Abstract
In addition to personal and psychological factors, structural factors may reduce the likelihood of optimal adherence to antiretroviral therapy (ART) among persons living with HIV. In this mixed-method study we report on the development of a scale to assess the salience of various structural barriers to ART adherence. After following conventional guidelines for scale development, two scales measuring structural barriers to adherence to clinic attendance and pill-taking were administered to 291 patients receiving ART at a public hospital in South Africa. Both exploratory and higher order factor analysis indicated that a single underlying general factor was appropriate for both scales. The final scales consisted of 12 items for the structural barriers to clinic attendance scale and 13 items for the structural barriers to medication-taking scale. Both scales displayed excellent internal consistency with Cronbach alpha coefficients above 0.80. Research to determine the construct validity of the scales may be a next step in this line of research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the beginning of the pandemic in the early 1980s, HIV has spread to almost 60 million people worldwide, with an estimated 25 million having died from HIV-related causes [1]. In 2009, an estimated 5.7 million people were living with HIV in South Africa, making it the largest population of person’s living with HIV (PLWH) worldwide [1]. Antiretroviral therapy (ART) remains the only treatment available for PLWH, and the success of ART in treating HIV/AIDS has rendered the disease as no longer life-threatening but a chronic and manageable condition [2]. Optimal adherence to ART is necessary for positive treatment outcomes, including a high CD4 count and low viral load. However, adherence for some patients may be suboptimal due to various psychological and structural barriers [3].
Considerable research has been directed at individual-level barriers to adherence to ART. In particular, individual factors such as depression [4], emotional distress [5], health literacy [6], forgetfulness [3], substance abuse [5, 7, 8], low self-efficacy [9], and fear of disclosure [10] have been associated with suboptimal medication adherence. Despite a steadily emerging literature, structural barriers to adherence have received much less attention. Shriver et al. [11] have defined structural factors as broad-based forms of social construction which include legal, political and environmental factors that act as barriers or facilitators to peoples’ actions. Kagee et al. [12] have divided structural barriers into three main groups, namely, (a) institution-related factors, (b) poverty-related factors and (c) culturally and politically-related factors [12].
Institution-related factors concern the influence of the healthcare environment on patients’ regular clinic visits. In the context of large patient numbers attending clinics, a lack of privacy at the clinics during consultations [13] and long waiting times [13–17] have been identified as barriers to clinic attendance. Moreover, many patients have reported a reluctance to attend clinic appointments due to their experience of nurses as unsympathetic or impatient [18, 19]. Yet, in the context of an overwhelming number of patients, low rates of remuneration, and difficult working conditions, burn-out and overwork are common among nurses [18, 20–22].
In terms of poverty-related factors, common barriers include difficulty with transport, i.e. insufficient funds to travel to clinics or the unavailability of public transport [15, 23–25], and food insecurity, i.e. not having the necessary foods to take with antiretrovirals (ARVs) [16, 26, 27].
Cultural and political-related factors that impede optimal adherence include HIV-related stigmatization that forces patients to hide their medication and attend clinics far from their homes to avoid detection by others [13, 28, 29]. Migration to other regional areas may also result in patients being lost to follow-up [13, 14]. In addition, some patients have reported that local charismatic church leaders, who wield considerable influence in many communities, have encouraged them to forgo biomedical treatment in favour of prayer [13, 14]. There is a growing literature on structural factors which, combined with individual factors, may yield suboptimal rates of adherence in many resource-constrained contexts.
The present study builds on previous research [13, 14, 30] which collectively formed Phase 1 of this research. Phase 1 qualitatively identified structural barriers to adherence from the perspectives of health professionals, patients, and patient advocates (PAs). The study represents an effort to quantify these barriers systematically by constructing two scales that measure the most salient structural barriers to adherence to clinic attendance and medication-taking that ART users face. As this research forms a continuation of our work on identifying and addressing structural barriers to adherence to ART, we have described the work presented in this paper as Phase 2. The different phases are discussed in the methods section below.
