Abstract
While individual determinants of HIV risk among MSM have been widely studied, there is limited understanding of how relational characteristics determine sexual risk. Based on data collected among 300 South African men who have sex with men (MSM) and using cluster analysis, this study developed a typology of four partnership types: the “Race–Economic Similar,” “Age–Race–Economic Discordant,” “Non-regular Neighbourhood,” and “Familiar” partnership types. Support for the meaningfulness of these types was found through associations of these partnership types with participant characteristics and characteristics of the last anal sex event. Furthermore, in a multivariate analysis, only partnership type independently predicted whether the last anal sex event was unprotected. Findings of the study illustrate the importance of taking into account the relational context in understanding unprotected sexual practices and present ways to target intervention efforts as well as identify relationship specific determinants of unprotected sex.
Resumen
Aunque los determinantes de riesgos individuales de VIH en HSH han sido ampliamente estudiados, existe un conocimiento limitado de como las características de las relaciones de parejas determinan el riesgo sexual. Basado en los datos recolectados entre 300 hombres sudafricanos que tienen sexo con hombres (HSH) y usando un análisis de agrupamiento, este estudio elaboró una tipología de cuatro tipos de relaciones: “Racial-Económica Similar,” “Edad-Racial-Económica Discordante,” “No del mismo Barrio,” y “Familiar.” Lo validez de estos tipos de relaciones fue encontrada a través de las asociaciones de estas parejas con las características de los participantes y características del último evento de sexo anal. Además, en el análisis multivariado, solamente el tipo de pareja predijo de forma independiente si el último evento de sexo anal fue sin protección. Los resultados de este estudio ilustran la importancia de tener en cuenta el contexto de la relación de pareja en la comprensión de las prácticas sexuales sin protección y presenta maneras de fijar esfuerzos de intervención así como identificar determinantes de las relaciones específicas del sexo sin protección.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Even though sexual risk practices are usually understood as occurring in a social context, most empirical studies that aim to identify determinants of sexual risk behavior test individual level factors. If interpersonal factors are included, they are studied directly in relationship to sexual risk. In this study, we wanted to explore whether it is possible to identify types of sexual partnerships, whether these types of partnerships are engaged in by different kinds of persons, and whether sexual risk is more prevalent in one kind of partnership type compared to others.
There is a long tradition of studies exploring and testing individual-level models of sexual risk behaviors and these studies have produced important directions for HIV prevention strategies. These overlapping models include the Health Belief model [1–3], Theories of Reasoned Action and Planned Behavior [4–8], and the Information-Motivation-Behavioral Skills Model [9]. Outcomes of these studies have informed various safer sex prevention interventions that have been proven to be successful in reducing HIV risk behaviors. Fisher and colleagues [10], for instance, tested an intervention that addressed AIDS risk reduction information, motivation, and behavioral skills deficits that had been empirically identified in a population of college students. The intervention did not only increase in AIDS risk reduction information, motivation, and behavioral skills, but also resulted in significant increases in AIDS preventive behaviors at a long-term follow-up.
Besides these determinants that are directly related to health, other individual-level factors have been found to be associated with HIV risk behavior as well. Such factors include mood states, personal history and various personality characteristics. Depression has for example been found to be related to sexual risk practices [11, 12], although study outcomes are inconsistent. In terms of personal history, many studies have explored the role of trauma, sexual abuse [13–16] and intimate partner violence [17] in particular. Personality characteristics that have been demonstrated to be related to sexual risk include internalized homophobia [18, 19] and sexual compulsivity [20–23]. Factors more directly related to actual risk behavior are alcohol and substance use. Numerous studies have demonstrated the association between alcohol and substance use and sexual risk (see for instance [24–27] and successful interventions have been developed that addressed alcohol use in relation to sexual risk (e.g., see Witte et al. [28]).
