Abstract
This study reports the feasibility, acceptability, and preliminary efficacy of the bio-behavioral community-friendly health recovery program—an integrated, HIV prevention intervention to improve pre-exposure prophylaxis (PrEP) adherence and HIV-risk reduction behaviors among high-risk people who use drugs. We used a within-subjects, pretest–posttest follow-up design to recruit participants, who were HIV-uninfected, methadone-maintained and reported HIV-risk behaviors and had initiated PrEP (n = 40; males: 55%). Participants were assessed at baseline (T0), immediately post-intervention (4 weeks: T4) and 4 weeks post-intervention (T8). Immediately after completing the four weekly intervention groups, participants underwent a post-intervention assessment including in-depth qualitative interviews. Feasibility was high, assessed by participant willingness to enroll (90.1%) and retention (95%). Results showed that participants were highly satisfied and perceived the intervention as valuable and acceptable [mean: 81.3 (range 0–100)]. Significant enhancements in self-reported PrEP adherence [F(2,74) = 7.500, p = 0.001] and PrEP-related knowledge [F(2,74) = 3.828, p = 0.026] were observed. Drug-related (e.g., injection of drugs, sharing of injection equipment) and sex-related (e.g., number of sexual partners, condomless sex) risk behaviors were reduced, while information, motivation, and behavioral skills (IMB) constructs increased. The results support feasibility and high acceptability and support further examination of the efficacy of this combination bio-behavioral intervention in a prospective clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While advances in HIV treatment have transformed the management of HIV among people living with HIV, similar progress has not been achieved in primary HIV prevention. People who use drugs (PWUD), in particular, have a disproportionate burden of HIV due to their engagement in preventable drug- and sex-related risk behaviors [1,2,3,4,5]. Moreover, a recent increase in opioid overdose rate has raised significant challenges to HIV prevention efforts as opioid use disorders (OUD) are consistently associated with HIV transmission [6]. Existing methods of HIV prevention for PWUD include approaches used across populations to reduce sexual transmission as well as approaches specific to PWUD to reduce HIV transmission through sharing of injection equipment [7]. These strategies, however, have not been sufficiently effective in reducing the incidence of HIV among PWUD [8,9,10], thus emphasizing the need for enhanced primary prevention approaches aimed at more effectively and efficiently preventing HIV among PWUD.
As such, pre-exposure prophylaxis (PrEP) represents an important innovation in evidence-based HIV prevention efforts and a key component of HIV-related public health initiatives. In order to expand access to and uptake of PrEP, the Centers for Disease Control and Prevention (CDC) issued clinical guidance on daily PrEP use for key risk populations, including for PWUD [11], who remain a critical conduit for HIV transmission. The scale-up of PrEP to date, however, is nearly absent among even very high risk PWUD, despite being ideal candidates and expressing strong willingness to use PrEP [12,13,14,15]. Issues surrounding adherence to PrEP and increased risk compensation represent formidable challenges to the implementation of PrEP among PWUD [16], particularly if it is rolled out as a mainstream primary HIV prevention strategy [17].
The advancements in biomedical approaches (e.g., PrEP) to reduce HIV transmission, and the growing consensus that neither biomedical nor behavioral interventions alone are sufficient to curb the epidemic has led experts to call for combination approaches to HIV prevention [18, 19]. Such integrated approaches could significantly advance primary prevention science by cost-effectively optimizing the PrEP continuum of care and HIV risk reduction [17, 18]. An integrated strategy is especially important when intervening with PWUD with neurocognitive impairment (NCI), which characterizes many PWUD [12, 20,21,22,23,24], due to the potential decreased effectiveness from PrEP when adherence is suboptimal, thereby necessitating behavioral interventions that focus on both reducing HIV risk and increasing adherence to PrEP.
The bio-behavioral community-friendly health recovery program (CHRP-BB) is an innovative combination approach that we developed in an effort to fill the significant void in primary HIV prevention for high risk PWUD (described later) [16]. We used a data-driven approach to integrate the biomedical component (i.e., PrEP) into the evidence-based Community-friendly Health Recovery Program (CHRP) [25]—a brief primary HIV prevention behavioral intervention for high risk PWUD based on the information-motivation-behavioral skills (IMB) model of behavioral change [26]. Here, we report on our initial evaluation of the CHRP-BB intervention, which we designed to promote PrEP adherence and HIV risk reduction among high risk PWUD. The current study aimed to: (1) determine the feasibility of recruiting, enrolling, and retaining high risk, HIV-negative PWUD in the CHRP-BB intervention; (2) evaluate the acceptability of the CHRP-BB intervention; and (3) assess the efficacy of the CHRP-BB intervention among high risk, HIV-negative PWUD.