Methods
The study was a mixed-method design with the purpose of constructing two scales aimed at identifying the most salient structural barriers to adherence to clinic attendance and medication-taking endorsed by the sample. A secondary aim of the study was to identify the underlying factor structure of these scales. The study builds on previous research [13, 14, 30] that collectively formed Phase 1. In Phase 1 we conducted in-depth qualitative interviews with ART users, doctors, nurses from a primary health care clinic and focus groups with PAs working at a non-governmental organisation that provides psychosocial support to ART users. The purpose of the interviews and focus groups was to gain an in-depth understanding of the chief structural barriers to ART adherence from the perspective of various role players [13, 14, 30]. The resulting data provided a composite list of the main structural problems that patients experienced in terms of clinic attendance and medication-taking.
In Phase 2, traditional guidelines in scale development [31] were followed. We conceptualised structural barriers at two levels, namely, barriers to clinic attendance and barriers to medication-taking, resulting in two corresponding scales. The items were constructed so that each respondent used him or herself as the anchoring agent, e.g. “I do not attend my clinic appointments because…”, and “I do not take my ART pills because…”. Each scale asked participants to endorse the extent to which the structural barrier applied to them on a 5-point Likert scale. Items were reviewed by an expert in scale development and a clinical researcher who had conducted previous research with ART users for clarity, conciseness, relevance, and possible omissions. Based on these expert reviews, redundant, lengthy, double-barrelled, and ambiguous items and those exceeding an acceptable reading level were adapted or discarded. This method of scale development has gained acceptance as a means of investigating the cultural manifestations of psychiatric problems [32]. Each of the scales was translated from English into Afrikaans, back-translated into English, after which the two English translations were compared. The measures were then administered to a larger sample in the form of a paper and pencil test.
Study Participants and Procedures
A convenience sample of 291 South African ART users was recruited in the study. Fifteen PAs working at a non-governmental organization were approached and asked to assist in data collection. The PAs role was to provide psychosocial support and care to patients receiving ART from both a hospital and primary health care clinic in the area where the study was conducted. A member of the research team (BC) met with the PAs on two occasions to explain the study, trained them in obtaining informed consent and questionnaire administration. PAs also received flyers and were asked to hand these to patients to invite them to participate in the study. Each of the 15 PAs received 20 copies of the questionnaire package to administer to their patients during a routine home-based or clinic visit. The questionnaire packages were available in English and Afrikaans and the consent forms were available in these languages as well as Xhosa, which is commonly spoken in the Western Cape province of South Africa where the study was conducted. Upon completion of the self-report questionnaire package, patients and PAs received a grocery voucher valued at $2.50 and $6.25, respectively, as a token of gratitude for participation and assistance in the study. Ethical approval was received from the Health Research Ethics Committee of the Stellenbosch University and permission to conduct the study was obtained from the Western Cape Department of Health and the City of Cape Town Department of Health.
Measuring Instruments
Demographic Information
A self-administered questionnaire assessed demographic information such as age, gender, marital status, living situation, highest level of education, employment status, annual income and language.
Structural Barriers to Clinic Attendance
The SBCA scale asks ART users to identify the extent to which each structural barriers to clinic attendance applies to their own circumstances. A Likert scale ranging from 1 to 5 was provided where 1 indicated “Never”, 2 indicated “rarely”, 3 indicated “some of the time”, 4 indicated “most of the time”, and 5 indicated “always”. The scale contains a total of 12 items.
Structural Barriers to Medication-taking
The SBMT asks ART users to identify the extent to which each structural barriers to medication-taking applies to their own circumstances. A Likert scale ranging from 1 to 5 was provided where 1 indicated “Never”, 2 indicated “rarely”, 3 indicated “some of the time” 4, indicated “most of the time”, and 5 indicated “always”. The scale contains 13 items.
