Abstract
Young men who have sex with men have the highest rates of new HIV infections in the U.S., but they have been understudied relative to other populations. As a formative step for the development of a text messaging HIV prevention intervention, this mixed methods study aimed to understand how adolescent gay and bisexual males (AGBM) make decisions about condom use and factors that may differ based on age, sexual experience, and rural versus urban residency. Four online, asynchronous focus groups were conducted with 75 14–18 year old AGBM across the U.S. Qualitative analyses uncovered themes related to relationship influences on condom use (e.g. marriage, trust), access issues, and attitudes and experiences that both encouraged as well as discouraged condom use. Mixed methods analyses explored differences between groups in endorsement of themes. For example, younger and sexually experienced participants were more likely to report the cost of condoms was prohibitive and sexually experienced and rural youth were more likely to describe being influenced by emotional aspects of the relationship. These data highlight both opportunities for as well as the importance of tailoring HIV prevention programs for sub-groups of AGBM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent gay and bisexual men (AGBM),Footnote 1 along with other young men who have sex with men (MSM) but do not identify with these labels, represent the majority of HIV diagnoses among youth in the U.S. and are the group showing the largest increase in new infections [1, 2]. Despite this elevated risk, targeted prevention programs for this group are largely non-existent [3]. Even in the presence of biomedical prevention strategies such as Pre-Exposure Prophylaxis (PrEP) [4], condom use remains a critical and primary intervention strategy in HIV prevention because the majority of these HIV transmissions occur through unprotected sex [2]. Identifying the key predictors of condom use and condom decision making is of vital importance in addressing the burgeoning HIV epidemic among AGBM. Several studies of AGBM have found that an increase in HIV risk behaviors, including reduced condom use, are associated with factors including relationship length [5, 6], illicit drug use [7], sexual partner age [8], and experiences of trauma [9] (for a review see [1]). Additionally, engagement in unprotected anal intercourse (UAI) has been shown to be significantly associated with individual differences in impulsive decision making and sensation-seeking [10]. While we can make inferences about the rationale behind AGBM’s decisions on whether or not to use condoms based on these predictors, empirical research is crucial for the development of effective HIV prevention programs for AGBM that can address both individual and structural barriers.
If we are to affect HIV incidence rates, a singular focus on sexually active populations is unwarranted. Youth must be given skills to make healthy sexual behavior decisions before they become sexually active—particularly because condom use at first sex may be one of the most crucial factors for current condom use [11–15]. To our knowledge however, very few studies have specifically examined beliefs, intentions, and barriers to condom use among AGBM who have not yet had sex or compared these factors with those who have initiated sex.
The emerging literature on socio-environmental influences on LGBT youth make clear the need to take environmental context, specifically rural versus urban residence, into account when developing HIV prevention interventions tailored for LGBT youth [16, 17]. Although most cases of HIV occur in urban areas, HIV prevalence continues to increase in rural areas [18]. Limited research has shown that AGBM who live in rural areas might be more socially isolated due to the presence of fewer other AGBM, socially conservative attitudes, and lack of access to LGBT-specific services compared with AGBM living in urban areas [19–22]. All adolescents, not just AGBM, also tend to encounter more barriers to accessing sexual health services in rural settings. For example, prior studies of rural heterosexual youth identified unique concerns about confidentiality and condom access, such as fear and embarrassment of being seen purchasing condoms by someone known to the individual [23, 24]. However, these findings have yet to be focused specifically on rural AGBM, and it remains to be seen if they experience similar obstacles to accessing condoms and other preventive measures as their heterosexual counterparts. Therefore, it is imperative to identify the different factors impacting LGBT youth living in these areas in order to increase our understanding of how these environmental influences might affect their HIV risk behaviors.
To address these gaps in the literature, we report qualitative findings related to condom use and condom decision making among AGBM who took part in national, online focus groups that were conducted as part of the development of Guy2Guy, a text messaging-based HIV prevention program for AGBM. To identify ways in which intervention content about condom use could be tailored so that it is more contextually-relevant, three important sub-groups of AGBM were compared using mixed-methods analyses: sexually inexperienced/abstinent and sexually experienced/active youth; younger (14–16 years old) and older (17–18 years old) youth; and youth who live in rural and urban areas.
Methods
Online focus groups with 75 gay, bisexual, or queer identified 14–18 year old males across the United States were conducted in November 2012 and January 2013. The research protocol was reviewed and approved by the Chesapeake Institutional Review Board (IRB) and the Northwestern University IRB. A waiver of parental permission was obtained to prevent youth from being required to disclose their sexual identity to their parents in order to get their permission to participate, which may have put youth at risk for abuse or neglect by their parents and would not have offered them additional protections [25].
Participants
Four focus groups were conducted online: two with sexually inexperienced GBQ males (n = 36), and two with sexually experienced GBQ males (n = 39). Groups were stratified based on past sexual experience (ever anal or vaginal sex, versus never) to allow for in-depth and relevant discussion about sexual experiences and expectations. Eligibility requirements reflected those of the forthcoming randomized controlled trial and included: male biological sex; self-identified as gay, bisexual, or queer; between 14 and 18 years of age; spoke English; owned a cell phone and enrolled in an unlimited text messaging plan; used text messaging for at least 6 months; and intended to have the same cell phone number for at least 6 months. Guided by previous work [26], candidates were also required to complete an assessment of decisional capacity as part of the informed assent process. One 15-year-old participant did not pass the test of decisional capacity and therefore was not enrolled; all other participants passed the assessment.
Recruitment
Participants were recruited through advertisements posted on Facebook and two national LGBT-focused organizations’ websites. Purposeful sampling was used to assure that a culturally diverse group of participants (e.g., race, ethnicity, age, urban–rural status) was enrolled for both sexually experienced and inexperienced groups. Purposeful sampling is a technique used in qualitative research, which typically has smaller sample sizes in comparison to quantitative research, to foster information-rich cases specific to the aims of the research [27]. Recruitment advertisements included a link to an online screener form, which interested candidates completed. The information was then emailed to the project coordinator. Based upon their screener response, those who appeared eligible were contacted to confirm eligibility and those who were ineligible were emailed resources for HIV prevention. Once eligibility was determined, the study details were provided and verbal assent/consent obtained.
