Abstract
HIV pre-exposure prophylaxis (PrEP) was FDA approved in 2012, but uptake remains low. To characterize what would facilitate health care providers’ increased PrEP prescribing, we conducted a 10-city, online survey of 525 primary care providers (PCPs) and HIV providers (HIVPs) to assess awareness, knowledge, and experience with prescribing PrEP; and, comfort with and barriers to PrEP-related activities. Fewer PCPs than HIVPs had heard of PrEP (76 vs 98%), felt familiar with prescribing PrEP (28 vs. 76%), or had prescribed it (17 vs. 64%). PCPs were less comfortable than HIVPs with PrEP-related activities such as discussing sexual activities (75 vs. 94%), testing for acute HIV (83 vs. 98%), or delivering a new HIV diagnosis (80 vs. 95%). PCPs most frequently identified limited knowledge about PrEP and concerns about insurance coverage as prescribing barriers. PCPs and HIVPs differ in needs that will facilitate their PrEP prescribing. Efforts to increase PrEP uptake will require interventions to increase the knowledge, comfort, and skills of providers to prescribe PrEP.
Resumen
Profilaxis pre-exposición por VIH (PrEP) fue aprobado por la FDA en 2012, pero su utilización ha sido lento. Para caracterizar lo que facilataría un aumento de la prescripción de profilaxis pre-exposición entre los proveedores de salud, se realizó una encuesta en línea con 525 proveedores de atención primaria (PAP) y los proveedores de VIH (PVIH) en diez ciudades, para evaluar la conciencia, conocimiento y la experiencia con la prescripción de profilaxis pre-exposición; y comodidad con y barreras a las actividades relacionadas con la prescripción de PrEP. Menos PAPs que PVIHs habían oído hablar de profilaxis pre-exposición (76 vs 98%), se sentía familiarizado con prescripción de profilaxis pre-exposición (28 vs. 76%), o habían prescrito (17 vs. 64%). Los PAPs eran menos cómodo que PVIHs con actividades relacionadas con la PrEP como hablar sobre las actividades sexuales (75 vs. 94%), las pruebas de VIH aguda (83 vs. 98%), o la entrega de un nuevo diagnóstico de VIH (80 vs. 95%). Los PAPs frecuentemente identificaron un conocimiento limitado sobre PrEP y preocupaciones acerca de la cobertura de seguro como barreras de prescripción. PAPs y PVIHs difieren en las necesidades que van a facilitar su prescripción de PrEP. Los esfuerzos para aumentar la absorción de la PrEP requerirán intervenciones para aumentar el conocimiento, la comodidad, y las habilidades de los proveedores para prescribir PrEP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Approximately 48,000 individuals in the US acquire HIV each year. In 2012, the FDA approved the use of emtricitabine/tenofovir (Truvada) as pre-exposure prophylaxis (PrEP) for HIV-negative individuals. PrEP reduces the risk of contracting HIV by 44–88% in at-risk populations [1–5], with risk reductions of 92–100% among individuals most adherent to PrEP [6–8]. PrEP has the potential to make a significant impact on the HIV epidemic if it can be prescribed to enough at-risk individuals.
PrEP uptake is growing [9–11], but not enough to have a substantial impact on HIV incidence, even in high-uptake cities [12]. While nearly 500,000 men who have sex with men (MSM) and 1.2 million US adults overall could benefit from being on PrEP, [13] only about 80,000 people are thought to be taking PrEP [9]. Access to PrEP requires that health care providers are aware of PrEP, competent to discuss it, and able to either prescribe it or refer patients elsewhere to receive it. Krakower and colleagues identified the “purview paradox” as a factor that may contribute to suboptimal PrEP prescription [14]. They identify the problem that HIV providers (HIVPs)—who have the knowledge and skills necessary to prescribe PrEP—are relatively few in number and may see few HIV-negative individuals. In contrast, primary care providers (PCPs), much greater in number, may encounter high-risk HIV-uninfected patients, but may be unaware of PrEP or uncomfortable prescribing it.
