Abstract
The FDA approval of emtricitabine/tenofovir disoproxil fumarate for pre-exposure prophylaxis (PrEP) in 2012 has raised questions about the delivery of PrEP in a real-world setting. iPad-based questionnaires were given to providers at conferences in California and New York to assess knowledge, experience and attitudes regarding PrEP in HIV and non-HIV providers. HIV provider status was defined either by self-identification or by having greater than 5 years of HIV care experience. Knowledge scores were the sum of correct answers from five PrEP knowledge questions. Univariate analyses used t-test to compare knowledge scores and Fisher’s exact test for past or future PrEP prescription between HIV and non-HIV providers. Multivariable linear or logistic regression models were used to assess factors associated with the outcomes. Of 233 respondents, the mean age was 40 years, 59 % were White, 59 % were physicians and 52 % were HIV providers. In univariate analysis, mean PrEP knowledge scores (max 5) were significantly higher for HIV providers (2.8 versus 2.2; p < 0.001), age > 41 (mean 2.8 versus 2.3; p = 0.004), White race (2.7 versus 2.2; p = 0.026) and participants in the New York region (3.0 versus 2.3; p < 0.001). In a multivariable model of knowledge scores, all but age remained significant. Among 201 potential prescribers, the rate of prior PrEP prescription was higher among HIV providers than non-HIV providers (34 versus 9 %; p < 0.001) and by knowledge score, but the association with provider status was no longer significant in multivariable analysis that controlled for knowledge. Intent to prescribe PrEP in the future was high for all provider types (64 %) and was associated with knowledge scores in multivariable analysis. The most common concerns about PrEP (>40 % of providers) were drug toxicities, development of resistance and patient adherence to follow-up; 32 % identified risk compensation as a concern. HIV providers had significantly greater PrEP knowledge than non-HIV providers, but differences by provider type in past PrEP prescription were largely dependent on knowledge. Future PrEP prescription was also associated with knowledge, though all providers expressed greater future use. Education of potential PrEP providers will be a key component of successful PrEP implementation.
Resumen
La aprobación de Emtricitabina/Fumarato de Disoproxilo de Tenofovir por la FDA para PrEP en 2012 ha originado preguntas acerca del suministro de profilaxis pre-exposición (PrEP) en un escenario real. Cuestionarios a través de dispositivo iPad fueron proporcionados a proveedores de salud especialistas en VIH y proveedores de salud en general durante conferencias en California y Nueva York para evaluar conocimiento, experiencia y actitudes en cuanto a PrEP. La categoría de proveedor de salud especialista en VIH fue definida por identificación propia o por tener más de cinco años de experiencia en el cuidado de VIH. Los marcadores de conocimiento fueron la suma de respuestas correctas a cinco preguntas de conocimiento sobre PrEP. El análisis univariado utilizó la prueba t-test para comparar los marcadores de conocimiento y la prueba exacta Fisher se utilizó para pasadas o futuras prescripciones médicas de PrEP entre proveedores de salud especialistas en VIH y proveedores de salud en general. Los modelos linear multivariable o de regresión logística fueron utilizados para evaluar factores asociados con los resultados. De 233 encuestados, la edad promedio fue 40 años, 59 % fueron raza Blanca, 59 % fueron médicos y 52 % fueron proveedores de salud especialistas en VIH. En análisis univariado, el promedio en el marcador de de conocimientos sobre PrEP (max 5) fue significativamente mayor para proveedores de salud especialistas en VIH (en un 2.8 versus 2.2; p<0.001), edad >41 (promedio 2.8 versus 2.3; p=0.004), raza blanca (2.7 versus 2.2; p=0.0.26) y los participantes de la region de Nueva York (3.0 versus 2.3; p<0.001). En el modelo multivariable de marcadores de conocimiento, todo excepto la edad permaneció significantivo. Entre 201 potenciales proveedores que prescribirán una receta médica para PrEP, el índice de haber prescrito con aterioridad fue mayor entre proveedores de salud especialistas en VIH que en los proveedores de salud en general (34 % versus 9 %; p<0.001) en cuanto a marcador de conocimiento, la asociacion de la categoría de los proveedores de salud no fue significantiva en el anáslisis multivariable que controló el conocimiento. Los planes de prescribir PrEP en un futuro fue mayor para los dos tipos de proveedores de salud (64 %) y estuvo asociada con los marcadores de conocmiento en el análisis multivariable. Las