To reduce the likelihood of fraud or deception (e.g., the same participant enrolling more than one time), multiple steps were taken: (1) the screener website did not refer to the incentive amount; (2) the IP address used to complete the online screener was recorded; (3) screeners were reviewed for duplicative entries (e.g., same phone number); (4) eligibility was verified over the phone by a live person; and (5) phone and online screener data were compared for consistency. Additionally, for participants to engage in fraud, they would have had to provide different contact information (e.g., name, email address, phone number), as well as create unique responses to the focus group questions.
Procedures
Focus groups were conducted on a password-protected bulletin board website asynchronously over three consecutive days. Participants were asked to create a unique user name that was not their real name in order protect participant privacy. Two moderators from the research team simultaneously facilitated the focus groups. Each day, two sets of questions (or threads) were posted: first in the morning and the second in the afternoon. Participants were instructed to visit the bulletin board at least two times a day and respond to the questions that were posted. Additionally, probe questions were posted publically to the bulletin board to elicit a more detailed response when a participant’s answer was unclear. Private messages were then sent to participants to alert them of the probe question, which produced a high rate of response to probes. Additionally, participants were encouraged to interact with one another through questions about consensus and disagreement (e.g., “What do other people think about [respondent’s] point?” or “Does anyone disagree?”). The software facilitated this process by allowing participants to quote another participants response in their posting. Participants received a $25 Amazon gift card incentive for their participation.
Measures
Demographics
Quantitative data was collected over the phone by the project coordinator during enrollment. Participants reported their age, race and ethnicity, biological sex (i.e., “the sex you were assigned by the doctor at birth”), and sexual identity (gay, bisexual, or queer). For purposes of analyses, participants were grouped into the following age categories: 14–16 years of age and 17–18 years of age. Sexual experience was queried with the following question: “Have you ever had sex?” Responses options were not mutually exclusive and included: (1) No; (2) Yes, with a guy; (3) Yes, with a girl. Participants who endorsed ever having sex with either sex were assigned to the sexually experienced focus group and participants who never had sex to the sexually inexperienced group. Zip code was used to classify participants according to their urban or rural residence by linking to a Metropolitan Statistical Area code provided by SAS® [28].
Focus Group Guides
The theoretical model guiding the development of the Guy2Guy intervention was the Information-Motivation-Behavioral Skills model [29], and as such this model informed the development of our interview guide as well. The topics and questions discussed the first day of the focus groups were the same for both the sexually experienced and sexually inexperienced groups and focused on attitudes and logistical aspects of the intervention development. Topics discussed during day two of the focus groups provided the primary data for this manuscript, and included: sexual decision making, pressures to have sex, deciding not to have sex, feelings about condom use, reasons young men do not use condoms, making decisions about condom use, where young men find information about sex, experiences with healthy sexuality program, and opinions about receiving education about how to have sex. Topic questions were tailored for the sexually experienced and inexperienced groups when appropriate. For example, in regards to condom use decision making, both groups were asked their thoughts about condoms, using condoms, reasons why young men like themselves choose not to use condoms, and overcoming embarrassment about getting condoms. The sexually experienced groups were also asked how to support regular condom use (e.g., “What do you think could be done to help you use condoms more regularly?”) and about condom use decision making when one has a serious boyfriend (e.g., “What do you think about using condoms when you have a serious boyfriend?”).
Similar to day one of the focus groups, day three content was the same for both sexually experienced and inexperienced groups. Topics explored included: participant’s thoughts and concerns about the healthy sexuality program features, participation incentive ideas, and ways to promote participant retention in the eventual 6-week long healthy sexuality program.
Analytic Approach
The bulletin board software used for the online focus groups enabled us to extract the 75 individual level transcripts for direct import into Dedoose [30], a mixed-methods analysis program. Our analysis focused on individual level data (as opposed to analyzing it at the group level) in order to examine individual responses to our research questions and to then conduct mixed-methods analysis across subgroups based on individual characteristics.
For code development and application, we applied two rounds of constant comparison analysis. During the first phase of open coding, we coded all 75 transcripts using the guideline questions as our initial categories as well as identifying emerging themes [31–33]. These themes were then reviewed and refined using constant comparison techniques aimed at assessing similarities and differences between codes [31, 33]. This open coding resulted in the development of a codebook with 25 broad thematic codes (including “condoms”).
The codebook included code descriptions and illustrative examples of excerpts in order to facilitate inter-coder agreement in the application of these codes to subsequent transcripts [34]. A lead coder then applied these broad codes to a subset of transcripts. Other coders then applied the codes and Dedoose calculated the pooled Cohen’s Kappa in order to summarize inter-coder agreement across many codes [35]. The pooled Cohen’s Kappa was .85 across coders, indicating excellent agreement between coders [30, 36]. After this demonstration of reliability, coders applied codes to all of the remaining excerpts. At the end of coding, inter-rater reliability was again calculated on the final five transcripts to assure coding drift had not occurred. Cohen’s Kappa was .87 for these final transcripts, indicating an excellent level of reliability throughout the coding process.
After coding all 75 of the individual transcripts with the 25 broad codes, we extracted the 335 excerpts to which we had applied the code “condoms.” The “condoms” code was applied to any excerpt in which there was any reference to condoms. We then went through another stage of open coding to identify what participants were actually saying about their experiences with and attitudes about condoms. Three coders independently generated lists of sub-themes pertaining to condoms for comparison, discussion, and refinement. We resolved any disagreements through consensus. These codes were retained and applied to an additional subset of excerpts while we read for additional emergent themes. This iterative process continued until all of the excerpts were reviewed and an initial list of 84 axial codes related to condoms was generated. Two coders then used constant comparison techniques [31] to refine these 84 axial codes into 28 discrete axial codes. In the final stage of the coding process, we grouped the 28 axial codes into three overarching thematic categories: relationship factors, access issues, and attitudes/experiences. Axial codes that were applied to less than 5 excerpts (10 codes) were removed from the present analysis. Analyses thus included 18 axial codes related to condoms (Table 2).
