Abstract
HIV-related stigma and mistrust contribute to HIV disparities. Addressing stigma with faith partners may be effective, but few church-based stigma reduction interventions have been tested. We implemented a pilot intervention with 3 Latino and 2 African American churches (4 in matched pairs) in high HIV prevalence areas of Los Angeles County to reduce HIV stigma and mistrust and increase HIV testing. The intervention included HIV education and peer leader workshops, pastor-delivered sermons on HIV with imagined contact scenarios, and HIV testing events. We surveyed congregants at baseline and 6 month follow-up (n = 1235) and found statistically significant (p < 0.05) reductions in HIV stigma and mistrust in the Latino intervention churches but not in the African American intervention church nor overall across matched African American and Latino pairs. However, within matched pairs, intervention churches had much higher rates of HIV testing (p < 0.001). Stigma reduction and HIV testing may have synergistic effects in community settings.
Resumen
El estigma y la desconfianza asociada con el VIH contribuyen a las disparidades del mismo. Abordar el estigma en asociación con líderes de fe puede ser eficaz, pero hasta ahora se han evaluado pocas intervenciones en iglesias para reducir este estigma. Implementamos una intervención piloto con 3 iglesias latinas y 2 iglesias afroamericanas (4, en parejas de intervención y control) en zonas de alta prevalencia del VIH en el condado de Los Angeles, con el objetivo de reducir el estigma y la desconfianza asociada con el VIH, así como incrementar las pruebas del HIV. Esta intervención incluyó educación y talleres con líderes de grupo; sermones acerca del VIH dirigidos por pastores a sus congregaciones describiendo escenarios de interacción imaginaria; y por último, jornadas de pruebas del VIH. Encuestamos a feligreses en la línea de base y 6 meses después (n = 1235), y encontramos reducciones estadísticamente significativas (p < 0.05) en el estigma y la desconfianza asociada con el VIH en las iglesias latinas donde implementamos la intervención, pero no en la iglesia afroamericana donde implementamos la intervención, ni a través de las iglesias afroamericanas y latinas que fueron evaluadas en pareja. Sin embargo, en las iglesias evaluadas en pareja, las intervenciones arrojaron tasas más altas de pruebas realizadas del VIH (p < 0.001). La reducción del estigma y la realización de pruebas del VIH pueden tener efectos sinérgicos en entornos comunitarios.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
African Americans and Latinos in the United States (U.S.) continue to be disproportionately affected by HIV. In 2010, together these groups represented 65 % of newly-identified HIV infections, while constituting only 28 % of the U.S. population [1]. Contributing factors to HIV-related disparities include individual attributes related to sex, race-ethnicity, and behavioral risk factors, as well as the overlapping social and economic systems (social environment, physical environment, health services, and structural and societal factors) or the social determinants of health [2]. Addressing such determinants and thereby reducing HIV inequities requires moving beyond individual-level interventions towards community-level strategies that prevent HIV transmission [3].
Stigma and discrimination, from HIV as well as HIV-related intersectional characteristics such as race-ethnicity and sexual orientation, have been proposed as structural factors that contribute to disparities across the HIV cascade, beginning with primary prevention and testing, the focus of the present paper [4]. For example, fear of HIV-related stigma and discrimination can discourage people from testing, particularly African Americans and Latinos [5], and coupled with socio-economic issues associated with poverty, such as reduced access to high quality health care, can limit the extent to which these groups benefit from available treatment [6]. Moreover, historical, societal, and personal experiences with discrimination due to race-ethnicity may contribute to mistrust of medical institutions, scientific research, and public health information, which in turn may lead to specific mistrust around HIV, including mistrust of public health messages regarding HIV testing, prevention, and treatment (also known as “HIV conspiracy beliefs”) [7]. HIV stigma may be furthered propagated by such mistrust, through misunderstanding of how HIV is spread. Given the pervasive negative effects of stigma and discrimination across the continuum of care [8], stigma reduction has been identified as essential to reducing HIV-related disparities [9].
To fully address HIV-related stigma and mistrust, multi-faceted, multi-level, community-based interventions are needed [10]. Partnering with community-based organizations and other stakeholders to develop and conduct HIV interventions can help build trust with underserved communities [4]. Such trust can also be effective in facilitating HIV screening. For example, conducting HIV testing in community-based venues has been found to expand screening access and utilization among underserved groups, including racial ethnic-minorities [11].
Religious congregations such as churches are often trusted resources in communities, particularly for African American and Latinos, who report higher levels of religious affiliation than other populations [12]. Congregations can be empowering for members [13] and act as buffers to life stressors through tangible support shared among members [14, 15]. This can be especially important for groups that have experienced racial and economic discrimination, such as African Americans [16]. Congregations have also historically played an important role in the civic and social incorporation of recent immigrants [17, 18]. However, previous studies have found that although health and social service programming is common among congregations, less than 6 % of congregations nationally provide support to people with HIV [19, 20].
Over the last decade there has been a burgeoning literature on HIV prevention education in partnership with African American churches [21–29], but there has been little evaluation regarding the extent to which these efforts decrease HIV stigma and mistrust. We know of only one study that assessed effects on stigma of an African American church-based HIV education and testing intervention [30], which found that the pilot intervention did not reduce HIV stigma. We know of no HIV stigma reduction interventions with Latino churches. Recent systematic reviews of HIV stigma reduction interventions in the U.S. and elsewhere have identified dozens of interventions of variable quality across a range of settings, but none were tested in churches [31, 32]. Thus, we developed a multi-component intervention for African Americans and Latinos—the Facilitating Awareness to Increase Testing for HIV (FAITH) Project—in collaboration with faith and public health leaders and based on extensive formative research on congregational HIV programming and HIV-related attitudes among clergy and lay leaders [33, 34].
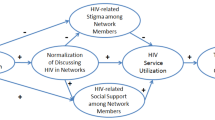
Our theoretical framework incorporates social psychological theories of stigma reduction, including the contact hypothesis [35], and draws on previous research that suggested that both informational and contact components are necessary to increase empathy for those who are stigmatized and in so doing, reduce stigma [36–38]. Further, we conceive of HIV testing and stigma reduction as mutually facilitative in congregational settings [39], as they “normalize” HIV as a health issue rather than a moral issue [40, 41].
