Abstract
A peer leader-based intervention using social media can be an effective means to encourage Peruvian gay men to test for HIV. The objective was to explore the feasibility of recruiting and training leaders to deliver a peer intervention via Facebook to promote HIV testing. Training consisted of three sessions focused on HIV epidemiology, consequences of stigma associated with HIV, and ways to use Facebook. We performed pre- and post-training evaluations to assess HIV knowledge and comfort using Facebook. We trained 34 peer leaders. At baseline, the majority of peer leaders were already qualified and knowledgeable about HIV prevention and use of social media. We found a significant increase in proportion of peer leaders who were comfortable using social media to discuss about sexual partners and about STIs. It is feasible to recruit peer leaders who are qualified to conduct a social media based HIV prevention intervention in Peru.
Resumen
Una intervención de líderes pares en una red social puede ser un medio efectivo para promover la prueba del VIH en hombres gays Peruanos. El objetivo fue explorar la factibilidad de reclutar y entrenar a líderes para ejecutar una intervención en Facebook para promover la prueba del VIH. El entrenamiento consistió en tres sesiones: Epidemiología del VIH, consecuencias del estigma asociado al VIH, y uso de Facebook para comunicarse. Entrenamos a 34 participantes. Antes del entrenamiento, la mayoría de líderes ya conocía acerca de prevención del VIH y estaba calificado para el uso de redes sociales. Encontramos un incremento significativo en la comodidad para usar Facebook para discutir acerca de parejas sexuales y de infecciones de transmisión sexual. Es factible reclutar pares calificados para conducir una intervención en Facebook para prevenir el VIH en gays Peruanos.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peer-leader based interventions are effective in improving health behaviors among MSM [1–5]. For example, in a study among young MSM in the U.S., an intervention that included a peer outreach worker, was effective in engaging and retaining participants in HIV care services (odds ratio for attending a clinic = 2.5) [6, 7]. Also, a peer leader–based HIV/STI intervention reported lower levels of stigma at 12- and 24-month follow-up in participants in the intervention group in Peru [4]. Leaders are persons who are similar to the target population in terms of age, education, sexual orientation and other characteristics [8]. They are trained on a health topic and then go into the community to communicate information in a culturally and socially appropriate manner [9], with the intent to educate and change social norms and behaviors [4, 8, 10]. These interventions have been associated with increased knowledge of HIV, condom use and decreased unprotected anal intercourse in both developing and developed countries [1–5].
In Peru the HIV epidemic is concentrated among men who have sex with men (MSM), characterized by a HIV prevalence of 12.4 % [11] in MSM compared to 0.5 % in the general population [12]. A cornerstone of the Peruvian National HIV and sexually transmitted infection (STI) prevention strategy is the engagement of peer educators [11]. Trained peers are sent to venues where MSM socialize (e.g. bars, clubs, parks, saunas) to deliver condoms, encourage safer-sex behaviors and make referrals to health centers for HIV and syphilis testing. While this approach as had some success [4], a major drawback is that only MSM who frequent such venues will be intercepted thereby missing MSM that do not frequent such spaces [11]. Consequently, alternative approaches are needed to successfully reach these men.
Delivering internet-based HIV prevention interventions to gay men seems to be feasible in Peru [13–15]. MSM use the Internet to find sexual partners, but also to seek HIV/STI information and services [14, 16]. Indeed, in a recent study that measured the preferences of MSM with regard to HIV programming delivered over the Internet, 70 % reported having had sex with an Internet partner during the previous year. Additionally, 94, 87 and 83 % reported being interested in receiving HIV prevention messages through web pages, chat rooms and emails, respectively [14]. This is enhanced by Internet cafes that are cheap and widely available [16, 17]. Peru is in the top 50 countries with regard to the number of Facebook users (9.58 million as of October 29, 2012) [18], one of the most used social networking websites worldwide. These features make social media a promising platform for recruiting peer leaders to deliver an online HIV/STI prevention intervention to Peruvian MSM who are not reached by traditional, venue-based peer educators.
