Abstract
The impact of depressive symptoms on ART initiation among Russian HIV-infected heavy drinkers enrolled in a secondary HIV prevention trial (HERMITAGE) was examined. We assessed 133 participants eligible for ART initiation (i.e., CD4 count <350 cells/μl) who were not on ART at baseline. Depressive symptom severity and ART use were measured at baseline, 6- and 12-months. Association between depressive symptoms and subsequent ART initiation was evaluated using GEE logistic regression adjusting for gender, past ART use, injection drug use and heavy drinking. Depressive symptom severity was not significantly associated with lower odds of initiating ART. Cognitive depression symptoms were not statistically significant (global p = 0.05); however, those with the highest level of severity had an AOR of 0.25 (95 % CI 0.09–0.71) for delayed ART initiation. Although the effect of depression severity was not significant, findings suggest a potential role of cognitive depression symptoms in decisions to initiate ART in this population.
Resumen
En este artículo se examina el impacto de síntomas depresivos en la decisión de bebedores de riesgo, infectados con VIH, para iniciar el TARV. Ellos fueron inscritos en un estudio en Rusia diseñado para prevenir el contagio del VIH en otras personas (HERMITAGE). Evaluamos a 133 participantes elegibles para comenzar el tratamiento TARV (i.e., recuento de CD4 < 350 células/μl) quienes no estaban en TARV al inicio del estudio. La severidad de los síntomas depresivos y el uso de TARV fueron medidos a 0, 6 y 12 meses. La asociación entre síntomas depresivos y la subsecuente iniciación de TARV fue evaluada usando regresión logística GEE ajustada por género, antiguo uso del TARV, uso de drogas inyectadas y uso de alcohol en exceso. La severidad de síntomas depresivos no está significativamente asociada con menores probabilidades de comenzar TARV. Síntomas de depresión cognitiva no fueron estadísticamente significantes (global p = 0.05); sin embargo, aquellos con mayor nivel de severidad tenían un ORA de 0.25 (95 % IC 0.09-0.71) en el retraso para iniciar TARV. Aunque los efectos de la severidad de la depresión no fueron significantes, los resultados sugieren un rol potencial de los síntomas de la depresión cognitiva en las decisiones para iniciar TARV en esta población.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Depression is the most commonly diagnosed psychiatric illness in people living with HIV, with prevalence rates 2–10 times higher than the general population [1, 2]. In addition to the heightened distress and reduced functioning that comes with depression, depressive symptoms have been shown to influence human immunodeficiency virus (HIV) progression (i.e., decreasing CD4 counts and increasing viral loads) [3–7], and have been associated with poor virologic response to treatment, increased immunologic failure, increased likelihood of AIDS-defining illness [2, 7], and increased risky behaviors (e.g., unsafe sex, alcohol and drug use) [8, 9]. Conversely, studies have shown that treatment of depression can lead to multiple positive health outcomes for those living with HIV, such as improved coping skills, better medication adherence to antiretroviral therapy (ART), and increased health-related quality of life [10].
A variety of biological and behavioral mechanisms may explain how depression influences HIV disease progression [6, 11–13], with one of the more important of these being its effects on adherence to ART [14]. The importance of early initiation and consistent use of ART has been well documented [15]. Delayed ART initiation is associated with multiple negative health outcomes including opportunistic infections, cardiovascular kidney, and liver disease, neurologic complications, and malignancy [15]. Timely ART initiation has been associated with multiple positive health effects, such as lower mortality, increased immune functioning, and lower rates of HIV transmission [16]. Among injection drug users (IDUs), excellent adherence to ART is associated with long-term virological response, behavioral support, and provision of opioid agonist treatment [17]. Effective use of ART has been shown to reduce transmission risk from an HIV-infected partner to an HIV-uninfected partner [15].