preocupaciones más communes en cuanto a PrEP (>40 % de los proveedores) fue la toxicidad del medicamento, desarrollo de Resistencia y la adherencia o apego de parte del paciente; 32 % identificaron a la compensación de riesgo como una preocupación. Proveedores de salud especialistas en VIH tuvieron un conocimiento de PrEP significativamente mayor que los proveedores de salud en general, pero las diferencias entre los tipos de proveedor en prescripciones médicas de PrEP anteriores fueron ampliamente dependientes del conocimiento. Prescripciones médicas de PrEP futuras fue asociado con conocimiento, sin embargo todos los proveedores expresaron una mayor utilización en el futuro. La educación sobre PrEP en proveedores de salud será un componente clave en el éxito de la implementación de PrEP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pre-exposure prophylaxis (PrEP) with tenofovir disoproxil fumarate (TDF) and emtricitibine (FTC) combined with comprehensive prevention services that include HIV testing, sexually transmitted infection screening and risk reduction counseling is an effective HIV prevention strategy as demonstrated in several randomized controlled trials [1–3]. In July 2012, the FDA approved a once daily fixed dose combination of FTC/TDF to reduce the risk of HIV infection in uninfected individuals at high risk of HIV infection and who may engage in sexual activity with HIV-infected or partners of unknown HIV serostatus [4]. The FDA approval has raised questions about the challenges facing the successful delivery of PrEP in real-world settings, especially in regard to which clinicians and care settings will serve as prescribers and how they will be educated about this HIV prevention strategy.
Before and after PrEP approval, several quantitative and qualitative studies were conducted on healthcare providers’ knowledge, perception and willingness to adopt PrEP implementation guidelines [5–9]. Overall, these studies showed high levels of awareness, though limited experience and variable willingness to prescribe PrEP. Concerns cited with the use of FTC/TDF for PrEP included the potential for drug resistance if HIV infection were to occur, cost, side effects, limited data regarding PrEP efficacy and the potential for risk compensation (i.e., increased practice of higher-risk behaviors due to reduced fear of HIV infection).
While these studies were informative about provider perceptions and acceptance of PrEP as an HIV prevention tool, the study populations consisted of providers potentially knowledgeable about PrEP or engaged in HIV prevention: infectious diseases specialists and HIV, community health clinic, STD and family planning clinic providers. Given the changing face of healthcare systems and the need to reduce expenditures with potential closures of STD and family planning clinics, primary care providers may have an increasingly important role in HIV prevention. In addition, in order to maximize the public health effectiveness of PrEP in real-world settings, a variety of healthcare providers will need to be able to prescribe PrEP.
In order to achieve rapid and successful implementation of PrEP, it is important to understand health care providers’ knowledge about and their interest in providing and monitoring PrEP, as well as their perceived assessment of potential barriers. This information will serve as a framework for defining critical educational needs and informing public health rollout strategies. In this study, we compared HIV and non-HIV providers to: (a) quantitate PrEP knowledge, (b) determine the current rate of PrEP prescription, (c) evaluate attitudes towards future PrEP provision, and (d) determine barriers and motivators to PrEP provision.
Methods
Study Population
HIV and non-HIV healthcare providers were invited to participate at HIV-related medical conferences and meetings in three high HIV-prevalence cities: New York, San Diego and Los Angeles. Participants included attendees at an International AIDS Society-USA (IAS-USA) meeting in New York City, those at AIDS rounds at University of California San Diego (UCSD), general internists at Medical Grand Rounds at UCSD and Scripps Mercy Hospital, and UCSD internal medicine and family medicine residents at formal didactic lectures. Providers who work at the UCSD HIV or Infectious Diseases Clinics and regularly attend AIDS rounds but were not present when the study were offered were asked to complete the survey during their office hours. HIV providers in Los Angeles who are part of a Southern California research group with access to the iPads but with no prior knowledge of this study were also asked to complete the survey during their office hours.
