Abstract
Female sex workers (FSW) have worse HIV outcomes in part due to lower anti-retroviral therapy (ART) adherence. Substance use and depression are important barriers to ART adherence, yet few studies have assessed these relationships among FSW in longitudinal studies. Cross-Lagged Panel Models and autoregressive mediation analyses assessed substance use (illicit drug use and alcohol use disorders) in relation to ART non-adherence and the mediation role of depressive symptoms among 240 FSW living with HIV in the Dominican Republic. In annual visits (T1, T2, T3), the majority (70%, 66%, and 53%) reported at-risk drinking and 15%, 13% and 9% used illicit drug during the past 6 months. Most FSW (70%, 62% and 46%) had mild-to-severe depression. Illicit drug use predicted later ART non-adherence. This relationship was not mediated via depressive symptoms. Integrated substance use and HIV care interventions are needed to promote ART adherence and viral suppression among FSW.
Resumen
Las trabajadoras sexuales (TRSX) tienen peores resultados de VIH debido en parte a la menor adherencia a la terapia antirretroviral (TAR). El uso de sustancias y la depresión son barreras importantes para la adherencia; sin embargo, pocos estudios longitudinales han evaluado estas relaciones entre las TRSX. Utilizamos modelos de panel y análisis de mediación para evaluar el uso de sustancias en relación a la falta de adherencia al TAR y el papel de mediación de los síntomas depresivos entre 240 TRSX con VIH en la República Dominicana. En visitas anuales (T1, T2, T3), la mayoría (70%, 66%, and 53%) reportó consumo riesgoso de alcohol y 15%, 13% y 9% consumieron alguna droga ilícita durante los últimos 6 meses. La mayoría (70%, 62% y 46%) tenían depresión leve a grave. El uso de drogas ilícitas predijo la falta de adherencia al TAR. Esta relación no fue mediada por síntomas depresivos. Se necesitan intervenciones integradas de atención del VIH y el uso de sustancias para promover la adherencia al TAR y la supresión viral entre TRSX.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, sex workers are disproportionately affected by HIV compared to adult women overall, with FSW experiencing 30 times greater odds of acquiring HIV than the general female population [1, 2]. The prevalence of HIV among cisgender female sex workers (FSW) is 10.4% globally [3]. Antiretroviral therapy (ART) has been proven to be effective in the treatment of HIV [4]. However, the benefits of ART rely on successful engagement in HIV care and adherence to ART [5]. FSW are a highly stigmatized population and FSW living with HIV face multiple structural, psychosocial and individual barriers to engaging in the HIV care cascade [6, 7]. Globally, a prior systematic review found that only 38% of FSW are estimated to have access to ART, and among those, a meta-analysis estimates that 57% are virally suppressed [8]. Two additional studies from Zimbabwe and Cambodia, respectively, found that less than half of FSW were virally suppressed [9, 10].
The prevalence of substance use is disproportionately high among FSW compared to the general population. Globally ~ 75% of FSW used alcohol in the past month [11], and 29% have ever used some illicit drug [12]. In prior research with FSW living with HIV in the Dominican Republic (DR), 54% reported alcohol use in the past week, and 25% reported having ever used illicit drugs [13]. Substance use is known to be an important barrier for optimal adherence to ART among people living with HIV (PLWH). Heavy alcohol use [14] and use of illicit drugs [15] (e.g. marijuana) have been reported to be related to reduced HIV management in PLWH [16]. Limited studies have assessed the relationship between substance use and HIV treatment outcomes among FSW living with HIV. The available literature [13, 17,18,19,20], based mostly on cross-sectional studies [13, 18,19,20], shows that similar to PLWH, alcohol use or illicit drug use are related to decreased ART adherence and lower likelihood of viral suppression in FSW. However, limited research [17] has assessed the relationship between substance use and ART adherence longitudinally. In addition, underlying mechanisms have not been well explored.
FSW also experience a disproportionate burden of mental health problems, e.g. depressive symptoms. Depressive symptoms are another critical barrier to ART adherence for FSW living with HIV [21]. The prevalence of depression is 41.8% among FSW from low and middle-income countries [22]. A review study reported significant interplays between substance use and depressive symptoms among FSW [22]. Substance use may lead to depressive symptoms via its effect on the brain [23]. Substances can lead to an overall reduction in the sensitivity of the brain's dopamine reward system, which has been reported to cause depressive symptoms [24, 25]. Meanwhile, FSW with depressive symptoms may use substances for temporary relief from negative mood [26], similar to the general population. A study among PLWH reported that depression mediated the relationship between alcohol problems and ART adherence [27]. However, again, limited studies have specifically assessed the role of mental health problems on the relationship between substance use and ART adherence in FSW living with HIV.
