Abstract
The updated National HIV/AIDS Strategy recommends widespread HIV education and testing and calls the faith community to assist in these efforts. Yet, limited information exist on church-based HIV testing interventions. This study examined feasibility and assessed HIV testing outcomes of Taking It to the Pews (TIPS), a multilevel HIV education and testing intervention. Four African American churches were matched and randomized to TIPS or a standard-information control arm. Intervention churches delivered the religiously-tailored TIPS Tool Kit, which included educational materials to individuals and ministry groups; pastoral activities (e.g., sermons preached, receipt of HIV testing role-modeled), responsive readings, and church bulletin inserts in church services; and HIV testing during church services and church outreach events. All churches delivered 2–3 tools/month and coordinated 3 HIV testing events. At 12 months, significant increases in receipt of HIV testing (59% vs. 42%, p = 0.008), and particularly church-based testing (54% vs. 15%, p < 0.001), relative to controls were found. TIPS has great potential to increase reach, feasibility, and impact of HIV testing in African American churches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A key goal of the updated National HIV/AIDS Strategy’s (NHAS) is to increase the percentage of Americans who are aware of their HIV-positive status to 90% by 2020 [1], which means that nearly all citizens will need to be aware of their HIV status. To accomplish this important goal and ensure early treatment for those who test positive, the NHAS recommends widespread HIV/STD education and testing, especially in high risk communities. This may be especially important for African Americans, who continue to be overrepresented among all new HIV cases [2].
Although African Americans report higher lifetime HIV testing rates compared to Whites in national studies (up to 68% vs. 49%, respectively) [2,3,4], receipt of routine HIV testing remains low and those who are unaware of their HIV infection may significantly contribute to the disproportionately high rates of HIV among African Americans by unknowingly infecting others. In 2006, CDC updated the HIV testing guidelines to include routine screening of individuals aged 13–64 in medical settings [5]. However, many African Americans have limited access to healthcare, tend to mistrust health professionals, often do not perceive themselves to be at risk, and may have limited transportation to other HIV testing sites [6,7,8,9]. Also, social barriers, such as HIV stigma and lack of support for HIV testing from significant others and health professionals, may hamper access to and receipt of HIV testing among African Americans [9,10,11].
A promising strategy to increase HIV education and testing among African Americans is to offer HIV services in African American churches. Of note, the NHAS calls on the faith-based sector to play a role in disseminating culturally-appropriate and destigmatizing HIV education and prevention approaches. Churches may be an ideal setting because they: are trusted sources of social support for church and community members; have multilevel church-wide, ministry group, and interpersonal communication outlets; have volunteer and space capacity that could facilitate intervention delivery; and have outreach ministries (e.g., food/clothing pantries, social services, recovery programs) that serve community members who may be at greatest risk for HIV [12,13,14]. Notably, over 50% of African Americans attend church weekly [15], providing ample opportunities for ongoing delivery of and exposure to wide-reaching church-based HIV education and testing interventions.
Despite a growing number of studies that have reported on delivery of HIV education in African American churches, only a few have reported on African American churches’ delivery of HIV testing services [16,17,18,19]. These reports have been case studies on churches’ ability to provide HIV education and testing to church and/or community members with only aggregate numbers of persons tested reported. Yet, these studies did not: employ theoretically-guided designs, describe participants and track their receipt of HIV testing longitudinally, identify and track theoretical factors longitudinally, or use multilevel approaches to increase reach and influence on uptake of HIV testing—and therefore did not provide experimental and theoretical information on uptake of HIV testing behavior. Additionally, no previous studies have clearly described how churches were engaged in coordination of church-based HIV testing events. As a recent exception, Derose et al. conducted a randomized church-based pilot intervention theoretically-designed to reduce HIV stigma through educational seminars, pastoral sermons on compassion for people living with HIV, and testing events with 3 Latino and 2 African American churches. HIV testing rates in the African American intervention church were significantly greater than its matched control church (32% vs. 13%, p < 0.001) at 6 months [20]. While these findings are promising, investigators were unable to match pretest and posttest participant surveys, theoretical factors guiding intervention design were not examined, and community members using church outreach ministries were not included. Also, exposure to intervention components was not tracked.
In addressing the limitations in the prior studies, we report on HIV testing outcomes of Taking It to the Pews II (hereafter referred to as TIPS), a theoretically-guided, religiously-tailored, multilevel HIV testing intervention in African American churches. The same participants were followed longitudinally and included church members and community members served through church outreach ministries (e.g., food/clothing pantries, social services). Using a community-based participatory approach (CBPR) with African American faith leaders, TIPS’ delivered was based on the socio-ecological model [21] to coincide with naturalistic, multilevel activities in African American churches. The design was guided by theory of planned behavior (TPB) constructs (attitudinal, normative, control beliefs, and intentions) [22], which were assessed at each time point. It was hypothesized that TIPS would lead to higher HIV testing rates at 6 and 12 months as well as enhancements in the TPB constructs regarding receipt of an HIV test. TIPS was compared to a multilevel HIV education control intervention, which was less intensive and non-tailored, to determine its relative efficacy. We report on TIPS theoretically-guided HIV testing outcomes. We also report on feasibility outcomes, including the reach of participating churches to broad segments of the African American community, intervention implementation by church leaders, and participants’ exposure and satisfaction with the intervention. Additionally, we describe how church members worked collaboratively with health agency partners to coordinate and implement their church’s HIV testing events.
