Abstract
Purpose
This study has the objective of assessing the psychiatric rehospitalization experience of a large cohort of persons with schizophrenia and modeling the effects of personal and systemic conditions on rehospitalization risk.
Methods
The study employs a secondary analysis of US data from Massachusetts’ casemix database of all patients discharged from acute general hospital units. It focuses on 11,291 patients during 1994–2000 who were discharged from acute adult psychiatric units. Predictors used include basic demographics, length of stay, continuity of care with doctors and facilities, diagnoses, discharge referral, type of insurance, and distance to and selected socioeconomic characteristics of the patient’s home zip code. Data are analyzed with descriptive statistics and modeled with the Cox proportional hazard model. The model was assessed through split-half reliability testing, the generalized R2, and Harrell’s Concordance Index.
Results
Overall, 13.4% of patients were rehospitalized within 1 month; 38.9% within 1 year; and 64.1% within 5 years. Predictors that are most strongly associated with lower rehospitalization rates include continuity of care, discharge to a chronic hospital, and density of home zipcode, whereas discharge to another acute psychiatric unit had the greatest effect on increasing risk of rehospitalization. Overall the Cox model has generalized R2 of 0.343 and a Concordance Index of 0.734.
Conclusions
The results highlight the need to enhance the continuity of the relationships with providers, whether these are with the assigned psychiatrists or other therapists and case managers, as well as workplace issues involving staff turnover and hospital assignment and admitting policies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The deinstitutionalization of inpatient psychiatric care has been an ongoing and contentious issue, one with multiple dimensions [1]. As these policies are pursued and hospitalization levels are minimized, rehospitalization following failures in community mental health placements has grown in importance. One of the groups most affected are those with schizophrenia who are known to be among the most disabled with some of the highest rehospitalization rates [2]. Although the rehospitalization experience of persons with schizophrenia has been widely researched, the results of these studies, with some exceptions, have not been cumulative. This is due to a remarkable diversity of definitions, samples, predictor and outcome variables, and analytical techniques used. These include the virtual absence of reports of statistics on the goodness-of-fit and predictability of models estimated, thus, preventing adequate assessment and comparison across studies. This study, thus, aims to address several of these problems in an examination of the rehospitalization experience of persons with schizophrenia over a 5-year period in a major US state.
Understanding and predicting rehospitalization are needed for both direct practice as well as planning and policy development. Determination of discharge readiness and discharge service plans requires an assessment of the risks for future relapse. Assessment of need for future hospitalization also has implications for the allocation of resources both for inpatient and community mental health services. These include the determination of the types and intensity of community services that are needed for patients to be discharged. In addition, strategies for linking hospital and community services are also dependent on the level of rehospitalization risk.
Background
Research on psychiatric rehospitalization in general has been remarkably varied in respect to the samples studied, the sets of outcome measures and predictors tested, analytical procedures, and the inclusion of interventions and other manipulable variables. Thus, results have varied dramatically as well. For this reason, it is not possible to either statistically aggregate these findings in a meta-analysis, nor even in a systematic review. However, an examination of 16 key studies published since 1990 on the rehospitalization of persons specifically with schizophrenia or schizoaffective conditions illustrates the methodological diversity employed, as well as an identification of several emerging themes in the results of this body of research.
The samples employed in prior research derive from a variety of national contexts, most notably Australia [3, 4], China [5], Denmark [6, 7], Germany [8,9,10], Japan [11], New Zealand [12], the UK [13,14,15], and the US [16], and include several studies [17, 18] that involve multi-national comparisons. Samples are of two types, those based on national or state registers, and those based on discharges from hospitals or clinics, typically, a single hospital or its outpatient clinic, but in a few cases, up to three. Whereas the case register studies included substantial samples of between 451 and 25,913 discharges, the samples from hospital and clinic studies typically ranged between 44 and 382 patients. Most of the hospital studies employed only availability sampling; however in a few cases, case control and matching procedures were used to facilitate comparisons between those with usual versus alternative treatments. In most cases no specific interventions were tested; however, occasionally follow-up programs such as an integrated treatment program were compared with standard medication follow-up [9], or in some other studies, alternative psychotropics were compared [5, 12].