Self-administered, iPad-Based, PrEP Survey
Participants were asked to complete a 35-question, self-administered, iPad-based survey designed to assess knowledge and experience with PrEP, as well as to evaluate perceived advantages and disadvantages of PrEP being provided by clinicians who do and do not generally care for HIV-infected persons and high-risk, HIV-uninfected individuals. A UCSD IRB-approved abbreviated consent was used, as it was determined that the research presented no more than minimal risk of harm to subjects. If subjects agreed to participate in the study after reading this consent form provided on the iPad, they were instructed to click “Agree” to accept the terms of the study. Study participants that completed the survey received a $5 Starbucks card. The survey was implemented using the iOS application iFormES (ref: https://www.iformbuilder.com/) and custom software libraries developed by the UCSD CFAR Bioinformatics and Information Technologies Core (ref: https://cfar.ucsd.edu/bit/). These software tools enabled the study staff to rapidly and securely collect surveys in the field in time-limited settings. At the completion of each individual survey, data was automatically uploaded to a secure remote data server and deleted from the local device thereby facilitating data privacy and completeness.
Survey Measures
The content of the survey was based on an instrument developed at the Fenway Institute [6], but modified to include specific knowledge-based questions and attitudes about the use of PrEP in the real-world. To evaluate barriers to PrEP provision, participants were given a list of potential concerns including drug toxicities, ART resistance, dosing frequency, limited provider reimbursement, increase in risk behaviors, patient monitoring/follow up, patient adherence, cost, insurance coverage and community backlash. Participants were allowed to select more than one response. Participants were asked to rate PrEP motivators using a Likert scale from not at all to very much that included patient request, providers, CDC recommendations, other societal guidelines, new study results and ease of obtaining PrEP medication. Participants were given statements about PrEP that aimed to assess their views about how PrEP should be used and offered and the impact it could have on both individual and global levels. They were asked to what extent they agreed or disagreed with statements such as “Patients would benefit from knowing about PrEP” and “Patients without HIV will not adhere to PrEP well enough to prevent infection” to examine these normative believes.
PrEP Knowledge Score
PrEP knowledge score was calculated by answering five basic questions about PrEP (Appendix A in Supplementary Material). Each correct answer was worth 1 point giving a knowledge score range of 0–5. The Kuder and Richardson Formula 20 (KR-20) was used to check the internal consistency of the provider knowledge score.
Statistical Analysis
Participant characteristics were summarized overall and were stratified by HIV provider status. Respondents were classified as HIV providers if they either self-defined as a primary HIV provider or if they indicated greater than 5 years of HIV experience. Knowledge scores were compared between HIV providers and non-HIV providers using the two-sample t-test. A multivariable linear regression model was used to study factors associated with higher knowledge scores, including age, race, region, practice setting and HIV provider status.
For the analyses of past and future PrEP prescriptions, we only included potential prescribers (i.e. physician, nurse, nurse practitioner, pharmacist and medical students). We included nurses, pharmacists and medical students for past and future PrEP prescription because they have the medical background to recommend PrEP and refer individuals to their physicians for prescription. Fisher’s exact tests were used to assess the univariate associations of prior PrEP prescribing and future intent to prescribe PrEP with HIV provider status and other co-variates that were considered to be potentially significant factors based on external clinical judgment. Multivariable logistic regression models were used to assess factors associated with prior PrEP prescribing, including age, race, region, practice setting, HIV provider status and knowledge score. Since HIV provider status and knowledge scores were found to be associated, two separate multivariable models were developed, one with the knowledge score and one without.
Other outcomes such as motivators and barriers to successful PrEP implementation were summarized by HIV provider status and overall. Statistical analyses were performed in R (http://cran.r-project.org), version 3.0.2.
Results
Participant Demographics and Characteristics
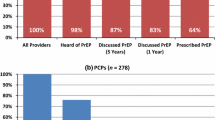
A total of 233 participants completed the survey. The mean age of participants was 40 years and 60 % were female. Nearly 70 % of participants were from Southern California and 27 % were from the tri-state area of New York, New Jersey and Connecticut. Fifty-nine percent were white, 19 % were Asian, 7 % were black and 70 % were non-Hispanic. Based on the above definition, 52 % of participants were HIV providers. Almost 60 % of participants were physicians, 13 % were nurse practitioners and about 6 % each were nurses, social workers and medical students. When asked to identify their primary area of medicine, 34 % chose internal medicine, 21 % HIV, 15 % infectious diseases and 13 % family medicine. The majority of participants, 62 %, worked in academic settings, whereas 20 % worked in community settings and only 5 % were in private practice. Overall, 85 % of participants reported being aware of PrEP prior to the study (See Table 1 for participant characteristics).