To address these gaps, we analyzed data from a longitudinal study among FSW living with HIV in the DR, involving three annual assessments. Approximately 90,000 women are estimated to engage in sex work in the DR [28]. Additionally, HIV prevalence among FSW in the DR is up to 6 times higher than the national prevalence [29, 30], making it an important site to study the population of FSW living with HIV. This study aimed to assess longitudinal associations between substance use and ART adherence to explore whether depressive symptoms mediated these relationships. We hypothesized that (1) prior substance use (illicit drug use and at-risk drinking) would predict subsequent ART non-adherence, and that (2) depressive symptoms would mediate the relationship between prior substance use and subsequent ART non-adherence.
Methods
A total sample of 240 cisgender FSW living with HIV in the DR were recruited to participate in a longitudinal observational study, “Stigma, cohesion and HIV outcomes among vulnerable women across epidemic settings.” Recruitment was based largely on an already established cohort of FSW living with HIV in Santo Domingo initiated during the Abriendo Puertas (Opening Doors) intervention [13], with additional recruitment led by peer navigators, key informants, and participants themselves. The eligibility criteria included women ≥ 18 years, with a confirmed HIV-positive diagnosis and who reported exchanging sex for money in the last month.
The study involved three waves (T1, T2 and T3) of annual assessments starting in 2018. Face-to-face survey interviews examined demographic, behavioral and socio-structural factors related to HIV care continuum outcomes. These surveys were interviewer administered with a pre-programmed tablet. Blood draws were also collected at each wave to assess viral suppression. Two hundred and one FSWs participated in data collection at T1, out of which 29 (14%) were lost to follow up at T2. An additional 39 FSW were recruited at T2 to compensate for attrition, resulting in 211 FSW at T2. Out of 211 FSW at T2, 187 FSW (89%) were followed up at T3. A total of 240 FSW participated in at least one assessment, with 162 (67%) having three assessments, 35 (15%) having two assessments and 43 (18%) having one assessment. A comparison of sample characteristics is presented in the supplemental Table 1.
Ethical Considerations
The study was approved by the Institutional Review Boards of the Johns Hopkins Bloomberg School of Public Health in the United States, and the Instituto Dermatológico y Cirugía de la Piel (IDCP) in Santo Domingo, DR. All participants provided oral informed consent prior to being enrolled.
Measures
HIV Outcomes
ART Non-adherence
Adherence to ART was self-reported based on the validated AIDS Clinical Trials Group (ACTG) measure which includes 5 behavioral items including: doses taken/missed over the last 4 days, doses taken/missed over the last weekend, how closely the participant followed the medication schedule, how closely they followed all instructions, and when the last skipped dose occurred [31]. A binary variable was created to indicate whether or not participants reported optimal ART adherence based on each of these items and then a summary score (range 1–5) was created for the 5 items with a higher score indicating greater ART non-adherence.
Viral Suppression
We also assessed the biological outcome of viral suppression, which was used to examine the validity of the self-reported ART non-adherence. One 10 mL tube of EDTA anticoagulated blood for each participant was drawn per study visit for the blood-based assessments. Viral load testing was conducted at the laboratory of La Clínica de la Familia in La Romana, DR, utilizing polymerase chain reaction (PCR) technology with the Roche Amplicor HIV-1 Monitor Test. Viral suppression was coded as ≤ 400 copies/mL and viral non-suppression as > 400 copies/mL.
Predictors (Substance Use)
Illicit Drug Use
Historic (ever) illicit drug use in lifetime was screened across a range of drugs (marijuana, crack, cocaine, heroin by injection, pills (ecstasy) and any other drug). If participants answered “yes”, they were asked about current use (frequency of use in last 6 months). The variable was coded as “yes” or “no” to indicate the use of at least one of these drugs in the last 6 months.
Alcohol Use
The Alcohol Use Disorders Identification Test (AUDIT)-C, developed by the World Health Organization, was used [32]. Questions included two quantity–frequency questions and one binge question with all responses on a five-point Likert scale. Participants were asked, “How often do you have a drink containing alcohol?” Participants reporting lifetime alcohol consumption were asked (1) “how many drinks containing alcohol do you have on a typical day when you are drinking?” and (2) “how often do you have ≥ 6 drinks on one occasion?” A summary score (range 0–12) was created and at-risk drinking was then defined as a score of ≥ 3 out of 12 [33].
Potential Mediator
Depressive Symptoms
Depressive symptoms in the last 2 weeks were assessed with the 9-item Patient Health Questionnaire (PHQ-9) [34]. Cronbach’s alpha was 0.85–0.89 across T1-T3. A summary score (range 0–27) was created and used in analyses with a higher score indicating greater depressive symptoms. We also described mild-severe depression using a cutoff of 5 (≥ 5 vs. 0–4) and moderate-severe depression using a cutoff of 10 (≥ 10 vs. 0–9).