Understanding current levels of knowledge and barriers to PrEP provision among these two provider groups is an important step in expanding PrEP uptake, as knowledge of PrEP has been correlated with future willingness to prescribe it [15]. Research in this area has mainly evaluated attitudes, perceived barriers, and experience with PrEP among HIV or sexual health providers [14, 16–23], although some studies have included non-HIV providers [15, 24–28]. One study of both HIV specialists and generalists in Massachusetts showed higher PrEP awareness among HIV specialists, but low prevalence of PrEP prescription in both groups [26]. A 2013 study showed that while 74% of infectious disease specialists supported the use of PrEP, only 9% had prescribed it [21]. A 2014 study showed that up to 79% of HIV providers were willing to prescribe PrEP to a patient with an HIV-positive partner in the next year, although experience prescribing PrEP was not measured [19, 23]. One survey of PCPs—conducted serially between 2009 and 2013—found increasing PrEP awareness over time, but minimal PrEP prescription, 4% in 2013 [29]. Another survey showed an increase in awareness of PrEP between 2009 (24%) and 2015 (66%), though willingness to prescribe PrEP to patients in 5 of the 6 potential risk groups did not increase over time [11].
Studies have also identified providers’ concerns about PrEP, including efficacy and safety, medication adherence, behavioral disinhibition, and inducing drug-resistant HIV strains [14, 16–18, 20, 21, 26, 28, 30]. Providers’ concerns about their capacity to screen, counsel, and follow patients taking PrEP have also been documented [20, 26, 27]. Notably, the majority of these studies were conducted prior to issuance of CDC’s PrEP guidelines in 2014 [31].
The present study expanded previous work by examining PrEP awareness, familiarity with prescribing PrEP, comfort with PrEP-related clinical activities, experience with PrEP implementation, and barriers to prescribing PrEP in a 10-city sample of US health care providers following the 2014 publication of the CDC PrEP guidelines. In addition, we aimed to identify strategies to increase PrEP provision by evaluating and comparing the responses of primary care providers and HIV providers.
Methods
Participants
We conducted a cross-sectional, online survey of PCPs and HIVPs, including physicians, nurse practitioners, and physician assistants, between July 2014 and May 2015. Potential participants were recruited using national databases from three professional organizations: the American Medical Association, the American Association of Nurse Practitioners, and the American Academy of HIV Medicine. We recruited providers who practiced in the 10 US cities with the greatest HIV prevalence (see Table 3), and further restricted recruitment to ZIP codes where HIV prevalence was at least 0.5%—greater than the US prevalence of 0.3% [32]. An estimated 2088 potential participants were sent an invitation by postal mail or email, depending upon which method of contact was available from each database. All providers completed the survey online, regardless of the method by which they were recruited to participate. Unique login and password combinations allowed entry into the survey. Eligibility criteria included: (1) working at least 4 hours per week in an ambulatory setting; (2) having patients ages 13–64 years in their practice; and (3) describing their practice as Family Medicine, Internal Medicine (IM), IM/Pediatrics, Obstetrics/Gynecology, Infectious Diseases, or HIV Medicine. The final option was included to accommodate non-physician providers who may classify their practice most closely with this option. Participants completing the survey were offered a $100 honorarium.
Measures
The 177-item measure began with questions assessing respondent demographic characteristics, professional background, and practice characteristics, including number of HIV-infected and HIV-negative patients. Eight items measured respondent comfort performing clinical activities that are important precursors to providing PrEP [discussing sexual orientation, discussing sexual activities, screening for sexually transmitted infections (STIs) and HIV, assessing HIV risk, providing risk reduction counseling, diagnosing acute HIV, and giving a patient a new HIV diagnosis]. 5-point Likert scales (1 = completely uncomfortable; 3 = neither comfortable nor uncomfortable; 5 = completely comfortable) measured respondents’ level of comfort performing each activity. The two most positive ratings (somewhat and completely comfortable) were used to designate participant comfort in performing the activity. Other items assessed awareness of PrEP, as well as self-reported degree of familiarity with prescribing PrEP, the latter measured on a 5-point scale ranging from 1 = very unfamiliar to 5 = very familiar. In addition, the measure assessed experience with PrEP, including number of PrEP discussions with patients in the past year (patient-initiated and provider-initiated), the year of first discussion, whether or not respondents had ever prescribed PrEP, and number of patients to whom the respondent prescribed PrEP in the past year.