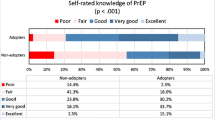
PrEP Knowledge
Overall, the average knowledge score for participants was 2.5. In univariate analysis, mean PrEP knowledge scores were significantly higher for HIV providers (2.8 versus 2.2; p < 0.001), age > 41 (mean 2.8 versus 2.3; p = 0.004), white race (2.7 versus 2.2; p = 0.026) and practicing in the NY region (3.0 versus 2.3; p < 0.001). Knowledge scores were also significantly higher for those who had previously prescribed post-exposure prophylaxis (PEP) (3.1 versus 2.2, p < 0.001), those who asked about sex practices (2.8 for those who asked all of their patients versus 2.0 for some versus 2.2 for few; p = 0.004) and those who felt comfortable determining if someone was a good candidate for PrEP (2.8 for those who felt very comfortable versus 2.5 for somewhat uncomfortable versus 2.0 for very uncomfortable; p = 0.005). In the multivariable analysis, being an HIV provider, from the NY region and white remained statistically significantly associated with PrEP knowledge (See Table 2). The KR-20 for internal consistency of PrEP knowledge score had an alpha score of 0.22. The reason for the finding of poor internal consistency may be due to having only 5 questions and the fact that the questions asked about more than one construct (e.g., specific data about clinical trials results and CDC guidance recommendations).
Prior PrEP Prescription
Out of 201 possible providers, 21 % reported previously having prescribed PrEP. In univariate analysis, prior PrEP prescription occurred significantly more often among HIV providers (p < 0.001), older providers (p < 0.001), those from the NY region (p = 0.006), those with higher knowledge scores (p < 0.001), private practitioners (p < 0.001), those who asked patients about sex practices (p = 0.004) and those who felt most comfortable determining PrEP candidacy (p = 0.027). Two multivariable analyses were done, which differed by inclusion (or not) of the PrEP knowledge variable. In the multivariable model 1, being an HIV provider and a private practitioner remained statistically significant; however, when knowledge was included in the model 2, HIV provider status was no longer significant, suggesting the knowledge score confounded (or accounted for) the effect of being an HIV provider (Table 2).
Future PrEP Prescription
Of 201 possible providers, 64 % reported being likely or very likely to prescribe PrEP in the future. In univariate analysis, there was no difference in likelihood of providing PrEP in the future by provider status (60 versus 66 % for HIV and non-HIV providers, p = 0.2). Future prescription was reported significantly more frequently in providers with greater PrEP knowledge, those from the New York region and those who had previously prescribed PEP (all p < 0.05). In multivariable model 1, which did not include knowledge score, being from the New York region was the only covariate that remained statistically significant. However, when knowledge score was included in model 2, being from the New York region remained significant, while HIV providers were at significantly lower odds of reporting intentions to prescribe PrEP in the future (Table 2).
Perceived Barriers and Motivators to PrEP
More than 40 % of providers reported that drug toxicities, development of resistance and patient adherence to follow-up might limit their willingness to prescribe PrEP. Thirty-six percent identified cost and unclear insurance coverage as additional concerns. About one-third cited risk compensation as a concern about prescribing PrEP; more HIV providers were concerned than non-HIV providers (39 versus 24 % respectively; p = 0.017). The majority (>80 %) of providers agreed that new studies showing efficacy, patient request, ease of patient obtaining PrEP and recommendations from CDC would likely increase their use of PrEP. Only 2 % of providers thought that PrEP should not be reimbursed.
Who Should Provide PrEP
Participants were asked which types of providers/clinics should provide PrEP. The most common responses were in HIV provider clinics (35 %), non-HIV provider clinics (31 %) and public health departments (21 %); only 10 % felt that STD clinics would be adequate places to dispense PrEP. There was no difference in response to where PrEP should be provided by any participant characteristic (i.e., HIV versus non-HIV provider or demographics) (See Table 3).
Normative Beliefs About PrEP
Overall, there was no difference in global beliefs about PrEP between HIV and non-HIV providers. Providers who reported being more likely to prescribe PrEP in the future were more likely to agree with the statement that individuals would benefit from knowing about PrEP (p < 0.001) and disagree with the statement that none of their patients would take PrEP even if it were recommended (p = 0.008).