The acknowledgment of the limitations of individual-level factors in understanding sexual risk [29, 30] and the need for intervention strategies that not only address individual factors but also include interpersonal and structural factors [31–36], have resulted in various studies exploring the relation between various interpersonal and structural factors and HIV risk. For instance, Poppen et al. [37] found that the dyadic variable of seroconcordance independently contributed to the prediction of unprotected anal sex with the most recent male partner beyond individual characteristics, stressing the importance of examining both individual and dyadic characteristics in the study of sexual behavior. Several other studies looked at partner type (primary versus casual) and HIV risk. One study, for instance, showed how the effect of alcohol consumption varies according to partner type: rates of unprotected anal intercourse varied as a function of alcohol use in sex with non-primary partners, but not in sex with primary partners [38]. Another study showed that sexual risk differed among various types of casual partners (one night stands and “sex buddies”) [39]. Probably the most studied relationship characteristic, although primarily studied in samples of women, is relationship power; several studies have demonstrated the direct association between relationship power and sexual risk [40–43].
Quantitative studies that explored the role of relational characteristics and structural factors generally only made a direct, bivariate link with sexual risk. Few empirical studies have explored the role of interpersonal and structural factors comprehensively. Studies that looked at these factors comprehensively are more likely to have adopted a qualitative approach, which seems more suitable [44–47].
Acknowledging the need for a more in-depth understanding of the interpersonal context of sexual risk, we set out to explore whether it is possible to distinguish types of partnerships in which men have sex with one another. Factors we expected to differentiate among such partnership types include age differences, difference in race and wealth, kind of involvement, and where partners met each other. Is it possible to identify partnership types based on such relational characteristics? Subsequently, we explored whether these partnership types were associated with sociodemographic and psychosocial characteristics of study participants and characteristics of the last time study participants had had anal sex with the respective male partner. Regarding the latter, we were interested in characteristics such as the place in which men had had sex, the specific sexual role men engaged in, whether alcohol was used and a transaction was involved. Finally, we explored the role of partnership types in explaining the risk of HIV transmission: does distinguishing partnership types have any relevance for understanding the occurrence of unprotected anal intercourse?
We expect our findings to have theoretical and practical relevance. If distinguishing partnership types is meaningful, it will contribute to our understanding of the way in which interpersonal factors contribute to sexual risk. Practically, our findings will facilitate targeting of HIV prevention activities by identifying subgroups of MSM as well as determinants that are relevant within specific relational contexts.
Data for the current study have been collected in South Africa. In terms of same-sex sexuality, South Africa has some specific features that set it apart from other countries. First of all, South Africa is one of the few countries where sexual orientation is acknowledged in the Constitution, while homosexuality was criminalized during Apartheid. At the same time, though, the social acceptance of homosexuality is extremely low [48] as elsewhere in Africa. While for a long time homosexual transmission of HIV did not receive any formal attention [49], gay men and other MSM are now included in South Africa’s National Strategic Plan [50].
Methods
Procedure
For this study, men were eligible to participate if they [1] lived in the greater Pretoria metropolitan area; [2] were between 18 and 40 years old; [3] reported having had oral, anal, or masturbatory sex with at least one man in the preceding year, regardless of involvement with women and including men who self-identify as gay; and [4] were conversant in English. To promote heterogeneity in the sample, our target was to stratify participants by age (MSM above and below 25 years of age) race and place of living (white MSM, black MSM living in townships and black MSM not living in townships). Because accessibility to MSM in South Africa varies based on race and place of living, multiple recruitment strategies were deployed in order to accomplish heterogeneity. White men were recruited at a local gay night club and invited to participate in the study. Black, men living in the city were invited to attend social events at an LGBT community centre where they were given the opportunity to participate in the study. For black men living in townships, social functions were held in various locations throughout local townships and attendees were invited to participate in the study. Informed consent was obtained verbally by the interviewers. Once confirmed, all participants were asked to fill out the questionnaire on the spot. Privacy was maintained by having participants complete the survey in quiet, usually adjacent rooms. A total of three hundred men were surveyed for the project.
Interviews were administered using Computer-Assisted Self-Interviewing in order to minimize social desirability bias. Participants received an incentive of 75 ZAR (about $9) for their participation in the study or were compensated in kind (food and non-alcoholic drinks). Participant recruitment and data collection were conducted from October to December 2008. The research protocol was approved by the Institutional Review Boards at the New York State Psychiatric Institute (New York, USA) and the Human Sciences Research Council (Pretoria, South Africa).