Respondents were presented with a list of 12 potential barriers to prescribing PrEP and used 5-point Likert scales to indicate how much of a concern each is to their prescribing PrEP (1 = not at all a concern; 5 = a major concern). The barriers, shown in Table 4, included domains reflecting administrative and insurance issues, time and clinic capacity issues, policy matters, and provider knowledge and comfort. Respondents who chose a 4 (somewhat of a concern) or 5 (a major concern) on an item were classified as endorsing that item as a barrier to PrEP provision. Participants also responded to 5 items assessing negative attitudes toward PrEP; these were considered additional possible barriers to prescription. These attitudes included views that taking PrEP results in risk compensation and that PrEP users are not likely to adhere; participants indicated their agreement on a scale of 1 (completely disagree) to 5 (completely agree). Respondents who chose a 4 or a 5 on an item were classified as endorsing the negative attitude. Finally, the measure requested that participants who never prescribed PrEP use a 5-point Likert scale to indicate their personal willingness to prescribe PrEP if they gained the required training, knowledge, and skills to do so. The items included in the barriers and attitudes sections of the survey were based on prior findings [14, 16–18, 25, 28] as well as theoretical constructs.
Statistical Analysis
We first classified participants as either HIVPs or PCPs based on their response to one item which asked whether or not they provide HIV-related care to HIV-positive patients, regardless of their profession or specialty training. The statistical analyses described sample demographics and used t-tests and χ2 tests to compare HIVPs and PCPs. Logistic regression (for binary outcomes), ordinal regression (for ordered categorical outcomes), and ANCOVA (for continuous outcomes) were used to examine the association between provider type and PrEP comfort, awareness, familiarity, discussion, prescription, barriers, and willingness, controlling for demographic and practice features that differed between provider types. We also used χ2 tests to explore differences in PrEP awareness, familiarity with prescribing PrEP, and PrEP prescription based on respondent city of residence.
Among eligible participants taking the survey, rates of missing data were modest; 84% of participants had complete data. Overall, 4% of data was missing; demographic and practice-related variables were missing for 9% of participants (likely due to their location at the end of the survey), barriers were missing for 7% of participants, and all other PrEP outcomes were missing for 3% or less of participants. Missing data was more common for HIVPs as compared to PCPs (22 vs. 11%, p < .01) and for non-physicians as compared to physicians (26 vs. 15%, p < .05); those with missing data were also slightly younger than those with no missing data (48 vs. 50 years, p = .05). There were no differences in PrEP awareness, familiarity prescribing PrEP, or in any other demographic or practice-related variables for those with and without missing data. Eligible participants were included in all analyses for which they provided data regardless of whether they completed the survey.
Results
Demographic Characteristics of Study Participants
Of the 627 individuals who entered the study website, 525 met study eligibility criteria, provided informed consent, and took the survey. Demographic and practice-related characteristics of participants are shown in Table 1. Between 8 and 12% of participants were from each city. On average, participants were 50 years old and had been licensed for 19 years. Most participants (85%) were physicians; 9% were nurse practitioners (NPs) and 6% were physician assistants (PAs). Providers specialized in Internal Medicine (50%), Family Medicine (30%), HIV Medicine (15%), and Infectious Diseases (5%).
HIVPs and PCPs were similar in terms of sex, age, and years of experience. A higher proportion of HIVPs than PCPs were non-physician (NP or PA) practitioners (25 vs. 6%). As expected, HIVPs reported a greater number of HIV-positive patients in their practices than did PCPs (176.1 vs. 14.6). We controlled for geographic region and professional training in all analyses involving provider type.
PrEP Comfort, Awareness, Familiarity, Discussion, and Prescription Practices
Table 2 shows the responses of providers to survey questions measuring their comfort conducting clinical activities that are precursors to prescribing PrEP, their awareness of PrEP and familiarity with prescribing PrEP, discussions with patients about PrEP in the past year, and experience in prescribing PrEP. The table shows responses of the full sample and responses separated by whether respondents were HIVPs or PCPs.