Discussion
Our study uniquely set out to compare HIV providers with clinicians who have had little to no experience with PrEP, but will likely play an important role in real-world PrEP implementation. We found that HIV providers had significantly greater knowledge about PrEP and were more likely to have prescribed PrEP than non-HIV providers. Based on multivariable models, the greater odds of HIV providers having prescribed PrEP, compared to non-HIV providers, was largely explained by including PrEP knowledge in the model. The proportion of clinicians that responded positively to prescribing PrEP in the future was more than 60 %, and intentions to prescribe PrEP were associated with greater knowledge about PrEP. Interestingly, models that included provider type and knowledge suggested a decrement in potential future PrEP prescription for HIV compared to non-HIV providers, but the actual difference between groups was small (60 versus 68 %, respectively). Regional differences in past and future PrEP prescription could be largely, though not completely, be explained by knowledge.
The key finding that provider knowledge about PrEP was associated with both past and potential future initiation of PrEP should be emphasized. A similar result was seen in a study in 2012 in the Southern United States, which found that a greater willingness to prescribe PrEP was associated with higher PrEP knowledge scores [5]. It must be noted that overall PrEP knowledge was low at 50 %. Education of potential PrEP providers about PrEP basics through avenues such as Continuing Medical Education courses, medical school and residency training didactics, online training and webinars developed by clinical experts in the field has the potential to increase knowledge of PrEP and subsequent intention to prescribe.
In addition to possessing PrEP knowledge, this prevention strategy can only be effectively implemented if providers feel comfortable asking about their patient’s sex practices and drug use and assessing risk for HIV acquisition. Having frank conversations about sexual practices and behaviors are not always easy and are often deferred among providers of primary care [10], STI care [11] and HIV care [12–14]. Furthermore, determining who is at “substantial risk of HIV acquisition,” as recommended in the CDC Clinical Practice Guideline for PrEP [15], may also pose a challenge as “substantial risk” may have different meanings for different providers. Thus, individual interpretation and variation could be substantial [16–20.] CDC guidance on sexual risk assessment is available [15, 21, 22]; brief questions to identify both MSM and heterosexual men and women who may be engaging in high-risk sexual practices, which are associated with the risk of HIV acquisition, were developed from epidemiological studies [23–26]. If PrEP delivery does occur across disciplines, all providers who may encounter individuals likely to benefit from PrEP should be able to assess risk and prescribe PrEP safely.
Another interesting finding from our study is the impact of practice region on differences in PrEP knowledge and willingness to prescribe in the future. While it should be noted that New York participants were almost entirely HIV providers, these differences persisted even when controlling for provider status. The idea of PrEP as a prevention strategy arrived earlier in large urban cities with high HIV prevalence such as New York City, San Francisco and Boston, which may explain why knowledge scores were higher among New York-based providers. However it is more difficult to understand the differences in future prescription between these two regions. Perhaps the disparity can be ascribed to more liberal values or PrEP familiarity in the New York area compared to Southern California that could explain why Southern California providers report being less likely to prescribe PrEP in the future. Although we found differences in knowledge that could be hypothesized to drive differences in future prescribing intentions, the HIV provider populations may not be comparable given how they were sampled. Indeed, there were more female (p = 0.015) and community-based providers (p = 0.001) in New York versus Southern California. In addition, New York providers were more likely to have previously prescribed PEP (p < 0.001). Further studies of regional attitudes need to be conducted.
We also examined provider beliefs about who would be best equipped to prescribe PrEP. When given a list of potential PrEP providers, both HIV and non-HIV providers more commonly (34–39 %) identified themselves as best suited to prescribe PrEP. Although the numbers were fairly consistent between HIV and non-HIV providers across potential PrEP providers, the most common response in both provider groups was that they felt they could prescribe PrEP. However, the lack of consensus about the ideal provider setting for PrEP provision may indicate that the purview paradox characterized in 2012 [27], where HIV specialists believe that PCPs would be best positioned to prescribe PrEP, could be less prominent today. Provider beliefs about their role in PrEP provision may indeed be evolving.
A unique aspect of this study was how data was collected. A self-administered, iPad-based survey offered a private, fast and convenient means of collecting data. These factors combined with a small incentive resulted in a response rate we informally estimated to be over 75 % of those approached, a response rate above mailed and online surveys reported in other studies [28, 29]. Furthermore, the data collected were immediately uploaded to remote servers and cleared from the iPad upon survey completion; facilitating data privacy and allowing study researchers to access the information immediately for analysis.