Covariates
FSW self-reported socio-demographic variables, including age in years, level of formal education, relationship status, and monthly income. We included these covariates at T1 in the models. For the 39 participants who were recruited at T2 instead of T1, they had missing values for these covariates at T1. For these participants, we filled in the missing values for demographic covariates with the information at T2 and used T2 age minus 1 year for T1 age.
Data Analyses
Descriptive analyses were conducted for selected sample characteristics at T1. In all the models, ART non-adherence (skewness within 0.74–1.15) and depressive symptoms (skewness within 0.55–1.15) were treated as continuous variables, while substance use (illicit drug use or at-risk drinking) was treated as a binary variable. The percentage of substance use and the average score of depressive symptoms and ART non-adherence were assessed at T1, T2 and T3. To assess whether there was a significant change in the mean score or prevalence over time (T1–T2 and T1–T3), linear mixed models for continuous variables and generalized linear mixed models for binary variables (mixed logit model) were conducted with time as a categorical variable and T1 as a reference. A random intercept at the participant level was used to account for clustering of repeated measures within each participant. Post-hoc estimation assessed changes in T2–T3. To assess the relationship between ART non-adherence and viral suppression, we conducted a generalized linear mixed model with viral suppression as the dependent variable and ART non-adherence at the same assessment as the independent variable, with a random intercept at the participant level.
Cross-lagged panel models (CLPM) examined the relationship of two variables including substance use (either illicit drug use or at-risk drinking), and ART non-adherence over time [35] by estimating the association of the exposure (substance use) at time T-1 on the outcome (ART non-adherence) at subsequent time T; it also allowed the exposure to be affected by the past assessment of the outcome variable. CLPM simultaneously assessed (1) the cross-lagged relationship of substance use assessed in a previous study visit to later ART non-adherence, and the reverse relationship of ART non-adherence in a previous study visit to later substance use, and (2) the autoregressive relationships of the same variable (e.g. substance use or ART non-adherence) on itself over time. Separate models were conducted for illicit drug use and at-risk drinking. The initial CLPM estimated cross-lagged paths freely without constraints. Wald tests then assessed equality of cross-lagged relationships over time and if non-significant, the paths were constrained to be equal over time. Modification index based on the LaGrange Multiplier test was used for model modifications to improve model fit [36]. The models controlled for all of the covariates.
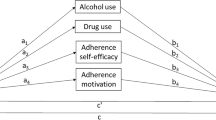
In mediation analysis, the mediation effect can be assessed based on the joint significance of a and b (a*b), where a indicates the relation between X (independent variable) and M (mediator) and b indicates the relation between M (mediator) and Y (dependent variable), controlling for X. The autoregressive mediation model, a longitudinal mediation model, was conducted [37] to assess the mediating role of depressive symptoms (M) in the relationship between substance use (X) and ART non-adherence (Y) over time. X, M and Y were assessed three times over time (X1–X3, M1-M3, Y1–Y3). Antecedent X was used to predict both M and Y in the next assessment, and antecedent M was used to predict Y in the next assessment. As shown in Fig. 2a and b, the mediation model accounts for the autoregressive effect (stability) of X, M and Y over time (sX, sM and sY); three longitudinal mediation effects were assessed: time-ordered mediation (a1*b1), mediation at the first lag (a2*b2), and mediation at the 2nd lag (a1*b2) [37], where a1 and a2 represent the two longitudinal a paths (M2 on X1 and M3 on X2, respectively) and b1 and b2 represent the two longitudinal b paths (Y2 on M1 and Y3 on M2, respectively). For both CLPM and mediation models, Weighted Least Square with means and variances adjusted (WLSMV) was used for estimation and models controlled for all covariates. Model fitness was assessed with a non-significant Chi-square test (X2) test, Comparative Fit Index (CFI) > 0.9, Tucker-Lewis index (TLI) > 0.9, Standardized Root Mean Square Residual (SRMR) < 0.08 and Root Mean Squared Error of Approximation (RMSEA) < 0.08 indicating a good model fit [38]. Mplus 8.2 statistical software was used in these analyses [39].
Out of the 240 participants, 5 participants did not report education (including one who did not report any covariate) at any assessment and were excluded from the CLPM or mediation models. Out of the remaining 235 participants, 196 (83%), 211 (90%) and 182 (77%) participants reported substance use and depressive symptoms, and 185 (79%), 209 (89%), and 178 (76%) participants reported ART non-adherence at T1-T3, respectively. Little’s covariate-dependent missingness (CDM) test supported missing at random (MAR) for substance use, depressive symptoms, and ART non-adherence (X2 = 256.15, df = 365, p = 1.000) [40], conditional on the covariates (age, education, income, and relationship status). WLSMV used the pairwise deletion method to handle missingness in Mplus [41].