Social sites have been shown to be feasible and acceptable platforms for delivering peer-leader HIV/STI interventions in the United States. For instance, the HOPE UCLA study was conducted in Los Angeles and was the first NIH-funded study to scale a community-based HIV testing intervention using an online social network [19–21]. The HOPE study recruited and trained peer leaders to use Facebook technologies to promote HIV testing among Los Angeles-based African American and Latino MSM. Leaders posted HIV-related content within secret groups of participants, which are Facebook groups that can only be seen by participants added by the group administrator. After 3 months of membership in the HIV group, participants who posted HIV prevention-related material on the wall of the secret group were significantly more likely to request an HIV testing kit (odds ratio: 11.14; p = 0.001) [21] compared to those who did not. In addition, those in the intervention condition were more likely to request an HIV test compared to those in the control group (44 vs. 20 %) [22].
Nevertheless, it is unknown whether it would be feasible to recruit peer leaders for a similar intervention in Peru. The aim of this study is to explore the feasibility of recruiting local peer educators who are both knowledgeable about HIV prevention and experienced using social media, to participate in a peer health intervention to promote HIV testing among MSM in Peru.
Methods
Human Subjects Considerations
The institutional review boards at Impacta, in Lima, Peru, and University of California approved the study.
Peer Leader Identification
We recruited participants who: (1) were male, (2) reported sex with a man in the past 12 months, (3) were 18 years of age or older, (4) lived in the Lima Metropolitan area, (5) were interested in educating others about HIV and STIs through online social networks, and (6) were experienced using Facebook. The peer leaders were recruited at a gay-serving community based organization (Epicentro) and were from referrals from Epicentro staff. They were chosen based on an existing network of MSM at Epicentro participating either as volunteers or regular center users. The study coordinator interviewed all candidates for peer leadership roles in-person before enrolling and training them. To motivate the potential leaders, he introduced the project to them by explaining that they would be using Facebook as frequently as they had done previously, but would additionally share information within a secret group and among their peers. Also, study staff explained to them that with the exception of the training sessions, the entire intervention was to be implemented on Facebook. Finally, study staff demonstrated that the minimum interaction on Facebook in order to earn a weekly incentive (13 USD) was easily reachable if they used Facebook at least twice a week. Each of the secret groups had 5–6 peer leaders and 28–32 participants. The intervention lasted 12 weeks and in order to be compensated weekly, each peer leader was required to share at least two posts on the wall of the secret group and send one private message to each of his assigned participants. Throughout the intervention the study coordinator provided continuous feedback to all leaders regarding the shared topics and any problems that arose among the participants. In this way, the coordinator of the study was integrated into all of the secret groups.
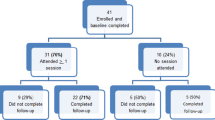
Enrollment
A total of 49 subjects were invited to participate in the training to become leaders. Of these, 34 were chosen to be part of the intervention because they completed all the training sessions. We aimed to train 34 leaders because the intervention arm aimed to enroll 230 participants, and previous research suggested that, in order to influence community norms, about 15 % of population need to be peer leaders (34/230 = 0.15) [8]. We oversampled slightly to account for participant attrition.
Training Sessions
Based on the HOPE study [20] which adapted the community popular opinion leader model for use on social networking sites [8], we performed 3 training sessions delivered over a 4-week period to train peer leaders as social media peer health educators. Each session lasted 3 h and was conducted at Epicentro. Leaders were to promote HIV testing and safe sex behaviors by using simple and friendly language and to promote Epicentro as a place where the participants could get an HIV test without being stigmatized. Therefore, the first training session covered essentials of HIV: the epidemiology of HIV in Peru; ways of transmission; types and importance of HIV testing; methods of prevention; and basic information about treatment (e.g. where to access free treatment in Peru). The second session covered the consequences of stigma and discrimination associated with low access to HIV testing services; and methods to communicate sensitive topics using simple and non-stigmatizing language. The third session focused on ways to use Facebook for communication, study logistics (such as HIV testing at Epicentro), and role-play exercises to integrate knowledge of HIV and the use of Facebook to make sure they were qualified to receive training. The requirements to be ready to be a peer leader were double-checked before training by exploring their regular posts on Facebook, during training sessions by performing role-playing, and at the completion of training, by receiving approval from the peer leader trainer. Finally, we gave leaders a peer leader training handbook with all the topics and logistical information about the study, including tips and specific examples to address the main objectives of the study. Training materials were adapted from Young et al. [21]. We worked with a local epidemiologist and a psychologist, who were both experienced in working with Peruvian MSM and sexual health, and the principal investigator of the HOPE study, in order to adapt these materials to the study population.
