Abstract
Indigenous leaders remain concerned that systemic oppression and culturally unsafe care impede Indigenous peoples living with HIV from accessing health services that make up the HIV cascade of care. We conducted a systematic review to assess the evidence related to experiences of the HIV care cascade among Indigenous peoples in Australia, Canada, New Zealand, and United States. We identified 93 qualitative and quantitative articles published between 1996 and 2017 reporting primary data on cascade outcomes disaggregated by Indigenous identity. Twelve involved data from Australia, 52 from Canada, 3 from New Zealand and 26 from United States. The majority dealt with HIV testing/diagnosis (50). Relatively few addressed post-diagnosis experiences: linkage (14); retention (20); treatment initiation (21); adherence (23); and viral suppression (24). With the HIV cascade of care increasingly the focus of global, national, and local HIV agendas, it is critical that culturally-safe care for Indigenous peoples is available at all stages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The HIV cascade of care has emerged as a key framework to understand “success” with respect to HIV prevention and treatment around the globe [1]. According to the HIV cascade of care framework, the ultimate clinical goal of HIV treatment is achievement of viral suppression, which in turn reduces HIV transmission, morbidity, and mortality [2, 3]. To reach viral suppression, people living with HIV must achieve and sustain the steps of the HIV care cascade: they must know they are positive, be linked and retained in care, initiate antiretroviral therapy (ART), and adhere to medications [4]. The HIV cascade framework has been widely accepted and is the basis of the global HIV treatment agenda outlined in the UNAIDS 90-90-90 treatment targets [1]. These targets seek to ensure that 90% of people living with HIV globally are diagnosed; 90% of those diagnosed are on treatment; and 90% of those on treatment are virally suppressed by 2020. If these global targets are met, it is hypothesized that an end to the HIV epidemic is possible by 2030. Recent figures indicate that 66% of people living with HIV globally know their status [5]. Among these, 77% are accessing ART and 82% of those on treatment are virally suppressed [5]. Addressing substantial gaps in HIV care that persist among populations facing significant barriers to treatment remains imperative [5, 6].
IndigenousFootnote 1 leaders and scholars continue to voice concerns that systemic oppression and lack of culturally safe prevention and care services impede Indigenous people living with HIV from accessing health services that make up the HIV care cascade. Culturally safe care is that which is free from racism and discrimination, where Indigenous perspectives of health and wellbeing are respected, impacts of ongoing colonization are acknowledged, and health providers adopt a humble, self-reflective clinical practice to walk beside Indigenous people on their health and wellness journeys [7,8,9]. HIV among Indigenous peoples must be considered in the context of ongoing colonization and systemic violence. Indigenous peoples in Australia, Canada, New Zealand, and the United States in particular share similar experiences of legislated dispossession and dislocation as a result of British colonial rule [10,11,12]. Colonization in these countries included legislated restriction of movement, criminalization of peoples seeking to maintain ceremonies and traditions, and forcible removal of Indigenous children from families and communities. The result of these colonial onslaughts has been termed a “soul wound” passed through generations [13]. The impacts of these policies are a powerful determinant of health, manifesting in preventable health inequities [14,15,16]. According to a recent review, HIV rates among Indigenous peoples in four countries are: Australia (31.2 per 100,000; Rate Ratio: 1.19), Canada (179.2 per 100,000; RR: 6.14), New Zealand (18.9 per 100,000; RR: 1.02) and United States (9.3 per 100,000; RR: 1.33) [17]. In all cases, these rates are higher than among non-Indigenous people [17, 18]. Given the disproportionate burden of HIV among Indigenous peoples, it is a serious concern that Indigenous people living with HIV may become the ‘10-10-10’ of the UNAIDS targets—those who are not engaged in care [19].
As the HIV cascade of care framework is increasingly the focus of global, national, and local HIV agendas, it is imperative that existing evidence is taken into account [20]. Two previous systematic reviews have focused on HIV incidence [21] and risk/prevention [17] among Indigenous peoples in Canada and elsewhere. An additional literature review by Nowgesic [22] focused on Indigenous people’s experiences of ART therapy, but did not include the additional cascade stages of HIV testing, linkage to care, and retention in care. Thus, this systematic review assesses the evidence related to epidemiology and experiences of the HIV cascade of care among Indigenous peoples in Australia, Canada, New Zealand, and United States. Further, it draws on included studies to support understanding of whether the HIV cascade of care framework is meeting the needs of Indigenous peoples and identify gaps in existing literature.
Methods
HIV Cascade of Care Framework
The HIV cascade of care is the guiding framework for this review and includes the following steps towards engagement in HIV care: (1) testing and diagnosis; (2) linkage to care; (3) retention in care; (4) ART initiation; (5) ART adherence; and (6) viral suppression (Fig. 1) [4].
Search Strategy
We followed the PRISMA guidelines for reporting systematic reviews [23]. Search terms (Table 1) combined keywords from each of three conceptual categories [1]: HIV/AIDS [2]; Indigenous peoples in Australia, Canada, New Zealand and the United States; and [3] HIV cascade of care. Medline, Embase, CINAHL, and Web of Science searches were conducted in March 2016 and again in January 2018, prompted by the publication of several valuable articles related to the cascade of care among Indigenous people living with HIV in 2016 and 2017. Three relevant journals (Pimatisiwin: Journal of Aboriginal and Indigenous Community Health; Canadian Journal of Aboriginal Community-Based HIV/AIDS Research; and International Journal of Indigenous Health/Journal of Aboriginal Health) were hand searched as they are not indexed. Finally, we reviewed references from eligible articles to identify additional relevant publications.
Assessment for Inclusion
Articles were included if they met the following criteria: (1) presented findings related to one or more of the stages of the HIV cascade of care: testing and diagnosis, linkage or retention in care, ART initiation or adherence, and viral suppression; (2) geographic: Australia, Canada, New Zealand, United States; (3) dates: January 1, 1996–January 11, 2018 (year HAART came out to present); (4) study design: qualitative, quantitative, mixed methods, observational studies, intervention studies; (5) types of articles: peer-reviewed and presenting primary data (exclude: reviews, commentaries, reports, conference abstracts, theses); (6) language: published in English; (7) population: Studies among Indigenous people living with HIV, and those with Indigenous participants living with HIV as part of a larger sample that included analysis by Indigenous identity. Articles were excluded if data on cascade outcomes were not disaggregated by Indigenous identity; did not report a cascade of care outcome; did not report primary data; or the quantitative study sample included < 10 Indigenous people.
First, two authors independently reviewed each title and abstract. An inclusive approach was taken at this stage to ensure that no relevant studies were missed. If reviewers disagreed on eligibility of an article, it was discussed until consensus was reached. Full-text was accessed for further clarification if necessary. Second, we retrieved full-text publications to further assess compliance with eligibility criteria. Those deemed not to meet the inclusion criteria after full-text review were discussed in person with at least one other author.
Data Extraction and Synthesis
We extracted data into a structured Google Forms database in three areas: study characteristics, HIV cascade of care outcomes, and quality assessment (detailed below). Study characteristics included author, year, title, study approach, study design, study name, country, Indigenous group, key population, sample size, total number of Indigenous participants, and level of Indigenous focus. To extract HIV cascade of care data, we used a checklist to identify the stage of the cascade dealt with in the article (testing and diagnosis; linkage to care; retention in care; ART initiation; ART adherence; or viral suppression). We also recorded the findings related to that cascade stage in as much detail as possible. Findings included frequencies, proportions, summary statistics, confidence intervals, and p-values, as well as qualitative themes. We prioritized understanding and describing cascade experiences among Indigenous peoples in absolute rather than relative terms (e.g., comparisons to other ethnicities). Due to variability in cascade stage definitions, we also extracted the definition provided in the article. The data extraction form was pilot-tested on five randomly selected included studies and refined accordingly [24]. Data from included studies were extracted by the lead author, and verified through independent extractions by co-authors on a selection (n = 21; 22.6%) of articles.
Analytical Approach
For quantitative studies, diversity of measures and heterogeneity of statistics prevented meta-summary or development of pooled estimates by cascade stage [20]. Instead, we used a textual narrative synthesis to highlight insights related to common measures of each cascade stage; volume and quality of available evidence; regional patterns; and trends over time. Bubble plots representing a rough overview of the most frequently occurring measure for each cascade stage are presented.
For qualitative studies, we meta-aggregated data within an existing theoretical framework (HIV cascade of care) using a modified Qualitative Assessment and Review Instrument (QARI) process [25, 26]. Each article that included qualitative findings was coded using the stages of the HIV cascade of care defined by Gardner et al. [4]. We extracted key findings and related illustrations (quotes) overall and for each cascade stage, grouped findings into categories, and then created a synthesized summary for each category [26].
Quality Assessment
Study quality was assessed in two stages. Given that this review engages with health research involving Indigenous peoples, it was important to assess the quality of the included studies through both Indigenous and mainstream lenses. Recent literature has called for efforts to strengthen and decolonize reviews to better meet the needs of Indigenous peoples [27, 28]. Yet, to our knowledge, no tool currently exists to evaluate the quality of evidence included in a systematic review from an Indigenous perspective. As a result, we (a team of Indigenous and non-Indigenous scholars) developed a brief checklist (Fig. 2) that would indicate whether included studies had taken steps to conduct their research with consideration of Indigenous research standards or ‘in a good way’. ‘In a good way’ is a term used by many Indigenous communities to describe an action that is done in accordance with Indigenous values and protocols [29]. We use it here to reflect an approach to research that embeds ethics, protocols, and cultural safety according to Indigenous paradigms and methodologies [11, 30,31,32]. Research continues to be a tool of colonization, used as a way of pathologizing and surveilling Indigenous peoples [11, 33]. However, others have identified the power of research, when done in a good way, to be empowering, healing, and self-determining [33]. Checklist items were identified from literature on Indigenous methodologies and research ethics, as well as the expertise of team members involved with this review [14, 15, 28,29,30,31, 34,35,36,37]. As Indigenous research standards are growing and developing, an ‘other’ category was included to capture actions not included on the existing list. Articles that incorporated some or several of the approaches listed are indicated with a ‘*’ in the table.