In respect to outcomes, most of this research has examined the occurrence of rehospitalization within one or more time frames, most commonly 2 or 5 years, and in the case of national registers, sometimes over as long as 20 years [17]. These and other studies sometimes also included total or percent of time rehospitalized, number of rehospitalizations, as well ratings and scores from various psychopathological, lifestyle, and functioning scales. In one report, the time frame of rehospitalization was not specified [11].
Most of the research consisted of retrospective naturalistic studies, either employing secondary analyses, or newly collected data in the case of some of the single-facility studies. Although a minority of these studies were restricted to describing rehospitalization rates, most also sought to uncover the relative contributions of various demographic, clinical, family, and treatment variables. In addition to basic demographics, variables examined include age of initial onset, treatment compliance, and various indicators of severity such as previous hospitalizations. Other clinical variables and scales included measures of life skills, cognition, insight, and social functioning. In a few, the compulsory or voluntary nature of the index hospitalization was examined [10]. Overlap between studies of the sets of variables has been minimal, except in the case of basic demographics such as age, sex, marital status, and the like.
Only about half of the studies employed Cox regression, designed for modeling time to event data, such as time from discharge to rehospitalization, a proxy for relapse. However, none of these reported any goodness-of-fit or overall predictability indices such as any adaptation of R2 or the Concordance Index (CI). A substantial minority employed logistic regression which ignores the problem of censored data of those who remain free of the event of interest (rehospitalization) by the time of data analysis. Individual studies sometimes employed procedures such as multiple regression, basic descriptive statistics, and in one case, Classification Analysis Regression Tree (CART) was used [8]. In general, the research has been undermined by serious methodological limitations such as the failure in the smaller studies, particularly those with a single institution, to consider rehospitalizations in other institutions, leading to underestimates of the levels of rehospitalization.
Given the range of methodologies described here, it is not surprising that these studies have few results in common. When descriptive statistics on actual rehospitalization levels have been reported, they are often in the range of 43–50% for 1 year of follow-up; 49–58% for 2 years, and 50–82% within a 5-year period. Regarding the overall rehospitalization experience, a few of the longer-term multi-national studies [18] identified patterns of progressive amelioration, that is, decreasing numbers and lengths of hospitalizations as the years of the illness have progressed. Frequently, measures of condition severity, including young age of onset, poor insight [19], lack of treatment adherence, and compulsory hospitalization have been found to be associated with shorter follow-up periods free of rehospitalization [2]. However, attempts to model the collective effects of various risk factors on rehospitalization of those with schizophrenia has met with only limited success due partly to the low levels of variation explained, when such statistics are even reported. For this reason, this study employs not only a procedure specifically designed for modeling time to event data, Cox regression, but also considers the overall goodness-of-fit of the estimated model. Specifically, this study aims to answer the following questions:
-
1.
What are the levels of rehospitalization of persons with schizophrenia, both in general and among selected subgroups?
-
2.
What are the relative contributions that key personal and systemic conditions contribute to the level of risk of rehospitalization?
-
3.
What is the overall predictability for hospitalization that can be accounted for by known individual and systemic risk factors?
Methodology
This project employs a secondary analysis with data from the US Massachusetts Case Mix hospitalization data base. Massachusetts state regulations (114.1 CMR 17.00) mandate that each acute hospital provide state-designated data items on each discharge, including patient demographics, diagnoses, costs, insurance, utilization, measures of severity, meeting defined standards.
