Abstract
Biomedical HIV prevention uptake has not taken hold among Black and Latinx populations who use street-marketed drugs. A pilot intervention providing a PEP informational video and direct pharmacy access to a PEP starter dose was conducted among this population. Four study pharmacies were selected to help facilitate syringe customer recruitment (2012–2016). Baseline, post-video, and 3-month ACASI captured demographic, risk behavior, and psychosocial factors associated with PEP willingness, and willingness to access PEP in a pharmacy. A non-experimental study design revealed baseline PEP willingness to be associated with PEP awareness, health insurance, being female, and having a high-risk partner (n = 454). Three-month PEP willingness was associated with lower HIV stigma (APR = 0.95). Using a pre-post approach, PEP knowledge (p < 0.001) and willingness (p < 0.001) increased overtime; however, only three participants requested PEP during the study. In-depth interviews (n = 15) identified lack of a deeper understanding of PEP, and contextualized perceptions of HIV risk as PEP access barriers. Pharmacy PEP access shows promise but further research on perceived risk and HIV stigma is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biomedical HIV prevention for occupational exposure has been available for nearly three decades. Post-exposure prophylaxis (PEP) has been proven effective in preventing HIV after sexual and needle-related exposures in animal [1, 2] and human studies [3,4,5,6] and consists of a HIV medications prescribed for daily use, over 28-days, and initiated within 72 h of exposure for best efficacy [7,8,9]. PEP efficacy trials, conducted mostly among men who have sex with men (MSM), have reported effectiveness in preventing HIV infection even in cases with less than 100% adherence [4,5,6], and have shown to be a cost-effective HIV prevention method [10, 11] with no evidence of increased high risk behavior [6, 12, 13]. In 2012, the U.S. Food and Drug Administration approved the first use of a daily antiretroviral drug to prevent HIV infection as pre-exposure prophylaxis (PrEP) among persons at high risk for HIV. A recent review noted that both continuous and intermittent PrEP use demonstrated high efficacy in preventing HIV seroconversion among heterosexual women, heterosexual HIV-discordant couples, and persons who inject drugs; however, most notable efficacy was observed among MSM [14,15,16,17,18]. While both biomedical HIV prevention strategies are available, the majority of uptake in the U.S. is among MSM and data among other high-risk groups, such as persons who are heavily drug-involved remain sparse.
In this report, data from a large-scale, sequential explanatory mixed methods study of PEP awareness, willingness to use PEP, and barriers to actual uptake of PEP in New York City (NYC) neighborhoods heavily burdened with drug use are presented. To increase PEP availability and uptake among persons who use drugs (PWUD), a pre-post pilot intervention study that offered direct pharmacy access to PEP, following a 10-min content PEP education video was completed in 2016. This was the next step in exploring an expanded public health role of pharmacists, given past success of pharmacies serving as safe syringe access sites through non-prescriptions syringe sales [19], and as rapid HIV testing sites [20]. Sociodemographic, psychosocial, and risk behavior characteristics associated with (1) willingness to take PEP, and (2) willingness to initiate PEP directly from a pharmacy among PWUD was investigated. In addition, change in PEP knowledge and PEP willingness, over time was examined using a non-experimental observational analytic approach. Lastly, to provide deeper insight for our quantitative results, we qualitatively assessed the reasons for not requesting PEP after a self-reported high-risk event.
Methods
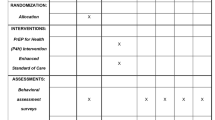
Between 2012 and 2016, we implemented the iPEPcare study (PEP Community Access Reaching Everyone), a pre-post pilot intervention that included a content video describing PEP, and subsequent access to a 10-day PEP “starter dose” obtained directly from a pharmacy, followed by a clinic visit during the week of PEP initiation. Four pharmacies registered with the NYS Expanded Syringe Access program (ESAP), a program allowing syringe sales without a prescription, were selected as study venues. Pharmacy selection was based on location in a low-income Upper Manhattan or South Bronx neighborhood, strong pharmacy staff willingness to participate, on-site space allowing for confidential conversations, and sufficient syringe customer volume to enroll into the study [21].