After all transcripts were coded, the qualitative data were analyzed thematically [37]; that is, we explored thematic differences (pertaining to condoms) in relationship factors, attitudes/experiences, and issues of access that were discussed by the AGBM during our focus groups. In order to draw comparisons between sub-groups of focus group participants, we merged the quantitative data (i.e., sexual experience, urban/rural status, and age groupings) using mixed methods approaches [38, 39] that have been used successfully in prior studies [40–42]. Because established consensus guidelines do not exist for the size of group differences needed to be considered meaningful in mixed-methods research, following Magee [41] we considered group differences to be meaningful if they met three criteria: (a) differences had to be noticed as a theme during qualitative analysis, (b) the themes being compared had to be endorsed by a minimum of five participants, and (c) code application rates within each of the two groups being compared had to differ by at least 20 %. To facilitate readability, minor changes in grammar and spelling were corrected in quotations from focus group participants.
Results
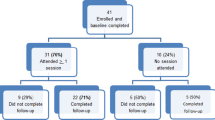
Four hundred and sixty total screeners were received, of which 193 were ineligible. One hundred and fifty-two candidates who appeared eligible were contacted, of which 80 were enrolled. Five enrolled participants never started the focus groups and therefore the analytic sample was 75. Assessment of recruitment source was added to the online screener mid-recruitment for FG1, as such the source of the first 14 participants enrolled is unknown. Based on the available data, 12 participants were recruited from Facebook and 49 were recruited from the two national LGBT organizations. Demographic characteristics were similar across the sexually experienced and sexually inexperienced groups, with the exception of those who were of mixed racial background, Hispanic ethnicity, and those who self-identified as gay, who were more often in the sexually experienced group (see Table 1). As an indication of engagement in the focus group, 95 % of participants (n = 71) posted at least one response in each session.
Qualitative Findings: Frequency of Code Application
The three thematic categories focused on here include: (a) relationship factors, (b) issues related to accessing condoms, and (c) attitudes and experiences with/about condoms. Table 2 includes descriptions of each of the 18 axial codes organized within these categories along with the number of participants and the number of excerpts that were coded with each axial code. We begin with a description of these themes and codes and then describe mixed-methods results of group differences in theme endorsement.
Relationship Factors
Three themes emerged: “relationship duration” (n = 25 excerpts), marriage/monogamy (n = 25 excerpts), and “trust” (n = 22 excerpts). Here “trust” refers to the perception of “knowing” or trusting a sex partner. The following quote provides an example of all three of these sentiments from the perspective of a 16-year-old, sexually experienced participant: “I personally want to continue using condoms until maybe 2 or 3 years after being married. It’s basically all about how much you trust your partner.”
While many of the comments made by participants referenced only one of these themes, this example shows the degree to which relationship factors may overlap, interacting in ways that together contribute to these young men’s decision making process around condoms. The co-occurrence of these themes reflects these interactions: half of the 22 “trust” excerpts were also coded with “marriage/monogamy” (11 excerpts) and 7 were coded with “relationship duration.” About a third of the 25 “relationship duration” excerpts also were coded for marriage (8 excerpts) or trust (7 excerpts).
While the themes “marriage/monogamy” and “trust” co-occurred in multiple excerpts, the meaning behind each theme remained discrete. For example, one 18-year-old sexually experienced participants said, “Why I wouldn’t wear a condom? Because I was either in a committed relationship with that person, or had known that person long enough to not question him when he tells me about his sexual past.” This example indicates that either being in a committed relationship (i.e. marriage or monogamy) or the duration of the relationship is described as leading to trust and the decision to not wear a condom.
Issues Related to Accessing Condoms
Problems accessing condoms centered on challenges buying them. Participants most frequently said that they felt embarrassed when buying condoms, were unsure of where they can purchase them, and/or that they were too expensive (39 applications). For example, when we asked participants to tell us what percentage of their peers used condoms, one 14-year-old sexually experienced participant shared:
“A very low percentage. For example, I would be extremely embarrassed to ask for them, and wouldn’t even know where to get them (I think they’re sold in vending machines! And pharmacies). Also, some don’t know how to use them properly and would feel awkward using them.”
Similarly, when we asked, “What do you think are reasons some young men like yourself don’t use condoms,” a 16-year-old sexually inexperienced participant emphasized the importance of this particular issue for teens stating,
“Umm… I think one of the more awkward aspects of it would be trying to figure out what kind to get, and not wanting to look stupid about it. I mean like if I were older (in my 20’s) then I’d be perfectly fine with it; at my current age if I were to go up to a cashier with condoms I would be mostly worried with the cashier giving me a dirty look, and thinking that I’m just another hormonal teen that’s craving sex.”
In addition to embarrassment, participants also described cost as an important barrier to condom use (n = 20 excerpts): “The price is my biggest factor. I don’t have a job and my parents wonder where my money goes” (16-year-old sexually experienced participant).
Another 16-year-old sexually experienced participant shared his views about why he thinks AGBM do not always use condoms saying;
“I view condoms as important. But many gay guys don’t use them (like 40 % do, I think) because they cost a lot and we can’t get pregnant from gay sex, and they don’t know too much about STDs. It would help if they were easier to get and a lot cheaper too!”
A 15-year-old sexually inexperienced participant said:
“I feel that they are essential to having safer sex, I mean I guess they are just part of staying healthy. I wish they were cheaper though because I have looked into prices before and WOW! They are pricey… condoms are like a little over a dollar each which I think is a lot.”
Attitudes and Experiences: Barriers to Condom Use
The attitude that being tested for HIV or STIs can enable you to know when a sex partner is “clean,” was talked about most frequently (n = 48 excerpts) as a reason to not use condoms. As described by a 14-year-old sexually experienced participant: “Only have bareback sex when you and your partner have both been tested for such diseases.”
The second most common theme as expressed here by a 15-year-old sexually inexperienced participant was the attitude that, “Many don’t like it because it doesn’t feel as good as without a condom.” This attitude/experience that condoms decrease pleasure was expressed in 44 excerpts, and included direct statements such as this comment made by an 18-year-old sexually experienced participant, “I HATE using condoms. I hate it. They almost dismiss the intimacy of sex and make it more of a business exchange. Not to mention feeling not even half as good, haha.”