Data Management and Analysis
Missing data were randomly distributed in the dataset and thus not replaced with mean or regression substitution. Listwise deletion of missing cases was selected for the psychometric analyses. Listwise deletion involves the removal of an entire case, should there be any missing data for a particular participant. Brief descriptive statistics including age, gender, marital status, living situation, highest level of education, employment status, annual income and language were computed to describe the sample. The scales were only available in English and Afrikaans, and thus an analysis of variance (ANOVA) was computed to see whether completing the scale in a language other than the respondent's first language had any significant effect on the way in which items were answered compared to those who did complete the scale in their first language. Principal components exploratory factor analysis (FA), with direct oblimin rotation, was conducted on both the SBCA and SBMT scales in order to identify the underlying factor structure of each. Only items with inter-correlations <0.80 were included exploratory factor analysis (EFA). Factors were extracted based on the scree plot and eigenvalues >1. A factor loading of .40 or greater was used to identify the primary factors on which the items loaded for each scale. EFA was selected because it does not impose a specific pattern on the data in an a priori manner. Instead, it provides an opportunity to identify a factor structure without any assumptive constraints. This approach determines whether a factor’s inclusion substantially clarifies interpretation of the data rather than whether the overall model fits better when a given factor is included rather than excluded as is the case in confirmatory FA [33]. EFA was warranted in this study as no previous research has examined the factor structure of structural barriers to ART adherence. The pattern matrix correlations between first-order factors (factors from the EFA) were subjected to a Schmid–Leiman Solution and transformed to a hierarchical structure where all the factors at all levels of the factor hierarchy are uncorrelated [34] thus producing a single higher order (or general) factor and three group or primary factors. This transformation allows for a clear evaluation of the relative influences of factors at different levels of the factor hierarchy [35]. We also computed an item-by-item descriptive analyses of the two scales; internal consistency of the scales using Cronbach’s alpha; item-total correlations; and Pearson’s product moment correlation coefficients (r) to determine the magnitude of the correlations between the total scores of the SBCA scale and the SBMT scale. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS).
Results
Description of the Sample
As can be seen in Table 1, the sample consisted of 291 participants. Of the 291 who participated, only 289 ticked the appropriate “gender” box on the demographics form. Based on this, 63.9 % of the sample was female and 35.4 % male. The mean age of the sample was 35 years (SD = 9.05). A large proportion of the sample was single (69.4 %) and 38.5 % of the sample reported living with other adults and children. Most of the participants indicated they were unemployed (59.8 %). Almost half (44.3 %) of the sample had attended high school but did not complete Grade 12. The majority of participants (59.1 %) reported Xhosa as their first language while for the rest it was English, Afrikaans or other. An ANOVA was conducted to test whether there were any significant differences in mean responses between those who answered in their first language and those who did not. ANOVA revealed no significant differences in the responses based on first language on either of the scales; F(4, 256) = 1.673, p > 0.05 for the SBCA, and F(4, 256) = 1.073, p > 0.05 for the SBMT. Therefore, despite the majority of participants not responding to the scales in their first language, it did not appear to influence the way in which items were answered.
Exploratory FA (EFA)
Structural Barriers to Clinic Attendance scale (SBCA)
On the first iteration of the EFA, inspection of the correlation matrix (R-matrix) yielded high correlations (r > 0.8) between two pairs of items, suggesting that one was redundant. On removal of this item, the EFA was then performed again. None of the inter-item correlations were above 0.80. The determinant was 0.001 which was greater than 0.00001, thus indicating that multicollinearity was not a problem [36].
The Kaiser–Meyer–Olkin Measure of Sampling Adequacy (KMO) value was 0.83, a value close to 1.00, which indicated that FA was a suitable method of analysis [36]. Bartlett’s test of sphericity was significant (p < 0.01), suggesting that the correlation matrix was significantly different from an identity matrix. This finding indicated that the items correlated with one another, making the possibility of finding factors more likely [36].
Primary Factor Structure
After the principal-components EFA was conducted, a total of three primary factors (based on the scree plot and eigenvalues >1 [37]) were extracted, accounting for 69.17 % of the total variance among the items. The pattern matrix correlations between these factors then formed the input data of the higher-order FA.
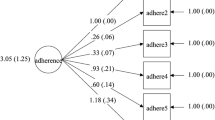
Higher Order Factor Structure
A hierarchical transformation [34] was performed to identify whether the items loaded strongly onto a higher order (or general) factor. As can be seen from Table 2 below, the items indeed loaded saliently onto a higher order factor, which we named structural barriers to Clinic Attendance. Thus, although three primary factors were identified, the results in Table 2 show that 63.2 % of the variance was explained by the higher order factor alone. This is proportionally much more than the variance explained by the three primary factors. On the basis of these results it may be concluded that the SBCA scale may be treated as a unidimensional scale, thus validating the calculation of a total score, with a minimum of 12 and a maximum of 60. A total score that exceeds 30 on this scale thus suggests that multiple barriers to clinic attendance were experienced. The mean score for this scale was 30.84, suggesting that on average participants experienced multiple barriers to clinic attendance.