Participant Recruitment
Pharmacy staff were trained to engage and schedule appointments for interested syringe customers. Targeted street outreach was also employed which included street-outreach in the surrounding pharmacy areas, and display of study posters in iPEPcare pharmacies and surrounding community-based organizations. Eligibility included ≥ 18 years of age; self-reported heroin, crack or cocaine use (in the past three months); and any accompanying peer of a syringe customer regardless of drug use history.
Qualitative interviews were conducted at the three-month follow-up visit among a purposive sample defined as study participants who did not request PEP and self-reported receptive syringe sharing or unprotected vaginal or anal sex with a high-risk partner defined as MSM, a history of transactional sex, and/or a history of injection drug use, or crack cocaine use. Among 51 participants who met this criterion, 15 were randomly selected and underwent an in-depth interview as study follow-up progressed.
Data Collection
All study activities took place in a private partitioned area of a study pharmacy. At enrollment, participants underwent informed consent and collection of contact information for follow-up reminders. Next, a baseline audio computer assisted self-interview (ACASI) was administered, followed by a 10-min vignette-based PEP educational video which included a description of the iPEPcare study (available in English and Spanish). Using social cognitive theory as a framework for video development, content and script design was developed iteratively by the study team and community partners, using actors representing the sociocultural fabric of the community with respect to language and dialogue, attire, and scenery/situations [22]. There were three scenes depicting what PEP is and how, when and why PEP should be used. Immediately post-video, participants repeated a brief ACASI to ascertain PEP knowledge and willingness to take PEP, underwent rapid HIV testing, and were given a 3-month follow-up appointment. Participants with an injection drug use history also underwent rapid HCV testing at baseline. At follow-up, those eligible and interested in undergoing an in-depth interview were also interviewed for 30 min and audio-recorded in the private partitioned pharmacy area. At the end of each study visit, research staff provided study participants with a PEP education pamphlet which included what, why, and when PEP should be requested and mapped locations of the study pharmacies where PEP could be requested. Questions and concerns were also addressed in a respectful and non-judgmental fashion.
PEP Request Protocol
Following the baseline visit, confirmed HIV-negative study participants were eligible to receive PEP at any point until study end. At the end of each visit, study participants were verbally instructed and given written materials on how PEP could be directly accessed through the study. Study staff emphasized arriving to the pharmacy immediately following potential exposure and not to exceed 72 h following the potential exposure event. For a PEP request, pharmacy staff called the research staff to come to the pharmacy to conduct a rapid HIV test to confirm HIV negative status, and for female participants, a urine sample was collected for a pregnancy test to confirm non-pregnant status. If HIV-negative, not pregnant, and deemed eligible based on timing of potential HIV exposure event, the study physician was called to conduct a phone risk assessment and prescribe a 10-day “starter dose”. Participants were also given three follow-up clinic appointments: within 2–5 days, 14 days later, and 28-days later to monitor parameters (complete blood count, liver function tests, creatinine and creatinine clearance for renal function) and assess tolerance and adherence.
Measures
Dependent Variables
The primary pre-post outcome measures were: (1) willingness to take PEP, and (2) willingness to initiate PEP directly from a pharmacy. Outcomes were ascertained at 3 time-points, baseline prior to viewing the iPEPcare video and receiving information about direct pharmacy PEP access (pre-video), post-video, and 3-month follow-up. Outcomes were based on the following questions: “Would you be willing to take medications to prevent HIV infection after unprotected sex, sharing syringes, or being accidentally stuck by a needle? This medication consists of taking 2–3 pills every day once or twice a day for 28 straight days.” “Would you be willing to come to this pharmacy to see if you can start HIV prevention medications after a recent possible exposure to HIV?”.