While there is a fairly large body of research on depression and treatment adherence and/or cessation, relatively little work has been conducted on depression and the initiation of ART. The few studies that have explored ART initiation among patients with depression have produced mixed findings. Some studies have shown that patients with depression were more likely to be put on ART [18], while others showed delayed times and/or decreased rates of initiation [19, 20]. Varying methods for assessment of “psychiatric disorders” (e.g., diagnosis by primary care physicians vs. self-rated scales vs. psychiatrists/psychologists), small cohorts, and different populations may all contribute to these disparate findings in these few studies. There is more consistent evidence in studies that have compared depressed patients who do receive pharmacological treatment for depression compared to those who do not receive treatment. These studies indicate that patients treated for depression are more likely to receive ART than non-treated patients [19, 21]. While this may be a consequence of the beneficial effects of reduced depressive symptoms on ART initiation, it is also possible that such differences could be a function of these patients’ general tendencies to accept and initiate pharmacotherapy for medical conditions.
Although some research suggests that depressive symptoms among HIV patients are associated with decreased rates of ART initiation or delays to initiation when they do begin ART [19, 20, 22, 23], not all studies have identified depression as a statistically significant predictor [24, 25]. Moreover, as Martinez et al. [25] have noted, the majority of these studies were conducted in resource-rich settings where timely ART initiation is the standard of treatment. Very few studies have focused on depressive symptoms and ART initiation in populations outside of the United States.
Understanding factors associated with ART initiation may be particularly useful in locations where ART is not as commonly prescribed. Russia is important in this regard, as it has experienced in the past decade an analogous explosion in HIV infection rates as the United States did in the 1980s. Despite high rates of testing for HIV in the medical system, Russia is among the countries with the lowest ART coverage for those with advanced HIV [26]. The estimate for adult coverage in 2010, based on the 2006 and 2010 WHO guidelines of prescribing ART to those with CD4 <350 was estimated at between 16 and 23 % [26]. Moreover, and consistent with many countries, Russia has not yet implemented optimal public health prevention policies to reduce the spread of the infection [27]. At most recent count, the country had ~1 million HIV-infected people among its population of 140 million [26]. Together with the Ukraine, the two countries represent almost 90 % of newly reported HIV diagnoses in Eastern Europe and Central Asia [26].
Examining this population of IDUs and risky drinkers is of particular importance in the HIV literature. There is considerable documentation that alcohol and drug use are independently associated with increased HIV-risk behaviors [28–30], such as decreased condom utilization [31], lowered perception of risk [30, 32], expectations of enhanced arousal [33], and increased intentions of engaging in risky sexual behaviors [34], transactional sex [35], exposure risk to sexually transmitted infections [36], increased sexual contact with more partners [29], and sharing of needles for drug use [29]. Studies have consistently found an association between risky-drinkers, decreased adherence to ART, and poor HIV treatment outcomes [37]. Many studies also support the correlation between risky drinking and lower utilization of healthcare (defined broadly as hospitalizations, outpatient treatment, emergency room visits, ART utilization, and substance abuse and mental health treatment), though these findings were inconsistent [37].
Despite the importance of better understanding ART initiation in general and in the international setting in which IDUs are the major HIV risk group (the leading five countries: China, Vietnam, Russia, Ukraine, and Malaysia [38]), there is relatively little known about patient factors that predict the initiation of ART. Much of the research that has been conducted on ART initiation has focused on broader system-related factors. A qualitative study that investigated systemic barriers in accessing HIV treatment in Russia highlighted several of these issues, such as “macro-level structural factors” (e.g., adverse impacts of criminalization among IDUs), “meso-level systemic factors” (e.g., no access to opioid agonist treatment), difficult to navigate bureaucratic obstacles in treatment settings, and HIV treatment contingent upon resolved drug use [39].