Other, less frequently reported but nonetheless important reasons participants talked about not using condoms included their attitude that condoms were unnecessary (n = 28 excerpts). This attitude related to a lack of concern AGBM have about pregnancy risk, but was also linked to the notion that STIs do not pose a risk if both people are tested, as expressed by a 16-year old sexually inexperienced participant: “Guys probably don’t use them because they don’t have to worry about getting pregnant. As long as you are both tested and clean, I see no harm in not using them.” Feelings of invincibility (n = 10 excerpts) and thus not needing protection from STI’s were discussed by some of the AGBM in our groups. A 16-year-old sexually experienced participant conveyed this sentiment when describing why he thought young men like himself sometimes did not wear condoms: “The fact that we think we’re ten feet tall and bullet proof, we don’t think that we could catch something.”
In addition to attitudes, a number of experiences were described as negatively effecting condom use, including awkwardness while using condoms (n = 18 excerpts), having spontaneous sex (n = 14 excerpts), and fear of parents (n = 12 excerpts). Here, the term “awkward” was being used to refer to the potential discomfort of putting a condom on prior to having sex: “They think that …it ruins the moment to have to stop and put it on.” (18-year-old sexually experienced participant). Having spontaneous sex was also described as a reason some young men might not use condoms. A 16-year-old sexually experienced participant described this saying, “Because, in a lot of cases love just happens. Like I said, then you forget and live in the moment.” Similarly, a 15-year-old sexually experienced participant described the difference for him between having sex that was planned compared to spontaneous sex when he said:
“When it just happens it’s more because you’re in the moment. You don’t mean for it to carry on that far, but it did, so you’re not as careful as when you may plan it. When it’s planned, you always have condoms and such.”
Finally, some of these young men conveyed that they (and/or their peers) felt afraid that their parents might find their condoms, or find out that they were buying condoms and that that fear reduced condom use. For example, “…they may be afraid that their parents will see them in their room and just flip out” (15-year-old sexually experienced participant).
Attitudes and Experiences: Encouraging Condom Use
While there was a lot of discussion about barriers to condom acquisition and use among the young men in these focus groups, they also shared reasons that inspire or increase condom use for themselves or other AGBM. Most frequently (n = 52 excerpts), participants talked about their views that condoms are effective and that they know they should use them. For instance, a 17-year-old sexually inexperienced participant said, “I definitely feel that condoms are a necessity! It takes away a lot of worries of what could go wrong with sex.” Related to this, fears about the potential consequences of not wearing a condom (e.g., STIs) were voiced: “My last serious boyfriend and I decided to always use condoms for anal sex because I found out you can contract diseases or infections in the urethra of the penis after “bareback” anal sex.” (16-year-old sexually experienced participant). This sentiment, appearing in 40 excerpts, conveyed that fear functions as a motivator to use condoms. Finally, participants conveyed their rational intention to use condoms in 32 excerpts: “In my honest opinion, I feel like it’s simply irrational not to use condoms. Even in a monogamous relationship, I’d still use condoms. It protects myself and the person I love” (16-year-old sexually inexperienced participant). Another said: “I’d always wanna use them, no matter what. It’s not worth getting a disease.” (17-year-old sexually inexperienced participant).
Finally, since perceived peer norms are an important factor in adolescent condom use [43, 44], we asked participants to tell us what percentage of young men like themselves they thought used condoms. The majority of excerpts (25) addressing this question reflected the perception that most (more than half of) peers do not use condoms while 9 excerpts conveyed the perception that that most peers do use condoms.
Mixed Methods Results
Figures 1, 2 and 3 present the percentages of excerpts that were associated with a particular code, separately for each of the three different sub-groups examined. Using the approach built into the Dedoose software, these data were normalized because there were unequal numbers of cases in each group. The normalization function operates by assigning a weight of “1” to the group with the largest number of members (“basis group”) and then assigns weights to the other groups as a function of the numeric relation between the number of members in the group to that of the number of members in the “basis group” [30]. These weights are then used to adjust the number of raw counts to accomplish ratio equivalence across group and the weighted percentage is calculated based on these adjusted counts. This normalization is necessary because the graphical representation for code application frequency by group is relatively meaningless if there are unequal numbers of individual cases across each sub-group. As such, figures used for group comparisons were made using these normalized values.
Sexually Experienced and Sexually Inexperienced Groups
Sexually experienced participants talked more frequently about condoms (n = 223 excerpts, 66.6 %) than did sexually inexperienced participants (n = 112 excerpts, 33.4 %). As shown in Fig. 1, compared to their sexually inexperienced counterparts, focus group participants who were sexually experienced talked more specifically about not using condoms due to relationship factors including marriage/monogamy and the duration of their relationships (80 % of excerpts). In terms of access-related barriers, sexually experienced participants also more frequently referred to the cost of condoms (70 % of excerpts) and their feelings of embarrassment and difficulty when they were buying or trying to get condoms (64 % of excerpts).
In terms of attitudes about and experiences with condoms that could reduce condom use, sexually experienced participants most frequently (92 % of the excerpts) talked about being afraid that their parents would find their condoms or discover that they were spending money on condoms. Having spontaneous sex (86 % of excerpts), being tested/knowing that their partners were “clean” (75 % of excerpts), and oral sex (73 % of excerpts) were also reasons that were frequently discussed by sexually experienced participants in relation to not using condoms. Finally, the majority (88 %) of the comments conveying the perception that most (more than half) of their peers do not use condoms were made by sexually experienced participants.
There were fewer differences between groups in terms of attitudes that contributed to condom use. Sexually inexperienced participants more frequently indicated that they thought of condoms as effective and something they should use or plan to use when they have sex (65 % of excerpts).
Younger (14–16 years old) and Older (17–18 years old) Participants
Compared to their older counterparts, younger participants more frequently raised issues related to accessing condoms, especially the cost (72 % of excerpts; Fig. 2). Although in this sample age was balanced with sexual activity grouping, the experience of being a sexually experienced 14-year-old is likely to be different than an experienced 18-year-old, therefore we further examined age differences by sexually experienced versus inexperienced status. The majority of the comments made by younger participants referencing the cost of condoms were made by those who were sexually experienced (75 % of excerpts), whereas for older participants, sexually experienced and inexperienced participants made equal reference to cost (50 % of excerpts). Younger participants who were sexually experienced (75 % of excerpts) and older participants who were sexually inexperienced (64 % of excerpts) most frequently expressed feeling like condoms were inconvenient or embarrassing to buy.