Independent Variables
Exposure variables of interest were sociodemographic variables and included age, gender (male, female), race/ethnicity (Latinx, Black, White/other), education level (< high school vs. ≥ high school or equivalent), income from legal means (≤ $5000 vs. > $5000, past year), health insurance status (yes vs. no, past 3 months), current homelessness (yes vs. no, past 3 months), history of incarceration (yes vs. no), and sexual orientation (identify as homosexual, lesbian, bisexual, heterosexual, other or self-reported same sex partner type). Sex and drug use risk behavior variables (past 3 months) included unprotected vaginal or anal sex (proportion of total number of sex acts where condoms were used; always vs. not), transactional sex (sex for money, drugs or other needs/wants; yes vs. no), type of drugs used (heroin, crack, cocaine, speedball, methamphetamines daily, 2–3 times per week, once per week, once a month or less), and route of administration (snort, smoke, inject). A binary high-risk sexual network variable was created and defined as reporting at least one of the following partner types: history of injection drug use, history of crack cocaine use, history of transactional sex, or MSM. Psychosocial variables included externalized HIV stigma [23] (9-item scale of anticipated HIV shame and blame, overall index ranging 1–9), and depressive symptomology [24] (experiencing depressive symptoms most or all the time, past year; yes vs. no). Also included were PEP awareness (Have you ever heard of people trying to prevent HIV by taking medications right after being accidentally stuck by a needle while working/being on the job, for example, nurses, doctors, EMTs, janitors, sanitation workers? yes vs. no), and accurate PEP knowledge (post-video and 3-month follow-up only) defined as correctly answering each of the following four questions: (1) How soon after you’ve potentially been exposed to HIV should you come in to ask for PEP? (2) If someone starts PEP, do they have to go to follow-up appointments with a doctor? (3) If someone starts PEP, do they have to take the medications every day for 28 days? And (4) Under what circumstances should someone take PEP? [correctly circling three criteria].
Data Analysis
The quantitative analyses were restricted to HIV-negative participants (n = 454). Descriptive statistics were calculated overall and stratified by each outcome (willingness to take PEP, and willingness to initiate PEP from pharmacies) over time (post-video, and 3-month follow-up). Sociodemographic, psychosocial, and risk behavior characteristics of those willing to take PEP, and of those willing to initiate directly at a pharmacy were compared at each time point using chi-squared tests of association. Only key variables of interest, or those characteristics found to be associated with PEP willingness outcome measures via chi-squared test of association, were included in regression analysis. For each outcome, logistic regression analysis was used to obtain prevalence ratio estimates of the adjusted association between our PEP willingness outcome and key variables of interest. McNemar’s tests identified changes in PEP willingness and knowledge over time [pre-video (baseline), post-video, and 3-month]. All statistical analyses were conducted using SAS 9.3.
The qualitative analysis included transcripts of 15 participants which were read in their entirety twice by one of the authors (H-M L). The first time, to become familiar with how participants discussed their experiences and to engage in open coding, and the second time to selectively code for reasons why participants did not access PEP at the pharmacy. The emerging codes and sub-codes were applied to the transcripts and were reviewed by a second researcher that had not been involved with the study for reliability. Finalized codes and sub-codes were applied to the transcripts.
Results
Baseline sociodemographics, behavioral risks, PEP awareness, and PEP willingness outcomes are shown in Table 1. Of the 454 HIV-negative individuals enrolled, median age was 45 years, most were male (68%), Hispanic/Latino (56%), income ≤ $5000 (71.8%), health insurance (84%), and identified as heterosexual (85%). About one-third had less than a high school diploma or equivalent (36%) and were recently homeless (36%). Two-thirds (67%) reported recent heroin, crack, and/or cocaine use, and 32% recently injected drugs. Half reported unprotected sex (53%), and most reported a high-risk sexual partnership (62%). A large majority reported depressive symptomatology (69%), and a low level of perceived HIV stigma. Finally, while 34% of participants reported awareness of PEP, fewer reported accurate PEP knowledge including what, why, and when to use PEP (9%).