Internal Consistency of the SBCA
The SBCA showed highly satisfactory reliability (internal consistency) (α = 0.89). Table 3 below shows the item-by-item descriptive analyses for the scale and provides further evidence for the homogeneity of the scale. Table 3 also includes the mean responses of each item on the SBCA scale. From this table it is clear that items 3 (M = 2.8; SD = 1.55), 4 (M = 2.99; SD = 1.48) and 11 (M = 2.98; SD = 1.56) were endorsed to a higher extent than the other items on the scale. These items assess not being able to attend clinic appointments due to the amount of time spent travelling to the clinic, the fear of being identified as HIV positive by community members, and having to wait for several hours to receive clinical attention due to the overcrowded nature of the clinic.
Structural Barriers to Medication-taking (SBMT)
On the first iteration of the analysis, an inspection of the correlation matrix revealed a high correlation (r > 0.80) between two items. The redundant item was deleted and inspection of the correlation matrix showed no high correlations with a satisfactory determinant (0.002) [36]. However the pattern matrix revealed that one item did not load onto either of the two factors extracted from the EFA. This item (“I have difficulty obtaining my ART pills because the clinic is often out of stock of pills”) was subsequently removed. The EFA was then performed again. The KMO statistic was 0.86, which indicated that FA was a suitable analysis for the data. Bartlett’s Test of Sphericity indicated that the correlation matrix was significantly different from the identity matrix (p < 0.01).
Primary Factor Structure
Three primary factors were extracted based on the scree plot and eigenvalues >1 [37], which accounted for 64.03 % of the total variance explained. The pattern matrix correlations between these factors then formed part of the higher order FA to identify a higher order factor.
Higher Order Factor Structure
A hierarchical transformation [34] was performed to identify whether the items loaded strongly onto the higher order factor. As can be seen from Table 4 below, the items indeed loaded saliently onto a higher order factor, which was named structural barriers to Medication-Taking. Thus, although three primary factors were identified, the results in Table 4 show that 57.7 % of the variance was explained by the higher order factor, which is proportionally greater than the variance explained by the primary factors. On the basis of these results, it may therefore be concluded that the SBMT can be treated as a unidimensional scale, which validates the calculation of a total score. A maximum score of 65 and a minimum score of 12 may be obtained on the SBMT. The mean score for this scale was 32.39, suggesting that, on average, a number of patients who completed the scale experienced structural barriers to medication-taking as salient “some of the time”.
The SBMT scale showed highly satisfactory internal consistency reliability (α = 0.87). Table 5 below shows the item-by-item descriptive analyses for the scale and provides further evidence for the homogeneity of the scale. Table 5 displays the mean responses of each item on the SBMT scale. It is apparent that items 1 (M = 3.18; SD = 1.30), 2 (M = 3.49; SD = 1.37), 3 (M = 3.03; SD = 1.36) and 11 (M = 3.09; SD = 1.38) were endorsed to a higher extent than the other items on the scale. These items refer to food insecurity, side effects of the pills, and stigma.
We found a modest correlation (shown in Table 6) between the SBCA and SBMT scales (r = 0.327, p < 0.01), suggesting that barriers to medication-taking were somewhat related to barriers to clinic attendance.
Discussion
To our knowledge this is the first study to focus on identifying the underlying factor structure of scales to assess structural barriers to adherence to ART in terms of clinic attendance and medication-taking. Furthermore, the incorporation of qualitative data gathered from in-depth interviews (phase 1) with key stakeholders (patients, healthcare workers and PAs) presented a unique platform on which to build on the limited literature in this area.