Results
Table 1 presents selected sample characteristics. At T1, the mean age of FSW participants was 39.10 years (SD = 9.52), 67% were single, separated, divorced or widowed and 68% had no school or had primary education. Mean annual income was 12,179.6 Dominican pesos (SD = 10,237.02), which is ~ $219 (SD = ~ $184).
The average ART non-adherence score was 1.70 (SD = 1.75), 1.69 (SE = 1.77) and 1.59 (SD = 1.26) at T1, T2 and T3, respectively. There was no significant change over time (b = 0.04, SE = 0.14, p = 0.799 for T1–T2, and b = − 0.11, SE = 0.14, p = 0.439 for T2–T3). The mean score for depressive symptoms was 8.05 (SD = 5.91), 6.84 (SD = 5.30) and 4.59 (SD = 4.80) at T1, T2 and T3, respectively. There was a significant decrease in depressive symptoms between both T1 and T2, and T2 and T3 (b = − 1.22, SE = 0.47, p = 0.009 for T1–T2, b = − 2.25, SE = 0.47, p < 0.001 for T2–T3). An estimated 15%, 13% and 9% of participants used at least one illicit drug at T1, T2 and T3 respectively. There was no significant decrease in illicit drug use based on mixed logit model between T1 and T2 (b = − 0.65, SE = 0.49, p = 0.191), or between T2 and T3 (b = − 0.50, SE = 0.53, p = 0.347), but there was a significant decrease from T1 to T3 (b = − 1.15, SE = 0.55, p = 0.038). An estimated 70%, 66% and 53% of participants reported at-risk drinking during the past 6 months at T1, T2 and T3, respectively. There was a significant decrease in at-risk drinking between T2 and T3 (b = − 0.87, SE = 0.28, p = 0.002), but not between T1 and T2 (b = − 0.21, SE = 0.27, p = 0.435).
There was a significant relationship between ART non-adherence and viral suppression. At T1, T2 and T3, 27%, 24% and 16% of participants were not virally suppressed respectively (Table 1). A one unit increase in ART non-adherence was associated with about a 50% reduced likelihood of viral suppression (crude Odds Ratio, OR 0.51, 95% CI 0.40–0.66, p < 0.001; adjusted OR, aOR 0.53, 95% CI 0.41–0.69, p < 0.001 after adjusting for covariates, supplementary Table 2).
Reciprocal Relationships Between Illicit Drug Use and ART Non-adherence
Wald Chi-square tests for cross-lagged paths were non-significant (X2 = 0.29, df = 1, p = 0.591 for antecedent illicit drug use in relation to later ART non-adherence and X2 = 1.00, df = 1, p = 0.319 for antecedent ART non-adherence on later illicit drug use); thus, they were constrained to be equal over time. The model fits the data well (X2 = 5.17, df = 6, p = 0.522, RMSEA < 0.001, CFI = 1.0, TFL = 1.0, SRMR = 0.019; Fig. 1a). Antecedent illicit drug use was significantly related to subsequent ART non-adherence (standardized regression coefficient β = 0.25, SE = 0.11, p = 0.016 at T1–T2 and β = 0.08, SE = 0.04, p = 0.043 at T2–T3). In contrast, ART non-adherence was not related to subsequent illicit drug use (ps > 0.10). Illicit drug use had strong stability over time (β = 0.82, SE = 0.08, p < 0.001 at T1–T2 and β = 1.00, SE = 0.08, p < 0.001 at T2–T3, respectively). ART-non-adherence had small-to-moderate stability over time at T2–T3 (β = 0.21, SE = 0.08, p = 0.005 at T1–T2, β = 0.29, SE = 0.08, p < 0.001 at T2–T3, respectively). Illicit drug use and ART non-adherence were significantly correlated at T1 (β = 0.35, SE = 0.10, p < 0.001), but not at T2 or T3.