Table 2 depicts sociodemographic, behavioral risk, and psychosocial characteristics associated with each PEP willingness outcome at each survey time-point. At baseline (pre-video time-point), factors associated with willingness to take PEP included female gender (75.7% vs. 63.1%; p < 0.01), health insurance status (71.3% vs. 51.4%; p < 0.01), recent transactional sex (82.9% vs. 65.6%; p < 0.05), not having an MSM sex partner (65.9% vs. 4.0%; p < 0.01), PEP awareness (88.1% vs. 61.1%; p < 0.01) and 100% knowledge of PEP (97.1% vs. 64.8%; p < 0.01). At baseline, willingness to access PEP directly from a pharmacy was associated with health insurance status (79.3% vs. 60.6%; p < 0.01), having a sex partner with a history of crack use (83.5% vs. 73.2%; p < 0.05) and/or a high risk sex partner (82.4% vs. 72.6%; p < 0.05), PEP awareness (84.3% vs. 73.7%; p < 0.05), and 100% knowledge of PEP (91.2% vs. 73.5%; p < 0.05). At the post-video time-point, willingness to take PEP was associated with health insurance status (97.1% vs. 88.9%; p < 0.01), 100% PEP knowledge (96.9% vs. 91.6%; p < 0.05) and a low HIV stigma score (0 vs. 1; p < 0.05). No correlates were associated with willingness to initiate PEP in a pharmacy at post-video. Among the 78% of participants retained and who underwent a 3-month follow-up survey (n = 356), factors associated with willingness to take PEP included higher educational level (93.1% vs. 83.9%; p < 0.01), recent injection drug use (95.1% vs. 88.0%; p < 0.05), 100% PEP knowledge at post-video (91.8% vs. 83.3%; p < 0.05), and a low HIV stigma score (0 vs. 1; p < 0.05). Factors associated with willingness to initiate PEP in a pharmacy at 3-months included male gender (91.3% vs. 96.9%; p < 0.05), and a low HIV stigma score (0 vs. 1; p < 0.05).
Final adjusted models for correlates of PEP willingness outcomes at each time-point are provided in Table 3 and included bivariate associations that sustained after adjustment. At the baseline, PEP awareness (Adjusted Prevalence Ratio [APR] = 1.35; 95% Confidence Interval [CI] I 1.23–1.49), female gender (APR = 1.13; 95% CI 1.03–1.24), and health insurance status (APR = 1.24; 95% CI 1.01–1.53) independently predicted willingness to take PEP. Health insurance status (APR = 1.27; 95% CI 1.05–1.53), having a high-risk sex partner (APR = 1.14; 95% CI 1.04–1.25), and PEP awareness (APR = 1.12; 95% CI 1.02–1.24) independently predicted willingness to initiate PEP directly from a pharmacy. While no significant independent associations surfaced for either PEP willingness outcome at post-video, at 3-month follow-up, a low HIV stigma score significantly predicted PEP willingness (APR = 0.95; 95% CI 0.91–0.98), after adjustment.
Table 4 provides depicts increased and sustained PEP awareness, knowledge, and willingness over time. Individual questions regarding how often PEP should be taken, how soon PEP should be initiated, and need for clinical follow-up were assessed prior to viewing the video with correct answers ranging from 18 to 23.6%, and only 9% answering all three questions correctly. Immediately following the video, proportions increased significantly for each measure with correct answers ranging from 93.5 to 99.5%, and 78.8% correctly answering all three questions (p < 0.0001). These high proportions modestly decreased at 3-months (88.2–92.7%, and 68.8% correctly answering all three questions) and significant differences were observed when comparing pre-video vs. 3-month follow-up with respect to the proportion of participants reporting PEP knowledge (9.5% vs. 65.5%; p < 0.001).
Finally, only a few participants actually visited a study pharmacy to request PEP during the study period (n = 3), and only two of these individuals were eligible: one male did not complete the protocol because he entered a drug treatment facility and chose to drop out of the study; one female initially requested PEP when she found out a recent sex partner was HIV+ and never returned for her first clinical follow-up and asked to drop out of the study; and one male who requested PEP but was HIV+ .
Qualitative Results
When participants undergoing in-depth interviews were asked why they did not access PEP at the pharmacy following a high-risk behavioral event, most indicated they did not think about it or forgot it was an option. However, after deeper inquiry, four overarching themes emerged: (1) a range of PEP knowledge and understanding, (2) the importance of being able to categorize PEP as a form of treatment versus prophylaxis, (3) the role of the local perceptions and the context of the potential HIV risk exposure, and (4) willingness to take PEP and, specifically at a pharmacy.