Younger participants talked more frequently about the role of spontaneous sex as negatively affecting the use of condoms (79 % of excerpts). Similar to the sexually experienced participants described above, there was a trend for younger participants to more frequently report (66 % of excerpts) a fear of their parents finding their condoms or learning that they had purchased them. The majority of these comments were made by sexually experienced younger participants (90 %), however. Although older participants talked less overall about fears of their parents, all of those who did were sexually experienced. In contrast, both younger (49 % of excerpts) and older (51 % of excerpts) participants described feelings of invincibility as contributing to reduced condom use. Interestingly, in terms of invincibility, the majority of comments from the younger group were made by those who are sexually inexperienced (67 % of excerpts) whereas the majority of comments from older participants were those who were sexually experienced (75 %). Few differences existed by age in terms of motivators for condom use.
Urban and Rural Participants
As shown in Fig. 3, there was a trend for rural participants, compared to urban participants, to have made more frequent reference to relationship factors as reasons to reduce condoms use, including marriage/monogamy (67 % of excerpts), trust (59 %) and relationship duration (59 %). Other themes that were voiced more frequently by rural participants were attitudes/experiences including the sentiment that condoms are awkward to use (62 % of excerpts) and that spontaneous sex contributes to reduced condom use (59 %). The only theme that was mentioned more frequently by urban AGBM was the perception that condoms are effective and should be used (65 % of excerpts).
Discussion
Young MSM represent the largest proportion of new HIV diagnoses [2, 45], yet little research has been conducted to understand how this vulnerable population makes decisions about condom use—particularly among adolescents (versus young adults up to age 24 or even 29 who are frequently grouped with “youth”), those in rural areas, and those who have not yet had sex for the first time. Based upon data from online focus groups with 14–18 year old AGBM, themes emerged related to relationship influences on condom use (e.g. marriage, trust), access issues, and attitudes and experiences that both encouraged as well as discouraged condom. Our innovative mixed-methods analyses also uncovered differences between participants based on age, urban–rural status, or if they had yet to have sex for the first time.
Many AGBM who successfully obtained condoms said they did so online because they are inexpensive and you do not have to show your face in a store and thereby avoid embarrassment. Compared to purchasing in retail stores, online requisitioning of condoms for AGBM should be considered as a relatively low-cost option for inclusion in HIV prevention programs targeting this population. Similar to prior studies of adolescents [23, 46], embarrassment was cited as a major barrier among AGBM who did not access condoms. Importantly too, one in five said that the cost was prohibitive. These sentiments were most often expressed by younger and sexually experienced participants. These findings may be surprising to researchers in urban areas whose populations have access to many settings that provide free condoms. It may also reflect the younger age group in the current study. Unlike young adults who may go to bars, 14 and 15-year-olds in our focus groups, both rural and urban, described salient barriers to obtaining condoms. Prior research has shown the population health benefits of initiatives to make condoms freely and easily available [47–49] and the CDC has included condom distribution as a core element of their new “high-impact approach to HIV prevention” [50]. Our findings support the need for such programs to be further expanded to venues where adolescents have access (e.g., school health clinics, coffee shops, and other places where adolescents spend time) to assure these approaches will reach AGBM.
Our qualitative findings parallel quantitative research on late adolescent and young adult MSM that has consistently shown that characterizing a relationship as “serious” or a partner as a “main partner” is associated with unprotected anal sex [6, 8, 51–54]. These findings are also similar to prior quantitative studies of adult gay/bisexual men that have implicated feelings of intimacy, trust, and closeness in explaining unprotected sex [55–57]. We add to these prior studies by demonstrating the consistent impact of relationship factors within the very young sample. Our mixed-methods analyses also uncovered that when compared to sexually inexperienced youth, these sentiments are particularly salient for sexually experienced AGBM. Perhaps, sexually inexperienced AGBM have not yet had a serious romantic relationship and therefore have less to say about the eventual influence of emotions linked to serious relationships. Interestingly, these themes were also more often endorsed among AGBM living in rural areas. This may be because rural youth are more likely to be exclusively exposed to traditional monogamous relationships and less to discussion of infidelity or open relationships. HIV prevention programs should target messages to sexually experienced AGBM that norm condom use as a way of showing “love” and “trust”; and perhaps similar messages for youth living in rural areas across both sexual experience groups.
Another theme related to interpersonal processes was the concept that if a partner was known to be “clean” because he was tested for STIs/HIV, then condoms are unnecessary. Younger age groups of MSM have much higher rates of being unaware of an HIV positive status; the CDC estimates that 75 % of 18–19 year-olds who are HIV positive do not know their status [58]. Data for AGBM in our age range are not available. Thus, a partner could say that he is HIV negative, believe it, and yet be wrong. One way to assure a known partner HIV status is to test together. Recent research with adult MSM has found high levels of acceptance of couples testing [59] and the CDC has recently endorsed couples testing and counseling as an effective strategy for HIV prevention [60]. Some AGBM talked about the importance of testing together before discontinuing condom use. This suggests that similar strategies would be acceptable in HIV prevention programs targeting AGBM, although would likely require adaptation for developmental differences from adults (e.g., adolescent couples will generally have less relationship history, less ability to provide instrumental support in the case of an HIV diagnosis, etc.).
A number of themes emerged related to attitudes that inhibited condom use, including the perspective that they decrease pleasure and are awkward to use. Much has been written about the issue of condoms and sexual pleasure, with several studies showing that men who perceived a large decrease in pleasure with condom use less likely to use condoms [61–64]. To address the negative impact of perceived pleasure loss on condom use, one randomized trial of adult heterosexual couples found that providing instruction in how to “erotically” incorporate condoms into sexual behavior found that doing so significantly enhanced attitudes towards condoms at follow-up [65]. Intervention programs designed for youth that use a comprehensive sexual health framework [66] that address sexual pleasure, such as the online Queer Sex Ed intervention for LGBT youth [67], may be best positioned to provide instruction in pleasurable sex with condom use and thereby directly combat this reason for non-condom use. This may be difficult to do with younger cohorts, whose sensibilities may be more conservative, and protections by ethical review boards from “salacious” content may be stronger. Given the positive results of studies of even slightly older males however, researchers targeting this age range should evaluate developmentally appropriate approaches.