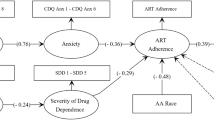
a Cross-lagged panel analysis of illicit drug use and ART non-adherence over time. Note Standardized path coefficients were presented. **p < 0.01. *p ≥ 0.01 and < 0.05. Covariates (age, education, relationship status, income) were included in the model, but not illustrated in the figure. Bolded lines are significant estimates and dashed lines insignificant. Drug: illicit drug use. b Cross-lagged panel analysis on at-risk drinking and ART non-adherence over time. Note Standardized path coefficients were presented. **p < 0.01. *p ≥ 0.01 and < 0.05. Covariates (age, education, relationship status, income) were included in the model, but not illustrated in the figure. Bolded lines are significant estimates and dashed lines insignificant. Alcohol: alcohol use
Reciprocal Relationships Between At-risk Drinking and ART Non-adherence
Based on MI, we included the 2nd order autoregressive relation for at-risk drinking. Wald Chi-square tests for cross-lagged paths were non-significant (X2 = 2.69, df = 1, p = 0.101 for antecedent at-risk drinking in relation to later ART non-adherence and X2 = 0.03, df = 1, p = 0.854 for antecedent ART non-adherence on later at-risk drinking); thus, both were constrained to be equal over time. The model fit the data well (X2 = 5.54, df = 5, p = 0.353, RMSEA = 0.021, CFI = 0.996, TLI = 0.969, SRMR = 0.026; Fig. 1b). At-risk drinking was not significantly related to subsequent ART non-adherence. ART non-adherence was not related to subsequent at-risk drinking (ps > 0.10). At-risk drinking had modest stability at T1–T2 (β = 0.53, SE = 0.11, p < 0.001) and at T1–T3 (β = 0.46, SE = 0.14, p = 0.001), but not at T2-T3. ART non-adherence had small-to-moderate stability over time (β = 0.25, SE = 0.08 p = 0.002 at T1–T2 and β = 0.31, SE = 0.08, ps < 0.001 at T2–T3,). At-risk drinking and ART non-adherence were significantly correlated at T1 (β = 0.24, SE = 0.09, p = 0.007), but not at T2 or T3 (ps > 0.10).
Mediation Effect of Depressive Symptoms on the Relationship Between Illicit Drug Use and ART Non-adherence
The model fit for the autoregressive mediation model [41] that assessed the mediating effect of depressive symptoms on the relation between illicit drug use and ART non-adherence was satisfactory (X2 = 17.69, df = 15, p = 0.280, RMSEA = 0.028, CFI = 0.996, TLI = 0.981, SRMR = 0.026, Fig. 2a). The longitudinal time-ordered mediation was not significant (unstandardized path coefficients a1*b2 = 0.012, SE = 0.014, p = 0.372), nor was the longitudinal mediation at the first lag of T1–T2 (a1*b1 = 0.029, SE = 0.031, p = 0.348) or the 2nd lag of T2–T3 (a2*b2 = 0.002, SE = 0.005, p = 0.618).
a Autoregressive mediation of depressive symptoms on illicit drug use and ART non-adherence over time. Note Standardized path coefficients were presented. **p < 0.01. *p ≥ 0.01 and < 0.05. Covariates (age, education, relationship status, income) were included in the model, but not illustrated in the figure. Bolded lines are significant estimates and dashed lines insignificant. Drug: illicit drug use, Dep: depressive symptoms. sX, sM, and sY indicate autoregressive path estimates for X, M and Y, separately. b Autoregressive mediation of depressive symptoms on at-risk drinking and ART non-adherence over time. Note Standardized path coefficients were presented. **p < 0.01. *p ≥ 0.01 and < 0.05. Covariates (age, education, relationship status, income) were included in the model, but not illustrated in the figure. Bolded lines are significant estimates and dashed lines insignificant. Alcohol: alcohol use, Dep: depressive symptoms. sX, sM, and sY indicate autoregressive path estimates for X, M and Y, separately
Mediation Model Between At-risk Drinking and ART Non-adherence
The initial model fitness was not satisfactory (X2 = 22.58, df = 15, p = 0.094, RMSEA = 0.046, CFI = 0.961, TLI = 0.810, SRMR = 0.038). Based on MI, the path from at-risk drinking at T1 to at-risk drinking at T was included. The model fit was satisfactory (X2 = 13.61, df = 14, p = 0.479, RMSEA < 0.001, CFI = 1.0, TLI = 1.0, SRMR = 0.030, Fig. 2b). The time-ordered mediation of ART non-adherence (T3) on at-risk drinking (T1) via depressive symptoms (T2) was not significant (unstandardized path coefficients a1*b2 = − 0.012, SE = 0.014, p = 0.371, Fig. 2b). The longitudinal mediation at the first time lag of T1-T2 (a1*b1 = − 0.031, SE = 0.032, p = 0.320) or the longitudinal mediation at the 2nd time lag of T2–T3 (a2*b2 = − 0.020, SE = 0.016, p = 0.211) was not significant either.
Discussion
This is one of the first studies to report on temporal relationships between substance use and ART non-adherence using a longitudinal research design among FSW living with HIV. In this sample of FSW living with HIV, we found that (1) illicit drug use predicted subsequent ART non-adherence, and (2) the relationship between illicit drug use or at-risk drinking and subsequent ART non-adherence was not mediated by depressive symptoms.
The findings are consistent with prior research indicating that substance use is a barrier for FSW to engage in optimal HIV treatment as illicit drug use predicted subsequent non-adherence of ART. Although findings did not reach statistical significance, there was a trend in the positive direction for prior at-risk drinking and subsequent ART non-adherence. These findings are consistent with prior research on substance use as a barrier for FSW to engage in HIV treatment. For example, among FSW in Malawi, marijuana use was related to 1.9 times of non-use of ART, and harmful drinking doubled the prevalence of viral non-suppression [18]. Several studies among FSW in the DR have shown that lifetime drug use [19, 20] and drug use before sex [13] were both related to adverse HIV outcomes. Alcohol use was also related to lower ART adherence among FSW in a prospective study in Kenya [17].