In addition, we used a condensed Newcastle–Ottawa Quality Assessment Scale—Cohort Studies to assess quality of included quantitative observational studies, which make up the bulk of those identified in this review [38]. The condensed scale assesses external and internal validity using four items with four possible responses that represent the highest level of validity to lowest. For each item, a star is awarded if the highest or second highest level of validity is achieved [38].
Results
Two areas of evidence emerged over the course of this review. One focused on narratives, contexts, and experiences of engagement in the HIV cascade of care among Indigenous peoples using qualitative data. The other focused on the epidemiology of the HIV cascade of care among Indigenous peoples including rates, comparisons, and predictors. We begin with an overview of the included studies. Next, overarching determinants of engagement in the HIV cascade of care among Indigenous peoples are discussed [27]. Then, we present detailed results by each stage of the HIV cascade of care, starting with experiences (qualitative evidence) followed by epidemiology (quantitative evidence).
Overview of Included Articles
Database searches yielded a total of 5668 articles (Medline = 1649, Embase = 1740, CINAHL = 645, and Web of Science = 1634) (Fig. 3). We identified an additional 19 articles through hand-searches of un-indexed journals. After duplicates were eliminated, 3255 records were screened and 179 full-text articles that met the eligibility criteria were further assessed for eligibility. Of these, 91 articles were excluded for the following reasons: data on cascade outcomes were not disaggregated by Indigenous identity (n = 34); did not report a cascade of care outcome (n = 40); did not report primary data (n = 14); or quantitative study sample included < 10 Indigenous people (n = 3). Reviewing reference lists identified an additional five articles. In total, 93 articles fulfilled the inclusion criteria and were included in this review (Fig. 4).
Overall, the 93 included articles involved approximatelyFootnote 2 52,000 Indigenous participants in 70 studies (Table 2). In total, 14 (15.1%) were qualitative, 72 (77.4%) quantitative, and 7 (7.5%) mixed methods. By country, 12 (12.9%) involved data from Australia, 52 (55.9%) from Canada, 3 (3.2%) from New Zealand, and 26 (28.0%) from the United States. Additional characteristics of included studies can be found in Table 2.
Overarching Determinants of Engagement in the HIV Care Cascade
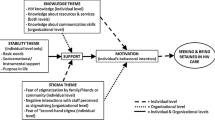
Several overarching determinants of engagement in the HIV care cascade among Indigenous peoples emerged from the 21 studies presenting qualitative data, each of which applies to the cascade of care as a whole or to multiple stages (Fig. 5). The determinants identified were interconnected. Some helped promote engagement in care, while others hindered it.
Indigenous Culture, Identity, and Ceremony
Indigenous identity was a source of strength and wellbeing identified by participants in the qualitative studies [39, 40]. Participation in the ceremonies and cultural activities of their nation was an important way to maintain health and wellness in the context of HIV for some Indigenous people living with HIV (IPHAs) [41, 42]. For others, HIV diagnosis prompted learning more about Indigenous spirituality and traditional healing [43]. Culture and ceremony were identified as especially helpful for the spiritual and emotional aspects of living with HIV, including coming to terms with diagnosis [42, 44, 45]. For example, a participant in Ka’opua’s study among Native Hawaiian people living with HIV described participating in ho’oponopono, a relational wellness ceremony convened by her family to ease her stress and depression related to living with HIV [42]. Many IPHAs sought to integrate traditional wellness practices alongside mainstream services. Care providers who supported this approach were valued [46,47,48]. However, the enduring legacy of spiritual abuse stemming from colonization, such as that which took place in Canada’s residential school system, could be a barrier to engagement with Indigenous cultural practices and ceremonies [40, 42, 49]. In addition, some IPHAs reported that they felt cultural wellness practices were sidelined in relation to the dominance of the mainstream biomedical model in care settings [46].
Strength, Resilience, and Determination
Resilience and determination despite adversities emerged as important contributors to engagement in HIV care, as well as health and wellbeing overall. Choosing to fight HIV was a deliberate decision made by a number of IPHAs involved in these qualitative studies [39, 40]. Responsibility for caring for their children and families was also a powerful motivator to seek care, as well as a source of strength and self-worth [41, 42, 46, 50]. For example, Ka’opua et al.’s interviews with six Native Hawaiians living with HIV revealed that being well enough to fulfil kuleana (responsibilities), such as taking care of an extended family member, was a major reason to manage health [39, 42]. Other studies revealed that involvement in the HIV community, such as through volunteering, activism, or peer support, contributed to an individual’s own wellbeing and sense of self, which in turn contributed to their participation in HIV care [39, 45, 46]. Taken together, this suggests that engagement in HIV care is likely to be enhanced if it includes assessing and building from IPHAs strengths, rather than areas of weakness.
Social Support Systems: A Circle of Care
Another overarching theme was the critical importance of having other people in life to help navigate the challenges and complexities of living with HIV and the demands of sustained engagement in care. As one of Mill et al. participants explained, “I can’t deal with this alone” [43]. Included articles identified and described several different types of social support systems. Family members (especially partners) were identified as providing tangible (e.g., cooking, medication reminders), affirmational (e.g., reason to keep going, love and affection), and spiritual (e.g., facilitating access to traditional healing) support [46]. Friends and peers (with HIV) often played an important role in IPHA support systems [39, 43,44,45,46, 51]. Professionals, including healthcare providers, social workers, and the organizations they work for, were also within IPHA support systems. Support systems were often reciprocal, with IPHAs having valued and meaningful responsibilities to fill within these relationships [43]. Further, human connectedness and sense of belonging had intrinsic value that contributed to health and wellbeing [46]. In this way, participation in these relationships was an important part of self-worth and identity for IPHAs. The current iteration of the cascade of care framework focuses on the individual; however, given the importance of support systems to sustained engagement in care, clinicians must recognize and support strong circles of care.
Historical, Intergenerational, and Lifetime Trauma
Included studies highlighted the ways Indigenous life in Australia, Canada, New Zealand, and the United States were forcibly disrupted by the arrival of settlers and establishment of colonial states. Trauma experiences continue to be fundamental determinants of HIV infection among Indigenous peoples [17, 52]. Historical, intergenerational, and lifetime trauma experiences may also be a barrier to engagement in HIV care and treatment through a number of pathways. Experiences included: grief and loss [40, 46]; childhood sexual abuse [44, 45, 47, 50, 53, 54]; domestic violence [39, 47]; spiritual, cultural, and community disconnection [42, 46]; forced removal from parents into residential schools or the child welfare system [46, 47, 54, 55]; and poverty [39, 56]. Acknowledging historical trauma and ongoing systemic oppression has been recognized as a critical element of successful health services for Indigenous peoples [44, 46, 47]. Further, supporting IPHAs to heal from trauma may be an important way to facilitate sustained engagement in the HIV cascade of care.
Articles identified several possible pathways through which trauma may affect engagement in care. First, experiences of trauma may contribute to a lack of self-worth and increased hopelessness, which may affect IPHAs interest or ability to consistently engage in care [47, 48]. Disconnection and dislocation from community and identity has a powerful impact on self-worth [42]. Grief and witnessing the death of loved ones and others may further contribute to hopelessness [40]. Second, some IPHAs cope with the pain and stress of these traumas through substance use, which emerged as a major proximal barrier to HIV care and treatment in the included studies [40, 47, 48, 50, 55]. For example, Ka’opua reported that one participant in her study described feeling kaumaha, a “profound heaviness associated with dislocation from family,” and desire to numb this feeling contributed to continued substance use [42]. Third, several IPHAs reported feeling distrustful of healthcare and/or healthcare providers which may reflect having experienced or witnessed harms perpetrated within the context of healthcare (e.g. medical experimentation, isolation, racism) [47, 57,58,59,60]. Finally, trauma experiences may also exacerbate negative social determinants of health, resulting in further marginalization from engagement in HIV care and services [39].
Stigma and Discrimination
Participants reported both fear and experiences of discrimination by healthcare providers, family, friends, and community [39, 55]. These experiences reflected multiple layers and intersections related to race, substance use, sexual or gender identity, and spirituality, as well as HIV [40, 44, 46, 55, 61]. Fear of discrimination led some IPHAs to avoid accessing services [47]. Other IPHAs undertook strategies to avoid these negative feelings, including seeking Indigenous-specific, gender-specific, or HIV-specific services [39, 47, 62]. However, these were not always available, especially for those living in small communities and remote areas. Internalized stigma also played a role in determining engagement in care [39].