While these system-related factors are important in initiating ART in IDUs in Russia, the current study sought to better understand the role of patient factors on the initiation of ART. This analysis focused on the impact of depressive symptoms on the initiation of ART among HIV-infected patients. This study investigated the effects of depression using two main indicators. We hypothesized that higher levels of depressive symptom severity would be associated with lower odds of initiation of ART for patients with HIV over the 12 month period of the study, controlling for known risk factors such as injection drug use, heavy drinking, and gender. Both established clinical cutoff scores [40] and severity of Beck Depression Inventory-II (BDI-II) scores were used to examine these hypotheses. Given the concern that assessment of depression may be confounded when there is significant overlap between the medical symptoms and somatic symptoms of depression [41], a secondary analysis was conducted to explore the association between depressive symptoms as indexed by the Cognitive subscale of the BDI-II (an index that excludes somatic symptoms [14]) and ART initiation.
Methods
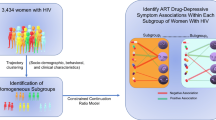
Study Design and Participants
From July 2007 through April 2010, HIV-infected heavy drinkers were recruited from inpatient and outpatient HIV and substance use care sites in St. Petersburg, Russia. These individuals were enrolled in a randomized clinical controlled trial of an HIV secondary prevention intervention (HIVs Evolution in Russia—Mitigating Infection Transmission and Alcoholism in a Growing Epidemic, or the “HERMITAGE” study). At inpatient settings, research associates approached patients, assessed eligibility, offered participation, obtained informed consent and conducted assessments. Subjects recruited from non-clinical sources (i.e., a needle exchange program and via “snowball recruitment”) were given information on the study and referred to one of the enrollment sites for eligibility assessment.
Patients were eligible for inclusion in HERMITAGE if they met the following criteria: 18 years of age or older; HIV-infected; and reported National Institute on Alcohol Abuse and Alcoholism (NIAAA) “at risk” drinking levels in the past 6 months, which we defined as “heavy” drinking. Exclusion criteria included cognitive impairment or acute illness precluding participation, pending legal issues which could lead to incarceration, or ongoing efforts to conceive. For this analysis, only HIV-infected heavy drinkers with CD4 levels <350 cells/μl who were not on ART at baseline were included.
This study used the Russian version of the BDI-II [42], an instrument that assesses depressive symptoms in a manner that is consistent with the diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR [43]). In addition to providing clinical severity cutoff scores, the BDI-II contains subscales to distinguish between cognitive and somatic symptoms of depression which may be particularly useful for specifying depressive symptoms among those with HIV [41].
Procedures
Baseline data were collected via a face-to-face interview with a research associate to gather quantitative data by way of interviewer-administered questionnaires. A portion of the questionnaire was self-administered for particularly sensitive questions (i.e., depression). In addition, chart review was performed to determine CD4 count when available. Interviews were conducted in Russian. Participants were compensated 200 rubles (US$7) for the baseline assessment and 800 rubles (US$28) and 1000 (US$35) at 6- and 12-month visits, respectively. The HERMITAGE study was approved by the Institutional Review Boards of Boston Medical Center and First St. Petersburg Pavlov State Medical University. All data about participants were collected in Russia. Training, adaptation of the protocols, and weekly meetings were conducted in Russia and Boston.
Measures
Independent Variables
BDI-II Scores
The main independent variable for this study was severity of depressive symptoms, based on the BDI-II, categorized as: none, mild, moderate, or severe. At baseline and 6-month visits, participants completed the self-report BDI-II. The questionnaire consists of 21 questions measuring depressive symptoms over the past 2 weeks, including the day the questionnaire was being administered. Respondents were asked to indicate for each item the degree, on a scale of 0–3, to which they experienced a given symptom (e.g., sadness, guilt, worthlessness). Total scores were coded as no depression (BDI-II score 0–13), mild depression (BDI-II score 14–19), moderate depression (BDI-II score 20–28), and severe depression (BDI-II score 29–63) according to the guidelines provided by Beck et al. [40]. The BDI-II also provides subscale scores for cognitive and somatic symptoms. Previous psychometric research on the BDI-II has indicated two highly correlated factors that represent cognitive (e.g., pessimism) and somatic (e.g., loss of appetite) features [43]. The HERMITAGE study used the official Russian version of the BDI-II [42].