The main objective of this study was to construct two measures to determine the extent to which ART users experienced structural barriers to clinic attendance and medication-taking as salient and to determine the factor structure for each measure. The results indicated that both scales have excellent internal consistency. Following principal-components exploratory FA, it appeared that a factor solution of three factors for the SBCA and three factors for the SBMT provided the best overall fit for the items included in the scales. However, following a higher order FA [34], it was clear that the responses to the items included in each of the scales were dominated by a higher order or general factor, indicating unidimensionality. This finding suggests that a single higher order factor drives the performance of the items on the scale, which in turn justifies the calculation of a total score for each of the scales [35].
Structural Barriers to Clinic Attendance
A total of 12 items loaded strongly onto the factor structural barriers to clinic attendance. Three of these items pertain to the transport difficulties experienced by patients when attending their clinic appointments. The nine other items relate to the patients’ experiences at the clinic itself in relation to the patient-provider relationship, waiting times, and overcrowding at the clinics, as well as a fear of being identified as HIV positive by others. As can be seen from Table 3, items 3 (“I do not attend my clinic appointments because it takes too much time to travel to and from the clinic”), 4 (“I do not attend my clinic appointments because I do not want to be identified as HIV positive)” and 11 (“I do not attend my clinic appointments because the clinic is too crowded)” were the most highly endorsed by a number of participants in this sample suggesting that issues of travelling to the clinic, stigma and overcrowding at the clinic posed as salient structural barriers to clinic attendance. These findings relate to other studies that have reported on barriers to clinic attendance. For example, several authors have reported that travelling long distances on a frequent basis acts as a barrier to clinic attendance [7, 13, 23, 24, 38, 39]. Given the location of the study, most participants resided in a resource-constrained environment characterised by inadequate roads, a lack of sufficient public transport and under-resourced public facilities which were likely to influence their clinic attendance. On the other hand, Falagas et al. [40] systematically reviewed 17 studies (nine longitudinal studies and eight cross-sectional studies) on the association between socio-economic status and adherence to ART. These authors found that only two out of the eight cross-sectional studies identified a low socioeconomic status as a predictor of non-adherence, suggesting a variable relationship between SES and adherence. Indeed, Nguyen et al. [41] has marshalled the concept of therapeutic citizenship to describe the way in which people living with HIV appropriate their treatment at times when they need to negotiate social needs and cultural norms in the face of limited financial support i.e. negotiate these at times conflicting moral economies. It is likely that the association between poverty and adherence may vary depending on specific circumstances that characterise community life where ART users reside.
Furthermore, several authors have reported on the extent to which stigma poses as a barrier to clinic attendance. For example, Coetzee et al. [13] reported that several patients in their sample stated that they sought health services for HIV outside of their neighbourhoods out of fear of being identified as HIV positive. In their study on perceived HIV-related stigma and disclosure following an HIV positive diagnosis, Derlega et al. [29] found that persons with an HIV diagnosis feared being identified as such as they believed it would lead to rejection by community members and threats to the security of family members or partners. Rintamaki et al’s [42] model of stigma concerns argues that perceptions of others’ attitudes towards HIV may produce anxiety in the ART user, precipitating dilemmas in which the importance of adherence to clinic attendance is weighed against others potentially learning about their status.
In accordance with our findings, several other authors have reported overcrowding at public health care facilities as a barrier to clinic attendance [3, 13, 15, 43]. The numbers of patients seeking ART at South African public health care clinics has increased dramatically since the national rollout in 2004 with almost 1.79 million patients currently enrolled [44]. With large numbers of patients seeking ART services at public healthcare facilities [45], patients have been forced to spend many hours waiting for a consultation. In the context of unemployment some patients are reluctant to forgo a day’s wage and spend such long hours at the clinics [13, 14].
Patients typically had little control over the above mentioned barriers. Therefore, it is possible that patients who succeeded in attending clinic appointments were motivated to negotiate and overcome these barriers despite the expected inconveniences.
Structural Barriers to Medication-taking
Thirteen items loaded strongly onto the factor structural barriers to medication-taking. The items assessed barriers such as requiring the necessary foods with which to take the pills, having no access to reminders to take their medication, not wishing to take pills in front of others, and being discouraged to adhere to medication by church leaders. As with the previous scale, decisions to either adhere to or forgo medication-taking may be based on many factors such as personal experience, available information, the experience of others, and beliefs about the effectiveness of the medication itself [46]. According to Remien et al. [46] medication-taking behaviour is affected by emotional, behavioural, and cognitive factors and is not a one-dimensional or static behaviour. Therefore, depending on the circumstances in which an individual finds him or herself, adherence levels may vary depending on circumstances at different points in the person’s life. Remien et al. refer to the impact of individual characteristics of a patient that are likely to affect medication-taking behaviour and thus describe it as multi-dimensional. Medication-taking behaviour should not be confused with our scale that measures structural barriers to medication-taking as one-dimensional.