Intersecting Health Concerns
A diverse set of wellness priorities—including but not limited to HIV health and wellbeing—were identified. Intersections of trauma, substance use, mental health, and HIV were important reoccurring themes. Substance use (e.g., alcohol, illicit drugs) and mental health issues (e.g., depression, post-traumatic stress) were understood simultaneously as risk factors for HIV acquisition, consequences of HIV diagnosis, and barriers to engagement in HIV care [39, 40, 48, 55, 61, 63]. As a result, supporting IPHAs to engage in care requires a wholisticFootnote 3 approach that addresses intersecting health needs and wellness priorities [64]. IPHAs continue to demand care and services that address the many factors impacting their lives in addition to HIV infection [51, 65, 66]. Of note, HIV was described as both a physical and emotional disease by participants in several studies [39, 40, 42, 45, 51]. Yet, the cascade of care framework focuses only on the physical aspects of HIV and does not explicitly address these emotional consequences which have tremendous implications for linkage, retention, and adherence.
Testing and Diagnosis
Screening is essential for early detection, treatment, and prevention of HIV infection [67]. Testing and diagnosis was the most well studied step in the HIV care cascade, involving 50 articles.
Experiences of Testing and Diagnosis
Fourteen articles provided qualitative insight into Indigenous people’s experiences of HIV testing, with the majority coming from Canada (n = 11). Unlike the quantitative literature which focused only on the testing event, these articles also focused on experiences of diagnosis. Fear of testing positive was a reoccurring theme and was a reason some Indigenous people chose to avoid or delay testing [47, 53, 63]. This was linked to the ongoing perception that HIV is a “death sentence”, as well as fear of being discriminated against by family, friends, and community [40, 45, 46].
Articles identified reasons Indigenous people choose to seek testing, including: having participated in behaviours that could result in HIV transmission [45, 47, 53, 63]; having HIV symptoms [45, 66]; part of regular screening [53]; or at the beginning of a new relationship [53]. Testing or diagnosis in the context of care for other health concerns was also common, including perinatal care [45, 47, 53, 63] and substance use treatment [50]. Testing took place in a number of settings, including with a physician, in a hospital, in a community or public health centre, or in an STI clinic [47, 63]. However, inconvenient hours and/or location of testing sites remained an obstacle to testing [62, 63].
Distrust of healthcare providers and institutional discrimination in healthcare were identified as formidable barriers to testing [47]. These barriers were rooted in the ongoing impact of colonization. For example, among women in Northern Alberta, fear that testing positive would result in their children being apprehended was a powerful impediment to testing [47]. Indigenous youth living with HIV from across Canada reported delaying testing until they began to have symptoms, which suggests a reluctance to engage with the healthcare system [45, 66]. Confidentiality concerns, including fear of disclosure and lack of anonymity in small communities, were a barrier to testing in a number of studies [45, 47, 53]. In response, some participants chose to be tested outside of their community [63]. Linked to confidentiality concerns was fear of discrimination and judgement by healthcare providers in the context of testing [47, 53]. In two studies, IPHAs shared that being asked personal questions about behaviours that could result in HIV transmission during testing was perceived as shaming and judgmental [45, 47]. Focusing on behaviour was seen to reflect a lack of understanding of life experiences, and participants preferred to focus on the present and future, rather than digging into past actions [47]. Healthcare providers in Reading et al.’s 2013 study reported that Indigenous women in particular were more likely to be asked personal questions, for example about sexual activity, compared to non-Indigenous women, and this reflected racist attitudes [46]. In contrast, testers who were nurturing, supportive, and took their time were valued [45]. Additional barriers to testing were low perceived risk [53, 63] and feeling invulnerable [53].
While testing may appear to be a discrete, highly defined step on the HIV care cascade, qualitative research suggests that coming to terms with diagnosis is a process that may affect both health and healthcare engagement. Participants described an emotional response to diagnosis, including shock, anger, fear, denial, and shame [40, 41, 45, 50]. Four studies proposed frameworks for understanding the process of coming to terms with diagnosis. Thompson et al.’s study involving 20 Indigenous people living with HIV in Western Australia suggested that immediately after diagnosis there may be a spike in behaviours like substance use as IPHAs try to avoid and escape this new reality; however, this was often followed by a “slowing down” of substance use as participants came to terms with their diagnosis and focused on their health [50]. Sazegar et al. developed a similar understanding in their interviews with IPHAs in Vancouver, Canada, describing three stages of post-diagnosis coping: shock and loss; scared and alone; and acceptance and healing [51]. Mill et al.’s study among eight Indigenous women living with HIV in Northern Alberta, Canada portrayed a “downward spiral” in reaction to diagnosis that lasted from six months to three years, before participants came to a “turning point” towards positive living [41]. Again, in a study among 31 IPHAs in Alberta, Mill et al. described a cycle which may take several years: receiving the diagnosis; adapting to the diagnosis; accepting the diagnosis; and ongoing challenges [45]. For many participants across studies and countries, the coping phase included escalation of substance use for numbing and a temporary escape [40, 42, 45, 50]; self-imposed isolation from others [40, 45]; as well as hopelessness and suicidal ideation [40, 45, 63]. Despite the difficulty of the diagnosis, HIV could be a turning point for IPHAs during which they actively made a decision “to live” and stay healthy [40, 41, 45]. This transition could involve seeking out alternate coping strategies such as support from others [43, 50, 51] and participation in Indigenous cultural practices and spirituality [41, 44, 45].
Epidemiology of Testing
Thirty-eight articles provided quantitative data on HIV testing among Indigenous peoples. They included diverse measures of testing, including proportion of people: ever tested (n = 15), tested in the past year (n = 10), tested in the context of care for another health concern (n = 7), with late diagnosis (n = 3), and others.
Thirteen studies with complete data reporting the proportion of Indigenous people who had ever received testing are summarized in Fig. 6. The proportion of those ever tested for HIV appears relatively steady over time in general and in youth populations, at approximately 50%. Studies with trans people, men who have sex with men, and people who use drugs, report higher proportions of those ever having been tested for HIV in recent years.
Studies reporting proportion of Indigenous people who had ever received testing (n = 13). Note: Plots are not comprehensive but represent an overview of the most frequently occurring measure for this stage. Each bubble represents one study. Bubble size represents sample size. Color indicates study country. Key populations are indicated with tags. If none is identified, the study involved a more general population
We identified varied results across studies that compared likelihood of HIV testing among Indigenous and non-Indigenous people. Six studies suggested that Indigenous people are more likely to be tested for HIV, compared to non-Indigenous people [68,69,70,71,72,73]. Three others observed no differences in likelihood of testing between Indigenous and non-Indigenous participants [74,75,76], including two that were in specific settings: remote antenatal care [74] and a pharmacy-based needle exchange program [76]. Just one—a New Zealand study from the early 1990s—observed lower odds of testing among Maori participants compared to others [77].
Testing and Diagnosis Summary
High proportions and odds of testing among Indigenous people identified in this review may reflect the perception that Indigenous people are ‘at risk’ and are therefore tested more often than non-Indigenous people.
Reviewing both qualitative and quantitative approaches to understanding testing and diagnosis among Indigenous people reveals that, from a clinical perspective, testing and diagnosis may be important but circumscribed events. In contrast, from the perspective of IPHAs, testing and diagnosis, especially in the case of a positive diagnosis, is a process that does not begin or end with the testing or diagnosis event. Appropriate supports are required to ensure that the healthcare system does not fail to keep IPHAs engaged during this transition period. For example, it is paramount that HIV diagnosis is followed up with access to culturally safe HIV care.
Linkage to Care
Delays in accessing care after an HIV diagnosis may increase the risk of disease progression and transmission [2]. Current guidelines recommend that those who test positive be immediately linked to care [78]. Yet, just 14 articles examined linkage to HIV care among Indigenous people.
Experiences of Linkage to Care
Very limited qualitative data are available on linkage to care. We identified just seven qualitative articles (all Canadian) that addressed this cascade stage. The emerging theme across these studies was that the challenges of post-diagnosis coping delay linkage to care [41, 45, 50, 51]. For example, Indigenous youth living with HIV in Canada reported that time to care after diagnosis ranged from a few months to seven years, with some waiting until they were very sick to access care [63, 66]. Fear, hopelessness, avoidance, misperceptions of care, substance use, and challenges accessing care in smaller communities underpinned delays accessing care across studies [39, 51, 63, 66]. Clinical recommendations for immediate linkage to care coincide with a stressful period in IPHAs lives which may include approaches to coping (e.g., substance use, isolation, hopelessness, denial) that are in opposition to care seeking. Sazegar et al. suggested that, until IPHAs reach a stage of acceptance and healing post-diagnosis, they may not be ready to engage in care (including self-care) [51].
Epidemiology of Linkage to Care
Eight quantitative studies reported on linkage to care. Indicators of linkage to care included: proportion of IPHAs presenting late to care (n = 3); receiving a blood test within a specified time period post diagnosis (n = 2); median time to care (n = 1); and self-reported access to HIV care (n = 1). While the diversity of measures limits comparisons across studies, evidence suggests that high proportions of Indigenous people have never accessed care [66, 79] or have delayed access [75, 79,80,81,82]. Three studies that examined the proportion of IPHAs presenting late to care reported that between 24 and 46% of IPHAs enter care when they are already seriously ill [80,81,82]. Studies that compared Indigenous and non-Indigenous participants observed mixed results. However, more studies found increased risk of delays among Indigenous people [75, 79, 80] than found decreased risk of delays [81].