In this paper, we describe our pilot study, which aimed to examine feasibility, acceptability, and preliminary effectiveness of a multi-component, church-based intervention to reduce HIV stigma and HIV mistrust and promote HIV testing among African Americans and Latinos.
Methods
Community Partnered Approaches
FAITH used a community-partnered approach throughout all phases of the study. A Community Advisory Board (CAB) composed of local religious and public health leaders provided input on all important aspects of the intervention design and advised the project team throughout all phases of the study, including the design of data collection, intervention activities, and evaluation procedures. In addition, the research team worked closely with the CAB and a local health department to develop intervention components (described below) and with participating churches to plan, schedule, and implement all church-based survey and intervention activities.
Setting
We focused on churches that primarily served African American and Latino congregants in and around the city of Long Beach, a high HIV prevalence area of Los Angeles County. Long Beach has a cumulative incidence rate of 1359 AIDS cases per 100,000 residents, a rate that is over twice that for Los Angeles County and three times that of California [42]. We focused on African American and Latino churches in these areas, given the disproportionate burden of HIV borne by these groups [43].
We began by enumerating the African American and Latino churches in Long Beach and adjacent areas through local faith-based lists and telephone directories and our CAB’s contacts. We collected basic information about each congregation (demographics, health-related activities) through a brief telephone screening survey. Of the 61 churches identified, 33 (54 %) completed the screening survey, 5 (8 %) refused and 23 (38 %) never responded. Of the 33 churches that completed the screener, 11 (5 African American; 6 Latino) were considered eligible (>70 % African American or Latino, ≥100 typical Sunday attendance, and the church reported having conducted no or almost no HIV-related activities previously). For the final criterion, church leadership was asked a general question about health-related activities (i.e., “What kinds of health-related activities has your church done recently or in the past?”), with specific probes to capture HIV-related activities (e.g., “Which health issue or topic do/did you address?”; “Has your church ever been involved in any type of HIV/AIDS-related activity, service, program or outreach?”).
Church Recruitment
We selected 6 churches for our pilot study, matching eligible churches on race-ethnicity, denomination, and congregation size. More specifically, we selected one pair of churches for each of the following three types: medium African American Baptist, large Latino Roman Catholic, and small Latino Pentecostal. We sent the pastor of each congregation a recruitment letter with a project brochure inviting the congregation to participate in the FAITH study and requesting a meeting with church leaders to provide more details about the project. Members of the research team followed up with churches over the phone and, in some cases, by visiting the churches during Sunday worship services. Once contact was made, in-person meetings were held with pastors and designated church coordinators to discuss project aims, project activities, church coordinator roles, and project incentives.
Ultimately, 5 churches agreed to participate in the pilot: 2 medium-sized (125–250 member) African American Baptist, 2 small (100 member) Latino Pentecostal, and 1 large (2000+ member) Latino Catholic churches. We were unable to find a suitable match as a replacement for the one Latino Roman Catholic church that did not agree to participate in the study. Because a majority of Latinos are Catholic, we deemed it important for studying feasibility, acceptability, and potential impact to implement the intervention in a Catholic church even without a matched control. Thus, the single Catholic church was assigned to the intervention condition, while the four other churches were randomized to either the intervention or control conditions within their matched pair.
Intervention Overview
Intervention components and development are described fully elsewhere [39] and are summarized briefly here. All intervention materials were professionally translated into Spanish and reviewed by bilingual members of the research team; adaptations were made by consensus.
HIV Education Workshops
These were designed to raise awareness about HIV, increase knowledge about HIV and HIV testing (through instruction, as well as brochures and videos on HIV transmission and testing), and engender empathy for those affected by HIV (through the use of a project-generated video with personal testimonials about people’s experiences with HIV stigma, particularly in the church). The workshop lasted about 90 min and was co-facilitated by a research team member and a health educator from the health department. Facilitators guided participants through discussions about HIV stigma, its consequences, and ideas about what churches can do to address it, as well as HIV myths and factual information about HIV prevention and testing. In terms of HIV mistrust, a key activity involved a question and answer discussion in which participants anonymously provided common beliefs and myths about HIV and people with HIV. Health department facilitators discussed these beliefs using a non-judgmental approach while correcting misperceptions.
Peer Leader Workshops
These sessions gave participants the opportunity to do role plays and develop skills for discussing HIV stigma and HIV testing with other congregants and community members. They also lasted 90 min and were co-facilitated by members of the project team. The facilitators used a motivational interviewing approach [44], which included open-ended questions, reflective listening, and exploration of ambivalence about HIV testing and reasons for HIV stigma.
HIV Sermon/Imagined Contact Scenario
Each pastor or priest was asked to deliver a sermon or homily about HIV, how HIV and related stigmas are affecting the community, and the importance of having compassion towards people affected. Our clergy co-chairs of the CAB drafted a sample sermon that wove together theological reflection with a hypothetical contact scenario that helped congregants visualize meeting someone with HIV in circumstances that might encourage empathy. This part of the intervention was based on research that suggests that simulated contact or interaction with someone with a stigmatized characteristic can help to reduce prejudice [45, 46]. Clergy were encouraged to adapt the sermon to their own preaching style and tradition and implement it at their principal worship services on one of the weekends leading up to or including an HIV testing event.
Congregation-Based HIV Testing Events
Health department counselors conducted rapid oral fluid testing and counseling through a mobile clinic stationed at the church during regularly scheduled services and activities. The congregations helped to promote the events and the project team provided logistical support.
Intervention activities were implemented during regular meetings of established groups within the church (e.g., prayer meeting, women’s group) as well as in between principal worship services. The timeframe for implementation of intervention activities spanned periods ranging from 2 months in the smaller churches to 4 months in the largest church.