Theme 1: PEP Knowledge and Understanding
Most participants revealed a basic understanding of PEP as a means of HIV prevention. A few had a complete understanding of PEP including specific features of the pharmacy-based PEP protocol. However, some felt they may have missed the window of opportunity to take PEP for it to be effective. For instance, one participant explained, “I’ve heard of a pill that you take if possibly exposed to the virus but I don’t know the name of it was or how long you had to take it, or the time period to start taking it… It (PEP) didn’t even come to mind until after two days. Then I was like, wait a minute, then I couldn’t remember if it was one day.” A few participants had accurate and complete knowledge of PEP and the pharmacy protocol. As one participant stated, “…if you think you’ve come in contact with a person that is diseased, go to your pharmacy and speak to your pharmacist… they will have you on a 28-day medication. That will let you know, help you, at least prevent from catching HIV.” This participant had recently referred a friend to a study pharmacy for PEP. Another participant also indicated that he knew how and when PEP should be used, “PEP is a pill they give you; you have to take it for a month… There’s another pill that she (physician) mentioned, it’s a pill you take before having unprotected sex… Yes (PrEP), she explained it all to me and I keep it in mind. Besides, I have all the brochures and I read them, and also search the internet.” Taking into consideration the different levels of PEP knowledge, two analytic themes surfaced as possible explanations for not accessing PEP when knowledge of PEP appeared to be high.
Theme 2: PEP—A Preventive or a Therapeutic Method?
The need for a deeper understanding of how PEP operates, including safety, were discussed by most participants. As one participant debated: “Yeah, you would take the medication and that would be it. It wouldn’t cause you to get HIV, it works if you have HIV and if you don’t have HIV it does not do anything… There’s no dangerous effect, that’s what I (am asking).” And, another participant asked: “Now, what is the outcome of using PEP? Does it just let me know that I can be HIV positive or does it eliminate the HIV from entering my system and me staying HIV positive?”.
Theme 3: Local Perceptions of HIV Risk and Prevention
In discussions of how and when participants could have been potentially exposed to HIV, participant definitions of what constituted HIV risk differed from the promoted public health definition of HIV risk. Based on their experiences of extensive drug use (e.g., injecting multiple times a day, sharing syringes) and engagement in high-risk sexual behavior (e.g., having multiple sex partners, or engaging in transactional sex), most participants did not consider having condomless sex with partners outside the sex trade or sporadically sharing needles as high risk behavior that would warrant PEP. Most reported frequent HIV testing and/or remaining seronegative over their lifetime and this minimized self-perception of risk. For instance, one participant indicated: “For starters, I was an intravenous user, which I am no longer. The way I used to prevent (HIV) was having my own syringes, my own cookers, and my own cotton. I protect myself while having sex, I wouldn’t put myself at risk with women that was selling their bodies… I pretty much prevented myself with knowing who is [HIV] positive and who is not.” He also tested regularly for HIV and remained negative. A similar risk account was provided by someone in a drug treatment program. “I’m not gonna sit here and tell that every time I had sex it was protected but obviously, I would tell you a lie, but the majority of the times that I do have sex it was with a condom.” [# 110] He added that “…the person I have had unprotected sex was someone I knew for a long time … from what I know (she is HIV negative).”
Finally, some participants who were still using drugs perceived HIV risk as secondary to the need to get high and avoiding withdrawal symptoms revealing another local definition of risk. For instance, a participant stated, “At one point when I was like strung out there, you get careless, you know. You just worry about that, ‘get high’ you don’t want to be sick, so you’re like, ‘fuck it’ (share a) cooker. Let me just get this shit.” Another participant weighing the HIV risk event against their drug use explained, “… they are so caught up in getting their fix… Usually when you are getting high you obviously don’t care about your health because… Because if you don’t get your medicine (drug) you’re sick…”.