Most survey respondents in both provider groups indicated that they were somewhat to completely comfortable engaging in the clinical activities needed to assess the appropriateness of PrEP for patients and performing other PrEP-precursor activities. Over 90% of HIVPs and at least 80% of PCPs said that they were somewhat to completely comfortable discussing patient sexual orientation, screening patients for STIs or HIV, screening for HIV sexual risk behavior, providing risk-reduction counseling, diagnosing acute HIV infection, and delivering a new HIV diagnosis. However, significantly fewer primary care than HIV providers reported comfort discussing patients’ sexual activities (75% of PCPs vs. 95% of HIVPs), and PCPs were less likely than HIVPs to be comfortable delivering risk-reduction counseling, testing for acute HIV infection, and delivering a new HIV diagnosis. Eighty-nine percent of HIVPs were somewhat or fully comfortable with all eight PrEP precursor activities, compared to 59% of PCPs.
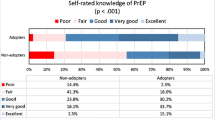
Regarding PrEP awareness, only 76% of PCPs reported that they had heard of PrEP, fewer than the 98% of HIVPs who reported PrEP awareness. As Table 2 also shows, only 28% of PCPs reported that they were somewhat or very familiar with prescribing PrEP, lower than the 76% of HIVPs who reported this level of familiarity with prescribing it.
Primary care providers in the sample had limited experience discussing PrEP with patients, and the large majority said they had never prescribed PrEP. Eighty-seven percent of HIVPs reported a history of discussing PrEP with patients, compared to only one-third of PCPs. PCPs also reported significantly fewer PrEP discussions in the past year than HIVPs (5.8 vs. 23.5). Sixty percent of PCPs’ PrEP-related discussions in the past 12 months were initiated by patients. By contrast, nearly 60% of HIVPs’ PrEP discussions were initiated by the provider. Finally, 39% of providers in the overall sample said they prescribed PrEP in the past year; almost two-thirds of HIVPs reported ever prescribing PrEP compared to only 17% of PCPs. HIVPs had also prescribed PrEP significantly more times in the past year than PCPs (18.6 vs. 3.3 times).
Geographic Variation in Providers’ PrEP-related Practice Characteristics
Table 3 shows sample responses by geographical area. Although all respondents practiced in one of the ten US cities with the greatest number of HIV cases, significant differences were observed in providers’ PrEP-related practice characteristics.
Familiarity with prescribing PrEP was lowest among HIVPs in Houston, Atlanta, and Miami and among PCPs in Dallas, Atlanta, and Miami. Having PrEP discussions with patients was least common among PCPs in Dallas, Miami, and Philadelphia. Fewer than 20% of PCPs in these cities reported ever talking about PrEP with their patients. With respect to PrEP prescribing, HIVPs in Atlanta, Miami, Philadelphia, and Chicago were less likely than HIVPs in other cities to have prescribed PrEP. There were no significant geographic differences in prescribing PrEP among PCPs; with the exception of PCPs in New York, San Francisco, and Los Angeles, no more than one in five PCPs had ever prescribed PrEP.
The PrEP Provider Experience “Cascade”
Figure 1 displays study findings in the form of a PrEP experience cascade by provider type. As depicted in the upper panel of Fig. 1, the large majority of HIVPs had heard of PrEP and had discussed it with patients. Most had prescribed PrEP. By contrast, the lower panel of Fig. 1, showing data for PCPs, shows a much larger drop-off at each step of the cascade, with fewer than one-third having discussed it recently with any patients, and only 17% ever prescribing PrEP.
Barriers to Prescribing PrEP
Table 4 shows responses to questions about perceived barriers to prescribing PrEP by provider group and by respondents in each group who had or had not prescribed PrEP. The most frequently-cited barriers to PrEP prescription related to administrative processes including completing prior authorizations and concerns about insurance coverage of PrEP. These barriers were cited by the majority of providers, both HIVPs and PCPs. More than one-third of PCPs, and especially those who never prescribed PrEP, cited as barriers their own limited knowledge of PrEP, the time needed to provide risk-reduction counseling, staff and clinical capacity, and the need for follow-up visits for PrEP monitoring. In almost all cases, these barriers were more frequently cited by PCPs than by HIVPs, and were always cited more often by PCPs who had never prescribed PrEP than by those with prescribing experience. Concerns about whether prescribing PrEP is ethical was the barrier least often reported by any type of provider.