Measures
The survey collected information on characteristics of the last sex event (LSE) that involved anal sex with a male partner, behavioral determinants, and demographic characteristics. Participants were asked questions about their LSE with a man that involved anal sex, including partnership characteristics such as how long ago they had met the respective partner, where they met, the relationship to this partner, and other relational attributes: discrepancies or agreements in age, race, neighbourhood, economic status, and gender expression. Participants were also asked questions regarding the sexual encounter such as where it took place, whether drugs or alcohol were used, whether it was in exchange for money or food, what type of sex occurred, knowledge of HIV status and whether condoms were used. Unprotected anal intercourse (UAI) during the LSE was defined as engaging in any anal sex without using a condom.
Behavioral determinants were assessed using constructs from the Information, Motivation, Behavioral Skills Model (IMB) model; this model has been used successfully to explain and change safer sex behavior on an individual level and has also been validated in South Africa [51, 52]. The IMB-constructs include HIV knowledge, social support, perceived social norms, and self-efficacy regarding HIV preventive behaviors. All of the IMB items were assessed using previously validated instruments [53–55]. All of the IMB constructs other than knowledge were measured on five-point Likert scales. HIV knowledge was measured using 15 items. HIV knowledge questions included: ‘‘As long as both partners wash themselves after sex, it is not necessary to use condoms’’; ‘‘Having a shower after sex prevents the spread and infection of HIV, therefore it is not necessary to use condoms’’; ‘‘It is easy to get HIV by sharing a meal with someone who is HIV infected’’; and ‘‘You can tell by looking at someone if they have HIV.’’ Response options were ‘true,’ ‘false’ or ‘do not know.’ HIV knowledge scores were calculated as the number of correct answers provided; ‘do not know’ was coded as incorrect. Social support was measured using five items that asked how true it would be that there is someone that the person can rely on for money, food, a place to stay, to talk to if he has problems, to accompany him to the doctor, or help him if he gets hurt (α = 0.86). Response options ranged from 1 = ‘Never true’ to 5 = ‘Always true.’ Social norms supporting HIV prevention were measured using 4 items that asked how true it would be that most people who are important to the person think that he should use a condom during insertive or receptive anal sex with a steady or non-steady partner (α = 0.89). Response options ranged from 1 = ‘Very untrue’ to 5 = ‘Very true.’ Self-efficacy regarding HIV prevention was assessed by measuring respondents’ self-efficacy for implementing HIV preventive skills. The measure included six items that asked how easy it would be for the respondent to perform certain HIV preventive behaviors, such as talk about condom use with regular/steady partners, get tested for HIV, and not have any insertive or receptive anal sex without a condom (α = 0.81). Response options ranged from 1 = ‘Very difficult to do’ to 5 = ‘Very easy to do.’ For all IMB items, a high score indicates a stronger presence of the construct.
Data Analysis
Using two-step cluster analysis, all partnership characteristics of the LSE assessed in the study were used to generate clusters that would characterize sexual partnership patterns among the study population. Schwarz’s Bayesian Criterion and log-likelihood distance measures were used as the clustering criterion to select the ‘best’ number of clusters. Once clusters were generated, they were assessed by the authors to determine if they represent valid and distinguishable sexual partnership patterns. Exploratory analyses were then run to assess how these sexual partnership types related to respondent-level demographic characteristics and behavioural determinants. Next, analyses were run to assess how the sexual partnership types related to characteristics of the last anal sex event with a male partner. Ultimately, logistic regression was run to assess how sexual relationship types related to unprotected anal intercourse (UAI) during the LSE, while controlling for several respondent-level variables as potential confounders. SPSS 17.0 was used for all statistical analyses.
Results
Participants
Participants’ age ranged from 18 to 40 years with a mean of 26.1 years (SD = 5.9). Approximately two-thirds (64.3 %) of participants were Black and one-third (32.7 %) were White. Half of the participants (49.7 %) reported living in a township, all of whom were Black. Participants ranged in educational level from having not completed primary school to holding post-graduate degrees. About one-third (38.0 %) of respondents had graduated from secondary school. The majority (83.0 %) self-identified as gay; 9.7 % self-identified as bisexual, 3.7 % as straight, and 2.0 % as transgender.