Linkage to Care Summary
A paucity of evidence, inconsistency of measures, and mixed results overall suggest that linkage to care is an important area for future study to ensure that Indigenous people living with HIV are receiving timely care after diagnosis. Overall, findings suggest that supporting IPHAs to move through the difficult process of coming to terms with HIV diagnosis is an important aspect of enhancing engagement in the cascade of care. Recommended by Sazegar et al., a “first response strategy” involving physicians, counsellors, and peer support in the period immediately after diagnosis may help mitigate coping responses that can be an obstacle to linking to care [51]. Further, among youth, encouragement and support from family, friends, and professionals may be critical to initiating care and traditional healing practices post-diagnosis [66]. Clinical care must take into account the power of social support, as well as challenges of coming to terms with a positive HIV diagnosis, when developing strategies and programs to enhance linkage to care among IPHAs.
Retention in Care
Until a cure for HIV is available, staying well and reducing transmission while living with HIV demands lifelong engagement with health services [4]. We identified 20 studies that provided insight into retention in HIV care among Indigenous peoples.
Experiences of Retention in Care
Attending clinic appointments and participating in laboratory monitoring for CD4 counts and viral load (indicators of retention in care) were just two of many actions IPHAs took to stay healthy; other care strategies include reducing substance use, accessing traditional healing, and maintaining health through diet, sleep, and exercise [51, 66]. Some participants were keen to know the results of laboratory monitoring, but emphasized the need for clinicians to occasionally revisit the meaning and implications of these counts [51]. Others avoided appointments and lab testing for fear of what they would reveal: “I know I was supposed to take another blood test six months ago but I didn’t. I’ve been holding back and holding it off because I am scared…I don’t want to find out more than I know” [41].
How HIV care services were delivered played an important role in retention in care. Overall, being able to trust the care provider was essential [46]. Fear of discrimination from healthcare providers was a powerful deterrent, especially for IPHAs who had previous experience of discrimination in institutional settings [39, 48]. IPHAs reported that specialized services for people with HIV could be higher quality and participants could feel less judgement in these settings [39]. Some described positive experiences with a team approach to care which involved accessible support from a doctor, nurse, and social worker [43]. In contrast, lack of specialized services in non-urban areas could contribute to experiences with healthcare providers who were misinformed, judgmental, or unfamiliar with providing HIV care [39, 43]. Accessibility of care was also an important factor, as concerns were identified about limited hours, long wait times, and distance of care from home [39]. Some IPHAs, especially in small communities, reported that attending HIV health services had resulted in unwanted disclosure of their HIV status; others were concerned about the potential for disclosure if they were seen accessing care [39, 65]. One study briefly mentioned continuity as beneficial in relationships with healthcare providers; this warrants more attention in future research related to the HIV cascade of care among Indigenous people [43].
Other aspects of life also influenced retention in care. As mentioned previously, IPHAs often face a diverse set of health challenges and wellness priorities, which may enhance or diminish retention in care. Sazegar et al.’s study among people living with HIV (50% of whom were Indigenous) in Vancouver, Canada, included asking participants to identify and rank HIV-related health priorities. Drug addiction, mental illness, and unresolved trauma topped the list, with access to doctors and nurses ranking 28th of 29 priorities [51]. Five studies reported that periods of active substance use made regularly attending care a challenge [39, 43, 51, 54, 61]. McCall et al. found that among eight female IPHAs, those experiencing addiction reported that attention to substance use was their primary concern and HIV care was a lower priority [39]. Navigating domestic violence and meeting basic needs (e.g., housing, food) in the face of poverty were two other competing priorities next to HIV care [39]. Being pregnant was a motivator for women to attend clinic appointments and participate in regular laboratory monitoring to ensure the health of their child [66].
Epidemiology of Retention in Care
Ten quantitative studies were related to retention in care. However, lack of consistency in measurement made it difficult to compare across studies. Laboratory monitoring (n = 6), clinic visits (n = 2), self-reported retention (n = 1), and missed appointments (n = 1) were all used to measure retention in care. Three recent studies measuring proportion of IPHAs who had at least two lab tests at least three months apart within a one-year period identified that 34.9–58.9% of IPHAs were retained in care, according to this definition [83,84,85]. Several studies included comparisons between Indigenous and non-Indigenous people. All but one [79] observed worse retention in care outcomes for IPHAs, compared to those of other ethnicities [81, 83, 85,86,87].
Retention in Care Summary
These findings highlight the need for wholistic approaches to retention in care. The qualitative articles in this review demonstrate that retention in care is about a sustained relationship or partnership between an IPHA and a team of care providers over a lifetime. In contrast, the quantitative articles suggest that retention in care is primarily about laboratory monitoring, a key clinical priority. To strengthen care partnerships as a way of improving retention in care, the pressing health and wellness priorities of IPHAs must not be sidelined.
Further, there is a lack of consensus on the best way to understand and measure retention in care. Existing data are insufficient to determine whether Indigenous people living with HIV are adequately retained in care. The qualitative literature demonstrates that trusting, respectful, culturally safe relationships with care providers are imperative to sustained engagement in HIV care. We must improve measures and data collection related to retention in care to understand the extent to which IPHAs remain engaged in HIV care over the long term.
ART Initiation
Mounting evidence supports early or immediate initiation of ART for all people living with HIV, regardless of CD4 + count [88, 89]. However, supporting all people living with HIV to begin treatment remains a challenge globally [6]. Twenty-one studies examined ART initiation among Indigenous peoples.
Experiences of ART Initiation
Participants who initiated ART noticed positive changes in their lives, including increased energy, better appetite, and affirming improvements in CD4 and viral load levels [51]. Incentives to initiate treatment included pregnancy [41, 65, 66]; feeling sick [41]; or clinical indications/advice [66]. However, others decided not to initiate medication despite experiencing HIV-related symptoms and illnesses [39].
Several studies reported on experiences of ART initiation and identified a number of reasons that IPHAs choose not to begin medication, including feeling healthy or not having been told by a physician to start ART [66]. Some IPHAs did not have confidence in the efficacy of ART, were concerned about side effects, believed that ART was not good for them, or did not perceive HIV as a treatable illness [39, 41, 66, 90]. For others, taking ART was a constant unwanted reminder of their HIV status [39] or a trigger related to a history of substance use [41]. Another concern was the potential for disclosure of HIV status to family, friends, or colleagues if medications were noticed [65]. In addition, two studies shared that some female IPHAs articulated a sense of hopelessness or internalized shame that prevented treatment initiation [39, 41]. Of note, no articles reported lack of access to ART, including financial barriers, as a reason for not initiating ART [65].
Epidemiology of ART Initiation
Eighteen studies described the epidemiology of ART initiation. Main quantitative measures of ART initiation included ever having been on ART (n = 7) or currently being on ART (n = 11). Seven studies reported proportions of Indigenous people ever receiving ART, with the lowest proportion (54.4%) among IPHAs who died in BC, Canada between 1995 and 2001 [91], and the highest (72.0%) among Maori people living with HIV in 2001-2002 [90]. In addition, 11 studies reported proportions of IPHAs currently on ART, with the lowest proportion (29.2%) reported among IPHAs who use drugs between 1996 and 2003 in Vancouver, Canada [92], and the highest proportion (94%) among IPHAs who use drugs in Vancouver in 2014 [93]. Those with complete data are presented in Fig. 7, which suggests improvements in ART initiation over time.
Studies reporting proportion of Indigenous people on ART (n = 8). Note: Plots are not comprehensive but represent an overview of the most frequently occurring measure for this stage. Each bubble represents one study. Bubble size represents sample size. Color indicates study country. Key populations are indicated with tags. If none is identified, the study involved a more general population
In terms of comparisons with other cultural groups, two older Canadian studies demonstrated differences between Indigenous and non-Indigenous people in terms of ART initiation [91, 92]; however two more recent studies in Toronto [94] and Vancouver [93] indicated no differences. These findings hint that the gap between Indigenous and non-Indigenous people on ART may have declined in recent years.
ART Initiation Summary
Clinical guidelines for treatment initiation center around CD4 count thresholds; however, evidence from the qualitative studies in this review suggest that IPHAs arrive at “readiness” for medication only when they have reached a point of acceptance of their HIV diagnosis [51]. “Readiness” may involve a transition from hopelessness in the period immediately after diagnosis, to a desire “to stay healthy and alive” [66]. This process is challenging and may take several months or even several years. Again, the clinical underpinnings of the cascade of care framework do not reflect the lived realities of IPHAs. Clearly, there is an opportunity to bridge these two understandings of ART “readiness” so IPHAs and providers can work in tandem towards timely ART initiation.
Measurement of ART initiation is relatively homogenous compared to other cascade stages. However, as in other stages, the available data is fragmented. Australia is the only country for which recent population-level national estimates of ART initiation among IPHAs are available [87]. Lack of this vital data limits our ability to draw conclusions and measure progress in meeting treatment targets among Indigenous people living with HIV.
ART Adherence
Once initiated on ART, people living with HIV must continue treatment for life without interruption in order to achieve sustained viral suppression, prevent illness, and avoid resistance [95]. Overall, 23 of the studies focused on ART adherence.
Experiences of ART Adherence
Qualitative studies reflected that adherence to ART is not simply a matter of taking or not taking medications each day, but rather about balancing management of health and wellbeing with other responsibilities and challenges. Staying healthy and surviving for themselves, as well as for their children and loved ones, were reasons IPHAs chose to keep taking ART [39, 42, 66]. However, substance use [42, 48, 50, 54, 55, 65, 66]; homelessness [39]; food insecurity [39, 48]; mental health issues [48]; and lack of self-worth [42, 48], all contributed to making adherence more difficult. IPHAs also reported that ART adherence was easier when they also received support with other challenges in their lives, such as trauma, mental health, substance use, and poverty [48, 56, 65]. Some chose to stop or reduce drug use, sometimes with the support of opioid substitution therapies, to enhance their adherence [48, 50]. For others, attention to their spiritual health, including participation in cultural practices and ceremonies, contributed to better adherence [42, 44, 46, 48].