Negative attitudes toward PrEP by provider group and by respondents in each group who had or had not prescribed PrEP are also included in Table 4. None of the negative attitudes were endorsed by the majority of either HIVPs or PCPs. The most frequently-endorsed negative attitude was the idea that people should use condoms instead of PrEP. About one-third of the overall sample endorsed that idea. About one-fifth of the sample expressed concern about risk compensation among PrEP users, development of HIV resistance, and potential lack of adherence to PrEP. Although PCPs were more likely than HIVPs to hold at least one negative attitude toward PrEP, there were no differences in the frequency of endorsing specific negative attitudes by provider type. Several negative attitudes were more likely to be held by PrEP non-prescribers than by PrEP prescribers; these included views that people should use condoms instead of PrEP and that the use of PrEP could increase resistance (among HIVPs only) as well as views that PrEP users are not likely to adhere to their medication regimen (for both provider types). Only 16% of participants expressed concern over the cost of PrEP.
Willingness of Providers to Engage in PrEP-prescribing Activities
Table 5 shows responses of PrEP non-prescribers about their willingness—after gaining appropriate knowledge and skills—to initiate PrEP discussions, prescribe PrEP, refer PrEP candidates to other providers, and accept patients referred to them for PrEP. Ninety-one percent of HIVPs said that with training they would initiate discussions with patients about PrEP, 85% would prescribe PrEP, 76% would accept patents referred for PrEP, and 70% would refer candidates to other providers for PrEP. Nearly 90% of PCPs said that—with appropriate knowledge and skills—they would initiate conversations about PrEP, 96% would refer PrEP candidates to other providers, and over three-fourths would themselves prescribe PrEP.
Discussion
This study represents the largest survey to date to measure PrEP awareness, knowledge, experience, and barriers to PrEP provision among both HIV providers and primary care providers, and is the first, to our knowledge, conducted after release of the CDC’s PrEP guidelines. These findings are important to consider as work continues to increase the availability of PrEP for individuals at risk for HIV acquisition.
We found near universal awareness of PrEP among HIVPs, similar to earlier studies [16, 25]. However, the majority of the HIVPs in our study—64%—had prescribed PrEP, much higher than the rates found previously, even in studies conducted as recently as early 2014 [15, 21]. Of interest was the relatively wide variation between cities in the proportion of HIVPs who had prescribed PrEP, varying from 44 to 88%, even in the 10 US cities with the most HIV cases that were included in this study. Additional efforts may be needed to train or encourage more HIV providers in some of these cities (and others beyond those in our study) to prescribe PrEP. Also of interest is that the steepest decline on our “PrEP provider experience cascade” for HIVPs was between the steps of discussing PrEP and prescribing it. Further research to better understand the reasons for this finding are warranted.
There were significant differences between PCPs and HIVPs at every point in the PrEP provider experience cascade. Differences in PrEP awareness and prescribing are consistent with previous research [14, 25, 26]. However, we also found important differences between PCPs and HIVPs with regard to comfort conducting PrEP-related clinical activities—most notably, discussing sexual behaviors, diagnosing acute HIV infection, and delivering a new HIV diagnosis, which may underlie the differences seen in the provider experience cascade. Of interest, we asked participants to rate their comfort level with these activities prior to any mention of PrEP. When asked later in the survey about how different barriers may affect their ability to prescribe PrEP, fewer PCPs identified their own comfort level discussing sexual matters with patients as a barrier. This may suggest that some respondents underestimate the importance of understanding patients’ sex practices in the process of prescribing PrEP. These results demonstrate the need for PrEP educational programs that include skill-building around sexual history-taking in addition to knowledge-based PrEP content.