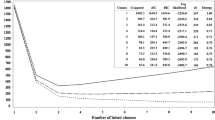
Cluster Analysis
The two-step cluster analysis identified four sexual partnership types as the ‘best’ fit for the data based on a Schwarz’s Bayesian Criterion score of 3605.784 and the largest ratio of log-likelihood distance measures (1.262) compared to other possibilities (1.231 for three clusters and 1.175 for five clusters). Using the distribution of the characteristics of the partnership during the LSE among the four sexual partnership types, we labeled them as [1] race–economic similar (32.6 %); [2] age–race–economic discordant (28.9 %); [3] non-regular neighbourhood (23.0 %) and [4] familiar (15.5 %; Table 1). The race–economic similar partnership type was characterized by high concordance among the relational attributes (age, race, economic status, gender expression) and featured a particularly high proportion of partners with a similar economic status (76.9 %) compared to the other partnership types. The age–race–economic discordant partnership type was characterized by discrepancies in relational attributes. Particularly, this category featured the lowest proportion of partners with similar age (7.2 %; in most of these cases, 72.5 %, the partner was older) and similar economic status (0 %; 50.7 of the partners was richer than the participant), and the largest proportion of interracial couples (23.2 %). The non-regular neighbourhood partnership type was characterized by the highest proportion of pre-existing partnerships that were not steady relationships (54.1 %) and partners from the same neighbourhood (64.9 %). The familiar partnership type was also characterized by a low proportion of concordance on age (10.9 %) and economic status (12.7 %); this category featured the highest proportion of previously known partners (both those in a relationship (45.5 %) and known partners that had sex for the first time (27.3 %, combined (82.8 %)) and the highest proportion of partners from a different neighbourhood (83.6 %).
Characterization of Clusters
Bivariate comparisons of the sexual partnership types on respondent-level demographic characteristics and behavioral determinants showed that the partnership types differed on age, race, living in a township, education, social support and self-efficacy of HIV prevention (p < 0.05) (Table 2). The non-regular neighbourhood partnership type had the highest proportions of respondents aged 25 and older (74.2 %), of respondents who were Black (91.9 %), and of respondents living in a township (86.5 %). The non-regular neighbourhood type also had the least social support (3.6) and self-efficacy of HIV prevention (2.8). The familiar partnership type had the highest proportions of respondents who were White (60.0 %) and not living in a township (67.3 %).
Bivariate comparisons of the sexual partnership types on characteristics of the LSE showed that the partnership types differed according to where sex occured, alcohol/drug use, transactional sex, sexual roles (insertive and/or receptive), knowledge of HIV status, and UAI (p < 0.05; Table 3). The race–economic similar partnership type had the lowest proportion of transactional sex (3.8 %). The age–race–economic discordant partnership type had the highest proportion of sex in a hotel (11.8 %) and the lowest proportion of sex at home (25.0 %). The non-regular neighbourhood partnership type had the highest proportions of transactional sex (32.4 %), of respondents who were penetrated (72.2 %), and the lowest proportion of respondents that knew their partner was HIV negative before they had sex (3.0 %). UAI occurred in 31 % of the sexual events described. The non-regular neighbourhood partnership type had the highest proportion of partners that did not discuss their HIV status (72.7 %) and who engaged in UAI (45.5 %), although the difference was not significant.
Clusters and Sexual Risk
In bivariate analyses, none of the respondent-level variables were associated with UAI during the LSE except for race (p = 0.02) (Table 4). The non-regular neighbourhood partnership type and the familiar partnership type were both associated with UAI in bivariate analyses (p < 0.05). In a multivariate model, the adjusted ORs of UAI during the LSE were 3.30 (95 % CI: 1.34–8.12) for the non-regular neighbourhood partnership type and 2.29 (95 % CI: 1.04–5.02) for the familiar partnership type (p < 0.05).
Discussion
Based on seven characteristics of sexual partnerships, we were able to distinguish four distinct sexual partnership types. Support for the meaningfulness of these types comes from the fact that these partnership types were linked to characteristics of the study participants as well as characteristics of the last anal sex event with a male partner. Finally, in a multivariate analysis, partnership type was the only variable that independently explained the occurrence of unprotected anal intercourse in the last anal sex event.