Together, these barriers and facilitators to adherence can result in IPHAs having “good days and bad days” [42]. For most, adherence was not an all or nothing situation, but rather some IPHAs experienced intermittent treatment interruptions as a result of illness or, for some, periods of high intensity substance use [42]. Feeling sick, whether it was a result of side effects or HIV symptoms, sometimes resulted in treatment interruptions [41, 42] or a decision to stop treatment altogether [42, 48, 50]. In one study, women reported discontinuing treatment after giving birth as their counts were good, or because they had found the treatment regimens frustrating or difficult [65].
Social support was identified as being vital to ART adherence, including resuming treatment after an interruption [42, 48]. Ka’opua reported that among six Native Hawaiians living with HIV, intimate partners provided a variety of supports that enhanced adherence, especially on “bad days” [42]. These supportive actions included ensuring IPHAs took their medications, preparing meals, and taking care of other family responsibilities so that IPHAs could focus on their health [42]. Partners provided affection, helped reduce feelings of isolation, and provided or supported access to traditional healing [42]. These actions served to re-inforce participants’ commitment to medication adherence. As one participant explained, when her partner provided this support, “I feel like someone’s really there on my side and it encourages me to be good” [42]. Other IPHAs noted that support from outreach workers who helped participants take their medications were also important for maintaining adherence [48].
Epidemiology of ART Adherence
Thirteen quantitative studies addressed ART adherence. Again, inconsistency in how adherence is measured prevented comparisons across studies. Measurements included pharmacy refill (n = 4); treatment interruption (n = 3); doses taken (n = 4); or other (n = 2). Three Canadian studies reported large proportions of treatment interruptions among IPHAs, ranging from 21.8 to 60.4% [96,97,98]. Another three Canadian studies reported greater than 95% adherence through linkage to pharmacy refill data, ranging from 32.8% among IPHAs who used drugs [93] to 77.1% among male IPHAs with a history of injection drug use [99]. Among studies that compared IPHAs with non-Indigenous people, six reported no differences [91, 93, 96, 100,101,102] and four reported higher non-adherence among IPHAs [97,98,99, 103]. Interestingly, seven of these studies showing varied results involved cohorts of people living with HIV in BC, Canada. One large recent study capturing population-level data for all people living with HIV in BC between 1995 and 2015, involving 1022 IPHAs, observed higher treatment interruptions among Indigenous people compared to non-Indigenous people [98].
ART Adherence Summary
Adherence was measured in a variety of ways, including use of scales, self-reported adherence, treatment interruptions, and prescription refills. Even within measurements, significant variation in the data prevents us from reaching a conclusion about ART adherence among IPHAs. Researchers must bring measurement into alignment to improve consistency across studies.
Treatment interruptions emerged as a concern in both the quantitative and qualitative literature. One qualitative study identified a lack of understanding about how to deal with missed doses; for example, whether it was possible to “catch up” [50]. This may be an important area for discussion during clinic visits.
Viral Suppression
Suppression of HIV viral replication to undetectable levels in the blood through sustained use of ART has been demonstrated to significantly reduce morbidity, mortality, and HIV transmission [2, 3, 104]. In total, 24 articles provided evidence related to viral suppression among IPHAs.
Experiences of Viral Suppression
Despite being a focus of many quantitative studies related to HIV care among Indigenous people, considerations of viral suppression appear in just two of the qualitative studies. A case study of one female IPHA in Vancouver indicated that the participant’s viral load was detectable [54]. Among 26 people living with HIV in inner-city Vancouver, 50% of whom were Indigenous, viral load was a low priority, ranking 23rd out of 29 HIV-related health priorities [51]. Compared to non-Indigenous participants in this study, viral load was ranked significantly lower on IPHAs list of priorities [51]. Notably, apart from these two studies, the other 12 qualitative studies involving IPHAs included no discussion of viral suppression in the context of HIV health and wellbeing at all.
Epidemiology of Viral Suppression
Twenty-two articles presented findings related to viral suppression among Indigenous participants. Despite attention to viral suppression in the epidemiological literature, there is still no consistent measurement of this outcome. Articles included median (n = 11), mean (n = 2), and proportion suppressed (n = 14). The latter, presented in Fig. 8, included a variety of thresholds (i.e., < 400, < 200, and < 50 copies/mL), which likely reflects changes in testing and guidelines over the past 20 years. Proportion suppressed varied widely, from 17.9 to 86.0%. Two recent population-level studies among IPHAs living in the US which reported that 33.6% [85] of female IPHAs and 45.1% of all IPHAs [84] were suppressed are especially concerning.
Studies reporting proportion of IPHAs whose viral load was suppressed (n = 14). Note: Plots are not comprehensive but represent an overview of the most frequently occurring measure for this stage. Each bubble represents one study. Bubble size represents sample size. Color indicates study country. Key populations are indicated with tags. If none is identified, the study involved a more general population
Comparisons of viral suppression between Indigenous and non-Indigenous people yielded mixed results. Two studies observed lower median viral load among IPHAs compared to others [101, 105]. Six studies indicated no differences in viral suppression related to Indigenous identity [87, 93, 94, 103, 106, 107]. Six studies identified worse viral suppression outcomes among IPHAs compared to non-Indigenous people living with HIV [85, 86, 108,109,110,111]. Notably, the three studies with the most Indigenous participants (≥ 497 each), two of which involved longitudinal data collected over more than 10 years, identified worse viral suppression outcomes among IPHA [85, 108, 111].
Viral Suppression Summary
Taken together, the strongest evidence available suggests that viral suppression targets have not yet been reached and that IPHAs may be experiencing disparities in this area compared to non-Indigenous people. This may reflect the apparent disconnect between clinical priorities as articulated within the HIV cascade of care, and the health and wellness priorities identified by IPHAs reflected in the qualitative literature. It is important that clinical care is patient-led to ensure that all concerns of IPHAs are addressed, including those related to mental, physical, spiritual, and emotional health, and are not limited to viral suppression.
Quality Assessment
Included studies were of varying quality. Of 93 studies, 48 (51.6%) took steps to incorporate Indigenous research standards outlined in the methods section above. The proportion of studies that used these approaches differed by type, including all of the mixed methods studies, 92.3% of the qualitative studies, and 38.9% of the quantitative studies. Ways study teams sought to do research in a good way included: (1) involvement of Indigenous scholars on study teams; (2) engagement of a community advisory board; (3) inclusion of ceremony and involvement of Elders in the research process; and (4) contextualization of both health and risk in terms of the underlying determinants of Indigenous health, including self-determination, Indigenous wellness practices, colonization, trauma, and discrimination. A few studies were reviewed by Indigenous research ethics boards [50, 56, 76, 112, 113].
One star was awarded if the study incorporated Indigenous research standards, and a possible four stars could be awarded related to epidemiological quality (Fig. 4). One quantitative study achieved the highest level of quality both in terms epidemiological and Indigenous research standards with five stars [114] and five others were of very high quality with a total of four stars [111, 112, 115,116,117]. Emerging examples of epidemiological studies that seek to meet both standards for quality provide a model for the work ahead.
Discussion
This review provides a comprehensive summation of peer-reviewed evidence related to epidemiology and experiences of the HIV care cascade among Indigenous peoples in Australia, Canada, New Zealand and the United States. Taken together, the findings affirm that significant gaps remain in achieving universal engagement in HIV care among Indigenous peoples. Evidence suggests that improving IPHAs linkage and retention in care must include policies to improve cultural safety in client-provider relationships and support healthy coping after an HIV diagnosis. Supporting ART initiation and adherence requires that clinicians provide culturally-safe, non-judgmental care that builds on IPHAs existing support systems and addresses other health and wellness concerns alongside HIV. Further, it is essential that social and structural barriers that continue to impede Indigenous peoples from engaging all along the HIV cascade of care, including stigma and racism, trauma experiences, and intersecting health concerns, are taken into account in healthcare settings.
Both qualitative and quantitative studies highlight a disconnect between the clinical priorities embedded in the HIV cascade of care framework, and experiences of IPHAs’ HIV journey. For example, the framework conceptualizes HIV-related health within a biomedical paradigm, focused on achieving specific therapeutic outcomes. Although IPHAs may seek cascade-related services as a way of maintaining good health and prolonging life, these actions may not capture the full extent of their health-seeking behaviours [118, 119]. Inclusion of social, spiritual, emotional, cognitive, and daily life outcomes would create a more culturally-inclusive framework within which to understand and support the engagement of Indigenous peoples in HIV-related care. Further, a critical consideration in moving forward includes recognition that the inherent willingness of the 90-90-90 approach to leave a tenth of the population living with HIV behind is incompatible with Indigenous worldviews that emphasize a wholistic and inclusive approach to health and wellness [120]. Finally, the model would benefit from a reshaping of its very linear process, to one that reflects prolonged or re-engagement in one or more phases of the cascade. This could be presented as a series of loops within and between each phase of the model.
Almost 100 articles that address HIV cascade of care outcomes among Indigenous peoples were identified over the course of this review. Yet, many of these studies lack sufficient Indigenous-specific context to support culturally relevant interpretation of the data. Given the distinct social drivers of HIV among Indigenous peoples globally (e.g. historical and intergenerational trauma as well as stigma and racism) care must be taken in interpreting data related to Indigenous people’s prioritization of testing and treatment as well as their engagement in the cascade of care. Despite the volume of available data, results are mixed and do not paint a clear picture. Tremendous diversity within measures of cascade of care outcomes was observed across included studies. Standardizing measures for each phase of the cascade will create relevant benchmarks and improve our capacity to assess trends over time and place, vital for program and policy planning.