Covariates
Gender
As women suffer from clinical depression twice as often as men [44], gender was used as a covariate in the analyses.
Injection Drug Use
At baseline, 6-, and 12-month visits, injection drug use was assessed for the past 30 days using a modified version of the Risk Behavior Survey [45]. The variable was dichotomized for the analyses as no injection drug use in the past 30 days and any injection drug use in the past 30 days.
Alcohol Use
At baseline, 6-, and 12-month visits, heavy drinking was assessed in a semi-structured clinical interview. Patients were first provided with information about how to define a standard drink for different kinds of alcohol. Next, each patient was shown a calendar, and reported the frequency and quantity of alcohol use over the past 30 days in accord with the Alcohol Timeline Followback (TLFB)-30 day [46]. Using the NIAAA standards of at “at risk”, the participant was classified as 0 = not at risk or 1 = heavy drinking. Heavy drinking for males is defined as >14 drinks per week or ≥5 drinks in 1 day [47]. For women, heavy drinking is defined as >7 drinks per week or ≥4 drinks in 1 day [47].
Outcome Measures
Self-report ART Use
Patients were assessed at baseline, 6-, and 12-month visits. At baseline, interviewers asked participants if they had ever been on ART and if they were currently on ART. Participants were asked gain at 6- and 12-months whether they were currently on ART. The primary outcome of this study was self-reported ART use (yes vs. no) at follow-up. At each time point, participants were given a list of all known ART medications with pictures of the pills with corresponding names. Use of pictures is consistent with other studies requiring patients to identify medications [48].
Statistical Analysis
We used descriptive statistics to characterize the study sample at enrollment (e.g., means and standard deviations were obtained for continuous variables and frequencies and proportions were obtained for categorical variables). Known risk factors, such as heavy drinking, injection drug use, and gender were controlled for in all analyses. Preliminary models were fit for 6- and 12-month outcomes separately, and associations were generally consistent over time. The main independent variable, depressive symptoms, was time “lagged” (i.e., BDI-II at one timepoint was used to predict ART initiation at the subsequent interview) in order to ensure it preceded ART initiation. The main analyses addressing the key research question of the study incorporated both the 6- and 12-month outcomes into a single model using generalized estimating equations (GEE) logistic regression models [49] to evaluate the association between depressive symptom severity (at study entry and 6-months) and subsequent ART initiation (at 6- and 12-months, respectively). Participants could contribute to a second observation if they were not on ART at 6 months. The GEE models were fit using a logit link and an independence working correlation matrix. The standard errors reported are based on the empirical variance estimator. If a participant missed the 6-month visit, ART status at the 12-month visit was used as the outcome for the baseline depressive symptom severity status. For the primary analysis, depressive symptom severity was based on clinical severity cutoff scores described above (i.e., none; mild; moderate; severe). Secondary analyses of the cognitive subscale were conducted to supplement the primary analyses. The cognitive subscale scores were categorized into quartiles to avoid assumptions of linearity. To minimize the potential for collinearity, we verified that no pairs of independent variables or covariates were highly correlated (>0.40). Adjusted odds ratios (AORs) and 95 % confidence intervals are reported for each model. All analyses were conducted using two-sided tests and a p value <0.05 was considered statistically significant. To minimize multiple testing, pairwise comparisons were not made unless the global p-value for the BDI-II was statistically significant. All statistical analyses were conducted using SAS version 9.2 [50].