Survey Assessments
A complete description of survey methods is provided elsewhere [47]. Briefly, survey assessments were performed two times at each church, before and after intervention implementation at the intervention churches. Control churches were given the option to complete intervention activities after the second assessment. The interval between the wave 1 (baseline) and the wave 2 (follow-up) assessments was approximately 6 months. The questionnaire used at waves 1 and 2 was pretested in English at a medium-sized African American Baptist Church and in English and Spanish in a large Latino Catholic church (similar to those participating in the pilot); results informed development of customized church-specific plans for survey promotion and implementation. Church coordinators and other congregational leaders helped to promote the survey within each congregation, and English and Spanish language group survey sessions managed by survey administrators were conducted at church sites during regularly scheduled ministry meetings and/or after religious services.
Given the sensitive nature of survey questions (including HIV status) and the church-based administration, we opted not to collect personal identifiers. To link surveys between waves, we created a unique, individually-generated, survey code from four ‘distinguishing’ items: first letter of mother’s first name, first letter of father’s first name, day of participant’s birthday, and month of mother’s birthday. As we explain below (under Data Analysis), we observed a low match rate in this survey code between baseline and follow-up (only 20 % provided adequate information that allowed us to match the surveys). Thus, below we explain our analytic approaches to account for the low match rate.
Overall response rates were 73 % at baseline and 79 % at follow-up, each calculated as a proportion of regular church attendees at the time of the survey. Participants received a $20 gift card and a meal for completing each survey.
Measures
Outcomes
HIV stigma, our primary outcome, was examined along several closely related dimensions, with items adapted from prior studies:
-
1.
Discomfort, 4 items about how comfortable (from 1 = very comfortable to 5 = very uncomfortable) respondents would feel being around people with HIV in various community settings (school, church, restaurant, and grocery story) [30, 48].
-
2.
Shame, 3 items about the extent to which respondents endorse (from 1 = disagree strongly to 5 = agree strongly) hypothetical feelings of shame if they had HIV (dirty, ashamed, concerned about mistreatment or discrimination) [49, 50].
-
3.
Blame, 2 items about the extent to which respondents endorse (from 1 = disagree strongly to 5 = agree strongly) beliefs that people with HIV are “responsible” for their illness or have “gotten what they deserve” [51].
-
4.
Rejection, 3 items about whether respondents endorse (from 1 = disagree strongly to 5 = agree strongly) beliefs that if they had HIV, they would be rejected, fired, or couldn’t face their families [52]. These items were intended to capture anticipated HIV stigma, i.e., whether participants believed that they would be discriminated against in the future if they were found to be HIV-positive [8].
Using the items from these subscales, we created a 12-item overall measure of HIV stigma using a bifactor item response theory (IRT) model, which accounted for the covariance specific to each subscale [53]. The bifactor IRT-model estimated item parameters for the general dimension (i.e., HIV stigma), which were then used to generate an overall HIV stigma composite measure in each imputed dataset (see imputation description below). After standardization across imputed data sets, these HIV stigma scores were the primary outcome used in our analysis, which conveniently allowed for regression coefficients for the intervention and church effects to represent effect size impacts on the outcomes.
HIV-related mistrust was measured with a 7-item scale, with items adapted from previous research [7, 54]. Participants were asked to report their agreement (from “disagree strongly” to “agree strongly”) with the following statements: “A lot of information about AIDS is being held back from the public,” “HIV is a manmade virus,” “There is a cure for AIDS, but it is being withheld from the poor,” “HIV was created and spread by the CIA or U.S. government,” “AIDS is a form of genocide against people of my racial or ethnic group,” “AIDS was created by the U.S. government to control people of my racial or ethnic group,” and “AIDS was produced in a U.S. government laboratory.” HIV-related mistrust was also standardized to have a mean of 0 and a standard deviation of 1 in order to allow regression coefficients for the intervention and church effects to represent effect size impacts on the outcomes.
HIV testing, a secondary study outcome, was a binary measure of whether or not a participant received an HIV test during the course of study follow-up. It was computed by determining if a participant’s response to the Wave 2 question “what is the month and year of your most recent HIV test?” was after the study was launched in the participant’s church.
Control Variables
Respondents provided various types of demographic and socio-economic/cultural background information. For these analyses, we included variables that have been associated with HIV stigma among church-affiliated populations [55, 56]: age was a continuous variable; gender was defined as male (reference group) and female; and highest level of education was a 6-category variable that ranged from “6th grade or less” to “some graduate school or graduate degree.” In addition, since beliefs related to HIV (stigma, mistrust) are likely influenced by cultural norms, we created sub-groups related to race-ethnicity, nativity, and English language fluency: (1) African Americans (reference group); (2) U.S.-born Latinos who reported speaking English “well” or “very well”; (3) foreign-born Latinos who reported speaking English “well” or “very well” (high English proficiency); and (4) foreign-born Latinos who reported speaking English “not well” or “not at all” (low English proficiency). We also controlled for whether or not a respondent knew anyone (friends, family, co-workers, others) who “has HIV or AIDS or has died of HIV” (Yes/No), which has been shown to be related to HIV stigma [57–59].
Where possible, we used Spanish versions already available for items and scales in our survey. When no Spanish version existed, we used established procedures for developing culturally-appropriate versions through translation by committee. Specifically, an American Translator Association-certified translator who was a native Spanish speaker from Latin America translated the survey items using broadcast Spanish (suitable for both Los Angeles and the wider Latino population of the U.S.), which were then reviewed by a committee of 4 bilingual research team members (including the first author of this article) and 2 bilingual community collaborators to compare the original English version against proposed translation to identify discrepancies in meaning and/or errors. We used a consensus approach to make appropriate changes.
Data Analysis
Missingness rates in survey items ranged from 1.1 to 6.4 % with a mean of 3.6 %. We used multiple imputation (IVEware in SAS 9.2) to avoid dropping cases with missing data. Five imputed datasets were created using the Sequential Regression Imputation Method [60]. χ 2 and t tests were used to examine participant characteristics at baseline and assess any differences between churches within our matched pairs.
Multivariate Analyses
Two multivariate linear regression models, each jointly modeling outcomes at wave 1 and wave 2 (pre- and post-intervention), were fit to estimate the effects of the intervention on our outcomes. In the first model, we only used data from the four churches that formed complete pairs (a control and intervention church) and controlled for pair fixed effects, a main effect of the intervention, an indicator for whether the observation came from wave 2, interactions between the wave 2 indicator and both the pair fixed effects and the intervention indicator, and all the control variables listed above. This model aimed to assess the average impact of the intervention between waves 1 and 2.
