity (Padgett et al. 1994). There is no clear relationship between LOS and gender (Chung et al. 2010; Tulloch et al. 2011).
At a provider level, hospital capacity is positively associated with LOS (Chung et al. 2010) while healthcare staffing levels have a negative relationship with LOS (Imai et al. 2005). The positive relationship between LOS and hospital capacity is likely due to a desire to keep bed occupancy levels high and may also be related to the provider payment method (e.g. per diem) and hospital efforts to increase revenues (Chung et al. 2010). Lower staffing levels may be indicative of cost-cutting efforts on the part of hospitals that consequently reduce quality of care and increase LOS (Imai et al. 2005).
Data
Data Sources and Coverage
We drew on the literature on the determinants of LOS for psychiatric inpatient admissions to inform our choice of independent variables in our models. The independent variables comprise a range of admission-, patient- and provider-level variables that are likely to influence LOS. Admission- and patient-level variables were sourced from the hospital episode statistics (HES), a patient-level administrative dataset of all admissions, outpatient appointments and A&E attendances at NHS hospitals in England. HES information is stored as a large collection of separate records—one for each period of care—in a secure data warehouse and it is managed by the Health and Social Care Information Centre (HSCIC)—the national provider of information, data and IT systems for health and social care in England. Our study used HES data for 2009/2010 and 2010/2011, which we accessed through a data sharing agreement with the HSCIC. Sources for provider-level variables include HSCIC (variables sourced from HES), Hospital Activity Statistics, the Care Quality Commission, and the Department of Health Staffing Survey. These data are all publicly available on the websites of the respective organisations. The Hospital Activity Statistics are published by NHS England—an executive non-departmental public body of the Department of Health. The Care Quality Commission is the independent regulator of all health and social care services in England.
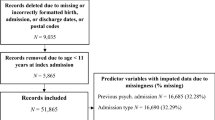
Our dataset consists of the majority (63) of public mental health care providers in England. Providers of mental health care comprise Mental Health Trusts, Care Trusts and Primary Care Trusts (PCTs).Footnote 1 We selected our study sample by trimming episodes of care to cover only patients with mental disorders treated by mental health care providers. More specifically, we dropped observations for admissions to primary care trusts (PCTs) without a record of an ICD-10 F chapter (mental and behavioural disorders) code or a Health Resource Group (HRG) Version 3.5 T code (Mental Health); observations for patients admitted prior to 1st April 2009 so that the dataset consists only of patients with finished episodes that were admitted during 2009/2010 and discharged during 2009/2010 or 2010/2011; and admissions with incorrectly coded age.
Dependent Variable
The dependent variable LOS is measured by the time elapsed between admission and discharge dates. LOS per admission ranges from a minimum of 0 days to a maximum of 708 days (Fig. 1).
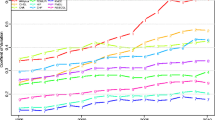
There is substantial variation in LOS between providers (Fig. 2).
Independent Variables
Level 1 relates to an admission i.e. a period of care in one provider. Level 1 variables can potentially change from admission to admission (admissions for an individual patient are not concurrent). Level 1 or admission-level independent variables reflect the diagnostic, treatment and socio-economic characteristics of patients included in the study and can potentially change from admission to admission. Patients can be transferred to or from another hospital provider. This indicator may be a proxy for patient case-mix because providers may specialize in the treatment of certain diagnoses and patients may be transferred if the provider they were originally admitted to cannot meet the needs of the patient. Patient death in hospital captures if the patient died during a particular admission. It reflects the percentage of all admissions with a reason for discharge coded as death. Patient death in hospital is a relatively rare event but it can act as an indicator of the quality of care provided (Department of Health and Human Services Agency for Healthcare Research and Quality 2002). Co-morbidities are measured using the total number of secondary diagnoses recorded for an admission. We include a number of indicator variables that describe the ICD-10 mental health chapter codes that represent the most common primary diagnoses recorded. Severity is reflected in psychiatric history represented by one or more previous psychiatric admissions. Another severity variable indicates if patients have been formally detained under the Mental Health Act (MHA). Marital status and a record of carer support signal the extent of social support available to patients. We include a variable that captures socio-economic deprivation as measured by the index of multiple deprivation (IMD) which has been widely used in applied research (Cookson et al. 2013; Sanchez-Santos et al. 2013). The IMD is measured at small area or lower layer super output area (LSOA) level and is assigned to patients on the basis of residency. LSOAs represent a geographic area with a mean population of 1500 (Health and Social Care Information Centre 2015). The IMD has seven domains, of which the IMD Income Domain is included in the dataset. The purpose of this Domain is to capture the proportions of the population experiencing income deprivation in an area (Noble et al. 2008). A higher score for the Income Domain indicates a greater proportion of the population in the area in which the patient lives experiences income deprivation. The scores for the Income Domain are rates which we multiplied by 100 to ease interpretation. So, for example, if an LSOA scores 0.72 in the Income Deprivation Domain, this means that 72 % of the LSOA’s population is income deprived. We indicate if an admission has been discharged to social care and this will include any delayed discharge which may increase LOS. Age is divided into 5 categories to capture any non-linearity in the relationship between LOS and age. Age category 2 (18–39) is the reference category.