Results
Descriptive Statistics
A total of 700 participants were enrolled in the HERMITAGE study. Of this sample, 133 (19 %) were included in analyses for this study and their characteristics are described in Table 1, both overall and stratified by depressive symptom severity. Of the 700 participants, 30 % were missing CD4 data, 37 % had a CD4 count >350, 8 % were on ART at baseline, and 6 % had no follow-up data. At baseline, the majority of patients (59.4 %) showed some level of depressive symptoms. The proportion with a range of depressive symptoms was as follows: none 40.6 % (n = 54); mild 16.5 % (n = 22); moderate 26.3 % (n = 35); and severe 15.5 % (n = 22). Females comprised 46.6 % of the sample (n = 62) and males 53.4 % (n = 71). The mean age was 29.8 years.
BDI-II Depression Severity Level and ART Initiation
The primary analyses evaluation of the association between BDI-II scores and ART initiation are presented in Table 2. Compared to no depressive symptoms, patients with depressive symptoms appeared to have lower odds of initiating ART (AOR for Mild: 0.86 [95 % CI 0.32, 2.32]; AOR for Moderate: 0.55 [95 % CI 0.21, 1.45]; AOR for Severe: 0.59 [95 % CI 0.21, 1.67]), however the results were not statistically significant (global p-value = 0.58). In secondary analyses, we also examined whether depressive symptoms dichotomized as moderate/severe versus mild/no depression was associated with ART initiation. The results were again suggestive of depressive symptoms reducing the odds of initiating ART (AOR 0.59 [95 % CI 0.27, 1.26]). However, as in the primary analysis, the association was not statistically significant (global p-value = 0.17). A number of covariates were associated with ART initiation. Males (AOR 2.51 [95 % CI 1.19, 5.29]) and those who had previously been on ART prior to enrollment (AOR 4.40 [95 % CI 1.60, 12.11]) had higher odds of initiating ART. Consistent with previous work [19, 51, 52], IDUs had lower odds of initiating ART (AOR 0.26 [95 % CI 0.10, 0.68]). Heavy drinkers also appeared to have lower odds of initiating ART (AOR 0.52 [95 % CI 0.26, 1.04]), however the results did not reach statistical significance.
BDI-II Cognitive Subscale Severity and ART Initiation
Given the overlap between somatic symptoms of depression and HIV symptoms, a number of investigators [14, 41] have suggested that cognitive symptoms of depression may provide a measure of depression for HIV patients that may reduce confounding by disease related symptoms. Thus as a secondary analysis, we examined the association between cognitive depressive symptom severity and outcomes. As shown in Table 3, there was a non-significant trend for higher scores on the BDI-II cognitive subscale to be associated with lower odds of ART initiation in adjusted models (p = 0.05). Compared to those with the least severe cognitive symptoms (i.e., lowest quartile of cognitive subscale), those with the most severe cognitive symptoms (i.e., highest quartile) (AOR 0.25 [95 % CI 0.09, 0.71]) and those in the second quartile (AOR 0.35 [95 % CI 0.13, 0.95]) had lower odds of ART initiation, but not those in the third quartile (AOR 0.55 [95 % CI 0.21, 1.45]). Other factors that were statistically significant in the primary analyses (i.e., male, injection drug use, lifetime ART use) remained statistically significant in this analysis.
Discussion
The current study examined the association between depressive symptom severity and ART initiation among heavy drinking HIV-infected patients in Russia who would be considered eligible for ART (CD4 <350). The primary analyses did not provide evidence that depressive symptom severity had a statistically significant effect on the odds of subsequent ART use. Consistent with previous work on ART initiation [19, 51, 52], injection drug use was associated with lower odds of ART initiation. Moreover, males and individuals that had previously been on ART both had statistically significant higher odds of ART initiation during the study follow-up period.