Means of descriptive statistics of the items (as can be seen from Table 5) showed that items 1 (I have difficulty taking my ART pills because I do not always have food with which to take them), 2 (Taking my ART pills when I do not have food to eat makes me feel ill), 3 (I do not take my pills if I have to take it in front of others), and 11 (I do not take my ART pills because I cannot afford the food I need to eat when I take them) were most strongly endorsed by the sample. These findings are similar to those of previous findings. For example, items 1 and 2 relate to food insecurity, a major consequence of poverty, and thus a defining feature of resource-constrained environments [27, 47]. Qualitative research among African samples has indicated that ART users are reluctant to take their medications when no food is available due to unpleasant side effects such as headaches, stomach pain, dizziness, shivers or tremors, loss of energy, fainting, sweating, and rapid heartbeat [13, 27]. ART is known to reduce nutrient absorption and patients therefore require foods that are rich in nutritional value [27]. When assessed at 6 and 12 month intervals, patients enrolled on an HIV-program at a clinic in Haiti who had access to food showed improved adherence to clinic appointments [48]. However, patients living in resource-constrained settings may not often have the finances to acquire even basic foods. As shown by Weiser et al ART users in their study considered skipping doses or not commencing treatment at all if they were unable to afford sufficient nutritious food.
The item “I do not take my pills if I have to take it in front of others” was endorsed by the majority of the sample, indicating concerns with being identified as HIV positive. The item “I do not take my ART pills in case my CD4 count increases and I may no longer qualify for a disability grant” had the lowest mean (M = 1.62) of all the items. Despite the fact that this barrier was cited by PAs in a qualitative study by Coetzee et al. [13] and has been addressed by other authors, it did not emerge as a major barrier to adherence among the sample.
Limitations of the Study
The present study is characterised by a few limitations. First, despite the utility of the data we obtained, a limitation of the study was that the instruments were not translated into Xhosa, thus limiting first language Xhosa ART users from completing the scales in their mother tongue. We therefore acknowledge that to some extent, the comprehension of items may have been limited. However, ANOVA yielded non-significant differences between participants who completed the questionnaires in their mother tongue and those who did not. Second, recruitment of the sample was conducted with the assistance of PAs, which may have led to sample bias. Serious defaulters, for whom the barriers may have been highly salient, would not have been recruited by this method as they may not have even have had a relationship with a PA. Future research may utilise an alternative method of sampling as a comparison. Third, the number of items in each of the questionnaire packages may have led to respondent fatigue, resulting in either incomplete questionnaires or uniform response sets, evident in some of the completed questionnaires. Fourth, PAs assisted some patients in completing the instruments, thus raising the possibility that the results may have been influenced by social desirability. Finally, participants were not given a time frame on which to base their behaviour, for example, asking them to base their responses on their adherence in the last month. Such a time dimension may have provided a clearer picture about the time specificity of the barriers endorsed.
Conclusion
This research is among the first to identify and assess structural barriers to adherence in a resource-constrained context. It represents the beginning of an approach to quantify the salience of such barriers for individual patients. Future research may determine the utility of the two scales in identifying ART users at risk of defaulting on their treatment with a view to intervening early so as to assist them in negotiating or overcoming structural barriers.
References
Joint United Nations Programme on HIV/AIDS. Global Report: UNAIDS report on the global AIDS epidemic. 2010.
Nischal KC, Khopkar U, Saple DG. Improving adherence to antiretroviral therapy. Indian J Dermatol Venereol Leprol. 2005;71(5):316–20.
Mills EJ, Nachega JB, Buchan I, Orbinski J, Attaran A, Singh S, et al. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–90.
Sledjeski EM, Delahanty DL, Bogart LM. Incidence and impact of posttraumatic stress disorder and comorbid depression on adherence to HAART and CD4+ counts in people living with HIV. AIDS Patient Care STDS. 2005;19(11):728–36.