Methods
Study Design, Setting, and Participants
We used a within-subjects, pre/test-post/test follow-up design to recruit 40 participants between September 2016 and July 2017. Participants were recruited from an inner-city methadone maintenance program (MMP) if they (i) were age 18 years or older, (ii) were confirmed HIV-negative, (iii) had recently started taking PrEP (in the past 30 days), (iv) reported drug- or sex-related HIV risk behaviors in the past 6 months; (v) owned a cell phone; (vi) met DSM-5 criteria for OUD and enrolled in MMP; and (vii) were able to understand, speak, and read English. Participants were assessed at baseline (T0), immediately post-intervention (4 weeks: T4) and at 1-month post-intervention (T8).
Procedures
Recruitment involved distribution of flyers at the community-based MMP in Connecticut with instructions to contact research staff directly to indicate their interest. Interested individuals were then screened for eligibility and, if eligible, were referred for additional screening (i.e., PrEP eligibility [11]) by an onsite primary care physician who either prescribed or referred participants to community providers to prescribe PrEP. Those who initiated PrEP were fully enrolled in the study and provided informed consent prior to completing the baseline assessment. Upon completing the baseline assessment, participants were scheduled to attend the intervention sessions in addition to receiving standard drug treatment care, which includes daily methadone and case management consisting of a minimum of 1-hour of monthly contact with a case manager. Immediately after completing the four weekly intervention groups, participants underwent a post-intervention assessment including an in-depth qualitative interview. A follow-up assessment was then conducted 4 weeks after the intervention was completed. Participants were reimbursed in cash for their participation in the study.
The study protocol was approved by the Institutional Review Board at the University of Connecticut and board approval from the MMP.
Intervention
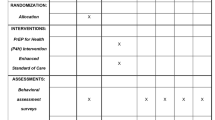
The CHRP-BB is a theory-driven, manual guided intervention comprised of four, 50-min weekly group meetings that address HIV risk behaviors and PrEP adherence among high risk PWUD in treatment (Table 1). The intervention groups were conducted privately by two graduate-level trained facilitators who delivered intervention content using cognitive remediation strategies designed to accommodate the mild to moderate cognitive difficulties that are common among this population [12, 20,21,22,23,24]. Material for each group was delivered using three modalities: verbal (e.g., didactic presentation of material by counselor and group discussion); visual (e.g., slides, videos, handouts, group responses written on flipcharts); and experiential (e.g., behavioral games, demonstrations, practice exercises). In addition to content related to drug- and sex-related HIV-risk reduction, the CHRP-BB intervention incorporated content specific to PrEP, including basics about PrEP, motivation to encourage PrEP use/adherence (e.g., pros and cons of achieving high levels of adherence to PrEP), problem solving skills (e.g., improving strategies for identifying and overcoming obstacles to adherence), facilitators of PrEP adherence (e.g., learning memory aids for improving adherence), enhancing decision-making related to PrEP, and overcoming stigma related to being on PrEP [16]. Additionally, the intervention included a short messaging service (SMS) delivered through text as a mHealth strategy (i.e., text messaging). As such, participants received daily SMS with PrEP reminders timed to coincide with individual-stated dosing preferences [16]. Participants were encouraged to continue taking PrEP as long as their engagement in risk behavior persisted. The manual-guided intervention sessions were audio-taped and rated by a licensed clinical psychologist for interventionists’ competence and adherence to the manual, as in prior trials [25, 27].
Assessments
In addition to demographic and social characteristics, we assessed health insurance status, visits to health care providers in the past 12 months, and current methadone dose. Other measures are described as follows:
Feasibility
Feasibility was assessed throughout the study via process indicators including number screened, eligible (willing to initiate PrEP), enrolled, and retained.