This is a state-wide register of episode level records for all patients who have been hospitalized in general hospitals, and is maintained by the Massachusetts Center for Health Information and Analysis. The specific data used in this project was a subset of records for all individuals with a primary or secondary diagnosis of schizophrenia who were hospitalized between 1994 and 2000 in any of the 45 general hospital acute psychiatric units in the state. Each of these episode records is linked together using an encrypted social security number, known as the Uniform Health Identifier Number (UHIN), that permits the de-duplication of these records to the level of the individual patient and thus, their anonymous tracking over the period of the project.
Sample
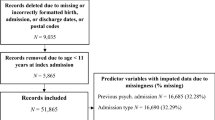
The primary sample consists of 11,291 patients, with one or more hospitalizations, who received an International Code of Diagnosis 9 (ICD-9) diagnostic code of schizophrenia, including the various subtypes (simple, disorganized, catatonic, schizoaffective, schizophreniform, latent, other, and unspecified) within the 295 code during the 1994–2000 period. Key demographics and other characteristics of the sample are summarized in Table 1. This file was randomly split into two files to permit split-half reliability testing for the model computed.
This sample was selected from the case mix data base records for 1994–2000 which included 5.2 million episode records for 1.8 million individuals. Of these episodes, 467,056 were treated on psychiatric units, and 444,993 or 95.3% of these had valid UHIN numbers required for the examination of rehospitalization, 53,119 of which were associated with a diagnosis of schizophrenia. These episodes represented 11,418 distinct individuals, out of which 11,291 or 98.9% were selected for inclusion in this study. Those rejected included those who died, or otherwise had incomplete data. The selected predictors included only those with substantially complete data, thus, no special treatment of missing data was required.
Variables and their measurement
Predictors were selected from those available in the case mix database and which were reported from prior research to be associated with psychiatric rehospitalization. The initial list of potential variables was then reduced further as a result of preliminary bivariate analyses and initial iterations of the Cox algorithm. These variables include those pertinent to patient demographics and diagnosis; distance to their home communities (zipcode) and its socioeconomic characteristics; and type of treatment. Demographic predictors include race, age, and sex. Diagnoses available from the Massachusetts case mix database include both primary and secondary ICD-9 co-morbid psychiatric diagnoses dichotomously recorded (1/0) for selected three-digit ICD-9 psychiatric diagnoses. Distance in miles to home zip code, as a measure of geospatial service access, was derived by computing the straight-line Euclidian distance between the centroids of the hospital and home zip codes. Socioeconomic status of the home community was based on STF-3C data from the 2000 US census on the educational, occupational, and income profile of the home zip code, and this is presented in detail in an earlier published study by the author [20].
Service variables include mean length of stay, time to next psychiatric hospitalization, prior medical (non-psychiatric) hospitalizations, and proportion of changes in facility and doctor over the course of recorded hospitalizations as measures of service continuity. These two continuity indices were defined and computed as the proportion of the total episodes for the patient for which a subsequent hospital episode involved a repeated doctor or facility. In the case of those with only one psychiatric episode, the mean index value of all cases with multiple episodes was used, in lieu of case deletion, as an interpolated projection to minimize the loss of valid cases. For descriptive purposes, these indices are recoded as dichotomous variables in Table 2; however, they are retained as continuous indices for the purposes of the Cox regression analysis.
Data reliability
Analyses of administrative data are often confronted with questions about data reliability, especially when such data are obtained through multiple sources. In this case, several studies have been conducted, both by the author and by the Massachusetts Center for Health Information and Analysis, which provide evidence of the data’s reliability in crucial areas. The reliability of the data on age, sex, and race was assessed by this researcher through an analysis of the consistency of these fields across multiple hospitalizations of the same individuals. These analyses demonstrated very high levels of reliability or interrater agreement among the three separate doctors for a subgroup of patients with at least three hospitalizations within any 3-month time span. Agreement about sex, age, and racial affiliation was all very high, 0.93 or above [21]. A parallel procedure was used to examine agreement between separate facilities as to patients’ diagnoses. Substantial reliability, using the Kappa index, was found for schizophrenia (0.74), and moderately strong reliabilities were found for affective disorders (0.54), adjustment reaction (0.48), and alcohol dependence (0.59). Although there have been serious criticisms of psychiatric diagnostic systems such as the ICD-9 [22], other studies have found good levels of reliability [23].