Kalichman SC, Rompa D, DiFonzo K, Simpson D, Austin J, Luke W, et al. HIV treatment adherence in women living with HIV/AIDS: research based on the information–motivation–behavioral skills model of health behavior. J Assoc Nurses AIDS Care. 2001;12(4):58–67.
Kalichman SC, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14(5):267–73.
Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P, Makhema J, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 2003;34(3):281–8.
Gordillo V, del Amo J, Soriano V, Gonzalez-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13(13):1763–9.
Berg CJ, Michelson SE, Safren SA. Behavioral aspects of HIV care: adherence, depression, substance use, and HIV-transmission behaviors. Infect Dis Clin North Am 2007; 21(1):181–200, x.
Ware NC, Wyatt MA, Tugenberg T. Social relationships, stigma and adherence to antiretroviral therapy for HIV/AIDS. AIDS Care. 2006;18(8):904–10.
Shriver MD, Everett C, Morin SF. Structural interventions to encourage primary HIV prevention among people living with HIV. AIDS. 2000;14(Suppl 1):S57–62.
Kagee A, Remien RH, Berkman A, Hoffman S, Campos L, Swartz L. Structural barriers to ART adherence in Southern Africa: challenges and potential ways forward. Glob Public Health. 2011;6(1):83–97.
Coetzee B, Kagee A, Vermeulen N. Structural barriers to adherence to antiretroviral therapy in a resource-constrained setting: the perspectives of health care providers. AIDS Care. 2011;23(2):146–51.
Kagee A, Delport T. Barriers to adherence to antiretroviral treatment: the perspectives of patient advocates. J Health Psychol. 2010;15(7):1001–11.
Hardon AP, Akurut D, Comoro C, Ekezie C, Irunde HF, Gerrits T, et al. Hunger, waiting time and transport costs: time to confront challenges to ART adherence in Africa. AIDS Care. 2007;19(5):658–65.
Dahab M, Charalambous S, Hamilton R, Fielding K, Kielmann K, Churchyard GJ, et al. “That is why I stopped the ART”: patients’ & providers’ perspectives on barriers to and enablers of HIV treatment adherence in a South African workplace programme. BMC Public Health. 2008;18(8):63.
Roura M, Busza J, Wringe A, Mbata D, Urassa M, Zaba B. Barriers to sustaining antiretroviral treatment in Kisesa, Tanzania: a follow-up study to understand attrition from the antiretroviral program. AIDS Patient Care STDS. 2009;23(3):203–10.
Swartz L, Dick J. Managing chronic diseases in less developed countries. BMJ. 2002;325(7370):914–5.
Cole FL, Abel C. Climate of care and nurses’ attitudes towards AIDS in the emergency department. Emerg Nurse. 2000;8(4):18–24.
Gueritault-Chalvin V, Kalichman SC, Demi A, Peterson JL. Work-related stress and occupational burnout in AIDS caregivers: test of a coping model with nurses providing AIDS care. AIDS Care. 2000;12(2):149–61.
Murray LK, Semrau K, McCurley E, Thea DM, Scott N, Mwiya M, et al. Barriers to acceptance and adherence of antiretroviral therapy in urban Zambian women: a qualitative study. AIDS Care. 2009;21(1):78–86.
Smit R. HIV/AIDS and the workplace: perceptions of nurses in a public hospital in South Africa. J Adv Nurs. 2005;51(1):22–9.
Maskew M, MacPhail P, Menezes C, Rubel D. Lost to follow up: contributing factors and challenges in South African patients on antiretroviral therapy. S Afr Med J. 2007;97(9):853–7.
Posse M, Meheus F, van Asten H, van der Ven A, Baltussen R. Barriers to access to antiretroviral treatment in developing countries: a review. Trop Med Int Health. 2008;13(7):904–13.
Tuller DM, Bangsberg DR, Senkungu J, Ware NC, Emenyonu N, Weiser SD. Transportation costs impede sustained adherence and access to HAART in a clinic population in southwestern Uganda: a qualitative study. AIDS Behav. 2010;14(4):778–84.