Methods
Our primary outcome was self-reported receipt of HIV testing (tested vs. not tested) among church members and community members who used church outreach services at 6 and 12 months. A cluster randomized controlled trial of the TIPS intervention versus an attention-matched control intervention in 4 African American churches was conducted in the Kansas City (KC), MO and KS urban areas. Churches were matched on size (membership attendance and outreach ministry) and randomized to intervention or control arms. Churches were randomized by the study statistician using a computer-generated randomization sequence. All churches were asked to hold 3 church-based HIV testing events (2 during church services and 1 during an outreach ministry service activity) over a 12-month period. HIV testing was available and free to all church and community members; however, intervention impact was tracked only among church and community members who completed pretest and follow-up survey assessments.
Participating Churches
Calvary Community Outreach Network (CCON), a faith-based organization that provides health promotion programming and assists churches in building health ministries, assisted in the church recruitment process for this study. Pastors of churches thought likely to meet eligibility criteria were contacted by CCON and were asked to meet with study staff to discuss the study. Study staff then met with the pastors to determine if they were interested in their church participating in the study and if their church met selection criteria for study participation. Church selection criteria included having: (a) a minimum of 150 African American adult church members; (b) a pastor willing to commit to study implementation by signing a memorandum of agreement that detailed all church study implementation activities; (c) 2 church members wiling to serve as church health liaisons (CHLs) to coordinate study implementation in their church; and (d) an active outreach ministry (e.g., recovery programs, food pantries, clothing programs) serving at least 50 community members monthly. All participating churches received $3000 to: (a) host study activities and assist with participant recruitment and retention and (b) provide $250 stipends to each of the 2 CHLS for participating in study trainings, delivering study activities, and reporting implementation data via an online system. Each church also received support for a technology enhancement (either a telephone messaging system or digital projector and screen; valued at about $900) to assist intervention delivery and maintenance.
Participants
Church members were recruited by study staff who provided study information during and after church services. Community members were recruited similarly during participating churches’ outreach ministry events. All were aged 18–64 years, willing to participate in 3 survey assessments (30–40 min each; baseline, 6 months, and 12 months), and willing to provide 2 phone numbers. All participants were consented prior to completing baseline surveys. To increase confidentiality, participants created a unique study ID code that they could reproduce at each assessment by answering a series of questions. Participants received $10 and promotional items (e.g., t-shirts, coffee mugs) for completing each survey. Study procedures were approved by the University of Missouri-KC Institutional Review Board.
TIPS Intervention Background, Theoretical Conceptualization, and Multilevel Description
Led by CCON, KC has a long-running National Church Week of Prayer (NCWP; formerly Black Church Week of Prayer) for the Healing of AIDS initiative, which occurs the first week of March each year. Many of the NCWP pastors expressed interest in delivering HIV-related activities in their churches beyond the NCWP, but also expressed challenges in doing so due to limited training, resources, and religiously-appropriate materials. Through collaborative efforts with CCON, our CBPR approach engaged NCWP African American faith leaders and health agency partners in all phases of the research process, including determining the research agenda (i.e., HIV testing as an appropriate church-based prevention strategy) and participating in TIPS intervention development, implementation, evaluation, interpretation, and dissemination of findings.
Development and delivery of TIPS intervention materials/activities was guided by the social-ecological model [21] and the TPB [22]. The TPB posits that attitudinal beliefs, subjective norms, and perceived behavioral control predict behavioral intentions to engage in a particular behavior (e.g., HIV testing), and intentions ultimately predict whether a person will engage in the behavior. For example, TPB-guided TIPS materials/activities included sermon guides to assist pastors in sharing accurate, myth-correcting information about HIV and encouraging members to get an HIV test to shift attitudinal and normative beliefs. Also, HIV testing events were coordinated by CHLs, held during church services and outreach events, and were free to anyone who wanted to get tested to shift behavioral control beliefs. The social-ecological model posits that behavior change becomes attainable and sustainable for more people when barriers are reduced and supportive mechanisms are built using strategies that have overlapping influence on individual, group, organizational, and community level factors. Use of this model aligns with public health interest in structural HIV interventions that are designed to be multilevel, build capacity within existing infrastructure, increase reach, and are context-driven, culturally appropriate, and sustainable through ongoing community engagement. Accordingly, the collaborative faith-health-academic team designed TIPS religiously-tailored, supportive materials/activities to fit naturally within existing church activities for delivery by trained church members through multilevel (i.e., individual/peer-to-peer, ministry groups, church services, community outreach ministries) church outlets.
Faith leaders assisted in developing content and selecting relevant scriptural references for many of the religiously-tailored intervention materials/activities (e.g., sermon guides, responsive readings, video testimonials, resource cards, educational games) and identifying multilevel delivery formats. They reviewed all intervention materials/activities for church-appropriateness. Health agency partners reviewed materials for HIV information accuracy. The intervention materials/activities were packaged in the TIPS HIV Tool Kit, which contained nearly 40 culturally-religiously-tailored “tools.” A case study on a formative phase of TIPS found that delivery of the tools was highly feasible [17].