Although the odds ratios were in the direction of the study’s original hypotheses, other factors such as drug- and heavy alcohol use that are often co-morbid with depressive symptoms appeared to have stronger associations with ART use [53]. Indeed, work has suggested that hazardous drinking may be the predominant factor in determining ART treatment delay in populations that are co-morbid for depressive symptoms [25, 54]. There may be a number of co-occurring factors (e.g., injection drug use, drinking, hesitancy to prescribe due to poor adherence and/or unstable living situations) that may be predictors of ART initiation which may obscure the relative contributions of depressive symptom severity. A potentially important additional factor might be the possibility that depressive symptoms as measured by the full BDI-II may be confounded with symptoms of HIV [41]. There is considerable discussion in the literature about the importance and diagnostic utility of somatic symptoms of depression for medical patients [55], including those with HIV [56]. The secondary analyses of cognitive symptoms provided stronger suggestive evidence for the potential importance of depressive symptom severity in ART initiation.
Though definitive implications of depressive symptoms on ART initiation cannot be derived from the results of this study, there are several outcomes worth discussing. First, while not statistically significant, the results from the analyses of cognitive symptoms of depression were suggestive and deserve further investigation in studies designed for ART initiation as a primary outcome. Next, it appears that in this particular population, other patient factors (i.e., gender, injection drug use, risky drinking) are more influential in delaying ART treatment than depressive symptoms. Moreover, there may be additional factors not addressed in this study that may contribute to delay of treatment. Clearly the role of systemic factors (e.g., access to care) must be included in any comprehensive model of ART initiation predictors. Despite the importance of these additional issues, these results provide initial evidence of the role of depressive symptoms and may contribute to the understanding of ART initiation in HIV-infected populations (e.g., substance users, IDUs, developing countries) that have similar population characteristics to Russia.
This study is not without limitations. This analysis was conducted from the primary study of a randomized controlled trial (HERMITAGE) with individuals who were both eligible and not eligible for ART. Consequently, not all participants enrolled in HERMITAGE were eligible for inclusion in this analysis, and not all participants had CD4 counts available. Despite these limitations, this study enabled an early examination of potential barriers to ART treatment initiation in the international setting with an injection-drug-driven HIV epidemic. Researching ART initiation in this population is critical, as our study demonstrated that IDUs and suggested that heavy drinkers were less likely to initiate ART. As the data also suggested but did not clearly document that depressive symptoms may delay ART initiation, future research should address this more explicitly. As previously mentioned, multiple negative health outcomes are associated with delayed initiation of ART. As such, it is imperative to identify these at-risk populations to find potential targets for increasing initiation rates. Future studies will continue to clarify these barriers, and will facilitate progress towards the goal of optimizing treatment for those in need.
References
Pence BW, O’Donnell JK, Gaynes BN. Falling through the cracks: the gaps between depression prevalence, diagnosis, treatment, and response in HIV care. AIDS. 2012;26(5):656–8.
Eller LS, Bunch EH, Wantland DJ, et al. Prevalence, correlates, and self-management of HIV-related depressive symptoms. AIDS Care. 2010;22(9):1159–70.
Cruess DG, Petitto JM, Leserman J, et al. Depression and HIV infection: impact on immune function and disease progression. CNS Spectr. 2003;8(1):52–8.
Ickovics JR, Hamburger ME, Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV epidemiology research study. JAMA. 2001;285(11):1466–74.
Leserman J, Petitto JM, Golden RN, et al. Impact of stressful life events, depression, social support, coping, and cortisol on progression to AIDS. Am J Psychiatry. 2000;157(8):1221–8.
Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman NM. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the south. Psychosom Med. 2005;67(3):500–7.
Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom Med. 2008;70(5):539–45.
Baum MK, Rafie C, Lai S, Sales S, Page JB, Campa A. Alcohol use accelerates HIV disease progression. AIDS Res Hum Retrovir. 2010;26(5):511–8.
Cook RL, Sereika SM, Hunt SC, Woodward WC, Erlen JA, Conigliaro J. Problem drinking and medication adherence among persons with HIV infection. J Gen Intern Med. 2001;16(2):83–8.
Spies G, Asmal L, Seedat S. Cognitive-behavioural interventions for mood and anxiety disorders in HIV: a systematic review. J Affect Disord. 2013;150(2):171–80.