Many studies were excluded, as key findings were not disaggregated by Indigenous identity, meaning that disparities and unique experiences of Indigenous peoples may not be adequately captured. This might reflect attempts to avoid research that has been criticized for pathologizing Indigenous peoples by focusing on health disparities without adequate context. Indigenous-led analyses of population-level data, disaggregated by Indigenous identity are required to understand what proportion of Indigenous peoples are disengaging at each stage of the HIV care cascade.
Limitations
Indigenous peoples, identities, experiences, and cultures in Australia, Canada, New Zealand and the United States are diverse. As there is no single Indigenous culture or experience, it is important to avoid generalizations. This paper is one step towards conceptualizing an Indigenized cascade of care framework. It has omitted an essential area of evidence related to Indigenous people’s experiences of the HIV cascade, specifically, oral knowledge and wisdom held by Elders and traditional knowledge keepers. Additional work must be done to incorporate these voices in conceptualizing the HIV care cascade through an Indigenous lens. We have deliberately sought out evidence representing diverse research approaches and paradigms. As a result, the heterogeneity of the studies included here prevented us from conducting a meta-analysis. Caution is required when comparing the results of various studies. Differences between countries may reflect different healthcare models that affect access to healthcare and medications. They may also reflect changes in treatment guidelines within countries and over time. We cannot discount that this review may be biased by selection of studies. It is probable that informative data related to Indigenous people’s engagement in the HIV care cascade remain unpublished. As the authors are based in Canada, it is possible that this review is biased as a result of greater familiarity with Canadian research landscape, including related to Indigenous research ethics and methodologies. Included data likely underestimate the total number of IPHAs, as some studies excluded those who identify with multiple categories or grouped Indigenous with non-Indigenous peoples into a single category (e.g., Asian/Pacific Islander).
Conclusion
In sum, with the HIV cascade of care framework increasingly becoming the focus of global, national, and local HIV agendas, it is critical that the contexts of Indigenous peoples’ experiences of HIV are understood and accounted for. At present, considerable research exists related to HIV testing and diagnosis; however, much less is known about post-diagnosis experiences, particularly linkage to and retention in care. More work is required to ensure that the perspectives of Indigenous people living with HIV are reflected within the clinically-focused HIV cascade of care framework. What remains essential is that Indigenous peoples have access to culturally safe services at all stages of the HIV cascade of care.
Notes
A note about terminology: we have chosen to use the word Indigenous to refer broadly to the First Peoples of the lands and territories that are the focus of this paper. We acknowledge that Indigenous peoples globally are diverse, made up of many nations and communities. Where possible, we have tried to honour the identities of the Indigenous participants involved in the research summarized here by using specific names; however, this is not always possible, especially where data are aggregated. In these cases, we use the term “Indigenous”. We use “Indigenous peoples” when referring to a group of populations and “Indigenous people” when referring to an individual’s engagement with care. When referring to individual Indigenous people living with HIV we use the acronym IPHA.
We have attempted to avoid counting participants twice by adjusting for multiple articles published by the same study. However, it may be that some participants are represented in more than one study.
This spelling is explicit as it implies “whole” instead of “hole” (deficit focused), as recommended by Mi’kmaq Elder Murdena Marshall.
References
UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Lima VD, Hogg RS, Harrigan PR, Moore D, Yip B, Wood E, et al. Continued improvement in survival among HIV-infected individuals with newer forms of highly active antiretroviral therapy. Aids. 2007;21(6):685–92.
Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
UNAIDS. Ending AIDS: Progress towards the 90-90-90 targets. Geneva: Joint United Nations Programme on HIV/AIDS; 2017.
UNAIDS. The gap report. Geneva: Joint United Nations Programme on HIV/AIDS; 2014.
Papps E, Ramsden I. Cultural safety in nursing: the New Zealand experience. Int J Qual Health Care. 1996;8(5):491–7.
FNHA. It starts with me: FNHA’s policy statement on cultural safety and humility; 2016.
Health Council of Canada. Empathy, dignity and respect: creating cultural safety for aboriginal people in urban health care. Ottawa: Health Council of Canada; 2012.
Chansonneuve D. Reclaiming connections: understanding residential school trauma among aboriginal people. Ottawa: Aboriginal Healing Foundation; 2005.
Smith LT. Decolonizing methodologies: research and Indigenous peoples. New York: Zed books; 1999.
McKenzie HA, Dell CA, Fornssler B. Understanding addictions among Indigenous people through social determinants of health frameworks and strength-based approaches a review of the research literature from 2013 to 2016. Curr Addict Rep. 2016;3:1–9.
Duran E, Duran B, Yellow Horse Brave Heart M, Yellow Horse-Davis S. Healing the American Indian Soul Wound. In: Danieli Y, editor. International handbook of multigenerational legacies of trauma. New York: Plenum Press; 1998. p. 341–54.
Reading C. Chapter 1: Structural determinants of aboriginal peoples’ health. In: Greenwood M, de Leeuw S, Lindsay NM, Reading C, editors. Determinants of Indigenous peoples’ health: beyond the social. Toronto: Canadian Scholars’ Press; 2015. p. 1.
Reading CL, Wien F. Health inequalities and the social determinants of aboriginal peoples’ health. 2nd ed. Prince George: National Collaborating Centre for Aboriginal Health; 2013.
Adelson N. The embodiment of inequity. Can J Public Health. 2005;96(Supplement 2):545.
Negin J, Aspin C, Gadsden T, Reading C. HIV Among Indigenous peoples: a review of the literature on HIV-related behaviour since the beginning of the epidemic. AIDS Behav. 2015;19(9):1720–34.
Shea B, Aspin C, Ward J, Archibald C, Dickson N, McDonald A, et al. HIV diagnoses in indigenous peoples: comparison of Australia, Canada and New Zealand. Int Health. 2011;3(3):193–8.
Pala M. Comment. Canadian Aboriginal AIDS Network Wise Practices V; Vancouver; 2015.
Xiao Y, Watson M. Guidance on conducting a systematic literature review. J Plan Educ Res. 2017. https://doi.org/10.1177/0739456X17723971.
Duncan KC, Reading C, Borwein AM, Murray MC, Palmer A, Michelow W, et al. HIV incidence and prevalence among aboriginal peoples in Canada. AIDS Behav. 2011;15(1):214–27.
Nowgesic EF. Antiretroviral therapy access, acceptance and adherence among urban Indigenous peoples living with HIV in Saskatchewan: the Indigenous red ribbon storytelling study. Toronto: University of Toronto; 2015.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):65.
Green S, Higgins J, editors. Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011]; 2011.
Noyes J, Lewin S. Chapter 6: supplemental guidance on selecting a method of qualitative evidence synthesis, and integrating qualitative evidence with cochrane intervention reviews. In: Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, et al., editors. Supplementary guidance for inclusion of qualitative research in cochrane systematic reviews of interventions. 1: Cochrane collaboration qualitative methods group; 2011.
Pearson A. Balancing the evidence: incorporating the synthesis of qualitative data into systematic reviews. JBI Rep. 2004;2(2):45–64.
McDonald E, Priest N, Doyle J, Bailie R, Anderson I, Waters E. Issues and challenges for systematic reviews in indigenous health. J Epidemiol Community Health. 2010;64(7):643–4.
Chambers LA, Jackson R, Worthington C, Wilson CL, Tharao W, Greenspan NR, et al. Decolonizing scoping review methodologies for literature with, for, and by indigenous peoples and the African diaspora: dialoguing with the tensions. Qual Health Res. 2017;28:175.
Flicker S, O’Campo P, Monchalin R, Thistle J, Worthington C, Masching R, et al. Research done in “a good way”: the importance of indigenous elder involvement in HIV community-based research. Am J Public Health. 2015;105(6):e1–6.
Wilson S. Research is ceremony: indigenous research methods. Winnipeg: Fernwood Publishing; 2008.
Kovach M. Indigenous methodologies: characteristics, conversations, and contexts. Toronto: University of Toronto Press; 2009. p. 201.
Absolon KEM. Kaandosswin: how we come to know. Winnipeg: Fernwood Publishing; 2011.
Castellano MB. Ethics of aboriginal research. Int J Indig Health. 2004;1(1):98.
Schnarch B. Ownership, control, access, and possession (OCAP) or self-determination applied to research. J Aborig Health. 2004;1(1):80–95.
Loppie C. Learning from the grandmothers: incorporating Indigenous principles into qualitative research. Qual Health Res. 2007;17(2):276–84.
Ermine W, Sinclair R, Jeffery B. The ethics of research involving Indigenous peoples. Saskatoon: Indigenous Peoples’ Health Research Centre; 2004.
Ermine W. The ethical space of engagement. Indig Law J. 2007;6(1):193.
Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2014.
McCall J, Browne AJ, Reimer-Kirkham S. Struggling to survive: the difficult reality of aboriginal women living with HIV/AIDS. Qual Health Res. 2009;19(12):1769–82.
Cain R, Jackson R, Prentice T, Collins E, Mill J, Barlow K. The experience of HIV diagnosis among aboriginal people living with HIV/AIDS and depression. Qual Health Res. 2013;23(6):815–24.
Mill JE. Describing an explanatory model of HIV illness among aboriginal women. Holist Nurs Pract. 2000;15(1):42–56.