Limitations of this study include the use of convenience sampling, which may introduce selection bias. Individuals attending an IAS-USA conference and the other venues from which participants were recruited may not represent the opinions of clinicians who do not attend such conferences. As noted above, the sampling methods may have contributed to the regional differences seen. In addition, study results may not be generalizable to individuals located in other regions of the country. The length of the survey could have lead to response fatigue and resultant measurement error. In addition, the knowledge test was designed a priori and measured specific aspects of PrEP knowledge. However, since it has not been formally validated, the study results that rely on this assessment should be considered hypothesis-generating about the relationship between knowledge and PrEP experience and intentions, but not definitive.
Education of potential PrEP providers with current guidelines, instructing them on risk assessment and appropriate sexual history taking, and addressing providers’ major concerns about prescribing PrEP will be a key component of successful PrEP implementation. Giving providers the knowledge and tools (e.g., guidance documents, insurance information support and risk calculators) to be able to prescribe PrEP in the real-world could greatly enhance PrEP sustainability outside of the research arena.
References
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. doi:10.1056/NEJMoa1110711.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. doi:10.1056/NEJMoa1011205.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi:10.1056/NEJMoa1108524.
FDA. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm312210.htm 2012. Accessed 12 March 2013.
Tripathi A, Ogbuanu C, Monger M, Gibson JJ, Duffus WA. Preexposure prophylaxis for HIV infection: healthcare providers’ knowledge, perception, and willingness to adopt future implementation in the southern US. South Med J. 2012;105(4):199–206. doi:10.1097/SMJ.0b013e31824f1a1b.
White JM, Mimiaga MJ, Krakower DS, Mayer KH. Evolution of Massachusetts physician attitudes, knowledge, and experience regarding the use of antiretrovirals for HIV prevention. AIDS Patient Care STDs. 2012;26(7):395–405. doi:10.1089/apc.2012.0030.
Puro V, Palummieri A, De Carli G, Piselli P, Ippolito G. Attitude towards antiretroviral pre-exposure prophylaxis (PrEP) prescription among HIV specialists. BMC Infect Dis. 2013;13:217. doi:10.1186/1471-2334-13-217.
Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58(5):704–12. doi:10.1093/cid/cit796.
Mimiaga MJ, White JM, Krakower DS, Biello KB, Mayer KH. Suboptimal awareness and comprehension of published preexposure prophylaxis efficacy results among physicians in Massachusetts. AIDS Care. 2014;26(6):684–93. doi:10.1080/09540121.2013.845289.
Wimberly YH, Hogben M, Moore-Ruffin J, Moore SE, Fry-Johnson Y. Sexual history-taking among primary care physicians. J Natl Med Assoc. 2006;98(12):1924–9.
Kurth AE, Holmes KK, Hawkins R, Golden MR. A national survey of clinic sexual histories for sexually transmitted infection and HIV screening. Sex Transm Dis. 2005;32(6):370–6.
Laws MB, Bradshaw YS, Safren SA, Beach MC, Lee Y, Rogers W, et al. Discussion of sexual risk behavior in HIV care is infrequent and appears ineffectual: a mixed methods study. AIDS Behav. 2011;15(4):812–22. doi:10.1007/s10461-010-9844-3.
Metsch LR, Pereyra M, del Rio C, Gardner L, Duffus WA, Dickinson G, et al. Delivery of HIV prevention counseling by physicians at HIV medical care settings in 4 US cities. Am J Public Health. 2004;94(7):1186–92.
Duffus WA, Barragan M, Metsch L, Krawczyk CS, Loughlin AM, Gardner LI, et al. Effect of physician specialty on counseling practices and medical referral patterns among physicians caring for disadvantaged human immunodeficiency virus-infected populations. Clin Infect Dis. 2003;36(12):1577–84. doi:10.1086/375070.
Centers for Disease Control aP. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States - 2014 Clinical Practice Guideline 2014. http://www.cdc.gov/hiv/pdf/PrEPguidelines2014.pdf. Accessed 23 June 2014.
Khawcharoenporn T, Kendrick S, Smith K. HIV risk perception and preexposure prophylaxis interest among a heterosexual population visiting a sexually transmitted infection clinic. AIDS Patient Care STDs. 2012;26(4):222–33. doi:10.1089/apc.2011.0202.