The collaborative faith-health-academic team also developed procedures to efficiently and appropriately deliver HIV testing events during church services and outreach ministry activities, which resulted in a TIPS HIV testing event checklist and an accompanying HIV testing event church request form. The checklist included: (a) steps to use the HIV testing event request form, (b) strategies to encourage church and community members to get tested at church-based screening events (e.g., pastor modeling receipt of testing, ministry group leaders volunteering to get tested first, health agency staff reviewing the testing process during church services and community events, members’ testimonials on getting tested); (c) a guide on how to setup the testing space; and (d) procedures on how to get their church’s aggregate number of tests performed and positives found from health agency partners. The HIV testing event church request form was adapted from an existing KCMO Health Department form for specific TIPS use. TIPS CHLs submitted the form to partnering health agencies with requested dates/times for the events, goals on number of members to get tested, and other relevant activities that would or would not be allowed (e.g., review of testing process during church services; tests for gonorrhea, chlamydia, syphilis; condom distribution). Health agency partners used this information to plan for an appropriate number of staff members, test kits, and other needed materials for the church-based HIV testing events. They also worked closely with our health partners’ evidence-based linkage to care program [23], to ensure anyone who tested positive for HIV (and anyone who disclosed they were positive but not in care) received needed HIV services.
Two members from each participating church served as CHLs and participated in 4 study trainings—2 prior to start of the study arms’ activities and 2 during the 12-month study, on HIV facts, study design, and how to coordinate delivery of their respective study arm’s materials/activities, HIV testing events, and survey data collection events in their church. To launch the TIPS intervention, CHLs coordinated their church’s TIPS Kick-off event, which was held during a Sunday morning service and included a TIPS sermon, responsive reading, church bulletin insert(s), testimonial, and church fan along with the first HIV testing event. CHLs were asked to coordinate 2 additional HIV testing events, for a total of 3 testing events, and to deliver 2 TIPS tools/month over 12 months through multilevel church outlets described below.
Individual/Interpersonal Level Activities
Automated Telephone Message Reminders and Encouragement for HIV Testing
Automated church phone messaging systems facilitated delivery of HIV testing event (and survey event) reminders to church and community members. Telephone reminders included messages to increase motivation, intention, and commitment to seek HIV screening. Also, during their natural interpersonal contacts with members, CHLs and pastors encouraged members to get tested for HIV.
HIV Print Materials
Brochures with HIV facts, risk checklists, and resource information were provided to church and community members from CHLs manning HIV resource tables.
Ministry Group Level Activities
Role Model Testimonials, Educational Games, and Videos
HIV risk reduction education was conducted with church ministry groups (e.g., singles, young adults, women, men) and outreach ministry groups. CHLs and ministry group leaders used printed role model testimonials, interactive education games (i.e., HIV testing and HIV basics games based on a Jeopardy-type format, Wheel of HIV Awareness), and accompanying facilitator guides to lead discussions on HIV testing and risk behaviors.
Church-Wide Level Activities
HIV Testing Events During Church Services
CHLs coordinated their church-based HIV testing events by first notifying local health agencies using the TIPS HIV testing event form to request specific HIV education and testing services. Each church agreed to hold an HIV testing event during the TIPS Kick-off church service and another testing event during a special church service (e.g., a choir extravaganza day). CHLs used the TIPS testing event checklist to normalize and de-stigmatize getting an HIV test during these services. The checklist included having: congregants read in unison about the impact of HIV on the African American community using the responsive reading tool, church leaders model getting tested for HIV as health agency staff described the test kit and testing process in front of congregants during the church service, and congregants celebrate the number of HIV tests completed. To reduce stigma and fear associated with testing positive for HIV, people living with HIV gave their testimonies on the importance of knowing one’s HIV status, maintaining their HIV care, and the effectiveness of HIV medications and healthy lifestyles in improving their quality and length of life. Church-level HIV testing events were held just prior to, during, and immediately after church services in a designated church area. Rapid HIV testing was provided by 4–5 staff members from local health agency partners following testing procedures per CDC quality assurance guidelines. Results were provided in about 20 min in private rooms.
Pastor-Led Activities
Pastors delivered at least 3 sermon messages and pulpit comments on HIV testing, risk and stigma reduction, and compassion for people living with HIV with the assistance of sermon guide and pastoral observation tools. Also, pastors received an HIV test during church and special event services in front of congregants and encouraged congregants to get tested.
Printed and Video HIV Educational Materials
CHLs with the assistance of church ushers delivered HIV Tool Kit educational materials to church members during church services and from resource tables. These materials included responsive readings (e.g., akin to liturgical readings with call-response formats to empower and unify members in fighting HIV and in promoting tested), church bulletin inserts and brochures (e.g., HIV Basics, HIV and Women, HIV Myths and Facts), posters, fact sheets, resource cards, bible bookmarks, and church fans. Also, 5-min testimonial videos on faith leaders’ decisions to get tested for HIV and a 20-min video depicting issues related to HIV stigma and the Black church were shown to increase motivation for testing and compassion for people living with HIV.
Community Level Activities
HIV Testing During Outreach Ministry Community Events
CHLs worked with church outreach ministry leaders to hold 1 HIV testing event during outreach ministry (e.g., food/clothing pantries, recovery programs, social services) or community events (e.g., health fairs, back-to-school fairs, national HIV awareness days) to be accessible to community members. Outreach ministry testing events followed similar procedures used in the church services with 4–5 staff members from local health agency partners providing rapid HIV tests. Pastors and church leaders encouraged community members to get tested, and print materials from resource tables were distributed to community members attending community outreach events.
Printed HIV Educational Materials
CHLs and outreach ministry leaders distributed print materials to community members during regular outreach ministry service hours.
Citywide TIPS Activities
CHLs participated in 3 TIPS project meetings to enhance TIPS churches’ collective capacity to address HIV, review emerging HIV information and study findings, and discuss how to sustain TIPS project efforts. TIPS churches also participated in annual NCWP for the Healing of AIDS in KC events. Additionally, TIPS pastors provided HIV-related sermons at churches with less experience in addressing HIV through community-wide TIPS church revival events during the NCWP.