The first partnership type, race–economic similar, is distinguished because of the similarity between partners, especially in socioeconomic respect; this partnership type was the least likely to involve transactional sex or alcohol use before sex. The second type, age–race–economic discordant, is primarily characterized by the age, racial and economic disparity between partners; compared to the other partnership types, partners were most likely to be of different race, while the partner was most likely to be older, and the actual sex was the least likely to take place in the home of the participant. The non-regular neighbourhood partnership type stands out because of the relational context: partners knew each other, were more likely to have had sex before the last anal sex event, but were not involved in an ongoing relationship; partners were most likely to have met in a public space (including shebeens and taverns); compared to other study participants, participants in these partnership types were most likely to be more feminine, relatively older, most likely to be black and to live in a township; these men experienced the lowest level of social support, while HIV prevention self-efficacy among these men was relatively the lowest. The last anal sex event in this partnership type was the most likely to have been unprotected. The final partnership type, familiar, distinguishes itself from the other types because partners in this type were the least likely to live in a township and most likely to be both White; level of education of participants in these partnerships were relatively the highest; furthermore, participants in these partnerships were the most likely to say that they already knew before the last anal sex event that the partner was HIV-negative. The latter might explain why the proportion of unprotected sex in the last anal sex event for this partnership was comparatively high.
Our study demonstrates that in order to understand sexual risk practices, it is meaningful to distinguish between types of partnerships that form the context of the sexual behavior. The relevance of this approach is further supported by the fact that the partnership types we were able to distinguish were associated with several demographic characteristics of the index person and characteristics of the last anal sex event. The importance of this relational approach is further underscored by the fact that in predicting sexual risk, none of the individual level factors except for race played a significant role.
For this study, we adopted an exploratory approach. Given the successfulness of this attempt, it seems relevant to develop a comprehensive theory about sexual partnership dimensions, how they relate to each other, and to HIV risk behavior. Based on this theory, hypotheses can be developed which could be tested in subsequent studies. The findings reported here suggest some critical elements of such a theory and hint at other, not yet included, factors.
The findings suggest that unprotected sex is differently determined in each partnership type. In the casual neighbourhood type, lack of HIV status disclosure, transactional sex, and being the receptive partner, as well as limited HIV prevention self-efficacy and social support seem to be dominant. In the familiar type, knowing that the partner was HIV negative likely contributed to not using a condom. In the other two partnerships types, unprotected sex was less common, which makes it harder to identify the most likely correlates of unprotected sex. Having had the last anal sex with a partner with whom the men were in a steady relationship seems to increase the chances of unprotected sex in the familiar partnership type, but not in the race–economic similar and age–race–economic discordant partnership types.
Although one might expect that similarity among partners creates a balance and results in increased protection, similarity does not seem to be a necessary factor. Not only in the race–economic similar partnership type, but also in the age–race–economic discordant partnership type were men most likely to protect themselves during sex (these two groups of men also did not differ in terms of demographic characteristics and behavioral determinants). It seems that factors that indicate a power advantage for the partner do not necessarily have to lead to unprotected sex.
The findings also elicit some new questions. Answers to these questions are relevant for a theory about the dimensions of sexual partnerships. To what extent do men get in these sexual partnerships what they desire, and to what extent is what these men desire shared or individual? Is this related to the ability to protect oneself? Without imposing standards of love and intimacy, one might wonder whether the men in the casual neighbourhood partnership type get the kind of partnership they desire or accept what they can get. To what extent are the kind of sexual partnerships that the men engage in affected by structural factors, such as the scarcity of partners with identical or complementary desires?
In terms of practical relevance, the partnership that stands out most is the non-regular neighborhood type because it was the most likely to have involved unprotected anal intercourse. Several factors seem to contribute to the relative vulnerability of participants in this partnership type. The sexual interactions in this partnership type seem to be of casual nature, even though men quite often had sex with each other before. While participants in these interactions are quite often older than their partners, they might lack power due to their relatively higher level of femininity. Lack of social support as well as reduced HIV prevention self-efficacy makes them particularly vulnerable. Partners’ HIV status was the least likely to be discussed in this partnership type. These partnership types are most likely to be found among Black men in townships. These findings indicate what kinds of partnership types deserve attention as well as which determinants prevention efforts should focus on: in prevention targeting the “non-regular neighborhood” partner type, HIV prevention self-efficacy seems an important determinant to be addressed.