This study assessed the mediating effect of depressive symptoms on the relationship between substance use and ART non-adherence. Although there were positive correlations among substance use, depressive symptoms and ART non-adherence at T1, this study did not find that depressive symptoms mediated the relationship between substance use and subsequent ART non-adherence over time, which was contrary to our hypothesis and a cross-sectional study of PLWH [27]. The current study found that depressive symptoms at T1 predicted ART non-adherence at T2 (Fig. 2a, b). This is consistent with a broader body of research on PLWH that suggests that mental health problems are related to difficulties in adhering to HIV treatment as PLWH with mental health problems are more likely to experience fatigue, hopelessness, lower motivation and concentration in terms of adherence to HIV treatment [42,43,44]. It is also consistent with a cross-sectional study that reported that depression was associated with lower ART adherence and viral suppression among FSW living with HIV in the DR as well as in Tanzania [21].
Contradictory to a review study among FSW [22], this study did not find illicit drug use in relation to subsequent depressive symptoms or that depressive symptoms served as a mediator in the relationship between substance use and subsequent ART non-adherence. One possible reason for this might be that depressive symptoms are common in this sample of FSW living with HIV with little variation among participants. It is also possible that depressive symptoms may be an independent risk factor for reduced ART adherence, in addition to substance use. The negative relationship between at-risk drinking at T2 and depressive symptoms at T3 as shown in the mediation model (Fig. 2b) is unexpected and might be explained by the possibility that alcohol acts as a sedative [45, 46] among FSW with mild-severe depression. However, this finding reflects only a one-year period. As reported by other studies, long-term at-risk drinking negatively impacts the health of PLWH [47, 48].
Limitations of this study must be discussed. First, ART non-adherence was self-reported. However, we assessed the relationship between ART non-adherence and viral non-suppression based on objectively measured viral load, and ART non-adherence had predictive validity of viral non-suppression. Second, we had a modest sample size. Future studies need to include a larger sample to repeat these analyses, especially on the relation between at-risk drinking and ART non-adherence. In addition, given that two-thirds of participants had mild-severe depression at T1, the lack of variation in depressive symptoms might also reduce the power to detect the mediation effect of depressive symptoms. These findings among a sample of FSW living with HIV where over half are suffering from mild-severe depression need to be replicated before being generalized to other populations living with HIV. Lastly, although we found a temporal relationship between substance use or depressive symptoms and subsequent ART non-adherence, this finding does not necessarily indicate a causal relationship. Future research might assess these relationships with intensive, short-term diary studies to advance our understanding of the dynamics.
In summary, this study adds to epidemiological evidence based on rigorous longitudinal analyses and contributes to the understanding of ART non-adherence among FSW living with HIV, a multiply marginalized population. Between 16 and 27% of participants were not virally suppressed at each assessment over time. One unit increase in ART non-adherence reduced the likelihood of HIV viral suppression by 50%, underscoring the importance of promoting ART adherence to ensure viral suppression in FSW living with HIV. Findings suggest that it is critical to prevent and treat both substance use and depression among FSW through integrated interventions to improve HIV outcomes in this key population. In addition, more studies need to be conducted to understand the mechanisms underlying prior substance use in relation to later ART non-adherence among FSW living with HIV.
Data Availability
Our manuscript has no associated data or the data will not be deposited due to the sensitive nature of the information they contained.
References
Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet. 2012;12(7):538–49.
UNAIDS. HIV and sex work — Human rights fact sheet series 2021. 2021; https://www.unaids.org/en/resources/documents/2021/05-hiv-human-rights-factsheet-sex-work.
Shannon K, Crago AL, Baral SD, et al. The global response and unmet actions for HIV and sex workers. Lancet (London, England). 2018;392(10148):698–710.
Thompson MA, Aberg JA, Hoy JF, et al. Antiretroviral treatment of adult HIV infection: 2012 recommendations of the International Antiviral Society-USA panel. JAMA. 2012;308(4):387–402.
Atkinson MJ, Petrozzino JJ. An evidence-based review of treatment-related determinants of patients’ nonadherence to HIV medications. AIDS Patient Care STDS. 2009;23(11):903–14.
Mountain E, Pickles M, Mishra S, Vickerman P, Alary M, Boily MC. The HIV care cascade and antiretroviral therapy in female sex workers: implications for HIV prevention. Expert Rev Anti Infect Ther. 2014;12(10):1203–19.