The majority of both HIVPs and PCPs identified insurance-related issues as barriers to prescribing PrEP, similar to findings from other research [21, 28]. Among HIVPs, there was a similar level of concern about insurance-related issues by those who had prescribed and those who had not prescribed PrEP. Thus, even experience with prescribing PrEP, and presumably with navigating insurance systems, does not lessen the perceived burden of insurance systems in the PrEP prescribing process among HIVPs. It is possible that HIVPs—presumably familiar with insurance-related issues involved with prescribing antiretroviral medications—see insurance issues as a barrier and burden, but not necessarily a deterrent to prescribing PrEP. Interestingly, among PCPs, insurance-related barriers were less commonly identified by PrEP prescribers than by non-prescribers. This suggests that some insurance-related barriers may be overestimated among non-prescribers and that experience in prescribing PrEP may decrease the perceived difficulty of dealing with insurance-related issues. In either case, provider interventions to increase PrEP prescribing competency should include information on navigating insurance systems, including identifying and training administrative staff who could assume some of these responsibilities, lessening the burden on providers. Additionally, advocacy may be needed to lessen the administrative burdens of getting antiretroviral drugs covered by patients’ insurance plans.
For nearly all of the other potential barriers—among both HIVPs and PCPs—there was a significant difference between PrEP prescribers and PrEP non-prescribers in the proportion of providers endorsing each barrier as a concern. This also suggests that the anticipated burden of barriers to prescribing PrEP is greater than what providers experience once they actually prescribe it. Thus, interventions promoting PrEP among providers may be more successful by addressing each barrier specifically and perhaps by presenting data from this and other studies [33] suggesting that the burden of these barriers is lower among providers who actually prescribe PrEP. The most prevalent concern or negative attitude toward PrEP was the thought that patients should use condoms instead of PrEP, an idea endorsed by about one-third of the sample. This could be addressed by including data on the efficacy of condoms in preventing HIV—significantly lower than that of PrEP for those most adherent to it [34]—in PrEP educational interventions. Similarly, concerns over risk compensation and promotion of HIV resistance—also identified in previous research [16, 21, 28]—could be allayed by presenting data from PrEP trials showing little evidence to support these concerns [35].
Our set of items regarding respondents’ willingness to provide PrEP—if they gained the appropriate knowledge and skills to prescribe it—were asked of PrEP non-prescribers and could be useful in considering how to increase PrEP rollout. Nearly all respondents were willing to at least initiate discussions about PrEP, and more than three quarters said they would prescribe it. Nearly all PCPs were willing to refer patients to other providers for PrEP, while half of PCPs and three quarters of HIVPs said they would accept patients referred to them for PrEP. This high degree of willingness to participate in at least the initial steps of PrEP provision suggests that knowledge and skills training for PrEP non-prescribers may be of great value in increasing PrEP availability. Our data suggest that Krakower and colleagues’ “purview paradox” need not be intractable if providers can be educated about PrEP. In our study, a similar proportion of HIVPs and PCPs expressed willingness to prescribe PrEP if they obtained the necessary knowledge and skills.
Our results have several potential limitations. First, our response rate was approximately 30%. While higher than that found in many studies of this topic, this response rate introduces the potential of non-response bias. Our method of recruitment using databases of providers makes it impossible to compare responders and non-responders. However, it is unlikely that non-responders to a survey on the topic of HIV prevention would be more experienced with PrEP than responders. Thus, it seems likely that our results represent the best case scenario with regard to the PrEP experience cascade. Differences in PrEP experience between HIVPs and PCPs could be influenced by the patient populations they see and should be interpreted with this caveat. For example HIVPs may be sought out more frequently by patients seeking PrEP, thus increasing their level of experience discussing and prescribing PrEP. Another potential limitation is that some constructs, such as familiarity with prescribing PrEP, were assessed with single-item measures. Finally, our study had low representation of non-physician PCPs, a group which may be important in expanding PrEP uptake.