Control Arm Activities
Similar to the intervention arm, control churches’ CHLs attended 4 trainings and were provided with and asked to deliver 2 non-tailored tools (e.g., HIV brochures passed out by ushers and placed on resource tables, testing event announcements in church bulletins) monthly through multilevel church outlets. Control church CHLs were trained to also coordinate 3 church-based HIV testing events with health agency partners; however, they were limited to only reading a scripted testing event announcement during church services and using flyers to promote testing with their church and community members.
Study Measures
Baseline surveys were conducted with church member participants at their respective church immediately after church services (Sunday school, Sunday or Wednesday services) and with community member participants during church outreach activities 1 month prior to the start of study arm activities. Follow-up surveys were conducted at 6 and 12 months at the same events.
Feasibility of Reach
Reach was assessed by determining the proportion of church and community participants recruited from estimated Sunday morning church service attendees and non-church community members served through church outreach ministries (e.g., food/clothing pantries, young adult ministries, recovery programs, social services).
Participant Characteristics
Participants were asked to report their age, sexual orientation, education level, marital status, average monthly income, and church denomination.
Religiosity
Religious beliefs and behaviors were measured with a 7-item version of the Religious Background and Behavior survey on participants’ engagement in church activities (e.g., prayed, meditated, attended a worship service; 0 = never to 7 = always) and 1 item on their description of their religiosity (e.g., atheist, spiritual, religious) [24].
HIV Testing
Self-reported receipt of HIV testing behaviors was measured using items adapted from national surveys and our pilot studies [17, 25]. These measures included items on receipt of an HIV test (ever, past year, past 6 months; yes/no), month/year tested, and whether tested at church (yes/no) in the past year.
Sexual Risk
A sexual risk score was estimated from participants’ responses to 4 yes/no items: (1) had sex with someone who had been in prison, (2) had sex with a man who has had sex with men, (3) had sex with a person who injects drugs; or (4) had sex while high on drugs or alcohol. Participants were also asked to report their number of lifetime sex partners.
Theory of Planned Behavior Constructs
TPB items were based on the recommended format and adapted from similar measures [22]. Intentions for HIV testing at church were measured with 4 items (e.g., “To what extent do you want to always get an annual HIV test at this church?”; 0 = not at all to 6 = extremely). Attitudinal beliefs about church-based testing (e.g., “Feel more comfortable/safe about taking the test”) were measured with 6 items (0 = disagree strongly to 6 = agree strongly). Also, a 1-item measure assessed the extent of agreement with the church discussing HIV testing, and 1 measure assessed the extent of agreement with HIV testing being made available in churches (0 = disagree strongly to 4 = agree strongly). Assessment of norms included communication about HIV regarding 7 HIV topics (e.g., HIV/AIDS testing, abstinence, condom use) discussed (yes/no) with others in their church. Norms were also assessed with amount of encouragement for HIV testing from 5 referents (friends, partner/spouse, church members, pastor, doctor; 0 = not at all likely to 6 = very likely). Perceived behavioral control was assessed with 6 items on control beliefs (e.g., “I can receive an HIV test at my church”; 0 = not at all likely to 6 = very likely), and 1 item on confidence to seek HIV testing (0 = not confident I will get tested to 10 = very confident I will get tested).
HIV-Related Stigma
Stigma was measured by summing 4 items adapted from national studies on HIV/AIDS stigma (e.g., “If you were going to be tested for HIV, how concerned would you be that you might be treated differently or discriminated against if your test results were positive for HIV?”; 1 = not concerned at all to 4 = very concerned) [26, 27].
Feasibility of Intervention Implementation
Implementation and Exposure
Using an online documentation system, CHLs reported on the type and number of tools implemented each month.
Participant Exposure
Participants reported their exposure to intervention components with an 11-item (yes/no) list of TIPS materials and activities (e.g., pastor-delivered sermons, responsive readings, brochures/church bulletins, video testimonies, presentations by health professionals or people living with HIV).
Participant Satisfaction
Satisfaction with the study at 12 months was assessed with 5-items (e.g., “How clearly information on HIV/AIDS was presented; How private and compassionately HIV testing was offered”; 1 = not at all satisfied to 7 = very satisfied).
Statistical Analysis
Categorical measures were compared using Chi square tests. Continuous measures were described using means and standard deviations with differences estimated from regression models that adjusted for clustering at the church level. Behavioral and psychosocial measures were examined at each time point and the mean difference of differences comparing intervention versus control arms were estimated for baseline to the 6- and 12-month follow-up time points. Mean difference of differences was estimated using linear regression models that adjusted for clustering at the church level.
This pilot study’s primary outcome endpoint was self-reported receipt of HIV testing. The hazard rate ratio for HIV testing was estimated using Cox proportional hazards regression. Factors determined to not be balanced between the intervention and control arms (sexual orientation and sexual risk, see Table 1) were evaluated as potential confounders. Adjustment for these variables did not result in a 10% difference in effect size, so unadjusted estimates are presented. All analyses were intention to treat and accounted for the cluster randomization at the church unit level. Stata (version 13) was used for analysis.
Results
Sample Description
Feasibility of Reach
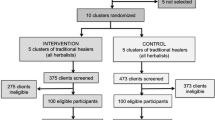
Of the 5 churches located in the KC metropolitan approached, 4 agreed to participate; 1 declined due to other commitments. Sunday morning church attendance among the 4 participating churches ranged from 150 to 250, and yielded a potential sample pool of about 800 church member participants. Community members served through the churches’ outreach ministries ranged from 30 to 300, and yielded a potential sample pool of about 400 community members. Overall, 543 church members (n = 417) and community members (n = 126) were recruited at baseline (n = 235 intervention participants; n = 308 control arm participants), as shown in Fig. 1. Of the baseline participants, 52 and 32% of the potential church and community members respective sample pools were recruited.