Level 2 relates to variables measured at the patient-level that do not change from admission to admission. Patient-level independent variables cover demographic characteristics of patients. Gender is measured as a dummy variable with females as the reference category. Patient ethnicity is categorized into White (the reference category), Asian, Black and Other ethnicity (e.g. mixed race, or unknown ethnicity).
Level 3 variables are measured at the provider-level and vary only for admissions and patients in different hospitals. Provider-level independent variables describe provider type and capacity, proportion of formal admissions, emergency readmission rate, co-morbidities recorded by a provider, quality of care and human resources. Two dummy variables are included in the models to indicate if a provider is 1) a Mental Health Trust and/or 2) has Foundation Trust status. Mental Health Trusts provide health and social services for people with mental health problems, in particular specialist services for people with severe mental health problems. Care Trusts provide a range of services including social care and mental health services. PCTs provide the equivalent full set of mental health services as Mental Health Trusts, but are unable to become Foundation Trusts. Foundation Trusts differ from other NHS Trusts in that they are independent legal entities and have different governance arrangements. They are not subject to the same levels of performance management and have significant financial freedoms.
The variable “total available beds” provides a measure of hospital size. Total bed occupancy provides an indication of utilisation and reflects average bed occupancy over a quarterly time period for 2010/11 and an annual time period for 2009/2010. Human resources variables are measured as the percentage of medical staff from total full time equivalent (FTE) staff and the percentage of nursing staff from total FTE staff. Nurses make up a higher percentage of total FTE staff. The proportion of formal admissions under the MHA provides information on patient severity. We include a variable on formal admissions at provider-level as well as admission-level as we expect providers to have different thresholds for detention. Similarly, we include a provider-level variable measuring the average number of co-morbidities recorded by a provider. This complements the admission-level co-morbidity variable and controls for systematic under- or over-recording of co-morbidities by providers.
The study utilises emergency readmission rates for mental health providers which have not been calculated nationally before. We calculated rates for mental health providers using HES data, following a Department of Health methodology used for acute providers (Health and Social Care Information Centre 2011). However, we adapted this to include readmissions treated by mental health specialities. The HSCIC excludes mental health speciality in its standard calculation of emergency readmission rates for acute providers. In the calculation of readmission rates for mental health providers, the numerator is based on a pair of admissions—the discharge (index) admission and the next readmission to reflect emergency admissions within 28 days of discharge from hospital. The readmission includes cases where the patient dies but excludes those with a main speciality of obstetrics or learning disability upon readmission, and those with a diagnosis of cancer (other than benign or in situ) or chemotherapy for cancer coded anywhere in the admission. The denominator excludes day cases, admissions with a discharge coded as death, admissions with obstetric and learning disability specialities and those with a diagnosis of cancer or chemotherapy treatment for any form of cancer in the 365 days prior to admission.
Quality of care is also represented by a number of variables upon which providers are performance managed by the regulator, the Care Quality Commission. Crisis Resolution and Home Treatment (CRHT) teams provide intensive home-based support for people in mental health crises in their own home and stay involved until the problem is resolved (Care Quality Commission 2009). An aim of CRHT teams is to prevent hospital admissions; therefore access to CRHT teams can provide an indication of the level of gate-keeping available. This indicator is measured using the number of admissions to the Trust’s acute wards (excluding admissions to psychiatric intensive care units) that were “gate-kept” by the CRHT teams as a percentage of the total number of admissions to the Trust’s acute wards (excluding admissions to psychiatric intensive care units). The indicator Care Programme Approach (CPA) 7 day follow-up measures the extent to which people under adult mental illness specialities on CPA receive follow-up (by phone or face-to-face contact) within seven days of discharge from psychiatric inpatient care. Providers are judged to have “achieved” this indicator if at least 95 % of patients receive timely follow up post-discharge. The patient experience score is based on five domains: access and waiting; safe, high quality, coordinated care; better information, more choice; building relationships; and clean, comfortable, friendly place to be and a higher score indicates a more positive experience (Care Quality Commission 2010). We hypothesise that efforts by providers to drive down LOS may be associated with commensurate declines in quality.
Methods
Study Sample
Our data exhibits a multilevel structure with admissions nested in patients, who are nested in providers. Some patients have multiple admissions the majority of which are to the same provider, but approximately 2 % of patients (accounting for 4 % of admissions) have admissions to different providers. We use hierarchical and non-hierarchical models to model these nested data structures. As the majority of our sample has admissions to only one provider, we treat our data sample as a three-level hierarchy with admissions nested in patients who in turn are nested in hospitals (Fig. 3).