In our second regression model for each outcome, we used data from all five churches to gain a better understanding of how each church changed over time. In this model, we fit a similar model as the one described above, using pooled data from waves 1 and 2. However, instead of using intervention and pair fixed effects in the model, we used the five church indicators to allow us to estimate the adjusted mean at wave 1 for each church and the change in that mean from wave 1 to wave 2 for each church.
For HIV testing, we computed the proportion of survey members who reported an HIV test during the follow-up period (i.e., since baseline) at each church and estimated a multivariate logistic regression model that adjusted for the control variables listed above as well as a dummy indicator for four of the five churches. In order to determine if the odds of testing were different in the Latino Pentecostal and African American Baptist intervention churches than in their paired control churches, we performed post-estimation testing of the null hypothesis that the church coefficients were equal within pairs.
A p value of less than 0.05 was considered statistically significant for all analyses. We note above that we only had a subset of our sample with repeated measures (20 % of our sample matched using a probabilistic matching algorithm adapted from Belin et al. [61]); because repeated measures data were available for only a portion of the sample, all models controlled for the correlations between repeated measures obtained on the same individual using robust standard error estimates in Stata. We conducted a sensitivity analysis restricted to cases with both baseline and follow-up data in which we modeled each outcome at follow-up on an indicator for the intervention, response at baseline, church pair, and demographic and socio-economic/cultural variables. Inferences from that analysis showed no major differences from the models reported here in Table 2 concerning the effectiveness of the intervention.
We also note that random effects or normal survey cluster adjustments could not be applied in this study to control for clustering within churches since there are only five clusters [62]; fixed effects of churches and pairs were the best available means we had to account for the similarity of responses expected within churches and to ensure our standard errors for other predictors in the model are not under-estimated.
Process Evaluation
In addition to the survey assessments, we conducted an extensive process evaluation to explore any variations in implementation across the intervention churches, as well as congregational contextual factors that might have influenced implementation and congregational response to the intervention. The process evaluation included systematic observations of all intervention activities; in addition, the HIV sermons were recorded (with permission) and transcribed verbatim, and HIV education and peer leader workshop participants completed anonymous questionnaires after each workshop to provide feedback. We also conducted telephone follow-up interviews with peer leader workshop participants to explore how well they were able to apply their skills. All data from the observation forms and telephone interview questionnaires as well as the HIV sermon transcripts were entered into Dedoose, a mixed (qualitative and quantitative) methods software program [63]. Qualitative data were coded combining content coding procedures [64–66] and grounded theory approaches [67, 68] to identify themes regarding implementation (e.g., messages transmitted through intervention activities, reactions of congregants to intervention activities, and implementation challenges). Comprehensive results of the process evaluation are reported separately; however, we incorporate here relevant findings related to variations in implementation that might have influenced results.
Results
Sample Characteristics
Table 1 shows the overall sample means across the five churches as well as a comparison of the wave 1 samples in our two complete pairs. The majority of the sample at wave 1 was female (63.2 %) with a mean age of 40.2 years. Approximately two-thirds (68.1 %) had at least a high school diploma or GED, while 32.1 % had less than a high school education and less than 20 % finished higher degrees. Thirty-four percent of the sample was African American; among Latinos, half had low-English proficiency and were foreign born, a quarter had high-English proficiency and were foreign born, and a quarter had high-English proficiency and were born in the US. A third of the sample had a friend or family member with HIV. In terms of HIV stigma, the sample had mean scores on the subscales that ranged between 2.4 for blame and 3.5 for shame. These scores indicate moderate levels of HIV stigma in the study sample. For the constructed HIV stigma scale (α = 0.88), we have a mean of 0.05, which is, as expected, close to 0, given the manner in which the variable was standardized. For HIV mistrust (α = 0.81), the mean was 2.8, suggesting that the sample also had moderate levels of HIV mistrust.
Table 1 also shows how well-balanced our matched church pairs were at baseline. Among the Latino-Pentecostal churches, there were no significant differences between the control and intervention churches. However, for the African-American Baptist churches, several differences emerged. The intervention church had significantly older attendees (mean age of 47.9 vs. 37.0; p < 0.001) with significantly higher educational attainment levels (44.1 vs. 23.4 % with bachelor’s degree or higher; p < 0.01). There were also baseline differences in HIV stigma: the intervention church had significantly lower HIV stigma than the control church (p < 0.01 for the composite scale and for HIV discomfort and shame). Finally, the proportion of the church that had been tested for HIV differed: the intervention church had a smaller proportion than the control church that had ever tested for HIV (68.5 vs. 81.7 %, p < 0.001).
Average Impact of the Intervention on HIV Stigma and Mistrust
Table 2 shows regression results for estimating the average impact of the intervention across the four churches in matched pairs (i.e., not including the large Latino Catholic church). On average, intervention churches at baseline had significantly lower mean levels of HIV stigma than control churches (−0.19 effect size difference; 95 % CI −0.37, −0.01), yet did not differ significantly on HIV mistrust (0.16 effect size difference; 95 % CI −0.03, 0.35). For both outcomes, after controlling for baseline differences, there was no evidence of a differential effect of the intervention in changing mean levels of the outcomes between baseline and wave 2. The adjusted mean differences in change between baseline and follow-up for intervention vs. control churches was −0.16 effect size change for HIV stigma (95 % CI −0.40, 0.08) and −0.11 for HIV mistrust (95 % CI −0.34, 0.11). These results provide no significant evidence that intervention churches changed any more or any less, on average, than control churches on HIV stigma and HIV mistrust during the course of the study.
Among individual control variables, only age was significantly related to the outcomes, with older age being associated with lower HIV stigma (regression coefficient = −0.10; 95 % CI −0.17, −0.03) and lower HIV mistrust (regression coefficient = −0.08; 95 % CI −0.16, −0.01). In models that were restricted to cases with both baseline and follow-up data and that regressed the outcomes on an indicator for the intervention, response at baseline, church pair, and demographic and socio-economic/cultural variables, we also found no significant effect of the intervention on response at follow-up (results not shown); however, we note that model sample sizes are small (N = 157).