Participant Characteristics
At baseline, participants had a mean age of 42 (SD = 14) and were primarily female, between the ages of 30–49, and not married or cohabiting; 85% reported being heterosexual. Participants’ denominations were primarily Baptist (36%, n = 196) and Church of God in Christ (32%, n = 175). At baseline, 75% of participants had ever received an HIV test, and 23% received an HIV test in the last 6 months. Most participants (71%) reported they would be open to receiving an HIV test at church. Regarding retention across arms, control arm retention rates were higher than intervention arm retention rates at 6 months (62% vs. 54%; p = 0.073) and 12 months (58% vs. 40%; p < 0.001), respectively. The analysis sample included 317 participants at 6 months and 271 participants at 12 months.
At baseline, intervention and control arm participants were similar on descriptive characteristics, as shown in Table 1, and on TBP constructs, as shown in Table 2, except that the control arm had a higher percentage reporting heterosexual sexual identity (p = 0.002) and a higher mean sexual risk score (p = 0.011). Also, intervention participants reported more discussion of HIV topics than control participants (p = 0.013). Due to the extent of loss at follow-up time-points, we compared characteristics of those lost to follow-up with those retained in the analysis set. Participants lost to follow-up were more likely to be community members with lower religiosity scores, lower levels of education, and low income, and who were single and never married compared to retained participants. Participants lost to follow-up also had higher sexual risk scores and were more likely to have been recently tested for HIV at baseline.
Receipt of HIV Testing
Intervention participants reported higher rates of testing in the last 6 and 12 months than control participants at the respective study follow-ups (6 months: 47% vs. 28%, p = 0.001; 12 months: 59% vs. 42%, p = 0.008). The intervention participants were also more likely than control participants to have received an HIV test at their church at 6 months (41% vs. 9%, p < 0.001) and 12 months (54% vs. 15%, p < 0.001), as shown in Fig. 2. Using time to event analysis with available month/year data, intervention participants received HIV testing at a rate 2 times faster than controls [hazard rate ratio (HRR) 2.08, 95% CI 1.10, 3.96], as shown in Fig. 3. Testing rates were not associated with sex, race/ethnicity, marital status, sexual orientation, income, religiosity or church member/community member affiliation, but were higher among those with increasing sexual risk scores (HRR 1.32, 95% CI 1.13, 1.53) or history of HIV testing (HRR 2.23, 95% CI 1.14, 4.34). Those 50 years and older (HRR 0.58, 95% CI 0.34, 0.97) and with a 4-year college degree (0.68, 95% CI 0.52, 0.89) had lower rates of testing.
Theory of Planned Behavior Constructs and HIV Stigma
At 6 months, intentions to test at church increased significantly for intervention churches (p = 0.007). Although significant shifts in TPB and HIV stigma measures were not detected at 6 months, trends toward significance were observed for attitudinal beliefs regarding discussion of (p = 0.083) and testing for HIV should occur in church (p = 0.079), and number of HIV topics discussed with a church member (p = 0.065). At 12 months, intervention participants had a mean intention to test at church score that was 1.32 higher than control participants (p = 0.005). The intervention arm also had significant increases compared to the control arm in beliefs that HIV testing should be discussed in church (p = 0.015) and HIV testing should be available in church (p = 0.011) along with the number of HIV topics discussed (p = 0.027). Finally, intervention participants’ control beliefs were significantly higher than controls at 12 months (p = 0.010).
Feasibility of Intervention Implementation
Intervention CHLs reported delivery of 39 tools, about 3 tools per month, over a 12-month period. Their most frequently reported tools delivered included brochures/bulletin inserts, resource table displays, and testimonials. All pastors signed a memorandum of agreement (MOA) committing to conduct study activities specific to their church’s randomly assigned study arm. Pastors at both TIPS churches delivered a full sermon about HIV at least once, commented about HIV from the pulpit at least twice, and received an HIV test in front of congregants 1 time.
At 12 months, intervention arm participants reported exposure to 72% (8 out of 11) of the TIPS components. The most frequently reported exposures were to sermons (93%), posters (91%), resource tables (90%), and brochures/church bulletins (85%). Overall, intervention participants reported being satisfied/highly satisfied with how: privately and compassionately HIV testing was offered (94%), HIV testing events were made available at their church (90%), HIV testing was free (88%), often HIV information and testing events were offered (87%), quickly they could get tested without a long wait time (84%), and compassionately their pastor discussed HIV (81%).
Discussion
To our knowledge, this paper is the first to examine the effects of a theoretically-based, religiously-tailored, multilevel HIV intervention specifically designed to increase receipt of HIV testing among African American church members and community members who used church outreach ministries. Regarding feasibility of reach, recruitment activities achieved enrollment of 543 participants from 4 African American churches. Of note, we recruited over 50% of the potential 800 church member sample pool and over 30% of the potential 400 community member sample pool. Almost 25% of the final baseline sample (n = 126) were community members who used outreach ministry services (e.g., food/clothing pantries, recovery programs), which strongly supports the feasibility and extended reach of church-based HIV interventions beyond the church into the communities they serve. Representation across age, marital status, and income was also achieved. However, there were more females than males (64% vs. 36%, respectively), which is consistent with other church-based health studies that have found females made up about two-thirds of church attendees [13, 17]. Also, more than 10% of baseline participants (mostly community members) did not identify as heterosexual, which is much higher than the 4% lesbian/gay/bisexual/transgender representation observed in national surveys [28], indicating that African American churches may also be able to reach non-heterosexual populations who are at greatest risk for HIV. Many church and community participants had 1 or more HIV risk factor (40%). They also had an average of 11 lifetime sex partners, with community members having nearly twice as many lifetime sex partners as church members. These baseline descriptions of our sample suggests that churches may be an important setting to extend HIV testing services to African American populations who may be at-risk for HIV, particularly African American women, sexual minorities, and people living on low-incomes.