Analysis and modeling
Initial data preparation of the database involved the transfer and definition of the seven annual files and variable transformations, as well as the merging, re-sorting, and selection of relevant psychiatric cases. Psychiatric cases were identified by the placement of an individual on a regular psychiatric or a psychiatric intensive care unit. Sequence variables of only psychiatric admissions were then initially computed for each individual year. All of the files were then merged into a master file of 5.2 million records and re-sorted, and a new overall sequence variable for psychiatric admissions was computed using lag transformations. Other lag variables were created, such as days between successive stays, which included data from the same patients over the 7 years studied. After a dataset of 11,291 individuals with a diagnosis of schizophrenia was selected from all records of patients with an initial hospitalization on a psychiatric unit (see “Sample”), transformations of the various indices used were finalized. This included computation of the continuity of facility and doctor indices, distance from home zipcode to hospital, number of previous medical hospitalizations, and a standardized index of the socioeconomic status of the home zipcode, based on income, mean education, and occupational profile of the home zipcode (see “Variables and their measurement”).
Descriptive statistics for 1 month, 1 year, and 5-year rehospitalization rates were computed, based on all the subsets of patients who had periods of at least 1 month, 1 year, and 5-year remaining in the period of the dataset’s coverage. These were also computed for the categories of selected predictors.
Modeling the relative effect of the various predictors was completed with Cox regression, using SPSS Version 24.0. This procedure assumes independence of survival times, constant hazard ratios over time, and a multiplicative relationship between the predictors and the hazard (schizophrenia). Selected diagnostics were examined, for instance, survival curves based on key predictors. The primary dependent variable is the number of days from discharge from the patient’s index or first recorded hospitalization for schizophrenia until subsequent psychiatric hospitalization within the Massachusetts system of general hospitals. A separate variable used in the Cox procedure records whether or not such a subsequent hospitalization actually occurred (1—yes/0—no). Since the database did not include VA hospitals or those out of state, estimates of rehospitalization reported here can be expected to error on the low side. If there was no subsequent hospitalization, the case was coded as a ‘0’, otherwise, ‘1’ flagged the event of rehospitalization. In total, 5559 or 49.2% of the cases had no subsequent rehospitalization within the system of care examined. Non-significant predictors were deleted and a final model recomputed. Validation was completed on a split-half basis, with the developmental model computed on a randomly selected half of the data, and the same model recomputed on the remaining half of the data. In addition, Harrell’s Concordance Index (equivalent to the AUC, area-under-the-curve index) [24, 25] was computed for both the development and testing subsets of the dataset with a macro supplied by IBM-SPSS’s technical assistance, and the Generalized R2 was computed [24, 25], also with both subsets of the data, with the following formula on an Excel Spreadsheet: R2 = 1 − E (− LLR null − LLR fitted)/n).
Results
A key question of this study (#1) involves the levels of rehospitalization of persons with schizophrenia, both in general, and among selected subgroups. Table 2 summarizes these results for three typically used time frames: 1 month, 1 year, and 5 years from initial recorded hospitalization. Overall, over an eighth or 13.4% of the patients were rehospitalized within 1 month of their discharge. Within 1 year, this rate approaches two-fifths or 38.9%, and within 5 years, it exceeds five-eighths or 64.1%. These aggregate rehospitalization rates take into account only those patients for whom the period of follow-up was at least these specified periods. It also excludes any rehospitalizations in acute units within the Veteran’s Administration system, or outside of Massachusetts.