Glick JL, Russo RG, Huang AK, et al. ART uptake and adherence among female sex workers (FSW) globally: a scoping review. Glob Public Health. 2022;17(2):254–84.
Mountain E, Mishra S, Vickerman P, Pickles M, Gilks C, Boily MC. Antiretroviral therapy uptake, attrition, adherence and outcomes among HIV-infected female sex workers: a systematic review and meta-analysis. PLoS ONE. 2014;9(9): e105645.
Muth S, Len A, Evans JL, et al. HIV treatment cascade among female entertainment and sex workers in Cambodia: impact of amphetamine use and an HIV prevention program. Addict Sci Clin Pract. 2017;12(1):20.
Cowan FM, Davey CB, Fearon E, et al. The HIV care cascade among female sex workers in Zimbabwe: results of a population-based survey from the sisters antiretroviral therapy programme for prevention of HIV, an integrated response (SAPPH-IRe) trial. J Acquir Immune Defic Syndr (1999). 2017;74(4):375–82.
Li Q, Li X, Stanton B. Alcohol use among female sex workers and male clients: an integrative review of global literature. Alcohol Alcohol (Oxford, Oxfordshire). 2010;45(2):188–99.
Iversen J, Long P, Lutnick A, Maher L. Patterns and epidemiology of illicit drug use among sex workers globally: a systematic review. In: Goldenberg SM, Morgan Thomas R, Forbes A, Baral S, editors. Sex work, health, and human rights: global inequities, challenges, and opportunities for action. Cham: Springer International Publishing; 2021. p. 95–118.
Kerrigan D, Barrington C, Donastorg Y, Perez M, Galai N. Abriendo puertas: feasibility and effectiveness a multi-level intervention to improve HIV outcomes among female sex workers living with HIV in the Dominican Republic. AIDS Behav. 2016;20(9):1919–27.
Cohen RA, Gullett JM, Porges EC, et al. Heavy alcohol use and age effects on HIV-associated neurocognitive function. Alcohol Clin Exp Res. 2019;43(1):147–57.
Lorkiewicz SA, Ventura AS, Heeren TC, et al. Lifetime marijuana and alcohol use, and cognitive dysfunction in people with human immunodeficiency virus infection. Subst Abuse. 2018;39(1):116–23.
Korthuis PT, Fiellin DA, McGinnis KA, et al. Unhealthy alcohol and illicit drug use are associated with decreased quality of HIV care. J Acquired Immune Defic Syndr (1999). 2012;61(2):171–8.
Long JE, Richardson BA, Wanje G, et al. Alcohol use and viral suppression in HIV-positive Kenyan female sex workers on antiretroviral therapy. PLoS ONE. 2020;15(11): e0242817.
Lancaster KE, Lungu T, Mmodzi P, et al. The association between substance use and sub-optimal HIV treatment engagement among HIV-infected female sex workers in Lilongwe, Malawi. AIDS Care. 2017;29(2):197–203.
Donastorg Y, Barrington C, Perez M, Kerrigan D. Abriendo Puertas: baseline findings from an integrated intervention to promote prevention, treatment and care among FSW living with HIV in the Dominican Republic. PLoS ONE. 2014;9(2): e88157.
Zulliger R, Barrington C, Donastorg Y, Perez M, Kerrigan D. High drop-off Along the HIV Care Continuum and ART interruption among female sex workers in the Dominican Republic. J Acquir Immune Defic Syndr. 2015;69(2):216–22.
Kerrigan D, Karver TS, Barrington C, et al. Mindfulness, mental health and HIV outcomes among female sex workers in the Dominican Republic and Tanzania. AIDS Behav. 2021;25:2941–50.
Beattie TS, Smilenova B, Krishnaratne S, Mazzuca A. Mental health problems among female sex workers in low- and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2020;17(9): e1003297.
Volkow ND, Michaelides M, Baler R. The neuroscience of drug reward and addiction. Physiol Rev. 2019;99(4):2115–40.
LeGates TA, Kvarta MD, Tooley JR, et al. Reward behaviour is regulated by the strength of hippocampus-nucleus accumbens synapses. Nature. 2018;564(7735):258–62.
Xu L, Nan J, Lan Y. The nucleus accumbens: a common target in the comorbidity of depression and addiction. Front Neural Circ. 2020. https://doi.org/10.3389/fncir.2020.00037.
Turner S, Mota N, Bolton J, Sareen J. Self-medication with alcohol or drugs for mood and anxiety disorders: a narrative review of the epidemiological literature. Depress Anxiety. 2018;35(9):851–60.
Malow R, Dévieux JG, Stein JA, et al. Depression, substance abuse and other contextual predictors of adherence to antiretroviral therapy (ART) among Haitians. AIDS Behav. 2013;17(4):1221–30.
Kerrigan D, Ellen JM, Moreno L, et al. Environmental-structural factors significantly associated with consistent condom use among female sex workers in the Dominican Republic. AIDS (London, England). 2003;17(3):415–23.