Change Within Churches on HIV Stigma and Mistrust
Table 3 shows regression results for estimating changes from baseline to follow-up for all five churches. The Latino Catholic intervention church showed a significant decrease between baseline and follow-up in both HIV stigma and HIV mistrust (effect size change = −0.16; 95 % CI −0.25, −0.06 for HIV stigma; −0.15 for HIV mistrust; 95 % CI −0.24, −0.05). Similarly, the Latino Pentecostal intervention church experienced a significant decrease in both outcomes between baseline and follow-up (effect size change = −0.38 for HIV stigma; 95 % CI −0.71, −0.05; −0.56 for HIV mistrust; 95 % CI −0.86, −0.27). The Latino Pentecostal control church also experienced a significant decline in HIV mistrust during the course of the study (−0.32 effect size decrease; 95 % CI −0.57, −0.07). For the African American Baptist intervention church, we found no significant change between baseline and follow-up, while the African American control intervention church experienced a significant increase in HIV mistrust (0.23 effect sizes; 95 % CI 0.02, 0.45).
Among the individual control variables, female gender was associated with lower HIV stigma and lower HIV mistrust (p < 0.01 and p < 0.05, respectively); older age was associated with lower HIV stigma (p < 0.01); foreign-born Latinos (both high and low English proficiency) had lower HIV stigma and HIV mistrust than African Americans (p < 0.01 and p < 0.001, respectively), and U.S.-born Latinos had lower HIV mistrust than African Americans (p < 0.001); higher education was associated with lower HIV stigma and lower HIV mistrust (p < 0.01 and p < 0.001, respectively); and having a friend or family member who has had HIV was associated with lower HIV stigma (p < 0.001).
Effects on HIV Testing
Figure 1 shows the unadjusted proportion of participants within each church that had an HIV test during the course of the study follow-up. Both the Latino Pentecostal and African American Baptist intervention churches had higher rates of HIV testing during the follow-up than their paired control churches (38 vs. 7 % in the Latino Pentecostal churches and 32 vs. 13 % in the African American Baptist churches). The differences between the intervention and control churches were highly significant in our multivariate logistic model (p < 0.001 for both), providing strong evidence that the intervention had a positive impact on HIV testing rates in these churches. The rate of HIV testing at the Catholic intervention church, which was much larger than the other churches, was lower than the other two intervention churches (16 % at follow-up).
Implementation Differences (From Process Evaluation)
Beyond the differences in congregational size, other contextual differences could have affected intervention implementation across the three churches. The intervention was implemented in each church in the context of its existing group structure, and in accordance with the congregational leaders’ preferences. For example, the pastor of the African American church requested that we combine the HIV education and peer leader workshops into one workshop and conduct it only once with a group of 20 core lay leaders. In the Catholic church, the pastor recommended that we work with various ministry groups to offer the two types of workshops; ultimately, we reached 89 people with one or both types of workshops. In the Latino Pentecostal church, we conducted both types of workshops with the women’s group, and when an HIV educational workshop that was open to others in the congregation went unattended, the pastor had our team conduct the workshop during one of the church’s regularly scheduled worship times, with everyone attending the service; thus, we reached 62 people with the HIV education workshop, or well over half of all adult members.
Implementation of the HIV sermon also varied across the three churches. Textual analysis indicated that the Catholic priests (3 different priests preached across the various religious services the day of the HIV sermon) emphasized how HIV was affecting the community, the stigmatization and marginalization of people with HIV, why congregants should show compassion for people with HIV, and the importance of getting tested. The Pentecostal pastor also talked about how HIV was affecting the community and why congregants should show compassion for people with HIV, but did not emphasize testing as much. The African American pastor admonished congregants to get tested, but did not talk about the negative effects of HIV stigma and the importance of showing compassion.
Discussion
In this pilot study, we successfully implemented a multi-component, stigma-reduction intervention in African American and Latino churches of diverse sizes and religious denominations using a rigorous experimental design. Several features of this study distinguish it from previous research. First, although several church-based HIV interventions are reported in the literature, we know of only one that has used randomization at the church level to assess effectiveness [30]. Second, our primary focus was explicitly on HIV stigma, rather than on general education about HIV prevention, reducing HIV risk behavior, [28, 29] or the promotion of HIV testing [23, 69]. Third, we implemented the intervention in a diverse set of congregational settings. Previous research has identified congregation size (a proxy for resources), race-ethnicity, and denomination as related to the likelihood of HIV programming in churches [20, 70]. Thus, the feasibility of implementing a single, theory-based intervention across settings that vary on these dimensions is encouraging. Our inclusion of Latinos is unique in the congregation-based HIV intervention literature, which has focused overwhelmingly on African American churches [23, 24, 28, 29]. As we note elsewhere [39], this diversity presented challenges in tailoring intervention materials, but provided us with a broader experience of how this kind of an intervention could be implemented.
In terms of effectiveness in reducing HIV-related stigma and mistrust, we found statistically significant reductions in the Latino intervention churches (Catholic and Pentecostal), but not in the African American intervention church, nor when we examined the average effect across the matched pairs of African American Baptist and Latino Pentecostal churches. As this was a pilot study, we were somewhat underpowered to detect effects, given that we only had two matched pairs. The fact that we did find significant reductions in Latino churches is nonetheless promising, particularly since, to our knowledge, there are no reports in the literature of church-based interventions that have significantly reduced stigma. Berkley-Patton et al. [30] reported “decreasing trends” in stigma at 6 months that “approached significance” from their Taking it to the Pews intervention, which was implemented among 4 African American churches in Kansas City. We are not aware of any HIV interventions that have been developed for and implemented in Latino churches.