Many AGBM cited perceived “invincibility” as a reason for not using condoms, believing that they would never get HIV/STIs. This finding is consistent with previous research with adolescents [68–70] and adult MSM [71]. Within our study, we also identified differences in endorsement based on age group: sexually inexperienced younger AGBM and sexually experienced older AGBM most frequently mentioned “invincibility.” The latter endorsement reflects the sentiment reported by many older MSM who think they are immune to HIV because they were not infected during prior condomless sexual encounters [71, 72], while the former is perhaps an artifact of their lack of sexual experience.
Unexpectedly, some of the AGBM expressed a belief that condoms are unnecessary because pregnancy is not possible with male-to-male sex. It is common for adolescents, particularly, to depersonalize risk [73, 74]. Perhaps this is a way of further depersonalizing risk for AGBM. If so, then prevention programs need to address this head on, and help AGBM internalize the benefits of condom use for themselves. Another concern raised about condoms was that parents may find them. This issue was more frequently raised by the youngest participants as well as those who were sexually experienced. This speaks to the benefits of family-based prevention programs where parents are taught along with adolescents about the benefits of condom use and how to serve as a resource to their child in accessing condoms. Such interventions have been widely studied among heterosexual youth [75], but not among AGBM [76, 77], likely due to the unfounded belief that very few AGBM are out to their parents [78].
Certainly, not all youth were against condoms. Barriers were specifically queried, which is why so many were identified. Facilitators of condom use also were queried and therefore voiced, the most common of which was that condoms are an effective way to stay healthy. This sentiment was expressed more often among those who had not had sex and those in urban settings. The fear of diseases was the second most commonly voiced motivator. This seemed to be expressed equally across all groups. That said, the majority of AGBM believed their friends did not use condoms when they have sex, echoing the influence of perceived peer norms and behaviors on condom use among adolescents reported by others [61, 69]. It is interesting to note that these three aspects are typically described as motivators for condom use in widely used theories of HIV preventive behaviors. For example, the Information-Motivation-Behavioral Skills Model [29] considers motivation a multidimensional construct that includes factors such as social norms, feelings of personal vulnerability, beliefs about consequences of HIV, and beliefs about condom use. These findings support the use of the IMB model and others that target these aspects of motivation for AGBM-focused HIV prevention programs.
Results must be interpreted within the context of study limitations. First, these findings come from AGBM recruited online. Therefore they may not generalize to AGBM who do not use the websites where we recruited or are unable to privately access the internet for three days of online focus groups. Nevertheless, AGBM who use the internet for sexual purposes—a group likely to be recruited using online recruitment approaches such as ours—are at increased risk for HIV infection [79] and understanding their perspectives on condom use will lead to better informed and uniquely targeted prevention programs. Moreover, the online recruitment strategy surely resulted in a broader sample than traditional methods that recruit participants from a specific city or circumscribed region. Second, we used an online focus group method, which means that participants had to be willing to share their beliefs in the online focus group. We required participants to use a username other than their own name to help assure anonymity in the group, but nevertheless, some participants may have been reluctant to share their perspectives in such a forum. At the same time, it has been suggested that individuals from stigmatized groups are more likely to participate in online than face-to-face forums [80]. Another limitation of the online text-based focus group method is that it is not possible to monitor non-verbal behaviors and reactions. Third, we did not define “sex” in the screener. If youth asked for clarification, study staff specified that it referred to vaginal or anal sex. It is possible that some youth self-selected into the groups in a way different from what was intended. Finally, this is one of the first mixed-methods studies to examine AGBM’s perspectives on condom use—particularly to include 14–15 year olds and rural youth. As such, replication is essential to confirm our novel findings. Future qualitative and quantitative studies can extend our findings by incorporating these beliefs into testable models of condom use decision making.
Conclusions
Based upon these focus group data, intervention messages for the Guy2Guy text messaging program were crafted to encourage AGBM to consider buying condoms online if they were embarrassed to go into a store. Other messages were written to address cost and let youth know that they can get condoms for free at health clinics. Messages also addressed the belief that not using condoms equals trust in a relationship, and suggested instead that caring about one’s health by using condoms connotes trust. Program content also highlighted the lack of awareness of one’s STI status. Finally, the benefits of condoms noted by focus group participants were used to counter reasons why AGBM may choose not to use condoms.
Adolescent gay, bisexual, and queer males of high school age are at risk for HIV and other STIs, but tailored healthy sexuality programs are completely lacking. As a result, there is a dearth of knowledge about their condom use decision making practices-particularly among those who have not had sex. Our focus group findings suggest that many factors observed in older MSM populations also resonate with adolescents: concerns that condoms decrease pleasure, that you do not need to use condoms in committed relationships, etc. Factors that appear unique to adolescence also emerged, including embarrassment about interacting with a store clerk when buying condoms and insufficient finances to buy them. These data highlight both opportunities for as well as the importance of tailoring programs for AGBM. Their experiences and concerns are similar, yet clearly different from older populations. A simple “find and replace” approach to developmentally tailoring existing HIV prevention programs would be ill advised.
Notes
We use the AGBM identifier because this study focuses specifically on adolescent boys that identify as gay, bisexual, or queer. These young men do not need to be sexually active to be involved in the study. However, much of the existing literature focuses on men who have sex with men (MSM) or lesbian, gay, bisexual, and transgender (LGBT) individuals. As such we use these additional identifiers as appropriate to the context of the literature we are describing.
References
Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–53.
CDC. Vital signs: HIV infection, testing, and risk behaviors among youths—United States. MMWR Morb Mortal Wkly Rep. 2012;61:971–6.
CDC. Compendium of evidence-based HIV prevention interventions. 2013; http://www.cdc.gov/hiv/prevention/research/compendium/rr/index.html. Accessed 10/07/2013.
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587–99.
Hart T, Peterson JL, Community Intervention Trial for Youth Study T. Predictors of risky sexual behavior among young African American men who have sex with men. Am J Public Health. 2004;94:1122–4.
Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychol. 2011;30:597–605.
Thiede H, Valleroy LA, MacKellar DA, et al. Regional patterns and correlates of substance use among young men who have sex with men in 7 US urban areas. Am J Public Health. 2003;93:1915–21.
Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on HIV infection among African American men who have sex with men in the Young Men’s Survey, Los Angeles, 1999–2000. AIDS Educ Prev. 2003;15:39–52.