A limitation of using a three-level model when patients have admissions to more than one provider is that each patient is allowed to have an admission to only one provider; patients with admissions to more than one provider are counted more than once meaning that the number of patients is artificially inflated. In non-hierarchical models, the data are not structured in a strict hierarchy. For the purposes of this study we consider the cross-classified non-hierarchical data structure (Fig. 4).
Cross-classified data occurs when lower-level units relate to more than one distinct higher-level unit. Lower level units will then be connected to a pair or group of higher level units resulting in two or more higher level units or classifications being crossed (Leckie 2013). In our data, a cross-classified model can be considered more appropriate and will result in more accurate standard errors, especially for variables measured at higher levels (Leckie 2013). Our use of both three-level and cross-classified models allows us to investigate if the models produce consistent results when only a small portion of the sample does not exhibit a strict hierarchy (Fig. 3, 4).
Estimation Model
Our estimation model is a random effects multilevel generalised linear model. Multilevel generalised linear models contain multivariate normal random effects in the linear predictor (Skrondal and Rabe-Hesketh 2009). We estimate a multilevel generalized linear model containing a column vector of admission, patient and hospital characteristics or fixed effects, level 2 random intercepts or patient specific effects and level 3 random intercepts or hospital specific effects. The random effects are considered multivariate normal with strictly exogenous covariates (Skrondal and Rabe-Hesketh 2009). Conditional independence of the responses is assumed with conditional distributions drawn from the exponential family (Skrondal and Rabe-Hesketh 2009). Since our response variable (LOS) can be evaluated as count data, a Poisson distribution with a log link is specified. The variance function is equal to the mean and the dispersion parameter is equal to one. The Poisson distribution assumes that equi-dispersion is present implying that the conditional mean is equal to the variance. For some admissions the conditional variance may exceed the mean so the assumption of equi-dispersion is too restrictive. Therefore we allow for an extra binomial variation parameter to allow for over- or under-dispersion. Statistical significance is tested at the 5, 1 and 0.1 % levels.
Having obtained estimates of the model parameters and treating them as the true parameter values, we can predict values of the level 3 or hospital random effects using Empirical Bayes techniques. This will allow us to quantify the residual variation (i.e. the unexplained variation which remains after taking account of all the variables in our model) and compare this residual variation across hospitals in terms of LOS. Empirical Bayes prediction uses the prior distribution of the hospital random effects combined with the likelihood to obtain the posterior distribution of the random effects given the observed response variable (LOS). Estimates of the provider-level random effects are “shrunken” towards the mean of the posterior distribution with the degree of shrinkage determined by the relative information available on the group. A high level of shrinkage reflects relatively little information about the group (the number of patients is small for a particular provider or the patient-level variance is large relative to the provider-level variance). Therefore this shrinkage is desirable as it means less weight is placed on units that provide less information (Steele 2008). In order to compare the residual variation across hospitals we use comparative standard errors. We assume a normal posterior distribution and known model parameters in order to form Bayesian credible intervals using the posterior mean and posterior standard deviation. The posterior standard deviation is commonly used as a standard error of prediction for multilevel generalised linear models (Skrondal and Rabe-Hesketh 2009). The empirical Bayes estimates of the provider-level random effects are ranked and graphically displayed. The residuals represent hospital departures from the overall mean, so a hospital whose confidence interval does not overlap the line at zero is said to differ significantly from the average at the 5 % level. However, it is not possible to conclude that two hospitals whose confidence intervals fail to overlap are statistically significantly different from each other at the 5 % level as the confidence intervals are too wide (Goldstein and Healy 1995). As we use a log link, we can interpret provider performance in days of LOS by calculating the exponentiation of the Empirical Bayes estimates.
The three-level model is estimated using restricted iterative generalised least squares (RIGLS) which corresponds to restricted maximum likelihood (Goldstein 1989). The cross-classified model is estimated using the Monte Carlo Markov Chain (MCMC) method. MCMC utilises simulation methods to produce parameter estimates (Browne 2012). For the cross-classified model presented here, the chain is first run for 5500 iterations until the Markov chain converges and is then run for an additional 350,000 iterations. Parameter estimates and standard errors are based on the means and standard deviations of the estimates produced during each of the 350,000 iterations (Leckie and Charlton 2012).
The models were estimated in MLwiN 2.29 (Rabash et al. 2009) using the runmlwin command (Leckie and Charlton 2012) in Stata 13.0 (StataCorp LP 2014).
The coefficients on the predictor variables are expressed using incidence rate ratios (IRRs). The IRR represents exponentiated coefficients that can be given a multiplicative interpretation (Cameron and Trivedi 2011). Therefore, a positive coefficient signals that the variable exerts an upward pressure on LOS and a negative coefficient a downward pressure.
Sensitivity Analysis
We conduct a sensitivity analysis by re-estimating the models using a dataset that excludes the observations with zero LOS to test if admissions with a positive LOS better reflect resource use. We also run the 3-level model for the sample that excludes those patients with multiple providers.