There are, however, statistically significant variations in the rates of rehospitalization depending on several of the predictors examined, ones that in general become more pronounced the longer the follow-up period examined. Most disparate are differences based on whether patients had continuity of care indices in the upper or lower halves of the patients. At the 5-year point, patients with relatively high continuity of assigned doctors had low rehospitalization rates (35.9%), whereas almost all those with low continuity were rehospitalized (97.1%). Similarly, 55.0% of those with high continuity of facilities were rehospitalized within 5 years, compared with 95.6% for those with low continuity. Less pronounced but statistically significant, is some of the differences based on length of initial stay, race, age, and co-morbid diagnoses involving affective, alcohol, and drug-dependence conditions. For example, those with short initial stays of seven or fewer days were rehospitalized 39.1% of the time within 1 year, and 66.1%, within 5 years, compared with patients with 15 or more days who were rehospitalized 35.8% within 1 year and 59.9% of the time within 5 years. Also, patients who had either an ‘other’ or a ‘black’ designation for race had relatively low rehospitalization rates at the 5-year mark; those with affective, alcohol, or drug-dependence comorbidities had elevated rehospitalization rates at the 5 years mark; and those under 18 or over 65 had relatively low 5-year rehospitalization rates. The remaining predictors involving gender, number of prior medical hospitalizations, type of hospital (community vs. university), and SES of home zipcode did not display any statistically significant disparities in rehospitalization rates, although in some cases, differences were suggestive of possible effects.
The foregoing rates essentially represent the zero-order associations of the various predictors with the rehospitalization event and are not controlled or adjusted for alternative explanations or predictors. For this reason, this study estimated a multivariate Cox regression model to answer the remaining two questions, involving the relative contributions of key personal and systemic conditions, and the overall predictability of rehospitalization that can be accounted for by the available predictors (questions #2 and #3). The results of the estimated Cox model are summarized in Table 3. Many of the statistically significant effects uncovered here involve predictors that serve to minimize risk of rehospitalization. Most noteworthy is that of continuity of doctors seen over the hospitalization experience. For each standard deviation increase in such continuity, there is a 1.424 standard deviation decrease in rehospitalization risk. This is also the case with continuity of facilities for which the size of the standardized effect is also large (B = − 0.699). A large effect (B = − 0.900) was also observed for population density of the patient’s home zip code in suppressing the risk of rehospitalization. Also statistically significant is the tendency for those discharged to a rehabilitation hospital to be rehospitalized less frequently (B = − 0.475), as well as those sent to a specialty mental health facility (B = − 0.341). Other predictors served to increase the possibility of return to a psychiatric unit, particularly discharge or transfer to another short-term or acute hospital unit (B = 0.802). Statistically significant effects were also observed for the presence of a personality disorder (B = 0.197), receipt of public insurance (B = 0.143) and the number of previous medical hospitalizations (B = 0.069), all of which had modest effects in increasing the possibility of psychiatric rehospitalization. Each of these effects, whether they diminished or increased the possibility of rehospitalization, is controlled or adjusted for the roles of each of the other predictors that were included in the final model reported here.
The final question of the study (#3) involving the overall predictability of the set of predictors considered is addressed by the various indices of goodness-of-fit and predictability reported in Table 3. The entire set of predictors accounts for just over a third of the variation in rehospitalization risk, both in the development (R2 = 0.343; p < 0.001) and the testing subsets of the data (R2 = 0.350; p < 0.001). The predictability of the estimated model was similarly found to be at a moderate level, with a Harrell’s concordance C of 0.734 for the development, and 0.740 for the testing subsets of the data. Thus, a statistically significant, though far from completely predictive model has been estimated based on the available predictors. It should be noted that a number of possible predictors were tested, but none of these contributed to a significant extent to the final model (see note in Table 3).