Nachega JB, Knowlton AR, Deluca A, Schoeman JH, Watkinson L, Efron A, et al. Treatment supporter to improve adherence to antiretroviral therapy in HIV-infected South African adults. A qualitative study. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S127–33.
Weiser SD, Tuller DM, Frongillo EA, Senkungu J, Mukiibi N, Bangsberg DR. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS ONE. 2010;5(4):e10340.
Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003;15(1):49–69.
Derlega VJ, Winstead BA, Greene K, Serovich J, Elwood WN. Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. J Health Psychol. 2002;7(4):415–32.
Nothling J. Strukturele hindernisse tot ART volhoubaarheidheid onder MIV positiewe pasiënte. Unpublished Masters Thesis, Stellenbosch University; 2009.
De Vellis RF (1991) Scale development: theory and applications. Applied Social Research Methods Series. Newbury Park: SAGE.
Bolton P, Wietse A, Tol JB. Introduction to special issue: combining qualitative and quantitative research methods to support psycho social and mental health programmes. Intervention. 2009;7(3):181–6.
Stevens J. Applied multivariate statistics for the social sciences. 2nd ed. Hillsdale: Erlbaum; 1992.
Schmid J, Leiman JM. The development of hierarchical factor solutions. Psychometrika. 1957;22:53–61.
De Bruin D. The dimensionality of the general work scale. A hierarchical exploratory factor analysis. SA J Ind Psychol. 2006;32(4):68–75.
Field AP. Discovering statistics using SPSS: (and sex, drugs and rock’n’roll). 2nd ed. London: SAGE; 2005.
Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39:31–6.
Miles KK, Clutterbuck DJ, Seitio OO, Sebego MM, Riley AA. Antiretroviral treatment roll-out in a resource-constrained setting: capitalizing on nursing resources in Botswana. Bull World Health Organ. 2007;85(7):555–60.
Jaffar S, Govender T, Garrib A, Welz T, Grosskurth H, Smith PG, et al. Antiretroviral treatment in resource-poor settings: public health research priorities. Trop Med Int Health. 2005;10(4):295–9.
Falagas ME, Zarkadoulia EA, Pliatsika PA, Panos G. Socioeconomic status (SES) as a determinant of adherence to treatment in HIV infected patients: a systematic review of the literature. Retrovirology. 2008;1(5):13.
Nguyen VK, Ako CY, Niamba P, Sylla A, Tiendrebeogo I. Adherence as therapeutic citizenship: impact of the history of access to antiretroviral drugs on adherence to treatment. AIDS. 2007;21(Suppl 5):S31–5.
Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDS. 2006;20(5):359–68.
Duff P, Kipp W, Wild TC, et al. Barriers to accessing highly active antiretroviral therapy by HIV-positive women attending an antenatal clinic in a regional hospital in western Uganda. J Int AIDS Soc. 2010;13:37.
Johnson LF. Access to antiretroviral treatment in South Africa, 2004–2011. S Afr J HIV Med. 2012;13(1):22–7.
Dorrington RE, Johnson LF, Bradshaw D, Daniel T. The demographic impact of HIV/AIDS in South Africa. National and Provincial indicators for 2006. Cape Town: Centre for Actuarial Research, South African Medical Research Council and Actuarial Society of South Africa; 2006.
Remien RH, Hirky AE, Johnson MO, Weinhardt LS, Whittier D, Le GM. Adherence to medication treatment: a qualitative study of facilitators and barriers among a diverse sample of HIV + men and women in four US cities. AIDS Behav. 2003;7(1):61–72.
Tomlinson M, Rohleder P, Swartz L, Drimie S, Kagee A. Broadening psychology’s contribution to addressing issues of HIV/AIDS, poverty and nutrition: structural issues as constraints and opportunities. J Health Psychol. 2010;15(7):972–81.
Ivers LC, Chang Y, Gregory Jerome J, Freedberg KA. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. 2010;26(7):33.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coetzee, B., Kagee, A. The Development of an Inventory to Assess the Structural Barriers to Clinic Attendance and Pill-taking Amongst Users of Antiretroviral Therapy. AIDS Behav 17, 319–328 (2013). https://doi.org/10.1007/s10461-012-0374-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0374-z