Theme 4: Willingness to Take PEP and Access it at the Pharmacy
It is noteworthy that nearly all participants expressed willingness to take PEP if they were exposed to HIV. Neither the pharmacy setting, nor the 28-day duration of PEP were deterrents. For instance, one participant said: “…I would be willing to do that (take a pill for 28-days), yea, yea and now actually, that kinda makes sense.” Another participant addressed stigma in accessing PEP at the pharmacy by saying, “I’m not ashamed, if I’m exposed, I will go (to the pharmacy), it’s my health.” Furthermore, one participant indicated, “Oh that’s the first step I would go through. God forbid, if I ever were to put myself in that predicament like that, PEP would be my first step.” This participant had also referred a friend to a study pharmacy after disclosing he had condomless sex with a female partner who disclosed she was HIV seropositive.
Discussion
This pilot intervention study revealed key sociodemographic, behavioral and psychosocial characteristics associated with the PEP willingness in the event of a potential HIV exposure, either willingness in general or directly accessed from a pharmacy. While being female, PEP awareness, and having a high-risk sexual partner were independent correlates of PEP willingness at baseline (either in general or directly from a pharmacy), these demographic effects diminished over time, and perceived HIV stigma remained the only independent predictor of PEP willingness at 3-months. Overall accurate recounts of PEP knowledge post-video to follow-up remained high over time. However, actual PEP uptake was not realized with only a few participants requesting PEP during the study period. In-depth assessment of reasons for not requesting PEP after a high-risk event revealed two key barriers: (1) lack of a more complete understanding of PEP, and (2) contextualized perceptions of risk that negated need for PEP. While the PEP video (the main intervention component coupled with direct pharmacy access) was associated with increased PEP knowledge that sustained at a fairly high level, survey data revealed a modest decrease at follow-up. This PEP knowledge decrease aligned with the qualitative findings which revealed a need for a more comprehensive understanding of PEP which underscored the inability the PEP educational video to contend with perception of risk.
Several key findings in this report warrant attention in the biomedical prevention discussion. First, among this high-risk study sample, a high proportion of PEP willingness was observed however, this expressed “willingness” did not translate into “action”. The qualitative data provided some explanation for this decision to not access PEP. For example, while someone may have selected the correct multiple choice answer on what, why, and when to initiate PEP during the quantitative survey, the opportunity to discuss how PEP worked during the qualitative interview exposed a lack of complete PEP understanding and/or confusion regarding whether PEP should be used for prevention or treatment. Such uncertainty may have undermined PEP uptake by potentially dampening motivation to access PEP. While a “booster” session that provided a clear and detailed explanation of how PEP acts in one’s body to prevent HIV infection would have been helpful (prior to 3-months), the qualitative data suggests that those who understood the use of PEP either did not perceive themselves to be at risk following a high-risk event or behavior or felt this was “a risk worth taking” and decided to forego the PEP request. These in-depth interviews highlighted how HIV risk is contextualized and how the meaning of “high risk” may vary by individual history and by community. For example, the heuristic that a familiar sexual partner is safe and thought to be HIV-negative would be considered faulty from a public health practitioner perspective. This perception of risk “in context” could play a fundamental role in the uptake of biomedical HIV prevention strategies and warrants exploration.
HIV stigma, which measured anticipated HIV shame and blame, surfaced in both survey and qualitative assessments and warrants heightened attention. While developing intervention strategies that contend with the disconnect between local contextualized perception of risk and risk as defined by public health practitioners, HIV-related stigma continues to surface as a barrier to uptake of HIV prevention and treatment strategies.
In sum, while further investigations are needed to understand the disconnect between willingness and action for increased PEP uptake, this study did offer preliminary evidence that supports use of pharmacies as sites providing direct access to PEP, and specifically the onsite viewing of a PEP educational video. Facilitating PEP access which included directly connecting the participant with a clinician during the pharmacy visit appeared to resonate with a higher risk group, at least initially. Interestingly, over time, higher risk behavior did not distinguish willingness to take PEP, for either outcome. This may indicate that the effect of the video was equalized across varying levels of risk, over time, however further research is needed to confirm this explanation.