Results
Descriptive Statistics
Table 1 presents the descriptive statistics for our data sample, presented according to the levels (admissions; patients; providers).
In-hospital death is a relatively rare event—it affects only 1 % of admissions in this dataset. The admissions in our sample had, on average, one co-morbidity recorded, but there was sizeable variation with some admissions recording no co-morbidities and up to seventeen co-morbidities recorded for others. Mood disorder was recorded for 20 % of admissions, making it the most common primary diagnosis followed by psychosis (16 %) and substance misuse disorder (9 %) while the primary diagnoses of organic, neurotic and personality disorders accounted for 6 % or less of admissions. Approximately 13 % of admissions were involuntary (i.e. the individual was detained under the MHA). In terms of social support, almost one-fifth (19 %) of the sample was married or had a civil partner while less than one-tenth (7 %) had a record of carer support. However, the latter may underestimate the true extent of carer support as it only reflects patients for whom there is a formal record. Almost half (41 %) of the sample have a history of psychiatric treatment. In our data, the IMD Income Domain variable has a minimum of 0 and a maximum of 83 %, with a mean of 20 %, which implies that the average admission was from a neighbourhood where 20 % of residents experienced income deprivation. Almost 6 % of admissions were discharged to a social care setting. Just over half of patients in our sample were male (51 %). White ethnicity accounts for the majority of the sample (85 %), followed by Other (6 %), Asian (5 %) and Black (5 %).
The majority (93 %) of providers in the sample are Mental Health Trusts and almost two-thirds (63 %) of providers have Foundation Trust status. Compared with those treated in Mental Health Trusts without Foundation Trust status, it is interesting to note that individuals in our dataset who are treated by Foundation Trusts are less likely to be transferred in from another hospital, have less comorbidity, and are less likely to have psychosis or a substance misuse disorder. They are less likely to have been formally detained, to have previous psychiatric admissions or be male, and more likely to be aged 65 years or over, or of White ethnicity.
The mean proportion of formal admissions under the MHA is 0.18 but this varies widely across providers from 0.04 to 0.65 suggesting that providers have different formal admission thresholds or different types of local populations. The mean emergency readmission rate is 0.12 but for one provider approximately one in twenty patients is readmitted while for another almost one in four patients is readmitted within 28 days. The providers in our sample have on average been successful in achieving the indicator measuring CPA 7-day follow-up with a mean score of 97 % and a maximum score of 100 %. However a minimum score of 83 % indicates that some providers failed to achieve adequate patient follow-up.
Estimation Results
Table 2 presents the estimates of the three-level and cross-classified models.
Admission-level variables with a significant positive association with LOS in both models include transfer-in, in-patient death, number of co-morbidities, a primary diagnosis of psychosis, a primary diagnosis of organic disorder, formal detention and discharge to social care. Of these, the variables measuring death in hospital, a diagnosis of psychosis, formal detention and discharge to social care have the largest significant effects on LOS. More specifically, patient death is associated with a 45 % increase in LOS in the three-level model and an 86 % increase in LOS in the cross-classified model. A primary diagnosis of psychosis is associated with an increase in LOS of around 40–50 % while detention under the MHA is associated with an increased LOS in the region of 50–60 %. Patients discharged to social care are associated with a LOS twice the duration of those who are discharged elsewhere. The association of a longer LOS with inpatient death, psychosis and formal detention is likely to reflect greater disease severity among these admissions. Similar to previous literature (McCrone and Lorusso 1999) we find evidence of a non-linear relationship between LOS and age with younger and older age groups having positive coefficients. The magnitude of the positive effect of age on LOS is greater for older age groups with the oldest age group (65 + years) associated with an approximately 50 % increase in LOS in the three-level model and a doubling of LOS in the cross-classified model. The variable measuring a primary diagnosis of mood disorder is also significant in the cross-classified model and is associated with an increase in LOS of 23 %.
Admission-level variables with a statistically significant negative association with LOS include transfer-out, a primary diagnosis of substance misuse and neurotic disorders, a record of carer support, psychiatric treatment history and income deprivation. A primary diagnosis of substance misuse disorder is associated with a 55 and 20 % reduction in LOS in the three-level and cross-classified model respectively. This finding may be because the presence of substance misuse disorder without a mental disorder diagnosis precludes detention under the MHA which we find to be associated with a longer LOS. A primary diagnosis of neurotic disorder is associated with a reduced LOS of around one-third in the three-level model and one-tenth in the cross-classified model. A record of carer support is associated with a 15–27 % reduction in LOS. Patients may be discharged earlier if a carer is available to provide care at home. Transfer-out reduces LOS in the order of 16–34 % while previous psychiatric treatment is associated with an 11–18 % decrease in LOS, possibly because services are familiar with the care of these patients.
Variables with opposing signs in the two models include a primary diagnosis of personality disorder and married/civil partner. A primary diagnosis of personality disorder is associated with a 17 % reduction in LOS in the three-level model and a 12 % increase in LOS in the cross-classified model. The negative association of personality disorder with LOS may be due to the behavioural challenges for some mental health services to manage this patient group. Married/civil partner is associated with a 9 % decrease in LOS in the three-level model but with a 10 % increase in the cross-classified model.