In terms of HIV testing, we saw significantly higher rates of testing across African American and Latino intervention churches, suggesting that this component was highly successful. We know of only one previous study [71] that examined the effectiveness of church-based HIV testing in a controlled study (i.e., with a comparison church). Further, our analyses of de-identified testing data suggest that these testing events reached many first time testers and uninsured individuals [72]. The lower rate of testing during the intervention period in the Catholic church (16 % of survey participants) compared to the other intervention churches (38 % of survey participants in the Latino Pentecostal church and 32 % of survey participants in the African American Baptist church), may be at least partially explained by size. The Catholic church was 12 times larger than the Latino Pentecostal church and 6 times larger than the African American Baptist church, and the health department experienced challenges meeting demand. It was difficult to conduct counseling and testing procedures with a large group of people who wanted to get tested immediately after worship services. To address this, the health department augmented their usual mobile clinic staff with other staff. However, other staff members were normally not scheduled to work on weekends, and thus adequately staffing multiple events over a short period of time was difficult. Finally, without a control church for comparison, it is difficult to know how this church may have differed from a Catholic church that did not receive the intervention.
An important goal in a pilot study of an intervention is to assess its feasibility and acceptability. In this study, it proved feasible to conduct a multicomponent intervention aimed at reducing HIV stigma in five churches serving mainly racial and ethnic minority populations within an area of Los Angeles County having high HIV prevalence. However, this component involved substantial resources, including HIV education, HIV testing, and counseling provided by a public health department. Even outside a research context, this type of intervention would require active collaboration of the type mounted in this study between church leaders and health professionals. Moreover, it is likely that the impetus for sustaining such a multi-component effort over the weeks and months required would need to come from outside the congregation, given the many competing demands faced by most church leaders. This is consistent with previous research, which has identified the importance of partnership for congregation-based health programming in general [73, 74] and for HIV in particular [21, 25–27].
As for acceptability, it is useful to distinguish two levels of participation: organizational and congregant level. At the organizational level, five of six churches invited to participate agreed to do so. None of these had characteristics that would make them “easy marks” for such an intervention, such as promulgating gay-welcoming messages or having conducted HIV-related programs in the past. Substantial recruitment efforts were required, involving both organizational incentives and persistent follow-up. Churches would likely have been much less willing to participate in the absence of incentives. At the congregant level, however, incentives were only provided to survey participants, not those who participated in intervention activities. Though a minority of congregants participated in the workshops and sometimes a minority participated in the church-based test events, those who did participate did so enthusiastically and provided very positive feedback. Our results therefore indicate that the intervention has broad acceptability to individual congregants. Although the intervention was also acceptable at the organizational level, given sufficient incentive to participate, it may not be intrinsically attractive enough to be adopted by most church leaders for its own sake.
This study was a pilot of the FAITH intervention and thus had a number of limitations. First, given the small number of churches enrolled, the study had limited statistical power. As shown by our results, the effects of the intervention, if they do exist, may be small (approximately −0.12 effect sizes for the HIV stigma scale). Second, our analyses had limitations due to balance, i.e., we cannot completely guard against the possibility that differences found at baseline, particularly between the paired African American churches, may have influenced the results. Third, given the challenges we had in matching at the individual level between baseline and follow-up, our results appear to be from two different samples within the same churches at baseline and follow-up. Generally, the samples at baseline and follow-up within the churches look very similar in terms of characteristics, though the percentage of specific race-ethnic groups varied slightly across the two waves in some churches (data not shown). Finally, although we controlled for many characteristics known to affect HIV stigma and mistrust, unobserved confounding could present a problem.
Nevertheless, our pilot study presents several advances in the science of congregation-based health programming and HIV stigma reduction in particular. Our approach implemented many of the recommendations made by Sengupta et al. [31] to improve studies of HIV stigma reduction interventions, namely: it was based on extensive formative research [33, 34]; we used a multi-dimensional instrument that had undergone psychometric analysis; we used an RCT study design; and we examined whether stigma reduction is accompanied by changes in health outcomes such as HIV testing. Further, by surveying 70+ % of all adult congregants before and after the intervention was implemented, we attempted to measure post- intervention changes at the congregation level rather than only among persons who participated in various intervention components. Because stigma resides in community-level attitudes and practices that devalue stigmatized groups, and not merely in individual attitudes, one of our goals was to change the dynamic within the church around HIV, stigma, and testing. Such change, especially when measured at the community-level, is likely to be incremental, and thus small effect sizes for HIV stigma and mistrust are not surprising. The more robust effects on testing, in spite of the testing capacity issues at the largest church, are also noteworthy given the health department’s previous experiences with very low turnout for HIV testing from congregation members at church-based events in the past. Our intervention activities aimed at reducing HIV stigma and mistrust may have created a climate where HIV testing was more acceptable, and the church-based test events increased access to HIV testing and may have helped normalize HIV as a health issue rather than a moral issue [40, 41]. This line of reasoning suggests that stigma reduction and HIV testing may have synergistic effects when provided in combination.
References
CDC. HIV in the United States: at a glance. Centers for Disease Control and Prevention November 2014. http://www.cdc.gov/hiv/pdf/statistics_basics_ataglance_factsheet.pdf. Accessed 1 March 2015.
CDC. Social determinants of health among adults with diagnosed HIV infection in 20 States, the District of Columbia, and Puerto Rico, 2010. HIV Surveillance Report, volumen 19(2). Centers for Disease Control and Prevention; Revised edition. 2014. http://cdc.gov/hiv/library/reports/surveillance. Accessed 1 March 2015.
CDC. Establishing a Holistic framework to reduce inequities in HIV, Viral Hepatitis, STDs, and tuberculosis in the United States. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2010. http://www.cdc.gov/socialdeterminants/docs/SDH-White-Paper-2010.pdf. Accessed 1 March 2015.
Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–36.
Murray K, Oraka E. Racial and ethnic disparities in future testing intentions for HIV: United States, 2007-2010: results from the National Health Interview Survey. AIDS Behav. 2014;18(7):1247–55.
CDC. HIV Among African Americans. Centers for Disease Control and Prevention. 2014. http://www.cdc.gov/hiv/pdf/risk_HIV_AfricanAmericans.pdf. Accessed 1 March 2015.
Bogart LM, Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005;38(2):213–8.
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77.