Most importantly, the TIPS intervention demonstrated impact on receipt of an HIV test. Our findings indicated a significant increase in HIV testing rates among TIPS intervention participants compared to participants in the non-tailored control arm at 6 and 12 month follow-up. At 12 months, 59% of participants from TIPS churches had completed HIV testing compared with 42% in control churches. TIPS participants were twice as likely to get tested for HIV and were more likely to receive an HIV test at church than control arm participants. TIPS HIV testing findings are much higher than those found in general population of African Americans getting an HIV test in the last year, which have ranged from 23 to 49% in national studies [29,30,31] and in the Derose et al. HIV stigma intervention study in Latino and African American churches [20]. Our findings provide methodologically strong evidence that churches can play a key role in assisting to achieve National HIV/AIDS Strategy recommendations to widely disseminate HIV education and testing programming using culturally-appropriate intervention strategies and ultimately get large numbers of at risk populations to be aware of their HIV status.
The TIPS intervention was designed to enhance HIV testing by targeting TPB constructs (intentions and attitudinal, normative, and control beliefs) regarding receipt of an HIV test. The TPB has been used successfully to develop health interventions to increase community-wide HIV testing in U.S. cities [32]. We found important increases in most of the TPB construct measures. For example, there were significant increases in attitudinal beliefs that HIV testing should be discussed and should be available in church, which is consistent with other church-based studies that have reported on acceptability of church-based HIV testing among church leaders and members [12, 33, 34]. Still, this is the first study to assess and demonstrate shifts in acceptability of church-based HIV testing in the context of an intervention study. Significant increases were also found in perceived behavioral control regarding getting tested for HIV, including beliefs and confidence and particularly in church settings. The church-based HIV testing events in this study were held during church services and outreach ministry events, were free to all church and community members regardless of participation in the study or level of risk, and provided testing results within 20 min using rapid tests, which may have been key access-related factors to enhance behavioral control to get an HIV test.
The intervention impacted most TPB constructs as expected. Although, we did not find significant reductions in social normative support for HIV testing from important referents (e.g., church members, pastor, doctor) or significant reductions in HIV stigma, we did find significant increases on discussion of HIV topics. Shifts in social norms and HIV stigma may have been attenuated due to ceiling and floor effects, since fairly high levels of reported encouragement from others to get an HIV test and low levels of reported stigma existed at baseline. Also, Derose et al. did not find shifts in stigma among African Americans in their church-based HIV stigma reduction intervention [20]. Taken together the findings indicate the TIPS intervention was successful in impacting most of the targeted TPB constructs thought to be key to successfully increase testing.
This study demonstrated the feasibility of CHL implementation of the TIPS intervention, with most tools being delivered at the church service level (sermons, brochures, testimonials). TIPS CHLs delivered more than 3 tools per month from the TIPS HIV Tool Kit consisting of materials and activities designed to fit within existing activities that naturally occur in churches (e.g., sermons, responsive readings, testimonials). This study also demonstrated the feasibility of providing HIV testing services during Sunday morning church services and midweek bible study for church members and during outreach ministry services and events for community members. This testing delivery approach was designed to increase reach, accessibility, and acceptance of church-based HIV testing by tapping into the large numbers of socially-connected members participating in church and community services and events. Commitments from pastors on delivery of TIPS components and HIV testing events during church and community services/events were critical to TIPS implementation feasibility. Studies have reported on the high levels of pastoral influence on church members’ health behaviors [35, 36], and the inherent capacity of churches to provide support for health behaviors [10, 12, 33]. Furthermore, a growing number of studies indicate the willingness of African American pastors to talk about HIV and encourage their members to get tested [10, 12, 33, 34, 37,38,39]. TIPS pastors preached about the importance of getting tested and showing compassion for people living with HIV, and they modeled receipt of an HIV test during church services. Also, intervention CHLs regularly delivered religiously-tailored TIPS tools (e.g., church bulletin/brochures, posters, resource cards) with HIV information about the impact of HIV on African Americans, transmission routes, protective behaviors, and risk checklists to church and community members. These implementation activities were reported by CHLs via an online implementation documentation system (and observed by study staff) and aligned with participants’ reported intervention component exposure—and their high level of satisfaction with TIPS, highlighting the feasibility of the intervention.
Taken together the results suggest church-based HIV interventions, such as TIPS, may provide scalable models of how pastors and their church members can appropriately distribute HIV information and promote HIV testing behaviors with African American church populations, especially when they are provided with religiously-tailored supportive tools designed by and with faith leaders. Feasibility and efficacy results should be interpreted in the context of our CBPR approach which engaged faith leaders and health agency partners in all phases of the study, including study design, implementation, and evaluation. This may have contributed to the large number of tools distributed by TIPS CHLs and members’ receptiveness to church-based HIV testing. Health agency partners were also included in the study design phase and may have helped to contribute to compassionate and religiously-appropriate provision of church-based HIV testing services and may have also contributed to church and community members’ receptiveness to getting tested in church settings.