All of the patient-level variables have a statistically significant association with LOS with the exception of male gender in the cross-classified model. Black and Asian ethnicities are associated with a longer LOS compared to White ethnicity with Black ethnicity associated with a 17–31 % increase in LOS. The only patient-level variable with a statistically significant negative association with LOS is Other ethnicity which is associated with a 14–27 % reduction in LOS compared to white ethnicity.
In terms of provider-level variables, the emergency readmission rate is associated with a reduction in LOS of 95 % in the cross-classified model only. The variable measuring if a provider is a Mental Health Trust is statistically significant only in the three-level model and is associated with an increase in LOS of almost 40 %. The variable measuring the proportion of admissions under the MHA is statistically significant in both models and exerts a strong upward pressure on LOS of over two and a half times in the three-level model and almost 4 times in the cross-classified model. In the cross-classified model, a higher number of comorbidities recorded by a provider is associated with a reduction in LOS of 10 %. The variables measuring total bed occupancy, CPA 7 day follow-up, and total patient experience score, are associated with a small increase in LOS, while access to a CRHT team, and the percentage of nurses from total full time equivalent (FTE) staff contribute to a small reduction in LOS of around 1 % or less.
Results of the sensitivity analysis for the sample that excludes those patients with multiple providers remained stable when compared to the three-level model for the full sample presented here. When admissions with a zero LOS were excluded from the analysis, the variables measuring a primary diagnosis of an organic disorder and if a provider was a Mental Health Trust were statistically significant at the 5 and 1 % levels respectively in the three-level model. In the cross-classified model, the variable measuring if a provider is a Mental Health trust became statistically significant at the 0.1 % level.
While the admission-, patient- and provider-level variables included in the model explain most of the variation in LOS, there remains some residual variation in LOS as captured by the provider random effects. Figures 5 and 6 presents the empirical Bayes estimates of the provider-level residual variation from the three-level and cross-classified models respectively. Hospitals above (below) the line at zero have higher (lower) residual LOS compared to the average, i.e. the most (least) unexplained variation in LOS after controlling for patient and provider characteristics. This implicitly assumes that the model has controlled for all known factors driving LOS and the remaining variation is due to a range of unobserved factors, one of which may be inefficiency. While the majority of providers do not differ significantly from zero, there are a number of providers with a statistically significantly higher or lower LOS compared to the average.
The Empirical Bayes estimates also suggest that relative to the average performing hospital with respect to unexplained variation in LOS (i.e. the residual), the worst performing hospital has a higher LOS of almost half a day in the three-level model (Fig. 5) and almost 1 day in the cross-classified model (Fig. 6) due to factors not considered in the model such as variations in efficiency, suggesting that there is scope for some providers to improve their relative performance.
Discussion
Contribution to the Current Evidence Base
This paper has sought to investigate the main drivers of variations in LOS for mental health providers in England.
The largest drivers of increased LOS at admission level are in-hospital death, a primary diagnosis of psychosis, formal detention, discharge to social care and the oldest age group (65 years and over). The first three of these factors are likely to reflect greater disease severity (or need) among these admissions. At a patient-level, Black ethnicity is associated with the largest increase in LOS. At a provider-level, the proportion of formal admissions under the MHA has a large positive association with LOS.
We contribute to the current evidence base in a number of ways. The use of three-level and cross-classified models has allowed us to exploit the multilevel nature of a patient-level dataset with national coverage—the hospital episode statistics (HES) data. Our results reveal that when a small proportion of the sample exhibits a cross-classified structure, three-level and cross-classified models provide somewhat similar results with differences most pronounced at the highest level of the data. HES provides rich information on a wide range of variables related to admission-, patient- and provider-level attributes which enables us to move beyond current literature in this field which considers a more limited range of variables. Moreover, we include provider-level emergency readmission rates calculated using HES data—a valuable addition as the HSCIC does not routinely calculate emergency readmission rates for mental health care providers. This allows us to investigate the relationship between variations in LOS and provider quality of care as measured by the emergency readmission rate—another novel contribution to the current evidence base.