CDC. Estimated HIV incidence in the United states, 2007-2010. 2012. http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf. Accessed 1 March 2015.
Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22:S67–79.
Bowles KE, Clark HA, Tai E, Sullivan PS, Song B, Tsang J, et al. Implementing rapid HIV testing in outreach and community settings: results from an advancing HIV prevention demonstration project conducted in seven U.S. cities. Public Health Rep. 2008;123(Suppl 3):78–85.
Pew Forum U.S. A Religious Portrait of African Americans. Pew Research Center’s Religion & Public Life. 2009. http://www.pewforum.org/2009/01/30/a-religious-portrait-of-african-americans/.
Maton KI, Rappaport J. Empowerment in a religious setting. Prev Hum Serv. 1984;3(2–3):37–72.
Maton KI. Community settings as buffers of life stress—highly supportive churches, mutual help groups, and senior centers. Am J Community Psychol. 1989;17(2):203–32.
Maton KI. Patterns and psychological correlates of material support within a religious setting - The bidirectional support hypothesis. Am J Community Psychol. 1987;15(2):185–207.
Levin JS. The role of the black church in community-medicine. J Natl Med Assoc. 1984;76(5):477–83.
Foley MW, Hoge DR. Religion and the new immigrants. How Faith communities form our newest citizens. Oxford: Oxford University Press; 2007. p. 288.
Stepick A, Rey T, Mahler SJ. Churches and charity in the immigrant city: religion, immigration, and civic engagement in Miami. New Brunswick: Rutgers University Press; 2009. p. 336.
Frenk SM, Trinitapoli J. U. S. Congregations’ provision of programs or activities for people living with HIV/AIDS. AIDS Behav. 2013;17(5):1829–38.
Williams MV, Haas A, Griffin BA, Fulton BR, Kanouse DE, Bogart LM, et al. Predictors of the existence of congregational HIV programs: similarities and differences compared with other health programs. Am J Health Promot. 2015;29(6):e225–35.
Agate LL, Cato-Watson D, Mullins JM, Scott GS, Rolle V, Markland D, et al. Churches united to stop HIV (CUSH): a faith-based HIV prevention initiative. J Natl Med Assoc. 2005;97(7 Suppl):60S–3S.
Baldwin JA, Daley E, Brown EJ, August EM, Webb C, Stern R, et al. Knowledge and perception of STI/HIV risk among rural African-American youth: LESSONS learned in a faith-based pilot program. J HIV AIDS Prev Child Youth. 2008;9(1):97–114.
Berkley-Patton J, Bowe-Thompson C, Bradley-Ewing A, Hawes S, Moore E, Williams E, et al. Taking it to the pews: a CBPR-guided HIV awareness and screening project with black churches. AIDS Educ Prev. 2010;22(3):218–37.
Berkley-Patton J, Moore EW, Hawes SM, Thompson CB, Bohn A. Factors related to HIV testing among an African American church-affiliated population. AIDS Educ Prev. 2012;24(2):148–62.
Marcus MT, Walker T, Swint JM, Smith BP, Brown C, Busen N, et al. Community-based participatory research to prevent substance abuse and HIV/AIDS in African-American adolescents. J Interprof Care. 2004;18(4):347–59.
Tyrell CO, Klein SJ, Gieryic SM, Devore BS, Cooper JG, Tesoriero JM. Early results of a statewide initiative to involve faith communities in HIV prevention. J Public Health Manag Pract. 2008;14(5):429–36.
MacMaster SA, Jones JL, Rasch RER, Crawford SL, Thompson S, Sanders EC. Evaluation of a faith-based culturally relevant program for African American substance users at risk for HIV in the Southern United States. Res Soc Work Pract. 2007;17(2):229–38.
Griffith DM, Pichon LC, Campbell B, Allen JO. Your blessed health: a faith-based CBPR approach to addressing HIV/AIDS among African Americans. AIDS Educ Prev. 2010;22(3):203–17.
Wingood GM, Simpson-Robinson L, Braxton ND, Raiford JL. Design of a faith-based HIV intervention: successful collaboration between a university and a church. Health Promot Pract. 2011;12(6):823–31.
Berkley-Patton J, Moore E, Berman M, Simon SD, Thompson CB, Schleicher T, et al. Assessment of HIV-related stigma in a US faith-based HIV education and testing intervention. J Int AIDS Soc. 2013;16(Suppl 2):18644.
Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87.
Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 Suppl 2):18734.
Derose KP, Mendel PJ, Palar K, Kanouse DE, Bluthenthal RN, Castaneda LW, et al. Religious congregations’ involvement in HIV: a case study approach. AIDS Behav. 2011;15(6):1220–32.
Bluthenthal RN, Palar K, Mendel P, Kanouse DE, Corbin DE, Derose KP. Attitudes and beliefs related to HIV/AIDS in urban religious congregations: barriers and opportunities for HIV-related interventions. Soc Sci Med. 2012;74(10):1520–7.
Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. 2006;90(5):751–83.
Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003;15(1):49–69.
Heijnders M, Van Der Meij S. The fight against stigma: an overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–63.
Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–79.
Derose KP, Bogart LM, Kanouse DE, Felton A, Collins DO, Mata MA, et al. An intervention to reduce HIV-related stigma in partnership with African American and Latino churches. AIDS Educ Prev. 2014;26(1):28–42.
Koch JR, Beckley RE. Under the radar: AIDS ministry in the Bible belt. Rev Relig Res. 2006;47(4):393–408.
McNeal C, Perkins I. Potential roles of black churches in HIV/AIDS prevention. J Hum Behav Soc Environ. 2007;15(2–3):219–32.
Long Beach Department of Health and Human Services. HIV/AIDS monitoring report; 2013. http://www.longbeach.gov/health/media-library/documents/planning-and-research/reports/hiv-reports/hiv-aids-monitoring-report/hiv-aids-monitoring-report-december-2013/. Accessed 23 Oct 2015.
CDC. HIV in the United States: The stages of care. Atlanta, Centers for Disease Control and Prevention, 2012. http://www.cdc.gov/hiv/pdf/research_mmp_StagesofCare.pdf. Accessed 1 March 2015.