Although this study was found to be impactful in increasing receipt of HIV testing with church-affiliated populations, several limitations exist. This study experienced high rates of attrition at 6 and 12 months, especially among participants who tended to be younger, male, and less educated/lower income. These characteristics were highly representative of our community member participants served through the participating churches’ outreach ministries (e.g., food pantries, social services). Community participants were more difficult to contact due their transience and intermittent contact with participating churches. Also, church leaders running the outreach ministries in 2 of the churches (1 intervention and 1 control church) reduced their roles soon after the launch of the interventions due to illness. Additionally, participants may have socially responded to HIV testing questions, especially considering surveys were completed at participating churches. Yet, baseline HIV testing findings suggest that if social responding occurred, it was similar between the randomized church arms. Finally, this faith-based study was designed for African American church-populations and engaged pastors who committed to addressing HIV with their members as designated in their memorandum of agreements; therefore, this study’s findings may not generalize to other church settings.
Although this study aimed to examine feasibility and outcomes of church-based HIV testing and did not have detection of new HIV cases as an outcome, we briefly provide some positive anecdotal aspects of this church-based study. One HIV-positive case, which was previously diagnosed, was detected and 3 persons living with HIV disclosed that they were positive but were not in care to our health agency HIV screeners. These individuals were linked to an HIV case manager to get assistance with linkage to HIV care. They expressed appreciation of their church’s focus on HIV education and testing and felt safe to share their HIV status with their pastor and seek the support they needed, which suggests the important role churches can serve in the linkage to care process. Just as important, church and community members who did not test positive received counseling on how to reduce their risk of contracting HIV in order to maintain their HIV-negative status, which aligns with NHAS goals. Also, 3 of the churches requested that testing for other STDs (chlamydia, gonorrhea, and syphilis) be provided by health agency partners during their HIV testing events. These positive side effects highlight the need to explore church-based provision of STD screening in conjunction with HIV testing, HIV/STD linkage to care services, capacity of health departments to provide church-based testing at nontraditional times (e.g., Sunday mornings), and possibly even pre-exposure prophylaxis services with at risk church-affiliated populations.
Expanding reach of HIV education and testing is a key strategy identified in the NHAS as the first step to more quickly diagnose new cases of HIV, get newly diagnosed people into care, and ultimately reduce the spread of HIV, especially in minority communities where new HIV cases continue to be disproportionately high. This study’s multilevel TIPS HIV testing intervention was designed and delivered collaboratively with faith leaders and health agency partners for church community settings. Findings indicated the TIPS intervention increased receipt of HIV testing, enhanced theoretical constructs that guided the design, and has the potential to assist in addressing NHAS goals for widespread HIV education and testing in African American churches.
References
White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States. 2015. http://www.whitehouse.gov/sites/default/files/ uploads/NHAS.pdf.
Centers for Disease Control and Prevention. HIV Surveillance Report, 2013. 2015. http://www.cdc.gov/hiv/library/reports/surveillance.
Chandra A, Billioux VG, Copen CE, et al. HIV testing in the U.S. household population aged 15-44: Data from the National Survey of Family Growth, 2006-2010. National health statistics reports; no 58. Hyattsville, MD: National Center for Health Statistics. 2012.
Kaiser Family Foundation. HIV testing in the United States. 2011 June. http://www.kff.org/hivaids/6094-11.cfm. http://www.kff.org/hivaids/6094.cfm.
Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(14):1–17.
Centers for Disease Control and Prevention. CDC health disparities and inequalities report—United States 2011. Health Insurance Coverage—United States, 2008 and 2010. MMWR. 2013;62(Suppl 3):61–64.
Bogart LM, Wagner GJ, Green HD Jr, et al. Medical mistrust among social network members may contribute to antiretroviral treatment nonadherence in African Americans living with HIV. Soc Sci Med. 2016;164:133–40. https://doi.org/10.1016/j.socscimed.2016.03.028.
Leibowitz AA, Taylor SL. Distance to public test sites and HIV testing. Med Care Res Rev. 2007;64(5):568–84. https://doi.org/10.1177/1077558707304634.
Berkley-Patton J, Hawes SM, Moore E, Bowe-Thompson C, Williams E, Martinez D. Examining facilitators and barriers to HIV testing in African American churches using a community-based participatory research approach. Ann Behav Med. 2012;43:s277.
Derose KP, Mendel PJ, Palar K, et al. Religious congregations’ involvement in HIV: a case study approach. AIDS Behav. 2011;15(6):1220–32. https://doi.org/10.1007/s10461-010-9827-4.
Mannheimer SB, Wang L, Wilton L, et al. Infrequent HIV testing and late HIV diagnosis are common among a cohort of Black men who have sex with men in 6 US cities. J AIDS. 2014;67(4):438–45. https://doi.org/10.1097/QAI.0000000000000334.
Berkley-Patton J, Martinez D, Bowe-Thompson C, et al. Examining church capacity to develop and disseminate a religiously-appropriate HIV tool kit with African American churches. J Urban Health. 2012;90(3):482–99.
Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34.
Lincoln CE, Mamiya LH. The Black Church and the African American experience. Durham, NC: Duke University Press; 1990.
Pew Research Center. America’s changing religious landscape. Washington, DC. http://www.pewforum.org/files/2015/05/RLS-05-08-full-report.pdf.
Agate LL, Cato-Watson DM, Mullins JM, et al. Churches United to stop HIV (CUSH): a faith-based HIV prevention initiative. J Nat Med Assoc. 2005;97(7 Suppl):60S.