Taken in sum, our findings suggest that most HIVPs are currently prescribing PrEP and have the capacity to provide PrEP to additional patients, and that most PCPs are willing to prescribe PrEP with appropriate training. Thus, PrEP uptake could be immediately increased by connecting potential PrEP users with all current PrEP providers—both HIVPs and PCPs—through pairing PrEP promotion activities for at-risk groups with the dissemination of easily-accessible PrEP provider directories. At the same time, our data suggest great potential for increasing the number of PrEP providers. Nearly all PCPs were willing to participate in at least some aspects of PrEP provision (e.g., discussing PrEP with patients and referring eligible patients to PrEP providers) and more than 75% of PCPs were willing to prescribe PrEP themselves if properly trained. Therefore, the development and implementation of effective educational interventions to help providers develop the knowledge and skills to screen patients for HIV risk, and recommend and prescribe PrEP are essential and urgent if PrEP’s potential effect on the HIV epidemic is to be realized. Attention to some of the differences between HIVPs and PCPs with regard to the PrEP provider experience cascade may help tailor such interventions more appropriately. That the steepest drop-off in the HIVP provider experience cascade occurred between discussing and prescribing PrEP may indicate that HIVP-directed education could focus on the practical aspects of PrEP (e.g., insurance coverage and prior authorization completion). Our findings of high levels of familiarity with prescribing PrEP and comfort with PrEP precursor activities (e.g., discussing sexual activities and risk for HIV) also suggests these topics may not be needed in HIVP-directed education. Meanwhile, the PrEP provider experience cascade for PCPs showed relatively large drop-offs between the earlier steps in the cascade. Our findings of lower levels of familiarity with prescribing PrEP and comfort with PrEP precursor activities among PCPs suggest that PCP-directed education should be more expansive and include all aspects of knowledge and skills needed to prescribe PrEP. Rapid development, testing, and implementation of appropriate provider-directed PrEP educational interventions could significantly increase PrEP availability and thereby avert incident HIV infections.
References
Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34.
Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Molina J, Capitant C, Spire B, Pialoux G, Chidiac C, Charreau I, et al. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay trial. Conference on Retroviruses and Opportunistic Infections. Seattle, 2015 [Abstract 23LB].
McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2015;387(10013):53–60.
Donnell D, Baeten JM, Bumpus NN, Brantley J, Bangsberg DR, Haberer JE, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J Acquir Immune Defic Syndr. 2014;66(3):340–8.
Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9.
Anderson PL, Glidden DV, Liu A, Buchbinder S, Lama JR, Guanira JV, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125.
Mera R, McCallister S, Palmer B, et al. Truvada for HIV pre-exposure prophylaxis (PrEP) utilization in the United States (2013–2015). 21st International AIDS Conference. Durban, 2016 [Abstract TUAX0105LB].
Laufer F, O’Connell DA, Feldman I. Increased Medicaid Prescriptions for Preexposure Prophylaxis Against HIV infection—New York, 2012–2015. MMWR Morb Mortal Wkly Rep. 2015;64(Early Release):1–6.
Smith DK, Mendoza MCB, Stryker JE, Rose CE. PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009–2015. PLoS ONE. 2016;11(6):e0156592.
Grant R, Hecht J, Raymond H. Scale-up of pre-exposure prophylaxis in San Francisco to impact HIV incidence. Conference on Retroviruses and Opportunistic Infections. Seattle, 2015 [Abstract 25].
Smith DK, Van Handel M, Wolitski RJ, Stryker JE, Hall HI, Prejean J. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64:1291–5.
Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers’ perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014;18(9):1712–21.
Blumenthal J, Jain S, Krakower D, Sun X, Young J, Mayer K, et al. Knowledge is power! increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19(5):802–10.
Tellalian D, Maznavi K, Bredeek UF, Hardy WD. Pre-exposure prophylaxis (PrEP) for HIV infection: results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDS. 2013;27(10):553–9.
Tripathi A, Whiteside YO, Duffus WA. Perceptions and attitudes about preexposure prophylaxis among seronegative partners and the potential of sexual disinhibition. South Med J. 2013;106(10):558–64.
Desai M, Gafos M, Dolling D, McCormack S, Nardone A. Healthcare providers’ knowledge of, attitudes to and practice of pre-exposure prophylaxis for HIV infection. HIV Med. 2015;15:28.
Adams LM, Balderson B, Packett BJ, Brown K, Catz SL. Providers’ perspectives on prescribing pre-exposure prophlaxis (PrEP) for HIV prevention. HIV Specialist. 2015;7(1):18–25.