O’Cleirigh C, Skeer M, Mayer KH, Safren SA. Functional impairment and health care utilization among HIV-infected men who have sex with men: the relationship with depression and post-traumatic stress. J Behav Med. 2009;32(5):466–77.
Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. J Acquir Immune Defic Syndr. 2011;58(2):181–7.
Gore-Felton C, Koopman C. Behavioral mediation of the relationship between psychosocial factors and HIV disease progression. Psychosom Med. 2008;70(5):569–74.
Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psychol. 2012;80(3):404–15.
Department of Health and Human Services. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. http://www.aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf. Accessed 30 Aug 2012.
Holmberg SD, Palella FJ Jr, Lichtenstein KA, Havlir DV. The case for earlier treatment of HIV infection. Clin Infect Dis. 2004;39(11):1699–704.
Spire B, Lucas GM, Carrieri MP. Adherence to HIV treatment among IDUs and the role of opioid substitution treatment OST). Int J Drug Policy. 2007;18(4):262–70.
Himelhoch S, Moore RD, Treisman G, Gebo KA. Does the presence of a current psychiatric disorder in AIDS patients affect the initiation of antiretroviral treatment and duration of therapy? J Acquir Immune Defic Syndr. 2004;37(4):1457–63.
Tegger MK, Crane HM, Tapia KA, Uldall KK, Holte SE, Kitahata MM. The effect of mental illness, substance use, and treatment for depression on the initiation of highly active antiretroviral therapy among HIV-infected individuals. AIDS Patient Care STDS. 2008;22(3):233–43.
Fairfield KM, Libman H, Davis RB, Eisenberg DM. Delays in protease inhibitor use in clinical practice. J Gen Intern Med. 1999;14(7):395–401.
Sambamoorthi U, Walkup J, Olfson M, Crystal S. Antidepressant treatment and health services utilization among HIV-infected Medicaid patients diagnosed with depression. J Gen Intern Med. 2000;15(5):311–20.
Murray LK, Semrau K, McCurley E, et al. Barriers to acceptance and adherence of antiretroviral therapy in urban Zambian women: a qualitative study. AIDS Care. 2009;21(1):78–86.
Kalichman SC, Graham J, Luke W, Austin J. Perceptions of health care among persons living with HIV/AIDS who are not receiving antiretroviral medications. AIDS Patient Care STDS. 2002;16(5):233–40.
Bhatia R, Hartman C, Kallen MA, Graham J, Giordano TP. Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: results from the steps study. AIDS Behav. 2011;15(6):1161–70.
Martinez P, Andia I, Emenyonu N, et al. Alcohol use, depressive symptoms and the receipt of antiretroviral therapy in southwest Uganda. AIDS Behav. 2008;12(4):605–12.
Joint United Nations Programme on HIV/AIDS (UNAIDS). Global report: UNAIDS report on the global AIDS epidemic, 2010. http://www.unaids.org/documents/20101123_GlobalReport_em.pdf. Accessed 30 Aug 2012.
Samet JH. Russia and human immunodeficiency virus—beyond crime and punishment. Addiction. 2011;106(11):1883–5.
Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health. 2010;55(3):159–66.
Drumright LN, Patterson TL, Strathdee SE. Club drugs as causal risk factors for HIV acquisition among men who have sex with men: a review. Subst Use Misuse. 2006;41(10–12):1551–601.
Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. J Stud Alcohol. 2002;63(4):476–85.
Kalichman SC, Simbayi LC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (Shebeens) in Cape Town, South Africa. Prev Sci. 2008;9(1):55–62.
Fromme K, Katz E, D’Amico E. Effects of alcohol intoxication on the perceived consequences of risk taking. Exp Clin Psychopharmacol. 1997;5(1):14–23.
Prause N, Staley C, Finn P. The effects of acute ethanol consumption on sexual response and sexual risk-taking intent. Arch Sex Behav. 2011;40(2):373–84.