Limitations
It is important to mention the following study limitations. First, self-reports of sensitive attitudes and behaviors may have resulted in underreporting. However, several reports have validated self-reported sex and drug use behavior [25, 26]. Second, the potential for selection bias exists given our community-based recruitment strategies and therefore, findings may not be representative of all PWUD in majority Black and Latinx, urban settings. Yet, our findings are corroborated by the extant literature reflecting low PEP uptake and offer insight into the current state of biomedical prevention uptake. Finally, the lack of a control group limited the ability to determine intervention effectiveness, but this quasi-experimental study provided strong support for more robust intervention research that contends with HIV stigma, and perceived HIV risk.
Conclusions
Preliminary evidence of an increase in PEP knowledge and awareness after viewing a brief PEP educational video coincided with sustained willingness to access PEP over time, and specifically from a pharmacy. However, those who were not willing to access PEP, were more likely to report HIV stigma. Further, willingness to access PEP did not translate into actual PEP requests. Contextualized perception of low HIV risk emerged qualitatively as a possible explanation for lack of PEP uptake. Biomedical HIV prevention research building on these data is needed and should consider addressing HIV stigma, and the structural context within which risk is defined.
References
Otten RA, Smith DK, Adams DR, et al. Efficacy of postexposure prophylaxis after intravaginal exposure of pig-tailed macaques to a human-derived retrovirus (human immunodeficiency virus type 2). J Virol. 2000;74(20):9771–5.
Tsai CC, Emau P, Follis KE, et al. Effectiveness of postinoculation (R)-9-(2-phosphonylmethoxypropyl) adenine treatment for prevention of persistent simian immunodeficiency virus SIVmne infection depends critically on timing of initiation and duration of treatment. J Virol. 1998;72(5):4265–73.
Cardo DM, Culver DH, Ciesielski CA, et al. A case–control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. N Engl J Med. 1997;337(21):1485–1490. https://doi.org/10.1056/NEJM199711203372101
Kahn JO, Martin JN, Roland ME, et al. Feasibility of postexposure prophylaxis (PEP) against human immunodeficiency virus infection after sexual or injection drug use exposure: the San Francisco PEP Study. J Infect Dis. 2001;183(5):707–14. https://doi.org/10.1086/318829
Landovitz RJ, Fletcher JB, Inzhakova G, Lake JE, Shoptaw S, Reback CJ. A novel combination HIV prevention strategy: post-exposure prophylaxis with contingency management for substance abuse treatment among methamphetamine-using men who have sex with men. AIDS Patient Care STDS. 2012;26(6):320–8. https://doi.org/10.1089/apc.2011.0432
Schechter M, do Lago RF, Mendelsohn AB, Moreira RI, Moulton LH, Harrison LH. Behavioral impact, acceptability, and HIV incidence among homosexual men with access to postexposure chemoprophylaxis for HIV. J Acquir Immune Defic Syndr. 2004;35(5):519–525.
Bailey AC, Fisher M. Current use of antiretroviral treatment. Br Med Bull. 2008;87:175–92. https://doi.org/10.1093/bmb/ldn032
Panlilio AL, Cardo DM, Grohskopf LA, Heneine W, Ross CS. Updated U.S. Public Health Service guidelines for the management of occupational exposures to HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2005;54(RR-9):1–17.
Smith DK, Grohskopf LA, Black RJ, et al. Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposure to HIV in the United States: recommendations from the U.S. Department of Health and Human Services. MMWR Recomm Rep. 2005;54(RR-2):1–20.
Pinkerton SD, Martin JN, Roland ME, Katz MH, Coates TJ, Kahn JO. Cost-effectiveness of postexposure prophylaxis after sexual or injection-drug exposure to human immunodeficiency virus. Arch Intern Med. 2004;164(1):46–544. https://doi.org/10.1001/archinte.164.1.46
Pinkerton SD, Martin JN, Roland ME, Katz MH, Coates TJ, Kahn JO. Cost-effectiveness of HIV postexposure prophylaxis following sexual or injection drug exposure in 96 metropolitan areas in the United States. AIDS. 2004;18(15):2065–73.