Miller RL, Reed SJ, McNall MA, Forney JC. The effect of trauma on recent inconsistent condom use among young black gay and bisexual men. J HIV/AIDS Soc Serv. 2013;12:349–67.
Dudley MG, Rostosky SS, Korfhage BA, Zimmerman RS. Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Educ Prev. 2004;16:328–40.
Shafii T, Stovel K, Davis R, Holmes K. Is condom use habit forming? Condom use at sexual debut and subsequent condom use. Sex Transm Dis. 2004;31:366–72.
Robertson A, Levin ML. AIDS knowledge, condom attitudes, and risk-taking sexual behavior of substance-abusing juvenile offenders on probation or parole. AIDS Educ Prev. 1999;11:450–61.
Lawrence JS, Scott CP. Examination of the relationship between African American adolescents’ condom use at sexual onset and later sexual behavior: implications for condom distribution programs. AIDS Educ Prev. 1996;8:258–66.
Hendriksen ES, Pettifor A, Lee SJ, Coates TJ, Rees HV. Predictors of condom use among young adults in South Africa: the Reproductive Health and HIV Research Unit National Youth Survey. Am J Public Health. 2007;97:1241–8.
Shafii T, Stovel K, Holmes K. Association between condom use at sexual debut and subsequent sexual trajectories: a longitudinal study using biomarkers. Am J Public Health. 2007;97:1090–5.
Hatzenbuehler ML. Social factors as determinants of mental health disparities in LGB populations: implications for public policy. Soc Issues Policy Rev. 2010;4:31–62.
Poon CS, Saewyc EM. Out yonder: sexual-minority adolescents in rural communities in British Columbia. Am J Public Health. 2009;99:118–24.
Hall HI, Li J, McKenna MT. HIV in predominantly rural areas of the United States. J Rural Health. 2005;21:245–53.
D’Augelli AR. Coming out in community psychology: personal narrative and disciplinary change. Am J Community Psychol. 2003;31:343–54.
D’Augelli AR, Hart MM. Gay women, men, and families in rural settings: toward the development of helping communities. Am J Community Psychol. 1987;15:79–93.
Oswald RF, Culton LS. Under the rainbow: rural gay life and its relevance for family providers. Fam Relat. 2003;52:72–81.
Stroup J, Glass J, Cohn TJ. The adjustment to U.S. rural college campuses for bisexual students in comparison to gay and lesbian students: an exploratory study. J Bisex. 2014;14:94–109.
Bell J. Why embarrassment inhibits the acquisition and use of condoms: a qualitative approach to understanding risky sexual behaviour. J Adolesc. 2009;32:379–91.
Garside R, Ayres R, Owen M, Pearson VA, Roizen J. Anonymity and confidentiality: rural teenagers’ concerns when accessing sexual health services. J Fam Plann Reprod Health Care. 2002;28:23–6.
Mustanski B. Ethical and regulatory issues with conducting sexuality research with LGBT adolescents: a call to action for a scientifically informed approach. Arch Sex Behav. 2010;40:673–86.
Mustanski B, Newcomb M, Garofalo R. Mental health of lesbian, gay, and bisexual youth: a developmental resiliency perspective. J Gay Lesbian Soc Serv. 2011;23:204–25.
Patton MQ. Qualitative research & evaluation methods. 3rd ed. Thousand Oaks: Sage Publications; 2001.
Hadden L, Zdeb M. A well-kept SAS® secret. 31st Annual SAS® Users Groups International Conference (SUGI 31). San Francisco, CA 2006.
Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychol. 1994;13:238–50.
Dedoose: Web application for managing, analyzing, and presenting qualitative and mixed method data. [computer program]. Version 4.5.91. Los Angeles, CA: SocioCultural Research Consultants, LLC.; 2012.
Glaser BG, Strauss AL. The discovery of grounded theory: strategies for qualitative research. Chicago: Aldine Publishing Co; 1967.
Carey MA, Smith MW. Capturing the group effect in focus groups: a special concern in analysis. Qual Health Res. 1994;4:123–7.
Ryan GW, Bernard HR. Techniques to identify themes. Field Methods. 2003;15:85.
MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Field Methods. 1998;10:31.
De Vries H, Elliot MN, Kanouse DE, Teleki SS. Using pooled kappa to summarize interrater agreement across many items. Field Methods. 2008;20:10.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. 2nd ed. Thousand Oaks: Sage Publications; 1994.
Axinn WG, Pearce LD. Mixed method data collection strategies. Cambridge: Cambridge University Press; 2006.
Boardman F, Griffiths F, Kokanovic R, Potiriadis M, Dowrick C, Gunn J. Resilience as a response to the stigma of depression: a mixed methods analysis. J Affect Disord. 2011;135:267–76.
DeHaan S, Kuper LE, Magee JC, Bigelow L, Mustanski BS. The interplay between online and offline explorations of identity, relationships, and sex: a mixed-methods study with LGBT youth. J Sex Res. 2013;50:421–34.
Magee JC, Bigelow L, Dehaan S, Mustanski BS. Sexual health information seeking online: a mixed-methods study among lesbian, gay, bisexual, and transgender young people. Health Educ Behav. 2012;39:276–89.
Mustanski B, Lyons T, Garcia S. Internet use and sexual health of young men who have sex with men: a mixed-methods study. Arch Sex Behav. 2011;40:289–300.
Diclemente RJ. Predictors of HIV-preventive sexual behavior in a high-risk adolescent population: the influence of perceived peer norms and sexual communication on incarcerated adolescents’ consistent use of condoms. J Adolesc Health. 1991;12:385–90.
Pedlow CT, Carey MP. Developmentally appropriate sexual risk reduction interventions for adolescents: rationale, review of interventions, and recommendations for research and practice. Ann Behav Med. 2004;27:172–84.
Mustanski B, Newcomb ME, DuBois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–53.
Ronis ST, LeBouthillier DM. University students’ attitudes toward purchasing condoms. Can J Hum Sex. 2013;22:86–94.
Burke RC, Wilson J, Bernstein KT, et al. The NYC condom: use and acceptability of New York City’s branded condom. Am J Public Health. 2009;99:2178–80.
Cohen DA, Farley TA, Bedimo-Etame JR, et al. Implementation of condom social marketing in Louisiana, 1993 to 1996. Am J Public Health. 1999;89:204–8.