George WH, Davis KC, Norris J, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: the roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38(4):498–513.
Safika I, Johnson TP, Levy JA. A venue analysis of predictors of alcohol use prior to sexual intercourse among female sex workers in Senggigi, Indonesia. Int J Drug Policy. 2011;22(1):49–55.
Boden JM, Fergusson DM, Horwood LJ. Alcohol and STI risk: Evidence from a new zealand longitudinal birth cohort. Drug Alcohol Depend. 2011;113(2–3):200–6.
Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–93.
Wolfe D, Carrieri MP, Shepard D. Treatment and care for injecting drug users with HIV infection: a review of barriers and ways forward. Lancet. 2010;37(9738):355–66.
Sarang A, Rhodes T, Sheon N, Page K. Policing drug users in Russia: risk, fear, and structural violence. Subst Use Misuse. 2010;45(6):813–64.
Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory-II. San Antonio: Psychological Corporation; 1996.
Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV/AIDS. J Nerv Ment Dis. 2000;188(10):662–70.
Beck AT. Depression inventory, Beck. Russian translation. Aaron T. Beck: Pearson Education, Inc.; 1996. 2007.
Steer RA, Ball R, Ranieri WF, Beck AT. Dimensions of the beck depression inventory-II in clinically depressed outpatients. J Clin Psychol. 1999;55(1):117–28.
World Health Organization. Gender and women’s mental health. http://www.who.int/mental_health/prevention/genderwomen/en. Accessed 28 March 2013.
Weatherby NL, Needle R, Cesari H, et al. Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach. Eval Program Plann. 1994;17(4):347–55.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported ethanol consumption. Totowa: Humana Press; 1992.
National Institute on Alcohol Abuse and Alcoholism (NIAAA). Moderate & binge drinking. http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed 15 Dec 2012.
Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14(5):267–73.
Diggle P, Liang KY, Zeger SL. Analysis of longitudinal data. New York: Clarendon Press; Oxford University Press; 1995.
SAS Institute Inc. SAS/STAT® 9.2. 2008.
Tran BX, Ohinmaa A, Duong AT, et al. Changes in drug use are associated with health-related quality of life improvements among methadone maintenance patients with HIV/AIDS. Qual Life Res. 2012;21(4):613–23.
Chander G, Himelhoc S, Moore RD. Substance abuse and psychiatric disorders in HIV-positive patients: epidemiology and impact on antiretroviral therapy. Drugs. 2006;66(6):769–89.
Sullivan LE, Saitz R, Cheng DM, Libman H, Nunes D, Samet JH. The impact of alcohol use on depressive symptoms in human immunodeficiency virus-infected patients. Addiction. 2008;103(9):1461–7.
Farley J, Miller E, Zamani A, et al. Screening for hazardous alcohol use and depressive symptomatology among HIV-infected patients in Nigeria: prevalence, predictors, and association with adherence. J Int Assoc Physicians AIDS Care (Chic). 2010;9(4):218–26.
Ferguson CJ, Stanley M, Souchek J, Kunik ME. The utility of somatic symptoms as indicators of depression and anxiety in military veterans with chronic obstructive pulmonary disease. Depress Anxiety. 2006;23(1):42–9.
Basu S, Chwastiak LA, Bruce RD. Clinical management of depression and anxiety in HIV-infected adults. AIDS. 2005;19(18):2057–67.
Acknowledgments
The study was supported by the National Institute on Alcohol Abuse and Alcoholism: R01AA016059, U24AA020778, U24AA020779, and K24AA15674. We appreciate the editorial assistance of Marlene C. Lira and translation service of Laura Wulach in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goodness, T.M., Palfai, T.P., Cheng, D.M. et al. Depressive Symptoms and Antiretroviral Therapy (ART) Initiation Among HIV-Infected Russian Drinkers. AIDS Behav 18, 1085–1093 (2014). https://doi.org/10.1007/s10461-013-0674-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0674-y