Policy Implications
We find that the provider emergency readmission rate has a strong negative association with LOS implying that providers with high emergency readmission rates are associated with a significantly shorter LOS. A plausible explanation is that providers may be compromising quality of care resulting in readmission and this is reflected in resource use in terms of LOS. Therefore, our findings lend some credence to the argument that, in the absence of clear guidelines on optimal LOS, decisions regarding duration of hospitalisation could be driven by economic rather than clinical considerations (Capdevielle and Ritchie 2008). Internationally, psychiatric LOS has experienced a downward trend corresponding to a decrease in psychiatric beds (OECD 2013) with shorter LOS associated with community-based mental health systems (Sytema et al. 2002). Yet, there lacks a clear consensus on what constitutes a short LOS or indeed on best practice in this area (Capdevielle and Ritchie 2008). A high emergency readmission rate may indicate an inadequate provision of mental health support in the community. It may also represent poor quality in-patient care during the index admission, in particular in relation to inadequate discharge preparedness (Durbin et al. 2007). Many previous studies have investigated the relationship between LOS and readmissions at the individual patient level for mental health. Shorter initial hospital stays have been shown to be related to higher readmissions (Appleby et al. 1993; Boden et al. 2011; Canadian Institute for Health Information 2008; Figueroa et al. 2004; Lin et al. 2006) but a long LOS has also been found to be associated with an increased risk of multiple readmissions (Korkeila et al. 1998). Efforts to reduce costs may drive shorter LOS (Capdevielle and Ritchie 2008; Lin et al. 2006) but risk compromising the quality of care leading to readmission which can in fact increase overall costs (Lin et al. 2006). Readmissions that take place within a relatively short period after discharge may be negatively associated with LOS due to the need for a longer inpatient stay to stabilise symptoms and provide adequate treatment. On the other hand, readmissions taking place within a longer period following discharge may be more likely to reflect the influence of factors beyond inpatient hospitalization, such as effective transitional care, the availability of community and family supports, access to primary care, housing and continued access and adherence to prescribed medications. This implies an important role for adequate discharge planning in protecting against early readmission (Durbin et al. 2007).
Our finding that shorter LOS comes at the expense of higher emergency readmission rates raises concerns of a ‘revolving door’ phenomenon that can undermine a policy of strong community care and has long-term cost and quality implications. Internationally, readmission rates have garnered policy focus as a result of an increased awareness of the need to achieve value for purchasers in terms of quality and cost (Burgess and Hockenberry 2014). This has led to the introduction of high-powered incentives in the form of financial penalties imposed on hospitals for levels of readmission that are deemed inappropriate (Burgess and Hockenberry 2014). In England, providers in the acute sector are not reimbursed for readmissions within 28 days of discharge under the National Tariff Payment System, and based on these results, such a policy may also be pertinent in the mental health care sector if it were to discourage reductions in LOS to such an extent as to have a detrimental impact on quality.
Limitations and Future Research
There are several limitations to this research. The interaction between acute and psychiatric inpatient care can have implications for inpatient psychiatric LOS which we do not take account of in this work. In order to gain a more comprehensive picture of the performance of mental health care providers it is necessary to model the entire care pathway across different settings. The majority of mental health care takes place in community-based settings and inpatient care is usually reserved for crisis stabilisation. Thus, by focusing on a relatively narrow segment of the care process we may misrepresent the true performance of mental health care providers. Moreover, consideration of the entire care pathway is likely to provide important insights into the interplay of other factors such as the range of outpatient and community-based services received, accommodation status, and crisis planning among others, which could not be considered in this model, but which may influence inpatient LOS. Future analysis using HES linked to the Mental Health Minimum Data Set (MHMDS)—a national–level dataset for specialist mental health care—would allow us to investigate provider performance across the entire care pathway. Our results find an association between reduced LOS and higher emergency readmission rates but we cannot infer a causal relationship. Moreover, while we have highlighted differences in residual variation across providers that we interpret as differences in provider performance, we cannot provide definitive reasons why some providers perform better than others once we account for observable admission-, patient- and provider-level variables. Nevertheless, the identification of providers with above- and below-average performance is in itself a useful exercise as this type of benchmarking highlights potential problems or potential efficiency savings allowing hospitals and regulators to undertake in-depth investigations to address such issues (Schleifer 1985).
Notes
From April 1, 2013 PCTs ceased to exist and were replaced by Clinical Commissioning Groups (CCGs) and local area teams (LATs).
References
Abas, M. A., Vanderpyl, J., & Robinson, E. (2008). Socioeconomic deprivation and extended hospitalization in severe mental disorder: A two-year follow-up study. Psychiatric Services (Washington, D. C.), 59(3), 322–325. doi:10.1176/appi.ps.59.3.322.
Appleby, L., Desai, P. N., Luchins, D. J., Gibbons, R. D., & Hedeker, D. R. (1993). Length of stay and recidivism in schizophrenia: a study of public psychiatric hospital patients. American Journal of Psychiatry, 150(1), 72–76.
Boden, R., Brandt, L., Kieler, H., Andersen, M., & Reutfors, J. (2011). Early non-adherence to medication and other risk factors for rehospitalization in schizophrenia and schizoaffective disorder. Schizophrenia Research, 133(1–3), 36–41. doi:10.1016/j.schres.2011.08.024.
Browne, W. J. (2012). MCMC estimation in MLwiN Version 2.26. Bristol: Centre for Multilevel Modelling University of Bristol.
Bryan, K. (2010). Policies for reducing delayed discharge from hospital. British Medical Bulletin, 95(1), 33–46. doi:10.1093/bmb/ldq020.