Acceptability
The acceptability of the CHRP-BB intervention was assessed using a series of eight items acceptability rating profile [28]. Participants used a 5-point Likert scale (0 = strongly disagree to 4 = strongly agree) to rate the extent to which they agreed with each acceptability statement (e.g., “This is an acceptable program for individuals who engage in high risk behaviors”, “I would be willing to recommend this program to my friends who may benefit from it.”). The measure was administered at the immediate post-intervention assessment. A mean intervention acceptability score was calculated with higher values indicating greater acceptability. Open-ended questions were asked to participants at T4 to elicit additional feedback about the intervention (Table 2).
Efficacy
PrEP adherence We assessed participants’ adherence to PrEP using a self-reported, three-item scale developed by Wilson et al. [29]. Summary scales were calculated as the mean of the three individual items, with higher score indicating better adherence (0–100) [29].
HIV risk reduction behavior The HIV risk assessment, adapted from NIDA’s risk behavior assessment [30] was used to measure several aspects of HIV risk behaviors in the past 30 days, including a measurement of “any” high risk behavior (sexual or drug-related) as well as measurements of event-level (i.e., partner-by-partner) behaviors.
IMB construct measures Data collection at all assessment points included measures of IMB model constructs [31] including (a) Information—PrEP- and HIV risk-related knowledge; (b) Motivation—readiness to change and intentions to change PrEP adherence and HIV risk behavior; (c) Behavioral skills—PrEP adherence skills and risk reduction skills; and (d) Behavioral outcomes—HIV risk and HIV risk reduction behaviors and PrEP adherence. Behavioral skills were also assessed as in prior controlled trials [32, 33] by having patients demonstrate (a) the specific steps necessary to properly clean a needle/syringe and (b) demonstrate the specific steps to properly select and apply a male and female condom using replicas.
Except for qualitative interviews, all self-report assessments at T0, T4, and T8 were collected using audio computer-assisted self-interview (ACASI). All qualitative interviews were audiotaped (with participants’ permission), and transcribed verbatim.
Data Analyses
All analyses of quantitative data were performed in SPSS version 23.0. Baseline descriptive analysis of the participant characteristics and HIV risk behaviors was conducted. Intervention feasibility is described as the percentage of participants screened, eligible, enrolled, and retained at each assessment point (Fig. 1). Intervention acceptability was based on descriptive statistics from the acceptability measure and qualitative analysis of responses to the open-ended questions. To evaluate changes in intervention outcomes from baseline to 1-month follow-up, we utilized analyses of variance with repeated measures on variables of interest. An intervention effect was defined as improvement in a measured outcome from the pre-intervention to the post-intervention assessment point (p < 0.05).
Analysis of qualitative responses to the intervention acceptability items was conducted using Atlas.ti software. Analysis followed a thematic analysis approach utilizing several qualitative data analysis techniques—including inductive analysis, and cross-case analysis. The primary themes identified formed the basis for the analysis of acceptability of the CHRP-BB intervention.
Results
Feasibility
Figure 1 shows results for screening, recruitment, and retention for the study period. One hundred seventy-three individuals expressed interest in the study and underwent pre-screening by research staff. Among those ineligible, the most common reasons for ineligibility were ‘no HIV risk behavior’ (64.9%) and not interested in taking PrEP (20.7%). Of those eligible in pre-screening, 2 were already on PrEP whereas the other 94 individuals were referred for PrEP assessment. Of those referred, 55 were deemed ineligible [i.e., deemed ineligible by physician (n = 7), lost follow-up (n = 47), no insurance (n = 1)] and 39 individuals were started on PrEP. Forty-one of 94 (43.6%) PWUD with risk behaviors either started or continued PrEP. None of these PWUD refused study participation. Of the total 41 individuals who were on PrEP, 1 individual (one of the two individuals who was already on PrEP) had a scheduling conflict, thus leaving 40 (23.1%) individuals eligible for the study, who completed a baseline assessment. Engagement in the pilot was high, with over 90% of participants completing all four intervention sessions. The rate of completion of follow-up assessments through 1-month post-intervention was also high, with 95% retention at post-intervention and 1-month follow-up. All participants reported to have continued to use PrEP throughout the course of the study.
Participant Characteristics
Participants were mostly in their mid-40s (mean = 44.8; SD = 11.8 years), male (55.0%), White (57.5%), and single (47.5%). Most participants identified as heterosexual (77.5%) and graduated from high school (75.0%). Only 7.5% of the participants reported being currently employed and 77.5% were earning less than $10,000 per year (Table 3).