In interpreting our findings, several limitations have to be taken into account. First of all, data were collected on the level of the index person. A more thorough approach would combine data from both persons making up the partnership. Collecting information from both partners might also counteract the limitation of self-report. Our data primarily reflect the participants’ subjective assessments; this is particularly a problem for subjective issues for which hard empirical indications are not available, such as masculinity and femininity, compared to, for instance, the possession of a car as an indicator of personal wealth. Second, the use of a cross-sectional design limits the ability to draw causal conclusions; it is, for instance, possible that men who want unprotected sex look for specific partnership types, instead of what we assumed, namely that risk results from the partnership type. Furthermore, any unprotected anal sex was understood as involving sexual risk; although we think this approach is warranted, it is possible that in some occasions not using a condom did not imply any risk of HIV transmission. Finally, it is not clear to what extent the partnership types that we distinguished here can be generalized to other populations of MSM.
In summary, the outcomes of this study underscore the importance of integrating the relational context in understanding sexual risk practices. Distinguishing various partnership types also creates the option of exploring the specific mechanisms at play within each partnership type that contribute to the occurrence of sexual risk.
References
Oyekale AS, Oyekal TO. Application of health belief model for promoting behaviour change among Nigerian single youths. Afr J Reprod Health. 2010;14(2):63–75.
Lin P, Simoni JM, Zemon V. The health belief model, sexual behaviors, and HIV risk among Taiwanese immigrants. AIDS Educ Prev. 2005;17(5):469–83.
Downing-Matibag TM, Geisinger B. Hooking up and sexual risk taking among college students: a health belief model perspective. Qual Health Res. 2009;19(9):1196–209.
Munoz-Silva A, Sanchez-Garcia M, Nunes C, Martins A. Gender differences in condom use prediction with theory of reasoned action and planned behaviour: the role of self-efficacy and control. Aids Care. 2007;19(9):1177–81.
Sneed CD, Morisky DE. Applying the theory of reasoned action to condom use among sex workers. Soc Behav Pers. 1998;26(4):317–27.
Jemmott LS, Jemmott JB. Applying the theory of reasoned action to aids risk behavior—condom use among Black-women. Nurs Res. 1991;40(4):228–34.
Brecht ML, Stein J, Evans E, Murphy DA, Longshore D. Predictors of intention to change HIV sexual and injection risk behaviors among heterosexual methamphetamine-using offenders in drug treatment: a test of the AIDS risk reduction model. J Behav Health Ser Res. 2009;36(2):247–66.
Catania JA, Coates TJ, Kegeles S. A test of the aids risk reduction model—psychosocial correlates of condom use in the Amen Cohort survey. Health Psychol. 1994;13(6):548–55.
Fisher JD, Fisher WA. Changing aids-risk behavior. Psychol Bull. 1992;111(3):455–74.
Fisher JD, Misovich SJ, Kimble DJ, Fisher WA, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15(2):114–23.
Alvy LM, McKirnan DJ, Mansergh G, Koblin B, Colfax GN, Flores SA, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2011;15(6):1171–9.
Houston E, Sandfort T, Dolezal C, Carballo-Diéguez A. Depressive symptoms among MSM who engage in bareback sex: Does mood matter? Aids Behav. doi:10.1007/s10461-012-0156-7.
El-Bassel N, Wingood G, Wyatt GE, Jemmott JB, Pequegnat W, Landis JR, et al. Prevalence of child and adult sexual abuse and risk taking practices among HIV Serodiscordant African-American couples. AIDS Behav. 2010;14(5):1032–44.
Meade CS, Kershaw TS, Hansen NB, Sikkema KJ. Long-term correlates of childhood abuse among adults with severe mental illness: adult victimization, substance abuse, and HIV sexual risk behavior. AIDS Behav. 2009;13(2):207–16.
Catania JA, Paul J, Osmond D, Folkman S, Pollack L, Canchola J, et al. Mediators of childhood sexual abuse and high-risk sex among men-who-have-sex-with-men. Child Abuse Neglect. 2008;32(10):925–40.
Gore-Felton C, Kalichman SC, Brondino MJ, Benotsch EG, Cage M, DiFonzo K. Childhood sexual abuse and HIV risk among men who have sex with men: initial test of a conceptual model. J Fam Violence. 2006;21(4):263–70.
Mittal M, Senn TE, Carey MP. Intimate partner violence and condom use among women: does the Information-Motivation-Behavioral Skills Model explain sexual risk behavior? Aids Behav. 2012;16(4):1011–9.