Donnell D, Mimiaga MJ, Mayer K, Chesney M, Koblin B, Coates T. Use of non-occupational post-exposure prophylaxis does not lead to an increase in high risk sex behaviors in men who have sex with men participating in the EXPLORE trial. AIDS Behav. 2010;14(5):1182–9. https://doi.org/10.1007/s10461-010-9712-1
Martin JN, Roland ME, Neilands TB, et al. Use of postexposure prophylaxis against HIV infection following sexual exposure does not lead to increases in high-risk behavior. AIDS. 2004;18(5):787–92.
García-Lerma JG, Cong M, Mitchell J, et al. Intermittent prophylaxis with oral truvada protects macaques from rectal SHIV infection. Sci Transl Med. 2010;2(14):14ra4. https://doi.org/10.1126/scitranslmed.3000391
Radzio J, Aung W, Holder A, et al. Prevention of vaginal SHIV transmission in macaques by a coitally-dependent truvada regimen. Ambrose Z, ed. PLoS ONE. 2012;7(12):e50632. https://doi.org/10.1371/journal.pone.0050632
Curtis KA, Kennedy MS, Luckay A, et al. Delayed maturation of antibody avidity but not seroconversion in Rhesus Macaques infected with simian HIV during oral pre-exposure prophylaxis. JAIDS J Acquir Immune Defic Syndr. 2011;57(5):355–62. https://doi.org/10.1097/QAI.0b013e3182234a51
Tsai CC, Follis KE, Sabo A, et al. Prevention of SIV infection in macaques by (R)-9-(2-phosphonylmethoxypropyl)adenine. Science. 1995;270(5239):1197–9. https://doi.org/10.1126/SCIENCE.270.5239.1197
Grant RM. Antiretroviral agents used by HIV-uninfected persons for prevention: pre- and postexposure prophylaxis. Clin Infect Dis. 2010;50(s3):S96–101. https://doi.org/10.1086/651479
Fuller CM, Galea S, Blaney S, et al. Explaining the relationship between race/ethnicity and pharmacy purchased syringes among injection drug users in New York City. Ethn Dis. 2004;14(4):589–96.
Amesty S, Crawford ND, Nandi V, et al. Evaluation of pharmacy-based HIV testing in a high-risk New York City Community. AIDS Patient Care STDS. 2015;29(8):437–44. https://doi.org/10.1089/apc.2015.0017.
Crawford ND, Amesty S, Rivera AV, Harripersaud K, Turner A, Fuller CM. Randomized, community-based pharmacy intervention to expand services beyond sale of sterile syringes to injection drug users in pharmacies in New York City. Am J Public Health. 2013;103(9):1579–82. https://doi.org/10.2105/AJPH.2012.301178
Crawford ND, Rudolph AE, Jones K, Fuller C. Differences in Self-reported discrimination by primary type of drug used among New York City drug users. Am J Drug Alcohol Abuse. 2012;38(6):588–92. https://doi.org/10.3109/00952990.2012.673664
Friedland BA, Sprague L, Nyblade L, et al. Measuring intersecting stigma among key populations living with HIV: implementing the people living with HIV Stigma Index 2.0. J Int AIDS Soc. 2018. https://doi.org/10.1002/jia2.25131
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association; 2013. https://doi.org/10.1176/appi.books.9780890425596
Anthony J, Vlahov D, Celentano D, et al. Self-report interview data for a study of HIV-1 infection among intravenous drug users: description of methods and preliminary evidence on validity. J Drug Issues. 1991;21(4):739.
Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51(3):253–63.
Acknowledgements
We would like to thank the study participants for sharing their experiences, and the study staff for their hard work. This research was sponsored by the National Institute on Drug Abuse, R01DA030253. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the funders.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lewis, C.F., Lekas, HM., Rivera, A. et al. Pharmacy PEP Access Intervention Among Persons Who Use Drugs in New York City: iPEPcare Study—Rethinking Biomedical HIV Prevention Strategies. AIDS Behav 24, 2101–2111 (2020). https://doi.org/10.1007/s10461-019-02775-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02775-3