Acceptability
Our results showed that participants were highly satisfied and perceived the CHRP-BB intervention as valuable and acceptable (α = 0.832). Mean acceptability (range 0–100) for the CHRP-BB intervention was 81.3 (± 12.1), which conveys strong agreement among participants about the value and acceptability of the intervention. Additionally, nearly all participants (95.0%) perceived the intervention as beneficial, especially for addressing high-risk behaviors (e.g., condomless sex, sharing of injection equipment). Similarly, there was high overall satisfaction (97.5%) and a pronounced desire to recommend CHRP-BB to others (97.5%). Additionally, most participants reported that the daily text messages were very helpful to remind them to take PrEP (80.0%) and indicated that they were willing to receive the messages in the future (85.0%).
Post-intervention feedback also indicated that the content delivered in the group sessions, integration of text messaging, and the overall CHRP-BB intervention was helpful in addressing PrEP adherence and HIV risk reduction. Four primary themes emerged during the qualitative assessment, including that: (1) the intervention was perceived as helpful and highly relevant to PrEP adherence issues and HIV risk reduction, (2) the mHealth content was appropriate and timing was not burdensome, (3) the intervention prompted participants to more strongly adhere to PrEP and change their risk behaviors, and (4) the format, content, and delivery of the group sessions was appropriately designed for this risk population. Exemplar participant responses included:
[Intervention] was very relevant. Especially, to be in a place like this [drug treatment setting], which is a high-risk place; it’s a must.
An hour-long session isn’t that bad, especially when you’re learning and practicing so many new things. I really liked the way the group rolled, quiz, and relaxation exercise at the end of each group.
I loved the day-to-day messages that I received from you [Program]. I like how you had different text messages for different days.
Efficacy
Both self-reported PrEP adherence [F(2,74) = 7.500, p = 0.001] and PrEP-related knowledge [F(2,74) = 3.828, p = 0.026] improved significantly and persisted at 1-month post-intervention. Drug-related risk behaviors—including injection of illicit drugs [F(2,72) = 10.283, p < 0.001], sharing of injection equipment [F(2,16) = 9.053, p = 0.002], and sex-related risk behaviors—including number of sexual partners [F(2,30) = 5.075, p = 0.013] were significantly reduced at the end of the intervention and remained reduced at the post-intervention follow-up. Additionally, condom use during sex [F(2,30) = 3.363, p = 0.048] significantly increased at both follow-ups. Significant improvements were also found in HIV risk reduction theoretical (IMB) constructs, including knowledge [F(2,74) = 6.753, p = 0.002], motivation [F(2,74) = 3.225, p = 0.045], and behavioral skills [F(2,74) = 6.476, p = 0.003], as well as demonstrated (objective) HIV risk reduction skills—including needle cleaning [F(2,74) = 56.51, p < 0.001], male condom application [F(2,74) = 66.57, p < 0.001], and female condom application [F(2,74) = 58.46, p < 0.001]—at post and these remained stable at follow-up (Table 4).
Discussion
With growing evidence of the effectiveness of available evidence-based interventions, scaling up of combination HIV prevention approaches has been widely recognized as vital for ensuring progress against the epidemic [18, 19, 34]. Findings from this study demonstrated evidence of feasibility, acceptability, and potential efficacy of the CHRP-BB intervention to optimize primary HIV prevention outcomes among high risk PWUD.
Our findings indicate that PWUD are willing to enroll in and complete the CHRP-BB intervention. It is important to note, however, that despite our extensive recruitment efforts (e.g., community outreach, flexible scheduling, transportation), our recruitment rate was approximately 24%. This recruitment rate is likely due to the challenges of recruiting individuals who meet relatively stringent inclusion criteria (e.g., high risk behavior, PrEP use or willingness to start PrEP). As suggested by the CDC guidelines, the successful identification of appropriate individuals is central to maximize its clinical, public health, and cost benefits [11]. This finding thus reinforces the need for identification of individuals at substantial risk of HIV infection and expanding access to comprehensive PrEP services to those who are interested as a critical component to improve the PrEP care continuum [35].