Ka’opua L. Treatment adherence to an antiretroviral regime: the lived experience of Native Hawaiians and kokua. Pac Health Dialog. 2001;8(2):290–8.
Mill (b) J, Keenan L, Lambert D, Larkin K, Ward K. “I can’t deal with this alone”: support for Aboriginal men and women living with HIV. Can J Aborig Community-Based HIV/AIDS Res. 2008; Supplemental Edition—Winter 2008.
Barlow K, Loppie C, Jackson R, Akan M, MacLean L, Reimer G. Culturally competent service provision issues experienced by aboriginal people living with HIV/AIDS. Pimatisiwin J Aborig Indig Community Health. 2008;6(2):155.
Mill JE, Lambert DT, Larkin K, Ward K, Harrowing JN. Challenging lifestyles aboriginal men and women living with HIV. Pimatisiwin J Aborig Indig Community Health. 2008;5(2):151–73.
Reading C, Brennan R, Masching R. Cultural concepts of care among aboriginal people living with HIV and AIDS: a study by the Canadian aboriginal AIDS network. Can J Aborig Community-Based HIV/AIDS Res. 2013;5:24–37.
Bucharski D, Reutter LI, Ogilvie LD. “You need to know where we’re coming from”: Canadian aboriginal women’s perspectives on culturally appropriate HIV counseling and testing. Health Care Women Int. 2006;27(8):723–47.
Chongo M, Lavoie JG, Hoffman R, Shubair M. An investigation of the determinants of adherence to highly active anti-retroviral therapy (HAART) in aboriginal men in the downtown eastside (DTES) of Vancouver. Can J Aborig Community-Based HIV/AIDS Res. 2011;4:32.
Truth and Reconciliation Commission of Canada. Honouring the truth, reconciling for the future: summary of the final report of the truth and reconciliation commission of Canada. Winnipeg: The Truth and Reconciliation Commission of Canada; 2015.
Thompson SC, Bonar M, Greville H, Bessarab D, Gilles MT, D’Antoine H, et al. “Slowed right down”: insights into the use of alcohol from research with aboriginal Australians living with HIV. Int J Drug Policy. 2009;20(2):101–10.
Sazegar P, Tu D, Littlejohn D, Myran A. Perspectives of Canadian inner city aboriginal and non-aboriginal people living with HIV and AIDS. Can J Aboriginal Community-Based HIV/AIDS Res. 2013;5:40–56.
Barlow JK. Examining HIV/AIDS among the aboriginal population in Canada in the post-residential school era. Ottawa: Aboriginal Healing Foundation; 2003.
Mill JE, Wong T, Archibald C, Sommerfeldt S, Worthington C, Jackson R, et al. AIDS is something scary: Canadian aboriginal youth and HIV testing. Pimatisiwin J Aborig Indig Community Health. 2011;9(2):277–99.
McCall J, Lauridsen-Hoegh P. Trauma and cultural safety: providing quality care to HIV-infected women of aboriginal descent. J Assoc Nurs AIDS Care. 2014;25(1):S70–81.
Nowgesic E, Meili R, Stack S, Myers T. The Indigenous red ribbon storytelling study: what does it mean for Indigenous peoples living with HIV and a substance use disorder to access antiretroviral therapy in Saskatchewan? Can J Aborig Community-Based HIV/AIDS Res. 2015;7(1):27.
Duran B, Harrison M, Shurley M, Foley K, Morris P, Davidson-Stroh L, et al. Tribally-driven HIV/AIDS health services partnerships: evidence-based meets culture-centered interventions. J HIV/AIDS Soc Serv. 2010;9(2):110–29.
Lux MK. Separate beds: a history of indian hospitals in Canada, 1920s–1980s. Toronto: University of Toronto Press; 2016.
Allan B, Smylie J. First peoples, second class treatment: the role of racism in the health and well-being of Indigenous peoples in Canada. Toronto: The Wellesley Institute; 2015.
Mosby I. Administering colonial science: nutrition research and human biomedical experimentation in Aboriginal communities and residential schools, 1942–1952. Soc Hist. 2013;46(1):145–72.
Geddes G. Medicine unbundled: a journey through the minefields of indigenous health care. Vancouver: Heritage House Publishing Co; 2017.
Masching R, Dell CA, Egan JP, McHugh NGL, Lee D, Prentice T, et al. The complexities of accessing care and treatment understanding alcohol use by aboriginal persons living with HIV and AIDS. Can J Aborig Community-based HIV/AIDS Res. 2014;6:70.
Burks DJ, Robbins R, Durtschi JP. American Indian gay, bisexual and two-spirit men: a rapid assessment of HIV/AIDS risk factors, barriers to prevention and culturally-sensitive intervention. Cult Health Sex. 2011;13(3):283–98.
Mill J, Jackson R, Worthington CA, Archibald CP, Wong T, Myers T, et al. HIV testing and care in Canadian aboriginal youth: a community based mixed methods study. BMC Infect Dis. 2008;8:13.
Marshall M, Marshall A, Bartlett C. Two-eyed seeing in medicine. In: Greenwood M, de Leeuw S, Lindsay NM, Reading C, editors. Determinants of Indigenous peoples’ health: beyond the social. Toronto: Canadian Scholars’ Press; 2015. p. 1.
Newman CE, Bonar M, Greville HS, Thompson SC, Bessarab D, Kippax SC. Barriers and incentives to HIV treatment uptake among aboriginal people in Western Australia. AIDS. 2007;21(Suppl 1):S13–7.
Prentice T, Mill J, Archibald CP, Sommerfeldt S, Worthington C, Jackson R, et al. Aboriginal youth experiences of accessing HIV Care and Treatment. J HIV/AIDS Soc Serv. 2011;10(4):395–413.
Ha S, Paquette D, Tarasuk J, Dodds J, Gale-Rowe M, Brooks JI, et al. A systematic review of HIV testing among Canadian populations. Can J Public Health. 2014;105(1):e53–62.
Denny CH, Holtzman D, Cobb N. Surveillance for health behaviors of American Indians and Alaska natives. Findings from the behavioral risk factor surveillance system, 1997–2000. Surveill Summ (Washington, DC: 2002). 2003;52(7):1–13.
Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the American Indian or Alaska native adult population: United States, 2004–2008. Natl Health Stat Rep. 2010;20:1–22.
Sawleshwarkar S, Harrison C, Britt H, Mindel A. Determinants of HIV testing. Sex Transm Infect. 2011;87(5):426–32.
Kwan KSH, Giele CM, Combs B, Mak DB. Improvement in antenatal testing for sexually transmissible infections and blood-borne viruses in Western Australian hospitals, 2007 to 2010. Sex Health. 2012;9(4):349–54.
Ford CL, Godette DC, Mulatu MS, Gaines TL. Recent HIV testing prevalence, determinants, and disparities among US older adult respondents to the behavioral risk factor surveillance system. Sex Transm Dis. 2015;42(8):405–10.
Bauer GR, Travers R, Scanlon K, Coleman TA. High heterogeneity of HIV-related sexual risk among transgender people in Ontario, Canada: a province-wide respondent-driven sampling survey. BMC Public Health. 2012;12:292.
Mak DB, Murray JC, Bulsara MK. Antenatal screening for sexually transmitted infections in remote Australia. Aust N Z J Obstet Gynaecol. 2003;43(6):457–62.
Plitt SS, Mihalicz D, Singh AE, Jayaraman G, Houston S, Lee BE. Time to testing and accessing care among a population of newly diagnosed patients with HIV with a high proportion of Canadian Aboriginals, 1998–2003. AIDS Patient Care STDs. 2009;23(2):93–9.
Paquette D, McEwan M, Bryant J. Risk practices among aboriginal people who inject drugs in New South Wales, Australia. Aids Behav. 2013;17(7):2467–73.
Connor J, Paul C, Sharples K, Dickson N. Patterns of disease and HIV testing at sexually transmitted disease clinics. N Z Med J. 1997;110(1057):452–5.
International Advisory Panel on HIV Care Continuum Optimization. IAPAC Guidelines for optimizing the HIV care continuum for adults and adolescents. J Int Assoc Provid AIDS Care. 2015;14(1 suppl):S3–34.
Kronfli N, Lacombe-Duncan A, Wang Y, de Pokomandy A, Kaida A, Logie C, et al. Access and engagement in HIV care among a national cohort of women living with HIV in Canada. AIDS Care. 2017;29(10):1235–42.
Dickson NP, McAllister S, Sharples K, Paul C. Late presentation of HIV infection among adults in New Zealand: 2005–2010. HIV Med. 2012;13(3):182–9.
Diamond C, Davidson A, Sorvillo F, Buskin S. HIV-infected American Indians/Alaska natives in the Western United States. Ethn Dis. 2001;11(4):633–44.
Connel C, Stroup JS, Stephens JR, Martin E. Characteristics of native Americans with HIV and implications for care. Baylor Univ Med Cent Proc. 2014;27(2):103–5.
Rachlis B, Burchell AN, Gardner S, Light L, Raboud J, Antoniou T, et al. Social determinants of health and retention in HIV care in a clinical cohort in Ontario, Canada. AIDS Care. 2017;29(7):828–37.
Mitsch A, Babu AS, Seneca D, Whiteside YO, Warne D. HIV care and treatment of American Indians/Alaska natives with diagnosed HIV infection-27 states and the District of Columbia, 2012. Int J STD AIDS. 2017;28(10):953–61.