Whiteside YO, Harris T, Scanlon C, Clarkson S, Duffus W. Self-perceived risk of HIV infection and attitudes about preexposure prophylaxis among sexually transmitted disease clinic attendees in South Carolina. AIDS Patient Care STD. 2011;25(6):365–70. doi:10.1089/apc.2010.0224.
Pringle K, Merchant RC, Clark MA. Is self-perceived HIV risk congruent with reported HIV risk among traditionally lower HIV risk and prevalence adult emergency department patients? Implications for HIV testing. AIDS Patient Care STD. 2013;27(10):573–84. doi:10.1089/apc.2013.0013.
Klein H, Tilley DL. Perceptions of HIV risk among internet-using, HIV-negative barebacking men. Am J Men’s Health. 2012;6(4):280–93. doi:10.1177/1557988311434825.
Peterson JL, Rothenberg R, Kraft JM, Beeker C, Trotter R. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res. 2009;24(1):119–27. doi:10.1093/her/cyn003.
Centers for Disease Control. A guide to taking a sexual history. http://www.cdc.gov/std/treatment/SexualHistory.pdf. Accessed 23 June 2014.
Lanier Y, Castellanos T, Barrow RY, Jordan WC, Caine V, Sutton MY. Brief sexual histories and routine HIV/STD testing by medical providers. AIDS Patient Care STDs. 2014;28(3):113–20. doi:10.1089/apc.2013.0328.
Jenness SM, Neaigus A, Murrill CS, Wendel T, Forgione L, Hagan H. Estimated HIV incidence among high-risk heterosexuals in New York City, 2007. J Acquir Immune Defic Syndr. 2011;56(2):193–7. doi:10.1097/QAI.0b013e318202a9c4.
LaLota M, Beck DW, Metsch LR, Brewer TH, Forrest DW, Cardenas GA, et al. HIV seropositivity and correlates of infection among heterosexually active adults in high-risk areas in South Florida. AIDS Behav. 2011;15(6):1259–63. doi:10.1007/s10461-010-9856-z.
Menza TW, Hughes JP, Celum CL, Golden MR. Prediction of HIV acquisition among men who have sex with men. Sex Transm Dis. 2009;36(9):547–55. doi:10.1097/OLQ.0b013e3181a9cc41.
Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Soc Sci Med. 1997;44(9):1303–12.
Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18(9):1712–21. doi:10.1007/s10461-014-0839-3.
Aitken C, Power R, Dwyer R. A very low response rate in an on-line survey of medical practitioners. Aust N Z J Public Health. 2008;32(3):288–9. doi:10.1111/j.1753-6405.2008.00232.x.
Grava-Gubins I, Scott S. Effects of various methodologic strategies: survey response rates among Canadian physicians and physicians-in-training. Can Fam Physician. 2008;54(10):1424–30.
Acknowledgments
The work was supported by award EI11-SD-005 from CHRP; by the UCSD Center for AIDS Research – Bioinformatics and Information Technology Core; and by NIAID grants AI064086 (K24 to RH), AI27670 (UCSD ACTU) AI36214 (UCSD CFAR), K23 MH098795 (to DK) and 5T32AI007036. Dr. Blumenthal is supported by Grant T32 AI007036. Dr. Krakower is supported by Grant K23 MH098795. Dr. Haubrich is supported by award from CHRP and NIAID Grants K24 AI064086, ACTU AI27670 and CFAR AI36214.
Conflict of interest
There are no relevant conflict of interests.
Disclosure
Jill Blumenthal has no financial disclosures. Sonia Jain has no financial disclosures. Douglas Krakower reports research support from Gilead Sciences and Bristol Myers Squibb. Xiaoying Sun has no financial disclosures. Jason Young has no financial disclosures. Kenneth Mayer reports research support from Gilead Sciences and Alere. Richard Haubrich reports having received honoraria or consultant fees from Bristol Myers Squibb, Gilead Sciences, Janssen and Merck and research support (to UCSD) from Abbott, GlaxoSmithKline, Pfizer and Merck.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Blumenthal, J., Jain, S., Krakower, D. et al. Knowledge is Power! Increased Provider Knowledge Scores Regarding Pre-exposure Prophylaxis (PrEP) are Associated with Higher Rates of PrEP Prescription and Future Intent to Prescribe PrEP. AIDS Behav 19, 802–810 (2015). https://doi.org/10.1007/s10461-015-0996-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-0996-z