Additionally, retention was high through the 1-month follow-up visit (> 95%). While it is possible that the higher retention rate could be because of the shorter follow-up time, the overall high retention rates, together with the fact that 90% of participants completed all four intervention sessions, suggests that the intervention has a high degree of feasibility and can be delivered within a common type of drug treatment setting (e.g., MMP) with excellent participant engagement. In the context of MMP, counselors can facilitate engagement and retention of at-risk clients in the intervention through referrals and case management/counseling. Recent studies, however, have shown that many addiction treatment counselors, with whom MMP patients are in daily contact, have limited awareness of PrEP [16, 36]. It is thus important to provide necessary information and skills training to MMP providers at the organization level so that they can facilitate participant engagement and retention just as they would for other services (e.g., HIV testing, referral) relevant to HIV prevention.
Moreover, attitudes toward the program were positive based on both quantitative and qualitative responses. These findings are promising because this is a population at high-risk for HIV and is thus an important target group in terms of potentially benefitting from the intervention. Overall, this pattern of results strengthens the evidence base that CHRP-BB is acceptable among high risk PWUD enrolled in MMP. We note, however, that 20% of participants did not feel positively about the daily text messaging component, one of the components of the CHRP-BB intervention. Potential reasons for this could be perceived breach of privacy, using other reminder strategies (e.g., pill organizer, alarm), preference for coded messages, and lack of interactive messaging since these were 1-way messages [37]. As such, it is important that future work address these concerns to improve the usability of mHealth in HIV prevention.
Analyses further demonstrated the preliminary efficacy of the intervention in terms of improving PrEP adherence and PrEP-related knowledge over time. It appears that the intervention was also successful in reducing HIV transmission risk among this high-risk group and in providing the appropriate information, motivation, and behavioral skills to support and strengthen HIV risk reduction outcomes. The intervention effect also remained durable from post-intervention to the 1-month follow-up point, with the exception of retaining information related to PrEP and HIV risk reduction. This suggest the potential utility of a booster session that reviews the key concepts covered during intervention groups to prevent decay in the initial intervention effects [38]. Furthermore, future implementation of the intervention will require long-term follow-up and surveillance for monitoring adherence, adverse events, drug resistance, and risk compensation. Overall, findings support continued efforts to pursue this innovation to address the HIV-related risk behaviors and PrEP uptake and adherence as experienced by many PWUD in treatment.
Although the results are promising, study limitations must also be noted. First, the preliminary efficacy pilot did not include a control group. Thus, we cannot rule out the possibility that outcomes were influenced by factors extraneous to the intervention. Second, the study included a relatively small sample of participants enrolled in the MMP, which limits our ability to detect the significance of small effects and effects with substantial variability and to generalize the findings to a different risk group (e.g., PWUD not enrolled in MMP). Third, our design included a short-term follow-up, which limits us from determining the durability of the intervention effects. Fourth, while PrEP adherence was high, it is unclear if it was related to the SMS or the behavioral intervention or both. Finally, this study relied solely on self-reported data (e.g., PrEP adherence, drug use, sexual risk behaviors) and results may thus be subject to social desirability bias. Future studies therefore need to utilize more reliable measures (e.g., dried blood spots) in addition to the self-report measure. Regardless of these limitations, we believe that our findings carry important implications for efforts to improve the PrEP continuum of care among high-risk PWUD in the US [39], where PrEP for primary HIV prevention still remains understudied and underutilized.
The magnitude of the problems being addressed—primary HIV prevention—is enormous. As such, information gleaned from this study can have a significant positive impact on the overall HIV epidemic. While the findings of this pilot study will add to the body of knowledge regarding combination approaches for HIV prevention, it has also provided us with a solid empirical foundation to proceed with a larger scale randomized controlled trial (RCT). Given the documented preliminary efficacy of the CHRP-BB intervention to improve adherence to PrEP and HIV risk reduction, this could have a direct and rapid effect in curbing HIV transmission among PWUD. Furthermore, if this intervention approach is successfully implemented in similar drug treatment programs or in the community, the impact could be even greater. This is particularly timely as we are now witnessing an alarming increase in opioid overdose throughout the US and other countries. Additionally, this intervention could be adapted and implemented among other risk groups (e.g., men who have sex with men), and thus has the potential for greater significance.
Conclusions
Overall, the CHRP-BB represents a feasible and acceptable intervention with preliminary efficacy to optimally address PrEP adherence and HIV risk reduction needs of high risk PWUD in substance abuse treatment. The reported outcomes are promising and indicate the benefits of systematically implementing this combination approach to foster PrEP adherence and HIV risk reduction. Future RCTs are warranted to further establish the efficacy of this intervention among high risk groups. Also, adapting this approach to other populations (e.g., racial and ethnic minorities, incarcerated individuals, youth, women), is necessary to determine whether similar results will be found among other priority populations.