Burgess, J. F, Jr, & Hockenberry, J. M. (2014). Can all cause readmission policy improve quality or lower expenditures? A historical perspective on current initiatives. Health Economics, Policy and Law, 9(2), 193–213.
Cameron, C. A., & Trivedi, P. K. (2011). Microeconometrics using Stata (Revised edititon). Texas: Stata Press.
Canadian Institute for Health Information. (2008). Hospital length of stay and readmission for individuals diagnosed with schizophrenia: Are they related?. Ottawa: Canadian Institute for Health Information.
Capdevielle, D., & Ritchie, K. (2008). The long and the short of it: Are shorter periods of hospitalisation beneficial? The British Journal of Psychiatry, 192, 164–165.
Care Quality Commission. (2009). Performance assessment 2008–2009. London: Care Quality Commission.
Care Quality Commission. (2010). 2009 Inpatient survey “Patient experience” performance indicator calculation. London: Care Quality Commission.
Chung, W., Oh, S. M., Suh, T., Lee, Y. M., Oh, B. H., & Yoon, C. W. (2010). Determinants of length of stay for psychiatric inpatients: analysis of a national database covering the entire Korean elderly population. Health Policy, 94(2), 120–128. doi:10.1016/j.healthpol.2009.09.004.
Cookson, R., Laudicella, M., & Li Donni, P. (2013). Does hospital competition harm equity? Evidence from the English National Health Service. J Health Econ, 32(2), 410–422. doi:10.1016/j.jhealeco.2012.11.009.
Dekker, J., Peen, J., Goris, A., Heijnen, H., & Kwakman, H. (1997). Social deprivation and psychiatric admission rates in Amsterdam. Social Psychiatry and Psychiatric Epidemiology, 32(8), 485–492.
Department of Health and Human Services Agency for Healthcare Research and Quality. (2002). Guide to inpatient quality indicators: Quality of care in hospitals—volume, mortality, and utilisation. Washington, D.C.: Department of Health and Human Services Agency for Healthcare Research and Quality.
Department of Health Payment by Results Team. (2012). A simple guide to payment by results. Leeds: Department of Health.
Durbin, J., Lin, E., Layne, C., & Teed, M. (2007). Is readmission a valid indicator of the quality of inpatient psychiatric care? The Journal of Behavioral Health Services and Research, 34(2), 137–150. doi:10.1007/s11414-007-9055-5.
Figueroa, R., Harman, J., & Engberg, J. (2004). Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatric Services (Washington, D. C.), 55(5), 560–565.
Goldstein, H. (1989). Restricted unbiased iterative generalized least-squares estimation. Biometrika, 76(3), 622–623. doi:10.1093/biomet/76.3.622.
Goldstein, H., & Healy, M. J. R. (1995). The graphical presentation of a collection of means. Journal of the Royal Statistical Society. Series A (Statistics in Society), 158(1), 175–177.
Health and Social Care Information Centre. (2011). Emergency readmissions to hospital within 28 days of discharge. Leeds, UK: Health and Social Care Information Centre.
Health and Social Care Information Centre. (2015). Lower layer super output area in NHS Data Dictionary. Leeds, UK: Health and Social Care Information Centre.
Horgan, C., & Jencks, S. F. (1987). Research on psychiatric classification and payment systems. Medical Care, 87(25), 22–36.
Huntley, D. A., Cho, D. W., Christman, J., & Csernansky, J. G. (1998). Predicting length of stay in an acute psychiatric hospital. Psychiatric Services (Washington, D. C.), 49(8), 1049–1053.
Imai, H., Hosomi, J., Nakao, H., Tsukino, H., Katoh, T., Itoh, T., & Yoshida, T. (2005). Characteristics of psychiatric hospitals associated with length of stay in Japan. Health Policy, 74(2), 115–121. doi:10.1016/j.healthpol.2004.12.018.
Jacobs, R. (2014). Payment by results for mental health services: Economic considerations of case-mix funding. Advances in Psychiatric Treatment, 20, 155–164. doi:10.1192/apt.bp.113.011312.
Korkeila, J. A., Lehtinen, V., Tuori, T., & Helenius, H. (1998). Frequently hospitalised psychiatric patients: A study of predictive factors. Social Psychiatry and Psychiatric Epidemiology, 33(11), 528–534.
Lakhani, A., Coles, J., Eayres, D., Spence, C., & Sanderson, C. (2005). Creative use of existing clinical and health outcomes data to assess NHS performance in England: Part 2—More challenging aspects of monitoring. BMJ, 330, 1486–1492.
Laudicella, M., Li Donni, P., & Smith, P. C. (2013). Hospital readmission rates: Signal of failure or success? Journal of Health Economics, 32(5), 909–921. doi:10.1016/j.jhealeco.2013.06.004.
Leckie, G. (2013). Module 12: cross-classified multilevel models LEMMA (learning environment for multilevel methodology and applications). Bristol: Centre for Multilevel Modelling, University of Bristol.