Discussion
The results of this study reveal that the rehospitalization rates for persons with schizophrenia in Massachusetts are comparable with those in other studies, particularly the 5-year rate which was found in this study to be 64%, compared with the range of 50–82% from the prior body of research. The data demonstrate that although these rates are substantial, the mean number of hospitalizations of 2.81 during the 7 years suggests that the characterization of the ‘revolving door syndrome’ may be accurate only for a particularly disabled subgroup of this population, some of whom have had as many as 86 rehospitalizations. One of the most significant findings of this study is the powerful effect that continuity of care, on both the levels of the assigned doctor and the institution, has on minimizing relapse. It should be noted that this analysis does not permit specific conclusions about the causal nature of such predictors, in part because the continuity indices used in this study are based on the entire recorded period of a patient’s psychiatric hospitalizations. Nonetheless, continuity of care can be interpreted as both existing partly prior to and as a concurrent characteristic of the pattern of psychiatric care, most likely in an ongoing interaction.
It is well known that persons with schizophrenia have substantial difficulties in maintaining relationships, thus, it is not unexpected that the highest rehospitalization rates should be associated with low service continuity. To what extent do characteristics of the assigned therapist and institution, including training, personality, supports, administrative policies and practices, and other workforce issues, aggravate this pattern cannot be concluded from this data; however, it would seem likely that they contribute significantly. And the extent to which the breakdown of such relationships is a cause or consequence of relapse and rehospitalization is an open question. The high staff turnover rates no doubt contribute to a fragmentation of the helping relationship.
A similar pattern is revealed by this model when the outcome or discharge disposition is considered as a predictor of rehospitalization. Whereas referral to home health, a specialty mental health program, IV drug therapy, or a chronic hospital all contribute to a minimization of rehospitalization, referral to another short-term or acute psychiatric unit has a dramatic effect in aggravating the risk of rehospitalization. Whether such a transfer is requested or demanded of the patient, such a dramatic break in the immediate treatment continuity contributes substantially to further relapse and rehospitalization.
Other contributors to rehospitalization risk, such as comorbidities involving substance abuse and poor socioeconomic conditions in the home neighborhoods, are not unexpected. However, that rehospitalization risk is diminished by higher population densities of the home address may be counter-intuitive given the known tendency for such environments to aggravate the course of schizophrenia. One alternative explanation is that fewer community supports may be available in less dense communities, particularly those in rural areas.
One strength of this study is that it confirms that it is possible to account for a moderate degree of the variability in the rehospitalization rates of persons with schizophrenia and to predict likelihood of relapse. However, an important limitation is that the model leaves unexplained about two-thirds of the variance in such experience, no doubt due to some combination of unmeasured biological, psychosocial, and socio-cultural and policy conditions, as well as personal choices, chance, and measurement error. For example, the extent that community mental health services and resources are utilized after the initial hospitalization would no doubt contribute explanatory power to such a model, but unfortunately, information on such services (other than the outcome or discharge of the hospitalization episode) is not available in the casemix database that was used. Additional future research is needed which combines data from such administrative case registers with clinical data, over extended periods of time. Long-term research on psychiatric recovery suggests that time frames of 10–20 years or longer may be needed for those considered to be seriously and persistently mentally ill. In addition, studies focused on patterns of service delivery are needed, rather than simply on rehospitalization.
Perhaps one of the most important implications of the current results is the need for additional attention to the challenge of maintaining the continuity of the relationships with providers, whether these are the assigned psychiatrists or other therapists and case managers. This will require addressing a wide variety of problems, including staff turnover, staff assignment policies, and hospital and medical policies that lead to discontinuation of prior service relationships when a patient is rehospitalized.