Pre and Post Training Evaluation
Based on the HOPE study [19], we performed a pre-training evaluation in order to assess whether leaders were qualified and ready to use Facebook to communicate HIV topics. Similar to the HOPE study in the U.S., the questionnaire included: general knowledge about HIV (measured with a series of 45 true/false questions; Table 1); experience using Facebook technologies (through yes/no questions on whether they had ever chatted, or sent messages or wall posts); and comfort using these technologies for health outreach and talking to another person about sexual risk behaviors. We measured comfort questions with 5-point Likert scales (1 = very uncomfortable, 5 = very comfortable) assessing their comfort (such as how comfortable they would be to use Facebook technologies to talk to another person about sexual risk behaviors). In order to receive certification that they were qualified to conduct the intervention, leaders needed to have a passing score above 70 % on the HIV knowledge questions, report being comfortable or very comfortable using social media for health communication outreach, and receive the peer trainer’s approval that they were prepared for social media health outreach. Similarly, we evaluated peer leaders with a post-training questionnaire to ensure that participants who were not already qualified would receive the skills and/or comfort needed prior to training.
Data Management and Analysis
Test score means and standard deviations for HIV knowledge were calculated out of a possible 100 points for each exam (using a rule of three, those who had the 45 answers correct received 100 points). We used paired t test to assess differences in mean scores for each exam before and after training and to detect differences based on peer leader training assignments. Peer leader comfort using social media was dichotomized combining responses of “very comfortable” and “comfortable” as comfortable and “very uncomfortable,” “uncomfortable” and “average” as not comfortable. Proportion of peer leaders indicating comfort on each topic was compared pre- and post training using the McNemar’s test.
Results
Demographics
We trained 34 peer leaders. The mean age was 30.4 years (19–45). All men self-reported as being homosexual and living in Metropolitan Lima. Fifty percent self-reported being professionals or students working in the communication field; 32 % were health care workers or students; and 18 % from other fields. All participants had a Facebook account at recruitment.
HIV Knowledge Score
The overall test scores were above a passing level both before and after training. Although the mean score after training was higher, there were no significant differences found in the scores on HIV knowledge tests before and after the training program (88.5, 95 % CI 86.4–90.58 vs. 90.37, 95 % CI 88.4–92.3; p value: 0.08; t statistic 1.79).
Comfort Score
Peruvian peer leaders were comfortable using Facebook before the training program. The proportion of peer leaders comfortable using the Facebook tools did not significantly change after the training program. Post training, all peer leaders described themselves as at least comfortable using each social media tool (Table 2). After training, the majority of peer leaders also rated themselves as comfortable discussing each of the topics (Table 3). We found a significant increase in proportion of peer leaders who were comfortable discussing about sexual partners (70.5 vs. 50 %; p value 0.04; t statistic: 5.44) and about STIs (85.3 vs. 64.7 %; p value 0.02; t statistic: 7) after the training. There was no significant change after training in percent of peer leaders who were comfortable discussing other topics.
There were no differences between leaders recruited via Facebook or in-person at Epicentro on either the HIV knowledge or comfort scales.