Hatzenbuehler ML, Nolen-Hoeksema S, Erickson SJ. Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: results from a prospective study of bereaved gay men. Health Psychol. 2008;27(4):455–62.
Newcomb ME, Mustanski B. Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: a meta-analysis. Arch Sex Behav. 2011;40(1):189–99.
Dodge B, Reece M, Cole SL, Sandfort TGM. Sexual compulsivity among heterosexual college students. J Sex Res. 2004;41(4):343–50.
Semple SJ, Strathdee SA, Zians J, McQuaid J, Patterson TL. Correlates of obsessive–compulsive disorder in a sample of HIV-positive, methamphetamine-using men who have sex with men. AIDS Behav. 2011;15(6):1153–60.
Smolenski DJ, Ross MW, Risser JMH, Rosser BRS. Sexual compulsivity and high-risk sex among Latino men: the role of internalized homonegativity and gay organizations. Aids Care. 2009;21(1):42–9.
Benotsch EG, Kalichman SC, Kelly JA. Sexual compulsivity and substance use in HIV-seropositive men who have sex with men: prevalence and predictors of high-risk behaviors. Addict Behav. 1999;24(6):857–68.
Lane T, Shade SB, McIntyre J, Morin SF. Alcohol and sexual risk behavior among men who have sex with men in South african township communities. Aids Behav. 2008;12(4 Suppl):S78–85. Epub 2008/04/09.
Woolf SE, Maisto SA. Alcohol use and risk of HIV infection among men who have sex with men. AIDS Behav. 2009;13(4):757–82.
Ross MW, Williams ML. Sexual behavior and illicit drug use. Annu Rev Sex Res. 2001;12:290–310.
Van Tieu H, Koblin BA. HIV, alcohol, and noninjection drug use. Curr Opin HIV AIDS. 2009;4(4):314–8.
Witte SS, Altantsetseg B, Aira T, Riedel M, Chen JH, Potocnik K, et al. Reducing sexual HIV/STI risk and harmful alcohol use among female sex workers in Mongolia: a randomized clinical trial. AIDS Behav. 2011;15(8):1785–94.
Van Campenhoudt L, Cohen M, Guizzardi G, Hausser D, editors. Sexual interactions and HIV risk: new conceptual perspectives in European research. London: Taylor & Francis; 1997.
Kashima Y, Gallois C, McCamish M. The theory of reasoned action and cooperative behaviour: it takes two to use a condom. Brit J Soc Psychol. 1993;32:227–39.
Choi KH, Yep GA, Kumekawa E. HIV prevention among Asian and Pacific Islander American men who have sex with men: a critical review of theoretical models and directions for future research. AIDS Educ Prev. 1998;10(3):19–30.
Kaufman MR, Shefer T, Crawford M, Simbayi LC, Kalichman SC. Gender attitudes, sexual power, HIV risk: a model for understanding HIV risk behavior of South African men. Aids Care. 2008;20(4):434–41.
Amaro H, Raj A. On the margin: power and women’s HIV risk reduction strategies. Sex Roles. 2000;42(7–8):723–49.
Scribner R, Theall KP, Simonsen N, Robinson W. HIV Risk and the alcohol environment advancing an ecological epidemiology for HIV/AIDS. Alcohol Res Health. 2010;33(3):179–83.
Mojola SA. Fishing in dangerous waters: ecology, gender and economy in HIV risk. Soc Sci Med. 2011;72(2):149–56.
Campbell C, Cornish F. Towards a “fourth generation” of approaches to HIV/AIDS management: creating contexts for effective community mobilisation. Aids Care. 2010;22:1569–79.
Poppen PJ, Reisen CA, Zea MC, Bianchi FT, Echeverry JJ. Predictors of unprotected anal intercourse among HIV-positive Latino gay and bisexual men. AIDS Behav. 2004;8(4):379–89.
Vanable PA, McKirnan DJ, Buchbinder SP, Bartholow BN, Douglas JM, Judson FN, et al. Alcohol use and high-risk sexual behavior among men who have sex with men: the effects of consumption level and partner type. Health Psychol. 2004;23(5):525–32.
van den Boom W, Stolte I, Sandfort T, Davidovich U. Serosorting and sexual risk behaviour according to different casual partnership types among MSM: the study of one-night stands and sex buddies. Aids Care. 2012;24(2):167–73.