References
Arasteh K, Jarlais DCD, Perlis TE. Alcohol and HIV sexual risk behaviors among injection drug users. Drug Alcohol Depend. 2008;95(1):54–61.
Marshall BDL, Friedman SR, Monteiro JFG, Paczkowski M, Tempalski B, Pouget ER, et al. Prevention and treatment produced large decreases in HIV incidence in a model of people who inject drugs. Health Aff. 2014;33(3):401–9.
Noar SM. Behavioral interventions to reduce HIV-related sexual risk behavior: review and synthesis of meta-analytic evidence. AIDS Behav. 2008;12(3):335–53.
Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376(9737):268–84.
Volkow ND, Montaner J. The urgency of providing comprehensive and integrated treatment for substance abusers with HIV. Health Aff (Project Hope). 2011;30(8):1411–9.
Green TC, McGowan SK, Yokell MA, Pouget ER, Rich JD. HIV infection and risk of overdose: a systematic review and meta-analysis. AIDS. 2012;26(4):403.
CDC. Effective interventions: HIV prevention that works. Atlanta: CDC; 2017.
Sadeghi-Najafabadi M. The influence of neurocognitive impairment on hiv risk reduction intervention outcomes among drug dependent methadone-maintained patients. Storrs: University of Connecticut; 2013.
Worley MJ, Tate SR, Brown SA. Mediational relations between 12-step attendance, depression, and substance use in patients with comorbid substance dependence and major depression. Addiction. 2012;107(11):1974–83.
Huedo-Medina TB, Shrestha R, Copenhaver M. Modeling a theory-based approach to examine the influence of neurocognitive impairment on HIV risk reduction behaviors among drug users in treatment. AIDS Behav. 2016;20(8):1646–57.
CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014: a clinical practice guideline. Washington, DC: Department of Health and Human Services USA—Centers for Disease Control and Prevention; 2014.
Shrestha R, Karki P, Altice FL, Huedo-Medina TB, Meyer JP, Madden L, et al. Correlates of willingness to initiate pre-exposure prophylaxis and anticipation of practicing safer drug- and sex-related behaviors among high-risk drug users on methadone treatment. Drug Alcohol Depend. 2017;173:107–16.
Stein M, Thurmond P, Bailey G. Willingness to use HIV pre-exposure prophylaxis among opiate users. AIDS Behav. 2014;18(9):1694–700.
Kuo I, Olsen H, Patrick R, Phillips G II, Magnus M, Opoku J, et al. Willingness to use HIV pre-exposure prophylaxis among community-recruited, older people who inject drugs in Washington, DC. Drug Alcohol Depend. 2016;164:8–13.
Shrestha R, Karki P, Altice F, Dubov O, Fraenkel L, Huedo-Medina T, et al. Measuring acceptability and preferences for implementation of pre-exposure prophylaxis (PrEP) using conjoint analysis: an application to primary HIV prevention among high risk drug users. AIDS Behav. 2017. https://doi.org/10.1007/s10461-017-1851-1.
Shrestha R, Altice F, Karki P, Copenhaver M. Developing an integrated, brief bio-behavioral HIV prevention intervention for high risk drug users in treatment: the process and outcome of formative research. Front Immunol. 2017;8:561.
Brown G, Reeders D, Dowsett GW, Ellard J, Carman M, Hendry N, et al. Investigating combination HIV prevention: isolated interventions or complex system. J Int AIDS Soc. 2015;18(1):20499.
Brown JL, Sales JM, DiClemente RJ. Combination HIV prevention interventions: the potential of integrated behavioral and biomedical approaches. Curr HIV/AIDS Rep. 2014;11(4):363–75.
Buchbinder SP, Liu A. Pre-exposure prophylaxis and the promise of combination prevention approaches. AIDS Behav. 2011;15(1):72–9.
Meade CS, Towe SL, Skalski LM, Robertson KR. Independent effects of HIV infection and cocaine dependence on neurocognitive impairment in a community sample living in the southern United States. Drug Alcohol Depend. 2015;149:128–35.