Discussion
Although studies in the United States have been able to recruit peer leaders who are knowledgeable about HIV prevention and experienced using social media [23], it was unknown and uncertain whether we would be able to recruit peer leaders with these qualifications in international settings, such as Peru. This study found that it was feasible to recruit participants who satisfied these requirements and were skilled both in HIV prevention and use of social media in Peru. Results support that it is feasible to recruit peer leaders in international HIV prevention studies who already are experienced using social media, are knowledgeable about HIV, and from groups at high risk for HIV. Indeed, even though participants came from different educational backgrounds, they shared a similar HIV knowledge at baseline.
Although the post training mean score of HIV knowledge was greater than the pre training mean score, the difference was not statistically different. The lack of differences from pre- to post was likely due to our focused attempts (and success) in recruiting peer leaders who were already knowledgeable and qualified to communicate about HIV-related topics. These results, therefore, support that it is feasible to recruit peer leaders who are already experienced in HIV prevention and using social media. These effects are consistent with results from the HOPE study [20], although this study provides further evidence with a larger group of participants in an international setting. Sessions were designed to help to supplement and prepare peer leaders who were not already qualified prior to training.
Importantly, trained leaders did feel more comfortable using social media for health communication methods after training (83 vs. 71 %), suggesting that it is still important to train peer leaders even though they might be qualified in some areas (e.g. knowledge) on initial screening. Peer leaders reported feeling more comfortable using Facebook for “Talking about sexual partners” and “Talking about STIs” after being trained. This accomplishment of the training is crucial because implementing an online HIV/STI prevention intervention requires that leaders feel comfortable discussing such topics. The other changes between comfort levels before and after training likely failed to reach significance due to having recruited peer leaders who already felt comfortable discussing HIV/STIs-related topics and using Facebook before training.
This study might be limited by the inclusion criteria with which we recruited qualified participants. For this reason, we were not able to find major differences before and after training. The measure of knowledge might have not been challenging enough and reached a ceiling effect at baseline. Nevertheless, as an attempt to use a previously established questionnaire, we used the same measure of knowledge for the study in Peru that had been used in Los Angeles. Nonetheless, we confirmed that using specific criteria and, social media health communication training, could be enough to yield qualified peer leaders. In addition, training did improve their comfort level for communicating with peers about HIV prevention related topics.
This is the first study to assess the feasibility of recruiting and training peer leaders to deliver an online HIV prevention intervention to MSM in Latin America. In addition, this is a scale-up study from the HOPE UCLA that could be replicated obtaining similar results but with greater participants. The next step is to implement and assess the impact of such intervention [21]. Current findings suggest the feasibility of recruiting peer leaders who are qualified to conduct an HIV prevention social media-based intervention in international settings with high rates of HIV.
Conclusions
Qualified peer leaders can be recruited to participate in a peer health intervention to promote HIV testing among MSM in Peru on Facebook. It is feasible not only in the United States, but also in international settings, such as Peru, to recruit people who are already experienced in using social media and are interested in educating others about HIV and STIs through online social networks.
Future peer leader-based HIV prevention interventions can use inclusion criteria similar to those used in this study to recruit qualified leaders. Training can be designed following our methodology in order to help to supplement and prepare peer leaders who are not already qualified prior to training.
References
Duan Y, Zhang H, Wang J, Wei S, Yu F, She M. Community-based peer intervention to reduce HIV risk among men who have sex with men in Sichuan province, China. AIDS Educ Prev. 2013;25(1):38–48.
Medley A, Kennedy C, O’Reilly K, Sweat M. Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev. 2009;21(3):181–206.
St Lawrence JS, Brasfield TL, Diaz YE, Jefferson KW, Reynolds MT, Leonard MO. Three-year follow-up of an HIV risk-reduction intervention that used popular peers. Am J Public Health. 1994;84(12):2027–8.
Young SD, Konda K, Caceres C, Galea J, Sung-Jae L, Salazar X, et al. Effect of a community popular opinion leader HIV/STI intervention on stigma in urban, coastal Peru. AIDS Behav. 2011;15(5):930–7.
Zhang H, Zhu J, Wu Z, Pang L, Zhang L, Li T, et al. Intervention trial on HIV/AIDS among men who have sex with men based on venues and peer network. Zhonghua Yu Fang Yi Xue Za Zhi. 2009;43(11):970–6.
Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. A systematic review of HIV interventions for black men who have sex with men (MSM). BMC Public Health. 2013;13:625.
Hightow-Weidman LB, Smith JC, Valera E, Matthews DD, Lyons P. Keeping them in “STYLE”: finding, linking, and retaining young HIV-positive black and Latino men who have sex with men in care. AIDS Patient Care STDS. 2011;25(1):37–45.
NIMH Collaborative HIV/STD Prevention Trial Group. The community popular opinion leader HIV prevention programme conceptual basis and intervention procedures. AIDS. 2007;21(Suppl 2):S59–68.
Mellanby AR, Newcombe RG, Rees J, Tripp JH. A comparative study of peer-led and adult-led school sex education. Health Educ Res. 2001;16(4):481–92.
Maiorana A, Kegeles S, Fernandez P, Salazar X, Cáceres C, Sandoval C, et al. Implementation and evaluation of an HIV/STD intervention in Peru. Eval Program Plann. 2007;30(1):82–93.
Peru Country Progress Report UNAIDS [Internet]. 2011. http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_PE_Narrative_Report.pdf. Accessed 23 Jan 2015.
UNAIDS Report on the global AIDS epidemic 2012 [Internet]. 2012. http://www.unaids.org/en/resources/documents/2012/20121120_UNAIDS_Global_Report_2012. Accessed 23 Jan 2015.
Blas MM, Alva IE, Carcamo CP, Cabello R, Goodreau SM, Kimball AM, et al. Effect of an online video-based intervention to increase HIV testing in men who have sex with men in Peru. PLoS One. 2010;5(5):e10448.
Blas MM, Alva IE, Cabello R, Garcia PJ, Carcamo C, Redmon M, et al. Internet as a tool to access high-risk men who have sex with men from a resource-constrained setting: a study from Peru. Sex Transm Infect. 2007;83(7):567–70.
Blas MM, Menacho LA, Alva IE, Cabello R, Orellana ER. Motivating men who have sex with men to get tested for HIV through the Internet and mobile phones: a qualitative study. PLoS One. 2013;8(1):e54012.
Curioso WH, Kurth AE. Access, use and perceptions regarding internet, cell phones and PDAs as a means for health promotion for people living with HIV in Peru. BMC Med Inform Decis Mak. 2007;7:24.
Curioso WH, Blas MM, Nodell B, Alva IE, Kurth AE. Opportunities for providing web-based interventions to prevent sexually transmitted infections in Peru. PLoS Med. 2007;4(2):e11.
Facebook statistics [Internet]. 2013]. http://en.wikipedia.org/wiki/Facebook_statistics. Accessed 18 Apr 2013.
Jaganath D, Gill HK, Cohen AC, Young SD. Harnessing Online Peer Education (HOPE): integrating C-POL and social media to train peer leaders in HIV prevention. AIDS Care. 2012;24(5):593–600.
Young SD. Analysis of online social networking peer health educators. Stud Health Technol Inform. 2012;181:253–9.
Young SD, Jaganath D. Online social networking for HIV education and prevention: a mixed-methods analysis. Sex Transm Dis. 2013;40(2):162–7.
Young SD, Cumberland WG, Lee S-J, Jaganath D, Szekeres G, Coates T. Social networking technologies as an emerging tool for HIV prevention: a cluster randomized trial. Ann Intern Med. 2013;159(5):318–24.
Young SD, Harrell L, Jaganath D, Cohen AC, Shoptaw S. Feasibility of recruiting peer educators for an online social networking-based health intervention. Health Educ J. 2013;72(3):276–82.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Menacho, L.A., Galea, J.T. & Young, S.D. Feasibility of Recruiting Peer Educators to Promote HIV Testing Using Facebook Among Men Who have Sex with Men in Peru. AIDS Behav 19 (Suppl 2), 123–129 (2015). https://doi.org/10.1007/s10461-014-0987-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0987-5