Campbell ANC, Tross S, Dworkin SL, Hu MC, Manuel J, Pavlicova M, et al. Relationship power and sexual risk among women in community-based substance abuse treatment. J Urban Health. 2009;86(6):951–64.
Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–21.
Pulerwitz J, Amaro H, De Jong W, Gortmaker SL, Rudd R. Relationship power, condom use and HIV risk among women in the USA. Aids Care. 2002;14(6):789–800.
Kershaw TS, Small M, Joseph G, Theodore M, Bateau R, Frederic R. The influence of power on HIV risk among pregnant women in rural Haiti. AIDS Behav. 2006;10(3):309–18.
Bowleg L, Lucas KJ, Tschann JM. “The ball was always in his court”: an exploratory analysis of relationship scripts, sexual scripts, and condom use among African American women. Psychol Women Quart. 2004;28(1):70–82.
Corbett AM, Dickson-Gomez J, Hilario H, Weeks MR. A little thing called love: condom use in high-risk primary heterosexual relationships. Perspect Sex Reprod Health. 2009;41(4):218–24.
Devries KM, Free CJ. Boyfriends and booty calls: sexual partnership patterns among Canadian Aboriginal young people. Can J Public Health. 2011;102(1):13–7.
Cornish F. Making ‘context’ concrete: a dialogical approach to the society-health relation. J Health Psychol. 2004;9(2):281–94.
Roberts B, Reddy V. Pride and prejudice: public attitudes toward homosexuality. HSRC Review. 2008;6(4):9–11.
Sandfort T, Reddy V, Rispel R. Taking research and prevention forward. In: Reddy V, Sandfort T, Rispel R, editors. From social silence to social science: same sex sexuality, HIV & AIDS and gender in South Africa. Pretoria: Human Sciences Research Council; 2009. p. 228–41.
South African National AIDS Council. National strategic plan on HIV, STIs and TB 2012–2016. Pretoria: SANAC; 2011.
Simbayi LC, Kalichman SC, Skinner D, Jooste S, Cain D, Cherry C, et al. Theory-based HIV risk reduction counseling for sexually transmitted infection clinic patients in Cape Town, South Africa. Sex Transm Dis. 2004;31(12):727–33.
Cornman DH, Kiene SM, Christie S, Fisher WA, Shuper PA, Pillay S, et al. Clinic-based intervention reduces unprotected sexual behavior among HIV-infected patients in KwaZulu-Natal, South Africa: results of a pilot study. Jaids J Acq Immun Def. 2008;48(5):553–60.
Bryan AD, Fisher JD, Benziger TJ. Determinants of HIV risk among Indian truck drivers. Soc Sci Med. 2001;53(11):1413–26. Epub 2001/11/17.
Simbayi LC, Kalichman SC, Jooste S, Cherry C, Mfecane S, Cain D. Risk factors for HIV-AIDS among youth in Cape Town. South Africa. Aids Behav. 2005;9(1):53–61. Epub 2005/04/07.
Cornman DH, Schmiege SJ, Bryan A, Benziger TJ, Fisher JD. An information-motivation-behavioral skills (IMB) model-based HIV prevention intervention for truck drivers in India. Soc Sci Med. 2007;64(8):1572–84. Epub 2007/01/30.
Acknowledgments
The study was supported by a grant from amfAR (106973; Principal Investigator: Theo Sandfort, Ph.D.) with additional support from a grant from the National Institute of Mental Health to the HIV Center for Clinical and Behavioral Studies (P30-MH43520; Principal Investigator: Anke E. Ehrhardt, Ph.D.). This research was further supported by a training grant from the National Institute of Mental Health (T32-MH19139, Behavioral Sciences Research in HIV Infection; Principal Investigator: Theo Sandfort, Ph.D.). We would like to thank the men who participated in the study and OUT Well-being, Pretoria, in particular Dawie Nel and Senku Maimane, for support in the implementation of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sandfort, T., Yi, H., Knox, J. et al. Sexual Partnership Types as Determinant of HIV Risk in South African MSM: An Event-Level Cluster Analysis. AIDS Behav 17 (Suppl 1), 23–32 (2013). https://doi.org/10.1007/s10461-012-0294-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-012-0294-y