Berkley-Patton J, Bowe-Thompson C, Bradley-Ewing A, et al. Taking It to the Pews: a CBPR-guided HIV awareness and screening project with Black churches. AIDS Educ Prev. 2010;22(3):218–37.
Griffith DM, Campbell B, Allen JO, Robinson KJ, Stewart SK. YOUR Blessed Health: an HIV-prevention program bridging faith and public health communities. Public Health Rep. 2010;125(1_suppl):4–11.
Whiters DL, Santibanez S, Dennison D, Clark HW. A case study in collaborating with Atlanta-based African-American churches: a promising means for reaching inner-city substance users with rapid HIV testing. J Evid Based Soc Work. 2010;7(1):103–14. https://doi.org/10.1080/15433710903175981.
Derose KP, Griffin BA, Kanouse DE, et al. Effects of a pilot church-based intervention to reduce HIV stigma and promote HIV testing among African Americans and Latinos. AIDS Behav. 2016;20(8):1692–705. https://doi.org/10.1007/s10461-015-1280-y.
Bronfenbrenner U. The ecology of human development: experiments by design and nature. Cambridge, MA: Harvard University Press; 1979.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211.
Craw JA, Gardner LI, Marks G, et al. Brief strengths-based case management promotes entry into HIV medical care: results of the antiretroviral treatment access study-II. J AIDS. 2008;47(5):597–606.
Connors GJ, Tonigan JS, Miller WR. A measure of religious background and behavior for use in behavior change research. Psychol Addict Behav. 1996;10(2):90.
Centers for Disease Control and Prevention. HIV Surveillance Report, 2009. 2011. http://www.cdc.gov/hiv/surveillance/resources/reports/2009report/pdf/cover.pdf.
Herek GM, Capitanion JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. Am J Public Health. 2002;92(3):371–7.
Herek GM. AIDS and stigma in the United States. Am Behav Sci. 1999;42(7):1130–47.
Gates G. In US, more adults identifying as LGBT. Gallup (Jan 2017). http://www.gallup.com/poll/201731/lgbt-identification-rises.aspx.
Centers for Disease Control and Prevention. HIV testing trends in the United States, 2000-2011. Atlanta, Georgia: 2013 Jan. https://www.cdc.gov/hiv/pdf/research/testing_trends.pdf.
Copen CE, Chandra A, Febo-Vazques I. HIV testing in the past year among the U.S. household population aged 15-44: 2011-2013. Hyattsville, MD: National Center for Health Statistics. 2015. NCHS data brief, no 202.
Kaiser Family Foundation. 2012 Survey of Americans on HIV/AIDS. 2012. http://kff.org/hivaids/poll-finding/2012-survey-of-americans-on-hivaids/.
Spoeth SK, Lee NR, Fraze, JL, et al. Utilizing social marketing to increase HIV testing in African American women: lessons from CDC’s Take Charge, Take the Test Campaign. Presented at the National HIV Prevention Conference; 2007; Atlanta, GA.
Bryant-Davis T, Ellis MU, Edwards N, et al. The role of the Black Church in HIV prevention: exploring barriers and best practices. J Community Appl Soc Psychol. 2016;26(5):388–408. https://doi.org/10.1002/casp.2270.
Pichon LC, Powell TW. Review of HIV testing efforts in historically black churches. Int J Environ Res Public Health. 2015;12(6):6016–26. https://doi.org/10.3390/ijerph120606016.
Davis DT, Bustamante A, Brown CP, et al. The urban church and cancer control: a source of social influence in minority communities. Public Health Rep. 1994;109(4):500–6.
Lumpkins CY, Vanchy P, Baker TA, Daley C, Ndikum-Moffer F, Greiner KA. Marketing a healthy mind, body, and soul: an analysis of how African American men view the church as a social marketer and health promoter of colorectal cancer risk and prevention. Health Educ Behav. 2016;43(4):452–60. https://doi.org/10.1177/1090198115604615.
Aholou TM, Cooks E, Murray A, et al. “Wake Up! HIV is at Your Door”: African American faith leaders in the rural south and HIV perceptions: a qualitative analysis. J Relig Health. 2016;55(6):1968–78. https://doi.org/10.1007/s10943-016-0193-z.
Berkley-Patton, J, Bowe-Thompson, C, Bradley-Ewing, A, Williams, E. Taking It to the Pews: a feasibility study of an HIV education and prevention tool kit approach with African American churches. Ann Behav Med. 2009;37(Suppl 1):D75, s201.
Pichon LC, Powell TW, Ogg SA, Williams AL, Becton-Odum N. Factors influencing Black Churches’ readiness to address HIV. J Relig Health. 2016;55(3):918–27. https://doi.org/10.1007/s10943-015-0117-3.
Acknowledgements
This research was supported by the National Institutes of Mental Health (K01 MH082640-02). The authors gratefully acknowledge the tremendous contributions of our health partners (KCMO Health Department, KC Care Health Center, and JayDoc Free Clinic) along with the committed implementation of Taking It to the Pews by church leaders with their church members and community members served through their outreach ministries. The authors would also like to thank Nia Johnson for assisting in preparing this paper for submission.
Funding
This study was funded by NIMH (K01 MH082640).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Research Involved in Animal Rights
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Berkley-Patton, J.Y., Thompson, C.B., Moore, E. et al. Feasibility and Outcomes of an HIV Testing Intervention in African American Churches. AIDS Behav 23, 76–90 (2019). https://doi.org/10.1007/s10461-018-2240-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2240-0