Arnold EA, Hazelton P, Lane T, Christopoulos KA, Galindo GR, Steward WT, et al. A qualitative study of provider thoughts on implementing pre-exposure prophylaxis (PrEP) in clinical settings to prevent HIV infection. PLoS ONE. 2012;7(7):e40603.
Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58(5):704–12.
Seidman D, Carlson K, Weber S, Witt J, Kelly PJ. United States family planning providers’ knowledge of and attitudes towards preexposure prophylaxis for HIV prevention: a national survey. Contracept. 2016;93(5):463–9.
Adams LM, Balderson BH. HIV providers’ likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: a short report. AIDS Care. 2016; doi:10.1080/09540121.2016.1153595.
Sachdev DD, Stojanovski K, Liu AY, Buchbinder SP, Macalino GE. Intentions to prescribe preexposure prophylaxis are associated with self-efficacy and normative beliefs. Clin Infect Dis. 2014;58(12):1786–7.
Mimiaga MJ, White JM, Krakower DS, Biello KB, Mayer KH. Suboptimal awareness and comprehension of published preexposure prophylaxis efficacy results among physicians in Massachusetts. AIDS Care. 2014;26(6):684–93.
White JM, Mimiaga MJ, Krakower DS, Mayer KH. Evolution of Massachusetts physician attitudes, knowledge, and experience regarding the use of antiretrovirals for HIV prevention. AIDS Patient Care STDS. 2012;26(7):395–405.
Sharma M, Wilton J, Senn H, Fowler S, Tan DH. Preparing for PrEP: perceptions and readiness of canadian physicians for the implementation of HIV pre-exposure prophylaxis. PLoS ONE. 2014;9(8):e105283.
Krakower DS, Oldenburg CE, Mitty JA, Wilson IB, Kurth AE, Maloney KM, et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: results from a survey of healthcare providers in New England. PLoS ONE. 2015;10(7):e0132398.
Smith, D, Mendoza, M, Rose, C. PrEP Awareness and attitudes in a nationally representative survey of primary care clinicians in the United States, 2009–2013. US National HIV Prevention Conference. 2015, Atlanta [Abstract 1686].
Desai M, Gafos M, Dolling D, McCormack S, Nardone A. PROUD study. Healthcare providers’ knowledge of, attitudes to and practice of pre-exposure prophylaxis for HIV infection. HIV Med. 2016;17(2):133–42.
Centers for Disease Control and Prevention (CDC). Preexposure prophylaxis for the prevention of HIV infection in the United States–2014: A clinical practice guideline. Atlanta: CDC; 2014.
Centers for Disease Control and Prevention (CDC). HIV Surveillance report, 2014. November, 2015. Report No.: 26.
Calabrese SK, Magnus M, Mayer KH, et al. Putting PrEP into practice: lessons learned from early-adopting US providers’ firsthand experiences providing HIV pre-exposure prophylaxis and associated care. PLoS ONE. 2016;11(6):e0157324.
Smith DK, Herbst JH, Zhang X, Rose CE. Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2015;68:337–44.
Fonner VA, Dalglish SL, Kennedy CE, et al. Effecitveness and safety of oral HIV pre-exposure prophylaxis for all populations. AIDS. 2016;30:1973–83.
Funding
This work was supported by Gilead Sciences, Inc. and the National Institute of Mental Health at the National Institutes of Health [Grant Numbers 5P30MH052776, K01-MH099956].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A.P. receives research support from Gilead Sciences, Inc. J.W., J.O., T.M., L.B., and J.K. report no conflict of interest.
Research Involving Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
This study was reviewed by the Institutional Review Board of the Medical College of Wisconsin. It met the Board’s definition of “minimal risk” and a waiver of informed consent was granted.
Rights and permissions
About this article
Cite this article
Petroll, A.E., Walsh, J.L., Owczarzak, J.L. et al. PrEP Awareness, Familiarity, Comfort, and Prescribing Experience among US Primary Care Providers and HIV Specialists. AIDS Behav 21, 1256–1267 (2017). https://doi.org/10.1007/s10461-016-1625-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1625-1