Rojas P, Malow R, Ruffin B, Rothe EM, Rosenberg R. The HIV/AIDS epidemic in the Dominican Republic: key contributing factors. J Int Assoc Phys AIDS Care. 2011;10(5):306–15.
Department of State. PEPFAR: U.S. President's Emergency Plan for AIDS Relief: Dominican Republic Country Operational Plan COP2020 Strategica Direction Summary. 2020; https://www.state.gov/wp-content/uploads/2020/07/COP-2020-Dominican-Republic-with-Appendix-C.pdf. Accessed 4 Dec 2021.
Fletcher CV, Testa MA, Brundage RC, et al. Four measures of antiretroviral medication adherence and virologic response in AIDS clinical trials group study. J Acquir Immune Defic Syndr. 2005;40(3):301–6.
Surah S, Kieran J, O’Dea S, et al. Use of the Alcohol Use Disorders Identification Test (AUDIT) to determine the prevalence of alcohol misuse among HIV-infected individuals. Int J STD AIDS. 2013;24(7):517–21.
Gordon AJ, Conigliaro J, Fielin DA. Selective methods used in alcohol research: screening in primary care methods and approaches. In: Victor R, Preedy RRW, editors. Comprehensive handbook of alcohol related pathology. Boca Raton: Academic Press; 2005.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Newsom JT. Cross-lagged panel analysis. In: Whitbourne SK, editor. The encyclopedia of adulthood and aging. Wiley: Hoboken; 2015. p. 1–6.
Chou C-P, Huh J. Model modification in structural equation modeling. 2012.
MacKinnon DP. Introduction to statistical mediation analysis. New York: Erlbaum; 2008.
Kline RB. Principles and practice of structural equation modeling; 2005.
Muthén LK, Muthén BO. Mplus User's Guide. Eighth Edition ed. Los Angeles1998–2017.
Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–202.
Muthén LK, Muthén BO. Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén 1998–2012.
Wagner GJ, Goggin K, Remien RH, et al. A closer look at depression and its relationship to HIV antiretroviral adherence. Ann Behav Med. 2011;42(3):352–60.
Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep. 2014;11(3):291–307.
Asrat B, Lund C, Ambaw F, Garman EC, Schneider M. Major depressive disorder and its association with adherence to antiretroviral therapy and quality of life: cross-sectional survey of people living with HIV/AIDS in Northwest Ethiopia. BMC Psychiatry. 2020;20(1):462.
Hendler RA, Ramchandani VA, Gilman J, Hommer DW. Stimulant and sedative effects of alcohol. Curr Top Behav Neurosci. 2013;13:489–509.
Chung T, Martin CS. Subjective stimulant and sedative effects of alcohol during early drinking experiences predict alcohol involvement in treated adolescents. J Stud Alcohol Drugs. 2009;70(5):660–7.
Vagenas P, Azar MM, Copenhaver MM, Springer SA, Molina PE, Altice FL. The impact of alcohol use and related disorders on the HIV continuum of care: a systematic review: alcohol and the HIV Continuum of Care. Curr HIV/AIDS Rep. 2015;12(4):421–36.
Edelman EJ, Williams EC, Marshall BDL. Addressing unhealthy alcohol use among people living with HIV: recent advances and research directions. Curr Opin Infect Dis. 2018;31(1):1–7.
Funding
This study was supported with an R01 Grant awarded by the U.S. National Institute of Mental Health (R01MH110158, PI: D. Kerrigan) and a pilot award (PI: Y. Wang) awarded by the District of Columbia Center for AIDS Research, an NIH funded program (P30AI117970) supported by NIAID, NCI, NICHD, NHLBI, NIDA, NIMH, NIA, NIDDK, NIMHD, NIDCR, NINR, FIC and OAR.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study. Conceptualization: YW, DK, CB. Methodology: YW, DK, CB. CB, NG, WD. Data collection: YD, MP, HG. Data analysis: YW. Data management: TK. The first draft of the manuscript was written by YW and all authors (YW, TK, CB, CB, YD, MP, HG, WD, NG, DK) contributed to interpretations of the results and provided comments on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interests to declare.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the following Institutional Review Boards: Johns Hopkins University Bloomberg School of Public Health (IRB No. 7065/CR662), and the Instituto Dermatológico y Cirugía de la Piel (IDCP) in Santo Domingo, DR. All participants provided oral informed consent prior to being enrolled. Informed consent was reviewed with participants during each data collection activity.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Karver, T.S., Berg, C.J. et al. Substance Use and Depression Impede ART Adherence Among Female Sex Workers Living with HIV in the Dominican Republic. AIDS Behav 27, 2079–2088 (2023). https://doi.org/10.1007/s10461-022-03940-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03940-x