Potvin S, Stavro K, Rizkallah E, Pelletier J. Cocaine and cognition: a systematic quantitative review. J Addict Med. 2014;8(5):368–76.
Anderson AM, Higgins MK, Ownby RL, Waldrop-Valverde D. Changes in neurocognition and adherence over six months in HIV-infected individuals with cocaine or heroin dependence. AIDS Care. 2015;27(3):333–7.
Shrestha R, Huedo-Medina T, Altice F, Krishnan A, Copenhaver M. Examining the acceptability of mHealth technology in HIV prevention among high-risk drug users in treatment. AIDS Behav. 2016;21:3100–10.
Shrestha R, Huedo-Medina T, Copenhaver M. Sex-related differences in self-reported neurocognitive impairment among high-risk cocaine users in methadone maintenance treatment program. Subst Abuse Res Treat. 2015;9:17–24.
SAMHSA. National registry of evidence-based programs and practices (NREPP). Rockville: SAMHSA; 2015.
Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111(3):455–74.
Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57(3):225–38.
Tarnowski KJ, Simonian SJ. Assessing treatment acceptance: the abbreviated acceptability rating profile. J Behav Ther Exp Psychiatry. 1992;23(2):101–6.
Wilson IB, Lee Y, Michaud J, Fowler FJ, Rogers WH. Validation of a new three-item self-report measure for medication adherence. AIDS Behav. 2016;20(11):2700–8.
Dowling-Guyer S, Johnson ME, Fisher DG, Needle R, Watters J, Andersen M, et al. Reliability of drug users’ self-reported HIV risk behaviors and validity of self-reported recent drug use. Assessment. 1994;1(4):383–92.
Shrestha R, Altice FL, Huedo-Medina TB, Karki P, Copenhaver M. Willingness to use pre-exposure prophylaxis (PrEP): an empirical test of the information-motivation-behavioral skills (IMB) model among high-risk drug users in treatment. AIDS Behav. 2016. https://doi.org/10.1007/s10461-016-1650-0.
Copenhaver M, Lee I, Baldwin P. A randomized controlled trial of the community-friendly health recovery program (CHRP) among high-risk drug users in treatment. AIDS Behav. 2013;17(9):2902–13.
Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Subst Abuse Treat. 2004;26(2):67–78.
Bekker L-G, Beyrer C, Quinn TC. Behavioral and Biomedical Combination Strategies for HIV Prevention. Cold Spring Harbor Persp Med. 2012. https://doi.org/10.1101/cshperspect.a007435.
Liu A, Colfax G, Cohen S, Bacon O. The spectrum of engagement in HIV prevention: proposal for a pre-exposure prophylaxis (PrEP) cascade. In: 7th international conference on HIV treatment and prevention adherence, Miami, FL (2012).
Spector AY, Remien RH, Tross S. PrEP in substance abuse treatment: a qualitative study of treatment provider perspectives. Subst Abuse Treat Prev Policy. 2015;10(1):1–10.
Siedner MJ, Haberer JE, Bwana MB, Ware NC, Bangsberg DR. High acceptability for cell phone text messages to improve communication of laboratory results with HIV-infected patients in rural Uganda: a cross-sectional survey study. BMC Med Inform Decis Mak. 2012;12:56.
Tolan PH, Gorman-Smith D, Henry D, Schoeny M. The benefits of booster interventions: evidence from a family-focused prevention program. Prev Sci. 2009;10(4):287–97.
Liu A, Colfax G, Cohen S, Bacon O, Kolber M, Amico K, et al. The spectrum of engagement in HIV prevention: proposal for a PrEP cascade. In: 7th international conference on HIV treatment and prevention adherence, Miami Beach, FL (2012).
Funding
This work was supported by grants from the National Institute on Drug Abuse for research (R01 DA032290 to MMC) and for career development (K24 DA017072 to FLA; K02 DA033139 to MMC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical Approval
The study protocol was approved by the Institutional Review Board (IRB) at the University of Connecticut and received board approval from APT Foundation Inc. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Shrestha, R., Altice, F.L., Karki, P. et al. Integrated Bio-behavioral Approach to Improve Adherence to Pre-exposure Prophylaxis and Reduce HIV Risk in People Who Use Drugs: A Pilot Feasibility Study. AIDS Behav 22, 2640–2649 (2018). https://doi.org/10.1007/s10461-018-2099-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2099-0