Leckie, G., & Charlton, C. (2012). runmlwin: A program to run the MLwiN multilevel modeling software from within Stata. Journal of Statistical Software, 52(11), 1–40.
Lin, H. C., Tian, W. H., Chen, C. S., Liu, T. C., Tsai, S. Y., & Lee, H. C. (2006). The association between readmission rates and length of stay for schizophrenia: a 3-year population-based study. Schizophrenia Research, 83(2–3), 211–214. doi:10.1016/j.schres.2006.01.012.
Martin, S., & Smith, P. (1996). Explaining variations in inpatient length of stay in the National Health Service. Journal of Health Economics, 15(3), 279–304.
Mason, A., & Goddard, M. (2009). Payment by results in mental health: a review of the international literature and an economic assessment of the approach in the English NHS. CHE Research Paper 50.
Mason, A., Goddard, M., Myers, L., & Verzulli, R. (2011). Navigating uncharted waters? How international experience can inform the funding of mental health care in England. Journal of Mental Health, 20(3), 234–248. doi:10.3109/09638237.2011.562261.
McCrone, P., & Lorusso, P. (1999). A comparison of psychiatric casemix in the UK and Italy. Social Psychiatry and Psychiatric Epidemiology, 34(8), 432–436.
Noble, M., McLennan, D., Wilkinson, K., Whitworth, A., Barnes, H., & Dibben, C. (2008). The English Indices of Deprivation 2007. London: Communities and Local Government.
OECD. (2013). Health Statistics 2013. Paris: OECD Publishing.
Padgett, D. K., Patrick, C., Burns, B. J., & Schlesinger, H. J. (1994). Ethnic differences in use of inpatient mental health services by blacks, whites, and Hispanics in a national insured population. Health Services Research, 29(2), 135–153.
Pertile, R., Donisi, V., Grigoletti, L., Angelozzi, A., Zamengo, G., Zulian, G., & Amaddeo, F. (2011). DRGs and other patient-, service- and area-level factors influencing length of stay in acute psychiatric wards: the Veneto Region experience. Social Psychiatry and Psychiatric Epidemiology, 46(7), 651–660. doi:10.1007/s00127-010-0231-1.
Rabash, J., Charlton, C., Browne, W. J., Healy, M., & Cameron, B. (2009). MLwiN Version 2.1. Bristol: Centre for Multilevel Modelling: University of Bristol.
Rothbard, A. B., & Schinnar, A. P. (1996). Community determinants of psychiatric hospitalization and length of stay. Socio-Economic Planning Sciences, 30(1), 27–38. doi:10.1016/0038-0121(95)00023-2.
Sanchez-Santos, M. T., Mesa-Frias, M., Choi, M., Nuesch, E., Asunsolo-Del Barco, A., Amuzu, A., & Casas, J. P. (2013). Area-level deprivation and overall and cause-specific mortality: 12 years’ observation on British women and systematic review of prospective studies. PLoS One, 8(9), e72656. doi:10.1371/journal.pone.0072656.
Schleifer, A. (1985). A theory of yardstick competition. RAND Journal of Economics, 16(3), 319–327.
Skrondal, A., & Rabe-Hesketh, S. (2009). Prediction in multilevel generalized linear models. Journal of the Royal Statistical Society, 172, 659–687.
StataCorp LP. (2014). Stata 13.0. College Station, Texas: StataCorp LP.
Steele, F. (2008). Module 5: Introduction to multilevel modelling concepts LEMMA (learning environment for multilevel models and applications). Bristol: Centre for Multilevel Modelling, University of Bristol.
Sytema, S., Burgess, P., & Tansella, M. (2002). Does community care decrease length of stay and risk of rehospitalization in new patients with schizophrenic disorders? A comparative case register study in Groningen, the Netherlands; Victoria, Australia; and South-Verona, Italy. Schizophrenia Bulletin, 28(2), 273–281.
Tulloch, A. D., Fearon, P., & David, A. S. (2011). Length of stay of general psychiatric inpatients in the United States: systematic review. Administration and Policy in Mental Health, 38(3), 155–168. doi:10.1007/s10488-010-0310-3.
Acknowledgments
An earlier version of this paper was presented at the meeting of the Health Economists Study Group, 8-10 January 2014, Sheffield, UK. We would like to thank Søren Rud Kristensen and session participants for their comments. We would like to thank participants at the Health Econometrics and Data Group seminar at the University of York, 19th June 2013, for feedback. We are also grateful to two anonymous referees for very helpful comments. Hospital Episode Statistics (HES) are Copyright ©1998/1999–2012/2013, re-used with the permission of The Health & Social Care Information Centre. All rights reserved.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s10488-016-0720-y.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Moran, V., Jacobs, R. & Mason, A. Variations in Performance of Mental Health Providers in the English NHS: An Analysis of the Relationship Between Readmission Rates and Length-of-Stay. Adm Policy Ment Health 44, 188–200 (2017). https://doi.org/10.1007/s10488-015-0711-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-015-0711-4