Nwangwu-Ike N, Hernandez AL, An Q, Huang TY, Hall HI. The epidemiology of human immunodeficiency virus infection and care among adult and adolescent females in the United States, 2008–2012. Womens Health Issues. 2015;25(6):711–9.
Martin LJ, Houston S, Yasui Y, Wild TC, Saunders LD. Rates of initial virological suppression and subsequent virological failure after initiating highly active antiretroviral therapy: the impact of aboriginal ethnicity and injection drug use. Curr HIV Res. 2010;8(8):649–58.
Templeton DJ, Wright ST, McManus H, Lawrence C, Russell DB, Law MG, et al. Antiretroviral treatment use, co-morbidities and clinical outcomes among aboriginal participants in the Australian HIV observational database (AHOD). BMC Infect Dis. 2015;15(1):326–8.
Grinsztejn B, Hosseinipour MC, Ribaudo HJ, Swindells S, Eron J, Chen YQ, et al. Effects of early versus delayed initiation of antiretroviral treatment on clinical outcomes of HIV-1 infection: results from the phase 3 HPTN 052 randomised controlled trial. Lancet Infect Dis. 2014;14(4):281–90.
INSIGHT START Study Group. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;5:4. https://doi.org/10.1056/nejmoa1506816.
Grierson J, Pitts M, Rua’ine G, Hughes AJ, Saxton PJ, Whyte M, et al. Mate Aaraikore A Muri Ake Nei: experiences of Maori New Zealanders living with HIV. Sex Health. 2004;1(3):175–80.
Wood E, Montaner JS, Tyndall MW, Schechter MT, O’Shaughnessy MV, Hogg RS. Prevalence and correlates of untreated human immunodeficiency virus type 1 infection among persons who have died in the era of modern antiretroviral therapy. J Infect Dis. 2003;188(8):1164–70.
Wood E, Kerr T, Palepu A, Zhang R, Strathdee SA, Tyndall MW, et al. Slower uptake of HIV antiretroviral therapy among Aboriginal injection drug users. J Infect. 2006;52(4):233–6.
Milloy M, King A, Kerr T, Adams E, Samji H, Guillemi S, et al. Improvements in HIV treatment outcomes among indigenous and non-indigenous people who use illicit drugs in a Canadian setting. J Int AIDS Soc. 2016;19(1):20617.
Jaworsky D, Benoit A, Raboud J, O’Brien-Teengs D, Blitz S, Rourke SB, et al. Comparison of coping strategies and supports between aboriginal and non-aboriginal people living with HIV in Ontario. AIDS Care. 2016;28(1):63–9.
Nachega JB, Hislop M, Dowdy DW, Chaisson RE, Regensberg L, Maartens G, et al. Adherence to nonnucleoside reverse transcriptase inhibitor-based HIV therapy and virologic outcomes. Ann Intern Med. 2007;146(8):564.
Samji H, Chen Y, Salters K, Montaner JS, Hogg RS. Correlates of unstructured antiretroviral treatment interruption in a cohort of HIV-positive individuals in British Columbia. AIDS Behav. 2014;18(11):2240–8.
Samji H, Taha TE, Moore D, Burchell AN, Cescon A, Cooper C, et al. Predictors of unstructured antiretroviral treatment interruption and resumption among HIV-positive individuals in Canada. HIV Med. 2015;16(2):76–87.
Wang L, Min JE, Zang X, Sereda P, Harrigan RP, Montaner JSG, et al. Characterizing Human immunodeficiency virus antiretroviral therapy interruption and resulting disease progression using population-level data in British Columbia, 1996–2015. Clin Infect Dis. 2017;65(9):1496–503.
Puskas CM, Kaida A, Miller CL, Zhang W, Yip B, Pick N, et al. The adherence gap: a longitudinal examination of men’s and women’s antiretroviral therapy adherence in British Columbia, 2000–2014. AIDS. 2017;31(6):827–33.
Ka’opua LSI, Mueller CW. Treatment adherence among native Hawaiians living with HIV. Soc Work. 2004;49(1):55–63.
Lima VD, Kretz P, Palepu A, Bonner S, Kerr T, Moore D, et al. Aboriginal status is a prognostic factor for mortality among antiretroviral naı̈ve HIV-positive individuals first initiating HAART. AIDS Res Ther. 2006;3(1):14.
Gunther M, Foisy M, Houston S, Guirguis L, Hughes C. Treatment beliefs, illness perceptions, and non-adherence to antiretroviral therapy in an ethnically diverse patient population. Int J Clin Pharm. 2014;36(1):105–11.
Miller C, Spittal P, Wood E, Chan K, Schechter M, Montaner J, et al. Inadequacies in antiretroviral therapy use among aboriginal and other Canadian populations. AIDS Care. 2006;18(8):968–76.
Montaner J, Guillemi S, Harris M. Therapeutic guidelines antiretroviral (ARV) treatment of adult HIV infection. BC Centre for Excellence in HIV/AIDS; 2013.
Antiretroviral Therapy Cohort Collaboration. Influence of geographical origin and ethnicity on mortality in patients on antiretroviral therapy in Canada, Europe, and the United States. Clin Infect Dis. 2013;56(12):1800–9.
Gilles MT, Dickinson JE, Cain A, Turner KA, McGuckin R, Loh R, et al. Perinatal HIV transmission and pregnancy outcomes in indigenous women in Western Australia. Aust N Z J Obstet Gynaecol. 2007;47(5):362–7.
Martin LJ, Houston S, Yasui Y, Wild TC, Saunders LD. All-cause and HIV-related Mortality rates among HIV-infected patients after initiating highly active antiretroviral therapy: the impact of aboriginal ethnicity and injection drug use. Can J Public Health. 2011;102(2):90–6.
Cescon A, Kanters S, Brumme CJ, Lepik KJ, Forrest JI, Hull M, et al. Trends in plasma HIV-RNA suppression and antiretroviral resistance in British Columbia, 1997–2010. J Acquir Immune Defic Syndr. 2014;65(1):107–14.
Lefebvre ME, Hughes CA, Yasui Y, Saunders LD, Houston S. Antiretroviral treatment outcomes among foreign-born and aboriginal peoples living with HIV/AIDS in northern Alberta. Can J Public Health. 2014;105(4):E251–7.
Erickson A, Becker M, Shaw S, Kasper K, Keynan Y. Substance use and its impact on care outcomes among HIV-infected individuals in Manitoba. AIDS Care. 2015;27(9):1168–73.
Benoit AC, Younger J, Beaver K, Jackson R, Loutfy M, Masching R, et al. A comparison of virological suppression and rebound between Indigenous and non-Indigenous persons initiating combination antiretroviral therapy in a multisite cohort of individuals living with HIV in Canada. Antiviral Ther. 2017;22(4):325–35.
Gorgos L, Avery E, Bletzer K, Wilson C. Determinants of survival for native American adults with HIV infection. AIDS Patient Care STDs. 2006;20(8):586–94.
Williams R, Lawrence C, Wilkes E, Shipp M, Henry B, Eades S, et al. Sexual behaviour, drug use and health service use by young Noongar people in Western Australia: a snapshot. Sex Health. 2015;12(3):188–93.
Miller PJ, Torzillo PJ. Private business: the uptake of confidential HIV testing in remote aboriginal communities on the Anangu Pitjantjatjara Lands. Aust N Z J Public Health. 1998;22(6):700–3.
Orchard TR, Druyts E, McInnes CW, Clement K, Ding E, Fernandes KA, et al. Factors behind HIV testing practices among Canadian aboriginal peoples living off-reserve. AIDS Care. 2010;22(3):324–31.
Iralu J, Duran B, Pearson CR, Jiang YZ, Foley K, Harrison M. Risk factors for HIV disease progression in a rural Southwest American Indian population. Public Health Rep. 2010;125:43–50.
Benoit AC, Younger J, Beaver K, Jackson R, Loutfy M, Masching R, et al. Increased mortality among Indigenous persons in a multisite cohort of people living with HIV in Canada. Can J Public Health. 2017;108(2):E169–75.
Pawluch D, Cain R, Gillett J. Lay constructions of HIV and complementary therapy use. Soc Sci Med. 2000;51(2):251–64.
Paparini S, Rhodes T. The biopolitics of engagement and the HIV cascade of care: a synthesis of the literature on patient citizenship and antiretroviral therapy. Crit Public Health. 2016;26:1–17.
Poitras M. Audience comment. 25th Annual Canadian Conference on HIV/AIDS Research; Winnipeg, Manitoba; 2016.
Acknowledgements
We are grateful for the guidance of the Cedar Project Partnership: Elders Violet Bozoki (Lheidli T’enneh) and Earl Henderson (Métis/Cree); Vancouver Native Health Society; Red Road HIV/AIDS Network; Canadian Aboriginal AIDS Network; Carrier Sekani Family Services; Positive Living North; Prince George Friendship Centre; All Nations Hope; Splatsin, Neskonlith and Adams Lake Indian Bands. Thank you also to Ursula Ellis, reference librarian at UBC's Woodward Library, for help developing the search strategy.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Ethical Approval
This article involves a review of published studies and therefore does not contain any studies with human participants performed by any of the authors for this publication. Author CL was an author involved in two of the 93 articles selected for inclusion, both of which were conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Cedar Project Partnership are listed in the acknowledgements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Jongbloed, K., Pooyak, S., Sharma, R. et al. Experiences of the HIV Cascade of Care Among Indigenous Peoples: A Systematic Review. AIDS Behav 23, 984–1003 (2019). https://doi.org/10.1007/s10461-018-2372-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2372-2