Cohen D, Scribner R, Bedimo R, Farley TA. Cost as a barrier to condom use: the evidence for condom subsidies in the United States. Am J Public Health. 1999;89:567–8.
CDC. High-impact HIV prevention: CDC’s approach to reducing HIV infections in the United States: Centers for Disease Control and Prevention; National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; Division of HIV/AIDS Prevention; 2011.
Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Arch Sex Behav. 2014;43:61–72.
Choi KH, Han CS, Hudes ES, Kegeles S. Unprotected sex and associated risk factors among young Asian and Pacific Islander men who have sex with men. AIDS Educ Prev. 2002;14:472–81.
Hart T, Peterson JL, Community Intervention Trial for Youth Study Team. Predictors of risky sexual behavior among young African American men who have sex with men. Am J Public Health. 2004;94:1122–4.
Stueve A, O’Donnell L, Duran R, San Doval A, Geier J. Being high and taking sexual risks: findings from a multisite survey of urban young men who have sex with men. AIDS Educ Prev. 2002;14:482–95.
Davidovich U, de Wit JB, Stroebe W. Behavioral and cognitive barriers to safer sex between men in steady relationships: implications for prevention strategies. AIDS Educ Prev. 2004;16:304–14.
Theodore PS, Duran RE, Antoni MH, Fernandez MI. Intimacy and sexual behavior among HIV-positive men-who-have-sex-with-men in primary relationships. AIDS Behav. 2004;8:321–31.
Zea MC, Reisen CA, Poppen PJ, Bianchi FT. Unprotected anal intercourse among immigrant Latino MSM: the role of characteristics of the person and the sexual encounter. AIDS Behav. 2009;13:700–15.
CDC. Prevalence and awareness of HIV infection among men who have sex with men: 21 cities, United States. MMWR Morb Mortal Wkly Rep. 2008;2010(59):1201–7.
Stephenson R, Sullivan PS, Salazar LF, Gratzer B, Allen S, Seelbach E. Attitudes towards couples-based HIV testing among MSM in three US cities. AIDS Behav. 2011;15(Suppl 1):S80–7.
CDC. Couples HIV Testing and Counseling. 2013; https://www.effectiveinterventions.org/en/HighImpactPrevention/PublicHealthStrategies/CHTC.aspx. Accessed 10 Jan 2014.
Brown LK, DiClemente R, Crosby R, et al. Condom use among high-risk adolescents: anticipation of partner disapproval and less pleasure associated with not using condoms. Public Health Rep. 2008;123:601–7.
Randolph ME, Pinkerton SD, Bogart LM, Cecil H, Abramson PR. Sexual pleasure and condom use. Arch Sex Behav. 2007;36:844–8.
Albarracin D, Ho RM, McNatt PS, et al. Structure of outcome beliefs in condom use. The Project RESPECT Study Group. Health Psychol. 2000;19:458–68.
Choi KH, Rickman R, Catania JA. What heterosexual adults believe about condoms. N Engl J Med. 1994;331:406–7.
Tanner WM, Pollack RH. The effect of condom use and erotic instructions on attitudes toward condoms. J Sex Res. 1988;25:537–41.
WHO. Defining sexual health: Report of a technical consultation on sexual health. 2006; http://www.who.int/reproductivehealth/publications/general/lancet_1.pdf. Accessed 13 Jan 2014.
Mustanski B, Greene GJ, Ryan D, Whitton SW. Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: The Queer Sex Ed intervention. J Sex Res 2014. doi:10.1080/00224499.2013.867924.
Duncan C, Miller DM, Borskey EJ, Fomby B, Dawson P, Davis L. Barriers to safer sex practices among African American college students. J Natl Med Assoc. 2002;94:944–51.
Grossman C, Hadley W, Brown LK, et al. Adolescent sexual risk: factors predicting condom use across the stages of change. AIDS Behav. 2008;12:913–22.
Thompson SC, Kyle D, Swan J, Thomas C, Vrungos S. Increasing condom use by undermining perceived invulnerability to HIV. AIDS Educ Prev. 2002;14:505–14.
Frasca T, Ventuneac A, Balan I, Carballo-Dieguez A. Inner contradictions among men who bareback. Qual Health Res. 2012;22:946–56.
Dufour A, Alary M, Otis J, et al. Correlates of risky behaviors among young and older men having sexual relations with men in Montreal, Quebec, Canada. Omega Study Group. J Acquir Immune Defic Syndr. 2000;23:272–8.
Gruber E, Chambers CV. Cognitive development and adolescent contraception: integrating theory and practice. Adolescence. 1987;22:661–70.
Elkind D. Egocentrism in adolescence. Child Dev. 1967;38(4):1025–34.
Pequegnat W. Family and HIV/AIDs: cultural and contextual issues in prevention and treatment. New York: Springer; 2011.
Mustanski B, Hunter J. Parents as agents of HIV prevention for gay, lesbian, and bisexual youth. In: Pequegnat W, Bell C, editors. Family and HIV/AIDS: cultural and contextual issues in prevention and treatment. New York: Springer; 2011 Chapter 12.
Garofalo R, Mustanski B, Donenberg G. Parents know and parents matter; is it time to develop family-based HIV prevention programs for young men who have sex with men? J Adolesc Health. 2008;43:201–4.
Mustanski B, Newcomb M, Garofalo R. Mental health of lesbian, gay, and bisexual youth: a developmental resiliency perspective. J Gay Lesbian Soc Serv. 2011;23:204–25.
Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the iceberg: young men who have sex with men, the Internet, and HIV risk. Am J Public Health. 2007;97:1113–7.
Fox FE, Morris M, Rumsey N. Doing synchronous online focus groups with young people: methodological reflections. Qual Health Res. 2007;17:539–47.
Acknowledgments
This research was funded by a Grant from the National Institute of Mental Health at the National Institutes of Health (R01MH096660; PIs: Mustanski and Ybarra). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank our two study consultants, Drs. Sheana Bull and Jeffrey Parsons, for their feedback on the design of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mustanski, B., DuBois, L.Z., Prescott, T.L. et al. A Mixed-Methods Study of Condom Use and Decision Making Among Adolescent Gay and Bisexual Males. AIDS Behav 18, 1955–1969 (2014). https://doi.org/10.1007/s10461-014-0810-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0810-3