Miller WR, Rollnick S. Motivational interviewing: preparing people for change. 2nd ed. New York: Guilford Press; 2002.
Blair IV, Ma JE, Lenton AP. Imagining stereotypes away: the moderation of implicit stereotypes through mental imagery. J Pers Soc Psychol. 2001;81(5):828–41.
Crisp RJ, Turner RN. Can imagined interactions produce positive perceptions? Reducing prejudice through simulated social contact. Am Psychol. 2009;64(4):231–40.
Hawes-Dawson J, Derose KP, Aunon F, Dominguez BX, Felton A, Mata M, et al. Achieving broad participation in congregational health surveys at African American and Latino churches. Field Methods (in press).
Herek GM, Capitanio JP. AIDS stigma and sexual prejudice. Am Behav Sci. 1999;42(7):1130–47.
Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–43.
Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007;64(9):1823–31.
Herek GM. AIDS and stigma. Am Behav Sci. 1999;42(7):1106–16.
Lauby JL, Bond L, Eroglu D, Batson H. Decisional balance, perceived risk and HIV testing practices. AIDS Behav. 2006;10(1):83–92.
Gibbons R, Hedeker D. Full-information item bi-factor analysis. Psychometrika. 1992;57(3):423–36.
Bogart LM, Wagner G, Galvan FH, Banks D. Conspiracy beliefs about HIV are related to antiretroviral treatment nonadherence among African American men with HIV. J Acquir Immune Defic Syndr. 2010;53(5):648–55.
Muturi N, An S. HIV/AIDS stigma and religiosity among African American women. J Health Commun. 2010;15(4):388–401.
Lindley LL, Coleman JD, Gaddist BW, White J. Informing faith-based HIV/AIDS interventions: HIV-related knowledge and stigmatizing attitudes at Project F.A.I.T.H. churches in South Carolina. Public Health Rep. 2010;125(Suppl 1):12–20.
Herek GM, Capitanio JP. AIDS stigma and contact with persons with AIDS: effects of direct and vicarious contact. J Appl Soc Psychol. 1997;27(1):1–36.
Mall S, Middelkoop K, Mark D, Wood R, Bekker LG. Changing patterns in HIV/AIDS stigma and uptake of voluntary counselling and testing services: the results of two consecutive community surveys conducted in the Western Cape, South Africa. AIDS Care. 2013;25(2):194–201.
Nambiar D, Rimal RN. Duty and destiny: psychometric properties and correlates of HIV-related stigma among youth NGO workers in Delhi, India. AIDS Care. 2012;24(11):1384–91.
Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regresion models. Surv Methodol. 2001;27(1):85–95.
Belin TR, Ishwaran H, Duan N, Berry SH, Kanouse DE. Identifying likely duplicates by record linkage in a survey of prostitutes. In: Gleman A, Meng X-L, editors. Applied Bayesian modeling and causal inference from incomplete-data perspectives: an essential journey with Donald Rubin’s statistical family. Hoboken: Wiley; 2004. p. 319–39.
Kreft GG, De Leeuw J. Introducing multilevel modeling. Thousand Oaks: Sage Publications; 1998.
Dedoose Version 5.0.11, web application for managing, analyzing, and presenting qualitative and mixed method research data [Internet]. SocioCultural Research Consultants, LLC. 2014. www.dedoose.com.
Altheide D. Qualitative media analysis. Thousand Oaks: Sage Publications; 1996.
Strauss A, Corbin J. Basics of qualitative research. Thousand Oaks: Sage Publications; 1990.
Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. 2nd ed. Thousand Oaks: Sage Publications; 1994.
Krippendorff K. Content analysis: an introduction to its methodology. Beverly Hills: Sage Publications; 1980.
Weber RP. Basic Content Analysis. 2nd ed. Newbury Park: Sage Publications; 1990.
Lightfoot M, Rotheram-Borus MJ, Towns B, Cline TR, Webber D, Murphy DA, et al. Religious groups as diffusers of HIV antidody testing and prevention messages. J Commun Psychol. 2001;29(4):459–72.
Tesoriero JM, Parisi DM, Sampson S, Foster J, Klein S, Ellemberg C. Faith communities and HIV/AIDS prevention in New York State: results of a statewide survey. Public Health Rep. 2000;115(6):544–56.
Berkley-Patton J, Moore E, Hawes S, Berman M, Thompson CB, Simon S. A faith-based HIV education and testing intervention: pilot study six-month findings. Ann Behav Med. 2014;47:S259-S.
Williams MV, Derose KP, Aunon F, Kanouse DE, Bogart LM, Griffin BA, et al. Church-based HIV screening in racial/ethnic minority communities of California, 2011–2012. Public Health Rep. (in press).
Steinman KJ, Bambakidis A. Faith-health collaboration in the United States: results from a nationally representative study. Am J Health Promot. 2008;22(4):256–63.
Trinitapoli J, Ellison CG, Boardman JD. US religious congregations and the sponsorship of health-related programs. Soc Sci Med. 2009;68(12):2231–9.
Acknowledgments
This study was supported by Grant Number 1 R01 HD050150 (Derose) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). Its contents are solely the responsibility of the authors and do not represent the official views of NICHD. The authors thank the study’s Community Advisory Board, especially Delis Alejandro, the Rev. Chris Ponnet, Mario Pérez, Sophia Rumanes, Renee Stampolis, and Richard Zaldivar, who provided excellent guidance and counsel throughout the study. We also thank the five churches that participated in our study, which, for confidentiality reasons, are not named. Finally, we acknowledge our former colleagues at RAND and the Long Beach Department of Health and Human Services (LBDHHS), who assisted with study implementation, Blanca Domínguez, Alexandria Felton, Frances Aunon, and Alexandria Smith (RAND) and Kerry Brown, Carlos Campos, and Patricia Montes (LBDHHS).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Derose, K.P., Griffin, B.A., Kanouse, D.E. et al. Effects of a Pilot Church-Based Intervention to Reduce HIV Stigma and Promote HIV Testing Among African Americans and Latinos. AIDS Behav 20, 1692–1705 (2016). https://doi.org/10.1007/s10461-015-1280-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1280-y