References
Hudson CG (2016) A model of deinstitutionalization of psychiatric care across 161 nations. Int J Ment Health 45(2):135–153
Emsley R, Chiliza B, Schoeman (2008) Predictors of long-term outcome in schizophrenia. Curr Opin Psychiatry 21:173–177
Parker G, Hadzi-Pavlovic D (1995) The capacity of a measure of disability (the LSP) to predict hospital readmission in those with schizophrenia. Psychol Med 25(1):157–163
Daniels BA, Kirby KC, Hay DA, Mowry BJ et al (1998) Predictability of rehospitalisation over 5 years for schizophrenia, bipolar disorder and depression. Australas Psychiatry 32(2):281–286
Lin CH, Lin SC, Chen MC et al (2006) Comparison of time to rehospitalization among schizophrenic patients discharged on typical antipsychotics, clozapine or risperidone. J Chin Med Assoc JCMA 69(6):264–269
Munk-Jorgensen P, Mortensen P, Machon RA (1991) Hospitalization patterns in schizophrenia. A 13-year follow-up. Schizophr Res 4(1):1–9
Morgensen PB, Eaton WW (1994) Predictors for readmission risk in schizophrenia. Psychol Med 24:223–232
Doering S, Muller E, Kopcke W et al (1998) Predictors of relapse and rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Bull 24(1):87–98
Schmidt-Kraepelin C, Janssen B, Gaebel W (2009) Prevention of rehospitalization in schizophrenia: results of an integrated care project in Germany. Arch Psychiatry Clin Neurosci 259(Suppl 2):S205–S212
Pfiffner C, Steinert T, Kilian R et al (2014) Rehospitalization risk of former voluntary and involuntary patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 49:1719–1727
Suzuki Y, Yasumura S, Fukao A et al (2003) Associated factors of rehospitalization among schizophrenic patients. Psychiatry Clin Neurosci 57(6):555–561
Dey S, Menkes DB, Obertova Z, Chauduri S et al (2016) Correlates of rehospitalisation in schizophrenia. Australas Psychiatry 24(4):356–359
Cole JD, Kazarian SS (1992) Predictive validity of the level of expressed emotion (LEE) scale: readmission follow-up data for 1, 2, and 5-year periods. J Clin Psychol 49(2):216–218
Soni SD, Gaskell K, Reed P (1994) Factors affecting rehospitalisation rates of chronic schizophrenic patients living in the community. Schizophr Res 12:169–177
Geddes J, Mercer G, Frith CD et al (2014) Prediction of outcome following a first episode of schizophrenia. A follow-up study of Northwick Park first episode study subjects. Br J Psychiatry 165(5):664–668
Robinson D, Woerner MG, Alvir JMJ et al (1999) Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry 56(3):241
Eaton WW, Mortensen PB, Herrman H et al (1992) Long-term course of hospitalization for schizophrenia: part I. Risk for rehospitalization. Schizophr Bull 18(2):217–228
Eaton WW, Mortensen PB, Herrman H et al (1992) Long-term course of hospitalization for schizophrenia: part II. Change with passage of time. Schizophr Bull 18(2):217–228
Lincoln TM, Lullmann E, Rief W (2007) Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull 33:1324–1342
Hudson CG (2005) Patterns of psychiatric hospitalization in Massachusetts, 1994–2000. Admin Policy Ment Health 32(3):223–242
Hudson CG, Dorwart DR, Wieman DA (1998) The impact of a Medicaid behavioral carve-out program on patterns of acute psychiatric hospitalization: The Massachusetts experience, FY 1996–FY 1997. Center for Applied Research and Development, Salem State University, Salem
Kendell R, Jablensky A (2003) Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry 160(1):4–12
Okasha A, Sadek A, Al-Haddad et al (1993) Diagnostic agreement in psychology; a comparison study between ICD-9, ICD-10, and DSM-III-R. Br J Psychiatry 162:621–626
Harrell FE, Califf RM, Pryor DB et al (1982) Evaluating the yield of medical tests. J Am Med Assoc 247:2543–2546
Wang X, Jiang B, Liu JS (2017) Generalized R-squared for detecting dependence. Biometrika 104(1):129–139
Acknowledgements
Supported by Grant from Office of Academic Affairs, Salem State University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Hudson, C.G. Five-year rehospitalization experience of a state-wide cohort of persons with schizophrenia. Soc Psychiatry Psychiatr Epidemiol 54, 861–870 (2019). https://doi.org/10.1007/s00127-018-1650-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-018-1650-7